Abstract
Exposure to cockroach allergen is a strong risk factor for developing asthma. Asthma has been associated with allergen-induced airway epithelial damage and heightened oxidant stress. In this study, we investigated cockroach allergen-induced oxidative stress in airway epithelium, and its underlying mechanisms. We found that CRE could induce reactive oxygen species (ROS) production, particularly mitochondrial-derived ROS, in human bronchial epithelial cells (NHBEs). We then used the RT2 Profiler™ PCR array and identified that COX-2 was the most significantly up-regulated gene related to CRE-induced oxidative stress. miR-155, predicted to target COX-2, was increased in CRE-treated NHBEs, and was showed to regulate COX-2 expression. Moreover, miR-155 can bind COX-2, induce COX-2 luciferase activity, and maintain mRNA stability. Furthermore, CRE-treated miR-155−/− mice showed reduced levels of ROS and COX-2 expression in lung tissues and PGE2 in bronchoalveolar lavage fluid (BALF) compared with wild-type (WT) mice. These miR-155−/− mice also showed reduced lung inflammation and Th2/Th17 cytokines. In contrast, when miR-155−/− mice were transfected with adeno-associated virus (AAV) carrying miR-155, the phenotypic changes in CRE-treated miR-155−/− mice were remarkably reversed, including ROS, COX-2 expression, lung inflammation, and Th2/Th17 cytokines. Importantly, plasma miR-155 levels were elevated in severe asthmatics when compared with non-asthmatics or mild-to-moderate asthmatics. These increased plasma miR-155 levels were also observed in asthmatics with cockroach allergy compared to those without cockroach allergy. Collectively, these findings suggest that COX-2 is a major gene related to cockroach allergen-induced oxidative stress and highlight a novel role of miR-155 in regulating the ROS-COX2 axis in asthma.
Keywords: Asthma, allergen, reactive oxygen species (ROS), asthma, miR-155, cyclooxygenase-2 (COX-2)
INTRODUCTION
Cockroach allergen exposure and sensitization is a particularly strong factor for developing allergic asthma and increases asthma morbidity (1–3). However, the mechanisms underlying cockroach allergen-induced asthma are poorly understood. Oxidative stress has been implicated in airway inflammation and is a determinant of asthma severity (5–8). In response to environmental pollutants (e.g., ultrafine particles, diesel exhaust particles (DEP), and smoking), epithelial and mucosal inflammatory cells may produce ROS, contributing to the pathophysiology of allergic inflammation and asthma (9–12). Though studies are limited, several allergens have been shown to induce ROS production, such as cat dander (13), pollen (14–16), and house dust mite (HDM) (17, 18), leading to allergic inflammation. Airway epithelial cells are the first line of defense against inhaled allergens, and epithelial cell activation is one of the hallmark characteristics of asthma (19). Recent studies suggest that HDM can induce ROS production and dampen antioxidant responses in bronchial epithelial cells (19), and ROS serve as a key checkpoint for IL-33 release by airway epithelia after exposure to Alternaria extract (20). We and others have shown that cockroach allergen can activate airway epithelial cells, thereby leading to allergic inflammation (21–23). However, it remains elusive as to whether cockroach allergen can induce oxidative stress in airway epithelial cells, as well as the related molecular mechanisms by which this induction may occur.
Cyclooxygenase (COX, also known as PTGS) is an oxidative stress-associated gene and a key limiting enzyme catalyzing the production of prostaglandin E2 (PGE2) from arachidonic acid (AA). An interaction has been suggested between ROS and COX-2 whereby COX-2 expression is triggered by ROS (24–26). There are two isoforms of cyclooxygenase, COX-1 (PTGS1) and COX-2 (PTGS2). COX-1 is constitutively expressed in most tissues, while COX-2 is often induced during inflammation (28) and is primarily responsible for the formation of prostaglandins in immune cells. Both COX-2 and its catalyzed product PGE2 were up-regulated during allergic inflammation in mouse models and asthmatic patients (29–33). Importantly, it was shown that COX-2 regulates Th1, Th2, and Th17 cells (31, 34, 35), and PGE2 is associated with the exacerbation of allergen-induced lung inflammation (36), systemic inflammation (37), and IgE production in vivo (38). These findings support the hypothesis that the COX-2-PGE2 axis may play a critical role in regulating cockroach allergen-induced lung inflammation.
Recent studies have implicated miRNAs as noninvasive biomarkers that play crucial roles in the regulation of cytokines and asthma pathogenesis (39). Several miRNAs, such as miR-146a, miR-155, miR-26b, miR-101, miR-137, miR-16 and miR-1297, have been suggested to target COX-2 and regulate COX-2 expression (40–47). Of these, miR-155 was markedly increased in an allergen-induced model of asthma. Intriguingly, studies have shown that miR-155 enhanced COX-2 expression in asthmatic human airway smooth muscle cells (41), and to be considered as a promising target for regulating COX-2 expression in colorectal and other cancers (49). These findings suggest that miR-155 may also be a target for antagonizing COX-2 and allergic inflammation in asthma. In this study, we provide evidence that cockroach allergen-induced oxidative stress in airway epithelia and identified COX-2 as the most significantly up-regulated gene related to oxidative stress. Moreover, we studied the epigenetic mechanisms by which miR-155 regulates COX-2 expression, and provided supporting evidence for a direct functional interaction between miR-155 and COX-2.. Furthermore, we found that miR-155 regulates COX-2 expression and lung inflammation in the cockroach allergen-induced mouse model of asthma. Finally, we show that severe asthmatic patients have higher levels of plasma miR-155 compared with those without asthma or asthmatics with mild-to-moderate asthma. Collectively, findings from these studies suggest a critical but previously unidentified role of miR-155 in regulating the functional axis of ROS-COX-2 in allergic asthma.
MATERIALS AND METHODS
Animals
C57BL/6J and miR-155 knockout (miR-155−/−) mice were purchased from the Jackson Laboratory (Bar Harbor, ME). Animals were maintained under specific pathogen–free conditions at the animal facility of the Johns Hopkins University School of Medicine. All mice were used at 6–8 weeks of age, and all experiments used age- and gender-matched controls. The experimental protocols in this study were reviewed and approved by the Animal Care and Use Committee at the Johns Hopkins University School of Medicine.
Measurement of intracellular ROS production by flow cytometry
ROS were detected using the general and mitochondria-specific oxidative sensitive fluorescent dyes CM-H2DCFDA (ThermoFisher) and MitoSOX (ThermoFisher), respectively. For flow cytometric analysis, human bronchial epithelial cell line (NHBEs, ATCC® CRL-4051™) were treated with 50 µg/mL CRE in the presence or absence of either the antioxidant N-acetyl cysteine (1 to 10 mM) (Sigma) or the mitochondria-specific antioxidant MitoTEMPO (1 to 10 nM) (Sigma) 1 hour prior to treatment in F-12K media at 37°C in a 5% CO2 atmosphere. ROS production was assessed using a FACScalibur flow cytometer (Becton Dickinson Biosciences) for detection of CM-H2DCFDA and MitoSOX. Under the same conditions, ROS production in mitochondria was assessed with MitoSOX by fluorescence microscopy. In brief, cells were incubated with 5 µM MitoSOX and 0.1 µM MitoTracker (ThermoFisher) for 30 min prior to CRE treatment. These cells were then imaged with a Nikon ETi fluorescence microscope. Fluorescence intensities were quantified using ImageJ (NIH).
Air-liquid interface culture
An air-Liquid Interface (ALI) culture system for human airway epithelial cells was used in which isolated epithelial cells from the central airways of human subjects (provided by Dr. Allen Myers at Johns Hopkins Bayview Histology Core Laboratory). These central airways were obtained from human organ donors through an established US provide IIAM. These cells were cultured for 21 days to fully differentiate into mature epithelial cells, as manifested by the formation of more mucociliary epithelium (51, 52). These mature cells were then treated with cockroach extract (CRE, B46, GREER Laboratories) and harvested at various time points, and total RNA was extracted for RT2 Profiler™ PCR array.
RT2 Profiler™ PCR array
Total RNA was isolated with an RNeasy Plus Mini kit (Qiagen), and cDNA templates were synthesized with SuperScript II (Life Technologies) and then loaded on the Human Oxidative Stress RT2 Profiler PCR Array, which included 84 genes functionally involved with the cellular oxidative stress response. The samples were run on an ABI Prism 7300 (Applied Biosystems, Carlsbad, CA) sequence detection system, and data analysis was performed using RT2 Profiler PCR Array Data Analysis software version 2.5 (Qiagen).
Quantitative RT-PCR
Quantitative RT-PCR (qRT-PCR) was performed in triplicate using SYBR®Green Universal 2× qPCR Master Mix (TherFisher) on an ABI Prism 7300 detection system. miR-155 (human, ID: 002623 and mouse, ID 002571) was measured using TaqMan Gene Expression Master Mix (ThermoFisher). Data were analyzed using the 2−ΔΔCT method as described by Livak and Schmittgen(53). The mRNA and miRNA levels were normalized to the internal control gene β-actin and U6 snRNA, respectively. Primer sequences are available upon request.
Western Blotting
Cells were collected and lysed in RIPA buffer (Sigma-Aldrich) containing Protease and Phosphatase Inhibitor Cocktails (Roche). Protein concentration was measured using a BCA™ Protein Assay kit (Pierce). Aliquots of 30–50 µg protein samples were used for SDS-PAGE electrophoresis and then transferred to a polyvinylidene difluoride membrane (Invitrogen). After blocking with 5% non-fat milk in TBST, the membrane was incubated with anti-COX-2 (Abcam, ab23672) or anti-β-actin antibodies. Blots were visualized with an HRP-conjugated secondary antibody (Santa Cruz) and ECL Western blotting detection system (GE Life Sciences).
Cockroach allergen-induced lung inflammation
Generation of a cockroach allergen-induced mouse model of asthma and analysis of lung inflammation was established as described previously (21, 55).
ELISA
BALFs were assessed by ELISA for cytokines (eBioscience) and prostaglandin E2 (Cayman Chemical) according to the manufacturer’s manual. Cockroach allergen-specific IgE and IgG1 serum levels were analyzed by ELISA according to a standard protocol as previously described (55).
Immunofluorescence staining
For immunofluorescence staining, sectioned lung tissues were first blocked using 5% BSA for 1 hour, followed by incubation with anti-COX-2 (Abcam, Ab23672) and epithelial cell marker anti-EpCAM (Abcam, Ab71916) overnight at 4℃. Sample sections were then incubated with secondary antibodies conjugated with Alexa Fluor dyes (ThermoFisher) at room temperature for 1 h. Isotype-matched negative control antibodies (R&D Systems) were used under the same conditions. Nuclei were counterstained with 6-diamidino-2-phenylindole, dihydrochloride (DAPI, ThermoFisher). Sections were mounted with the ProLong Gold Anti-fade Kit (Molecular Probes, Grand Island, NY) and observed with a Nikon Eclipse Ti-U microscope equipped with a DS-Fi2 camera (Nikon). The detection of intracellular superoxide in lung tissues was carried out using dihydroethidium (DHE) (ThermoFisher). To determine the fluorescence signal in tissue sections, fluorescent positive cells in five different high-power fields from each slide were quantified using ImageJ v1.50e (NIH) and presented as mean fluorescence intensity per square micrometer. Two to three slides from each sample were used for analysis.
miR-155−/− mice transfected with Adeno-Associated Virus (AAV)-miR-155
An adeno-associated virus (AAV) vector encoding the enhanced GFP reporter and expressing miR-155 (AAV-CMV-miR-155-eGFP), driven by the cytomegalovirus (CMV) promoter, was generated in SigaGene. The methods for the transfection of AAV into miR-155−/− mice and detection of GFP expression were described as described previously (55).
Transfection of miRNA mimics
Hsa-miR-155 mimics and their corresponding negative controls were purchased from ThermoFisher (USA). Transfection of the miRNA mimics was performed using Lipofectamine™ RNAiMAX (ThermoFisher).
Effect of miR-155 on a COX-2 3’-UTR reporter
A COX-2 reporter downstream of Firefly Luciferase in a vector that also contained Renilla Luciferase (pEZX vector) was obtained from Genecopoeia (Rockville, Maryland, USA), and the dual luciferase system was used to adjust for transfection efficiency. All analyses were performed using HEK293 cells (ATCC). Briefly, cells were seeded in a 6-well plate, and 50 ng of reporter plasmid or parent vector was transfected with 50 ng of a miR-155 mimic or miRNA Allstars Negative Control (both from Qiagen) using Attractene (Qiagen) per the manufacturer’s instructions. Cells were harvested, and dual luciferase assays were performed using the Promega Dual Luciferase Assay kit per the manufacturer’s protocol. Luminescence was measured using a Tecan SPECTRAFluor Plus instrument. After normalization of the Renilla:Firefly signal, the effects of miR-155 and the negative control on the parent and COX-2 reporters were assessed.
Analysis of miRNA-mRNA interaction
A synthetic miR-155 containing a biotin at the 3’end (or a negative control cel-miR-39 biotinylated miRNA, synthesized by Integrated DNA Technologies) was annealed with a complementary strand (Integrated DNA Technologies). 20 ng of the duplex was incubated with cell lysates of airway epithelial cells (10 million cells), and miRNA-mRNA complexes were isolated using streptavidin beads. After acid-phenol chloroform isolation and isopropanol precipitation of RNA, samples were reverse-transcribed using the High-Capacity Reverse Transcription Kit (ThermoFisher). The qPCR analysis was performed by using COX-2 primers to identify bound mRNA, and the enrichment was analyzed by the fold-change in miR-155 pulldown vs. that of the negative control miRNA.
mRNA stability
A549 cells were transfected with miR-155 mimics or control miRNA. After 48 h, these cells were treated with Actinomycin D (ActD, 5 µg/mL, Sigma-Aldrich), and total RNAs were then isolated at 0, 0.5, 1, 2, and 6 hours. The levels of COX-2 mRNA were detected with RT-PCR, and the RNA half-life (t1/2) was calculated by linear regression analysis.
Study population
Detailed descriptions for categorization of study subjects have been previously described (56, 57). Briefly, asthma was defined by a documented history of physician-diagnosed asthma, an FEV1 increase of 12% and 200 mL at least once within the last two years, or positive methacholine challenge. In addition, subjects were classified as moderate persistent or severe persistent based on current NHLBI guidelines. Allergy status was determined by clinical history of aeroallergen sensitivity and a multi-allergen IgE test (ImmunCAP or skin prick test). Allergic rhinitis was defined by allergic status and a clinical history consistent with allergic rhinitis (one or more: nasal congestion, runny nose, sneezing, eye redness or watering). The study of human subjects was approved by the Institutional Review Boards of Penn State College of Medicine Institute.
Measurement of circulating miR-155
Blood was collected by venipuncture in an EDTA purple top tube, and then centrifuged at 3000 RPM in a clinical centrifuge to isolate plasma. For isolation of total RNA, 2 µL of 50 nM synthetic cel-miR-39 was added as a “spike-in” normalization control to 500 µL of plasma(58). Afterwards, 1.5 mL of TRIzol (Life Technologies) reagent was added, followed by 1.5 mL of 100% EtOH. Total RNA was isolated using Direct-zol RNA columns (Zymo Research) according to the manufacturer’s protocol. RNA concentration was measured via A260/280 using a NanoDrop Lite Spectrophotometer (Thermo Scientific). The isolated RNA was reverse-transcribed to cDNA using the qScript microRNA cDNA Synthesis Kit (Quanta BioSciences). Quantification of miRNAs was performed by qRT-PCR on a CFX384 Real-Time System (Bio-Rad) by using stem-loop primers. Levels of miRNAs were expressed as copy number/µl, as determined by a standard curve generated from multiple dilutions of known concentrations of synthesized miR-39.
Statistical analysis
Data are expressed as the means ± SEM for each group. Statistical significance for normally distributed samples was assessed using an independent two-tailed Student’s t test or with ANOVA. Non-normally distributed samples were analyzed by Wilcoxon rank-sum test. Associations between miRNA expression and clinical variables was analyzed by linear regression analysis. All analyses were performed with GraphPad Prism version 5.1 software (GraphPad Software, La Jolla, CA). A p-value <0.05 were considered statistically significant for all analyses.
RESULTS
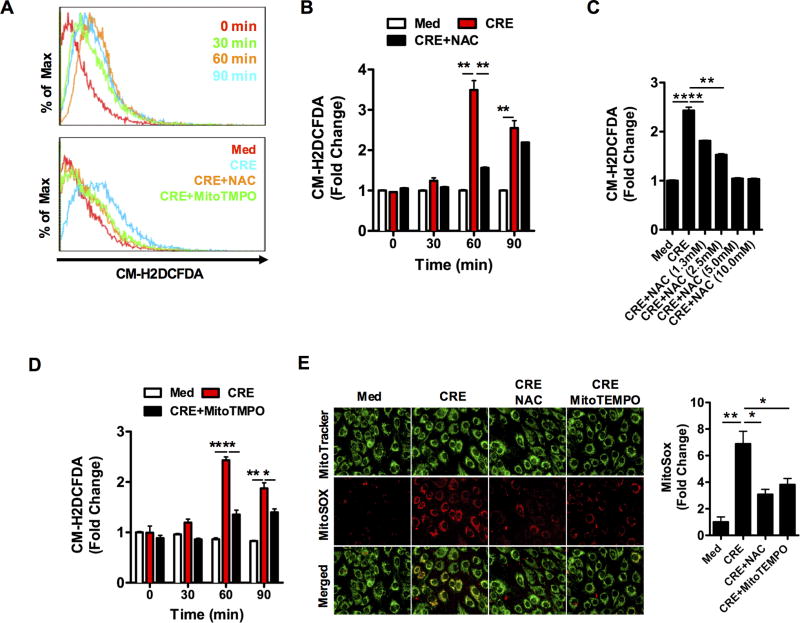
Cockroach allergen induced reactive oxygen species in epithelial cells
ROS are an important mediator that may contribute to oxidative damage and chronic inflammation in allergic diseases (22). To determine whether cockroach allergen can induce ROS generation in airway epithelial cells, intracellular ROS production was detected in NHBE cells after exposure to cockroach extract (CRE). Compared to untreated cells, intracellular ROS production was increased after treatment with CRE, as detected by flow cytometry with CM-H2DCFDA (Fig. 1A, 1B). The increased ROS were markedly abated by NAC in a dose -dependent manner (Fig. 1C). Next, we used MitoTEMPO, a mitochondria-specific antioxidant, to determine whether mitochondrial ROS is a major source for the CRE-induced ROS. As expected, the CRE-induced ROS was remarkably blocked when MitoTEMPO was used (Fig. 1D). This finding was further confirmed by directly detecting mitochondrial ROS expression with MitoSOX, a fluorescent mitochondrial ROS reporter, in CRE-treated NHBEs using co-immunostaining (Fig. 1E). We found that CRE induced the generation of mitochondrial ROS, which was abolished by either NAC or MitoTEMPO (Fig. 1F). These results were also confirmed in A549 cells (Supplementary Fig. 1). Collectively, these findings suggest that CRE can induce ROS production, particularly mitochondrial-derived ROS in airway epithelial cells.
FIGURE 1.
Cockroach allergen induced reactive oxygen species in bronchial epithelial cells (NHBEs). (A) Detection of intracellular ROS production with CM-H2DCFDA by flow cytometry. (B) CRE-induced intracellular ROS production and its inhibition by N-acetyl cysteine (NAC). (C) Dose-dependent inhibition of CRE-induced ROS generation by different doses of NAC. (D) CRE-induced intracellular ROS production and its inhibition by MitoTEMPO. (E) Detection of mitochondrial ROS with MitoSOX by co-immunofluorescence staining for MitoTracker (green) and MitoSOX (red). (F) Quantitative data for MitoSOX expression. Data were from three independent experiments (n=3). CRE: cockroach extract. Data are expressed as the mean ± SEM. *P<0.05, **P<0.01.
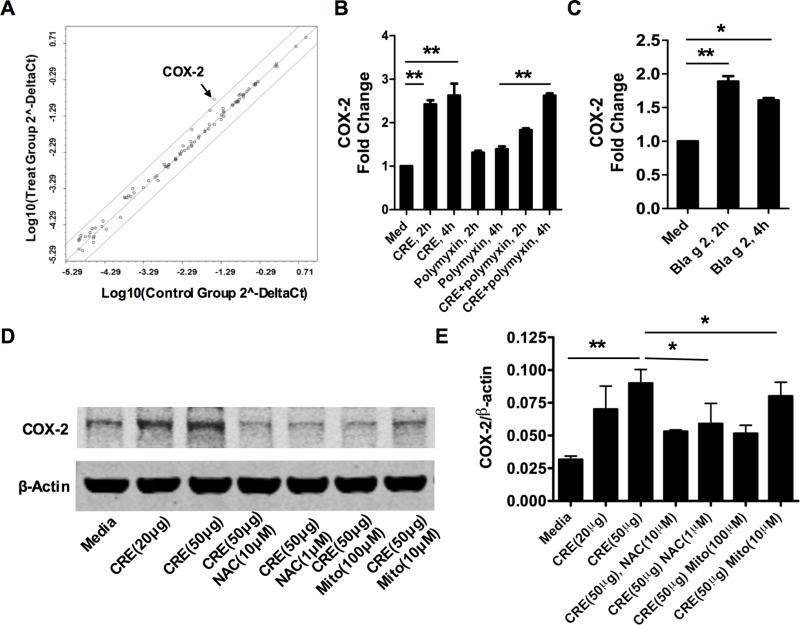
Identification of genes related to oxidative stress in cockroach allergen-treated epithelial cells
To identify genes that are related to cockroach allergen-induced oxidative stress, we performed PCR array analysis in cockroach allergen-treated ALI-cultured human airway epithelial cells using the Human Oxidative Stress RT2 Profiler PCR Array, which includes a total of 84 genes related to oxidative stress. Human PBECs from an ALI culture system, were treated with CRE for 2h, 4h, and 24h, respectively, and total RNA was extracted for RT2 Profiler™ PCR array analysis. We found that COX-2 was the only gene significantly up-regulated among all tested genes when 2-fold cut-off was applied at 2h (Fig. 2A) and 4h (Supplementary Fig. 2A). To determine whether LPS in CRE contributes to the increased COX-2 level, CRE was pre-treated with polymyxin to neutralize or absorb LPS and then used to treat the ALI-cultured human airway epithelial cells. No difference was noted for CRE-induced COX-2 expression in these airway epithelial cells with or without polymyxin pretreatment (Fig. 2B). The increased COX-2 expression was further observed in these airway epithelial cells after exposure to natural purified cockroach allergen Bla g 2 by RT-PCR (Fig. 2C). Given that previous studies have shown that ROS can trigger COX-2 expression (24–26), we used NHBE cells that are considered appropriate for the mechanistic studies and detected COX-2 expression in CRE-treated NHBE cells in the presence or absence of NAC or MitoTEMPO by Western blot (Fig. 2D, E). Interestingly, a significant inhibition of CRE-induced COX-2 expression was observed for NAC and MitoTEMPO treatments. These results were also observed in CRE-treated A549 cells (Supplementary Fig. 2B, C), suggesting that COX-2 may be a major gene participating in cockroach-induced oxidative stress in airway epithelial cells.
FIGURE 2.
Identification of genes related to oxidative stress by the Human Oxidative Stress RT2 Profiler PCR Array. (A) PCR Arrays revealed up- and down-regulated genes in ALI cultured human airway epithelial cells treated with or without CRE (n=84). X-axis: Medium, Y-axis: CRE; Cut off: ≥ 2-fold change. (B) RT-PCR analysis of COX-2 expression in CRE-treated ALI cultured human airway epithelial cells in the presence or absence of polymyxin (n=3). (C) RT-PCR analysis of COX-2 expression in Bla g2-treated ALI cultured human airway epithelial cells (n=3). (D) Western blot analysis of COX-2 expression in CRE-treated NHBEs in the presence or absence of NAC or MitoTEMPO. (E) Quantitative data for COX-2 expression relative to expression of β-actin. NAC: N-acetyl cysteine, MT: Mito TEMPO. CRE: cockroach extract. Data are expressed as the mean ± SEM. *P<0.05, **P<0.01.
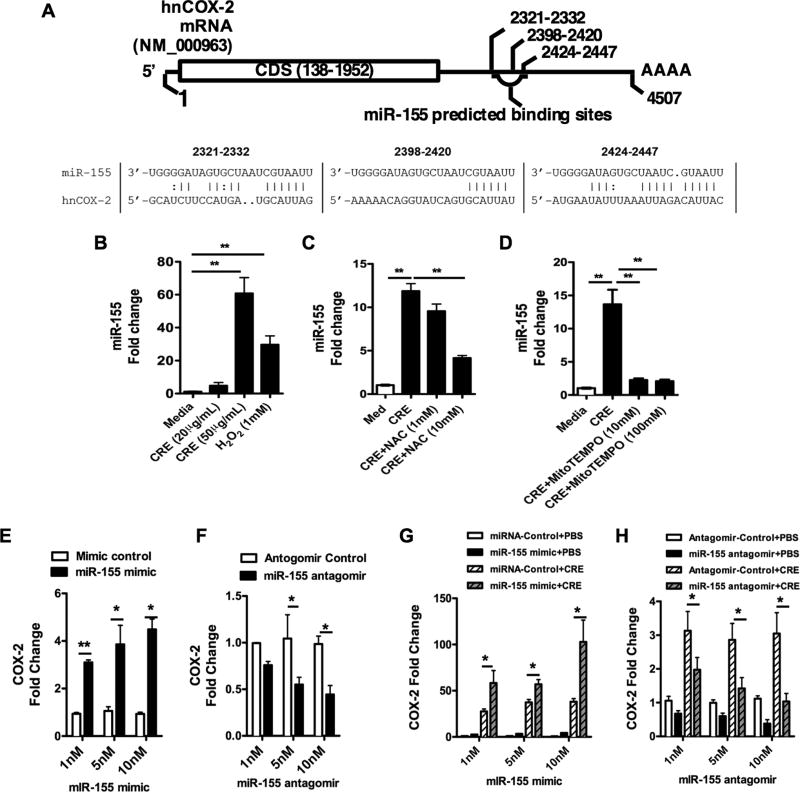
miR-155 up-regulates COX2 expression
To define the molecular mechanisms responsible for the CRE-induced COX-2 expression in airway epithelium, we tested the epigenetic regulation of COX-2 expression by miR-155. Recent studies have shown that miR-155 enhances COX-2 expression in human asthmatic airway smooth muscle cells(41). Our In silico analysis predicted that there are at least three potential miR-155 binding sites in the 3’-UTR of COX-2 (e.g., +2321–2332, +2398–2420, and +2424–2447 relative to the transcriptional start site) (Fig. 3A). To determine a potential interaction between miR-155 and COX-2 expression, we examined miR-155 expression in CRE-treated NHBEs. We found that miR-155 expression was increased in CRE-treated and COX-2 up-regulated NHBEs (Fig. 3B). Similarly, the increased expression of miR-155 was suppressed when either NAC (Fig. 3C) or MitoTEMPO (Fig. 3D) was used. Next, we investigated whether miR-155 regulates COX-2 expression in epithelial cells. Different doses of synthetic miR-155 mimic or negative control miRNA were transfected into NHBEs for 48 hours, and expression of COX-2 was determined by Western blot analysis. Compared to controls, cells transfected with the miR-155 mimic showed enhanced levels of COX-2 expression (Fig. 3E). In contrast, cells transfected with miR-155 antagomir showed reduced levels of COX-2 expression (Fig. 3F). Interestingly, the increased expression of COX-2 in miR-155 mimic transfected NHBEs was further enhanced after exposure to CRE (Fig. 3G). However, the CRE-induced expression of COX-2 was significantly inhibited in miR-155 antagomir transfected NHBEs compared to those transfected with antagomir control (Fig. 3H). Taken together, these data indicate that cockroach allergen can induce miR-155 production, which may promote COX-2 expression in airway epithelial cells.
FIGURE 3.
miR-155 up-regulates COX2 expression. (A) In silico predicted miR-155 binding sites in the 3’-UTR region of the human COX-2 gene. (B) RT-PCR analysis of miR-155 expression in CRE-treated NHBEs. (C–D) RT-PCR analysis of miR-155 expression in CRE-treated NHBEs in the presence or absence of NAC (C) or MitoTEMPO (D). (E–F) RT-PCR analysis of COX-2 expression in miR-155 mimic (E) and antagomir (F)-transfected NHBEs). (G–H) Expression of COX-2 in CRE or PBS treated miR-155 mimic (G) and antagomir (H)-transfected NHBEs. Data are representative of 3 independent experiments (n=3 per condition). Data represent mean ± SEM. *P<0.05, **P<0.01.
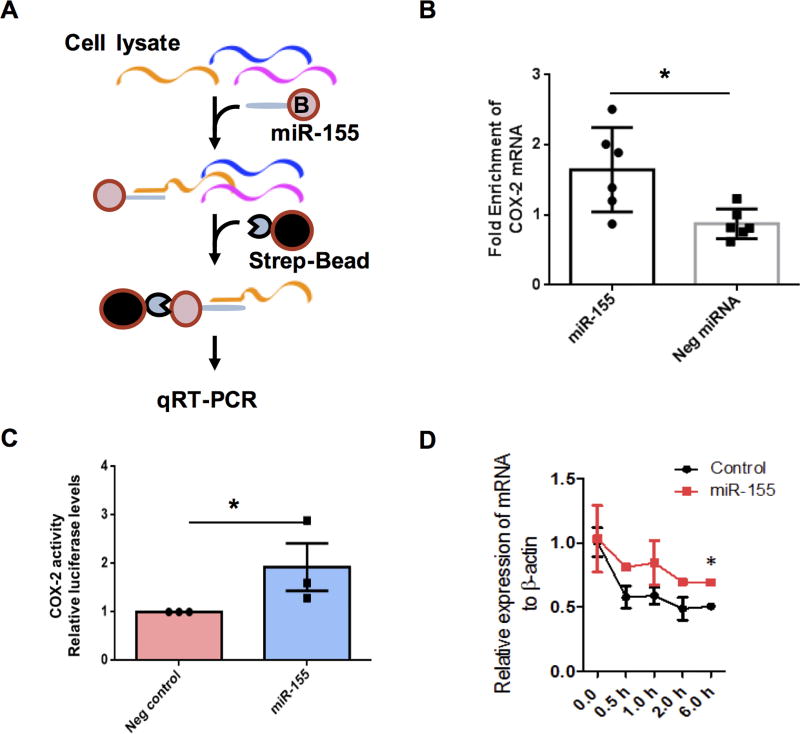
miR-155 binds COX-2 mRNA and up-regulates COX-2 luciferase activity and mRNA stability
To determine whether miR-155 is able to directly bind COX-2 mRNA and regulate its function, we developed a miRNA-mRNA pulldown assay to identify binding partners of miRNA, as outlined in Fig. 4 A. Using this method, COX-2 mRNA was identified in isolated miR-155-mRNA complexes from A549 cells (Fig. 4B), suggesting that there is direct binding between miR-155 and COX-2 in these epithelial cells. We next examined the regulation of miR-155 on COX-2 activity by luciferase reporter assay (59). Luciferase reporter constructs were created by cloning the 3’UTR of COX-2 with miR-155 predicted binding sites into the pmir-GLO Firefly luciferase plasmid (pmir-GLO-3’UTR-COX-2). The construct alone without the putative target was used as a negative control. A549 cells were transfected with miR-155 mimic for 24 h, with reporter plasmids for another 24 hs, and the relative luciferase activity was then detected. Compared to those transfected with negative control vector, cells transfected with the miR-155 mimic showed increased luciferase activity (Fig. 4C). In addition, we analyzed whether miR-155 affects COX-2 mRNA stability. A549 cells were transfected with miR-155 mimic or negative control for 48 hours, followed by actinomycin D treatment, and COX-2 mRNA levels were analyzed at various time points by RT-PCR. We observed that COX-2 mRNA was more stable in cells expressing the miR-155 mimic compared to those with the miRNA control (Fig. 4D), demonstrating that miR-155 could affect COX-2 mRNA stability.
FIGURE 4.
miR-155 binds COX-2 mRNA and up-regulates COX-2 luciferase activity and mRNA stability. (A) Schematic of technology developed to identify miRNA-mRNA interaction. (B) Enrichment of COX-2 mRNA in isolated miR-155-mRNA complexes from A549 cells. (C) Regulation by miR-155 of COX-2 activity by the luciferase reporter assay. Luciferase reporter constructs were created by cloning the 3’UTR of COX-2 with miR-155 predicted binding sites into the pmir-GLO Firefly luciferase plasmid. The construct alone with no putative target was used as a negative control. (D) Regulation by miR-155 of COX-2 miRNA stability in A549 cells (n=3). A549 cells were treated with 10 nM miR-155 mimic for 48 hours, followed by treatment with actinomycin D (5 µg/mL). Relative levels of COX-2 mRNA were determined using qRT-PCR. Data are expressed as the mean ± SEM. *P<0.05, **P<0.01.
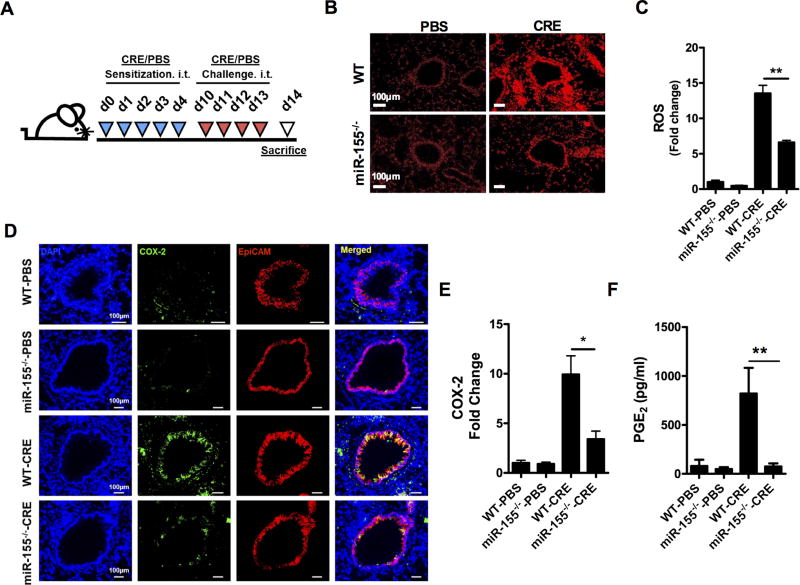
miR-155 regulates COX2 expression and Th2-associated lung inflammation
Subsequently, we asked whether miR-155 plays a role in the regulation of COX-2 in an allergen-induced mouse model of asthma. We used WT and miR-155−/− mice to develop a CRE-induced mouse model of asthma (Fig. 5A). We tested whether cockroach allergen can induce ROS production in the mouse model using the ROS fluorescent indicator DHE (Fig. 5B). Increased levels of ROS were noted in CRE-sensitized and challenged WT mice compared to PBS-treated controls (Fig. 5C). Interestingly, the increased ROS were significantly reduced in miR-155−/− mice. Furthermore, COX-2 expression was also detected in airway epithelial cells by co-staining for COX-2 and EpCAM, a marker for epithelial cells (Fig. 5D). Similar to ROS, lung sections from CRE-treated mice showed significantly increased expression of COX-2 in airway epithelial cells compared to those treated with PBS (Fig. 5E). Compared to WT mice, lung tissues from miR-155−/− mice showed much lower expression of COX-2. Reduced expression of miR-155 and COX-2 was also observed in lung tissues of PBS or CRE-treated miR-155−/− mice when compared to WT mice (Supplementary Figure 3). Additionally, the levels of PGE2 in BALFs mirrored those of COX-2 expression in those mice (Fig. 5F). miR-155−/− mice displayed much lower levels of PGE2 compared to CRE-treated WT mice when these mice were treated with CRE.
FIGURE 5.
miR-155 regulates epithelial COX2 expression levels in a mouse model of asthma. (A)Experimental model of cockroach allergen-induced asthma. (B) Representative images of dihydroethidium-stained (DHE-stained) airways of PBS- or CRE-challenged WT and miR-155−/− mice. Scale bar: 100 µm. (C) Quantitative data for ROS expression. (D) Co-localization of COX-2 (green) and EpCAM (red) in the lung sections of WT and miR-155−/− mice by immunofluorescence staining. Nuclei were stained with DAPI (blue). Scale bar: 100 µm. (E) Quantitative data for COX-2 expression. (F) Levels of PGE2 in BALFs of PBS- or CRE-treated WT and miR-155−/− mice. Quantification of gene expression in lung tissues was performed with ImageJ v1.50e. n=9–12 mice/group pooled from two independent experiments. Data represent the mean ± SEM. *P<0.05, **P<0.01.
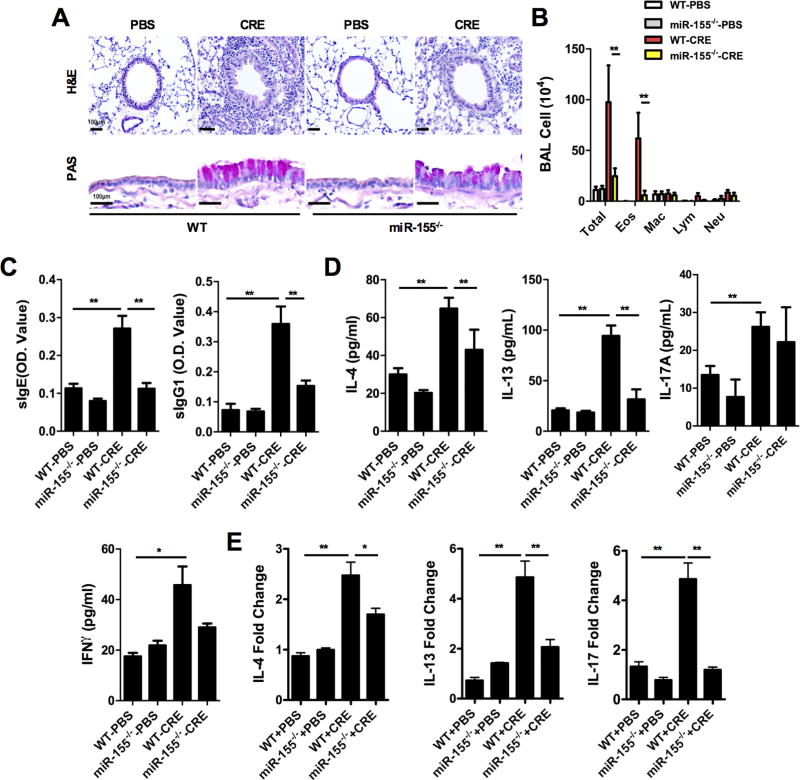
miR-155 regulates Th2/Th17-associated lung inflammation
Next, we assessed whether miR-155 regulates airway inflammation. We found that CRE-treated miR-155−/− mice displayed decreased recruitment of inflammatory cells to the lungs, with dense peri-bronchial infiltrates and goblet cell hyperplasia on histological examination (Fig. 6A, H&E and PAS) compared to WT mice. CRE-treated miR-155−/− mice showed reduced numbers of total inflammatory cells (Fig. 6B), specifically eosinophils in the BAL fluids. These CRE sensitized and challenged miR-155−/− mice also produced lower serum titers of cockroach allergen-specific IgE and IgG1 (Fig. 6C). Furthermore, compared to WT mice, BAL fluids from these miR-155−/− mice showed lower levels of IL-4 and IL-13 (Fig. 6D). No differences were observed for IFN-gamma, and IL-17A between CRE-treated WT and miR-155−/− mice. The levels of Th2/Th17 cytokines were further examined in lung tissues by RT-PCR, we found a reduced expression not only for IL-4 and IL-13, but also for IL-17 in CRE-treated miR-155−/− mice (Fig. 6E). Collectively, these results suggest that miR-155 may act to exacerbate Th2-associated lung inflammation through the up-regulation of COX-2 expression.
FIGURE 6.
miR-155 regulates lung inflammation in a mouse model of asthma. (A) Paraffin tissue sections of lungs from PBS- or CRE-challenged WT and miR-155−/− mice were stained with H&E (upper panel) and Periodic Acid-Schiff (PAS, lower panel). Scale bar: 100 µm. (B) Mouse BALF total and differential cell counts. (C) Serum levels of cockroach allergen-specific IgE and IgG1. (D)Levels of cytokines in BALFs. (E) RT-PCR analysis of Th1, Th2, and Th17 cytokines in the lung tissues. n=9–12 mice/group pooled from two independent experiments. Data represent the mean ± SEM. *P<0.05, **P<0.01.
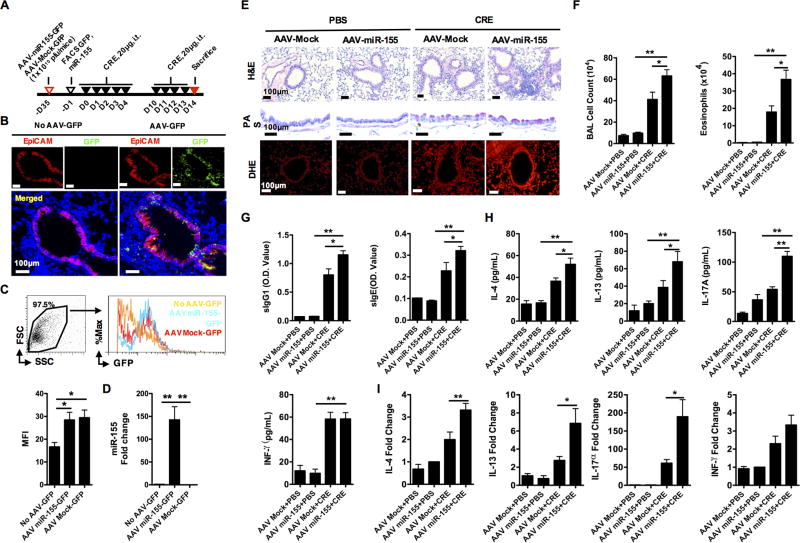
miR-155 exacerbates cockroach allergen-induced lung inflammation
To further determine whether miR-155 can directly promote cockroach allergen-induced inflammation, we generated an AAV vector expressing miR-155 (AAV-CMV-miR-511-3p-eGFP) and infected miR-155−/− mice according to the experimental approach in Fig. 7A. The AAV infection in these transfected mice, particularly airway epithelial cells, was confirmed on day 35 post-infection by co-imunostaining GFP with EpCaM (Fig. 7B) and flow cytometry analysis (Fig. 7C). Over-expression of miR-155 was confirmed in lung tissues of AAV-miR-155-GFP infected mice compared to those infected with AAV-Mock-GFP or un-infected (Fig. 7D). Those AAV infected mice were then used for generating cockroach allergen-induced mouse model of asthma following the protocol illustrated in Fig. 7A. As expected, CRE-triggered peribronchial inflammation (H&E), goblet cell hyperplasia (PAS), and ROS generation was exacerbated in the AAV-miR-155-infected mice compared to those AAV mock-infected controls (Fig. 7E). Similar pattern was also observed for COX-2 expression by immunostaining (Supplementary Figure 4). Furthermore, BAL fluids from AAV-miR-155-infected mice displayed an increased number of total inflammatory cells with a prominent increase in eosinophils (Fig. 7F). Serum from those mice had higher levels of CRE-specific IgE and IgG1 (Fig. 7G). BAL fluids from CRE-treated AAV-miR-155-infected mice had higher levels of IL-4, IL-13, IL-17A, but no changes for IFN-γ (Fig. 7H). Increased Th2/Th17 cytokine expression was also confirmed in the lung tissues by RT-PCR (Fig. 7I). Collectively, the results suggest that miR-155 may promote cockroach allergen induced lung allergic inflammation.
FIGURE 7.
miR-155−/− mice infected with AAV-miR-155 reversed the decreased lung inflammation in cockroach allergen-induced mouse model. (A) Experimental setup for mice infected with AAV-miR-155-GFP or AAV-Mock-GFP and subsequent mouse model of asthma. (B) Detection of GFP (green) in airway epithelial cells (red) of AAV-GFP infected or non-infected mice by immunostaining. Nuclei were stained with 6’-diamidino-2-phenylindole (DAPI, blue). Scale bar: 100 µm. (C) Detection of AAV-GFP in lung tissue cells of AAV-GFP infected or non-infected mice by flow cytometry. (D) RT-PCR analysis of miR-155 expression in lung tissues of AAV-infected or non-infected mice. (E) Paraffin tissue sections of lung tissues from PBS- or CRE-challenged AAV-Mock or AAV-miR-155 infected miR-155−/− mice were stained with H&E (upper panel), Periodic Acid-Schiff (PAS, middle panel), and DHE (lower panel). Scale bar: 100 µm. (F) Mouse BALF total and eosinophil cell counts. (G) Serum levels of cockroach allergen-specific IgE and IgG1. (H) Levels of cytokines in BALFs. (I) RT-PCR analysis of Th1, Th2, and Th17 cytokines in the lung tissues. n=6–10 mice/group pooled from two independent experiments. Data are expressed as the mean ± SEM. *P<0.05, **P<0.01.
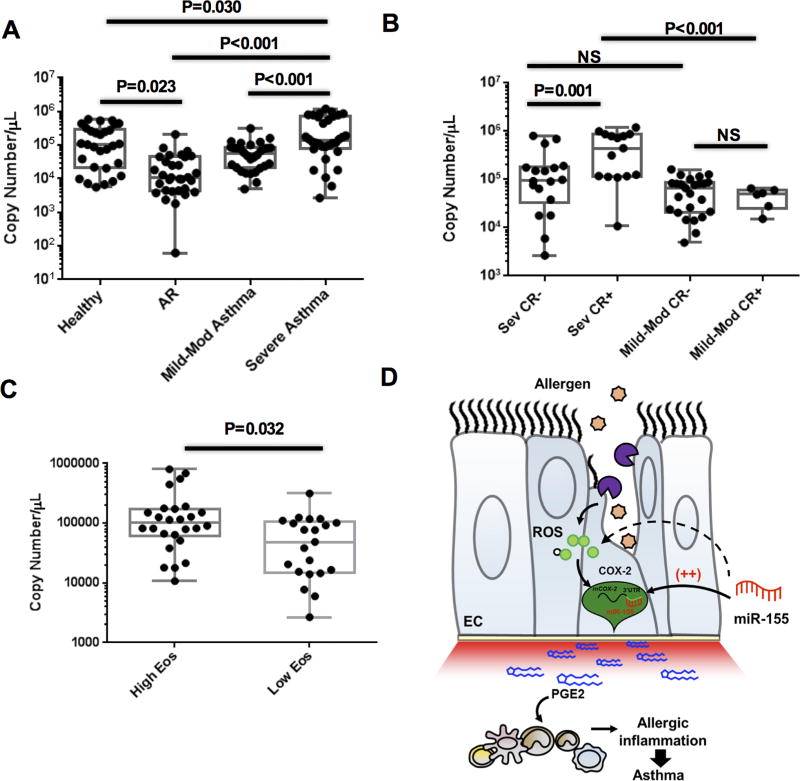
Elevated serum levels of miR-155 in asthmatic patients
To determine whether miR-155 is associated with human allergic asthma, we measured the expression of miR-155 in the plasma of human asthmatics and non-asthmatic controls. Detailed characteristics of the study subjects are presented in Table 1. The cohort of subjects included non-allergic, non-asthmatic subjects (n=22), non-asthmatic subjects with allergic rhinitis (n=25; n=8 cockroach allergic), and asthmatic subjects (n=62). The asthmatic subjects consisted of n=29 mild-moderate asthmatics (n=6 cockroach allergic) and n=33 severe asthmatics (n=13 cockroach allergic). The levels of plasma miR-155 were lower in patients with allergic rhinitis compared to the non-asthmatic subjects, consistent with our previous observation (61) (Fig. 8A). Interestingly, when comparing plasma miR-155 levels in asthmatics stratified by severity, levels were highest in severe asthmatics, lower in mild-to-moderate asthmatics, and lowest in allergic rhinitis. We next asked whether cockroach allergy status was associated with higher levels of plasma miR-155 in asthma. In severe asthmatics, the level of miR-155 was higher in subjects with cockroach allergy vs. those without (Fig. 8B). The levels were not different in cockroach allergic vs. non-allergic mild-moderate asthmatics. In addition, the level was higher in cockroach allergic, severe asthmatics compared to cockroach allergic, mild-moderate asthmatics. Together, these data suggest that cockroach sensitivity and asthma severity may affect plasma miR-155 levels. We next sought determine whether miR-155 levels were associated with blood eosinophil levels as a marker of Type 2 inflammation. We found higher levels of plasma miR-155 in these asthmatics with high eosinophils based on the median value in our population (≥200 cells/µl) when compared with those with low eosinophils (<200 cells/µl) (Fig. 8C).
Table 1.
Demographic and respiratory health characteristics of the study population
| Characteristics | Non-asthmatic (n=27) |
Asthmatic (n=32) |
p-value |
|---|---|---|---|
| Age, mean (SD) | 45.5 (15.2) | 43.9 (14.6) | 0.917 |
| Gender, male/female | 8/19 | 13/19 | 0.424 |
| BMI, mean (SD) | 28.7(6.6) | 28.4 (5.9) | 0.869 |
| Allergic rhinitis, n (%) | 17 (63) | 26 (81) | 0.147 |
| Asthma duration (Y), mean (SD) | N/A | 17.3 (11.1) | N/A |
| Blood eos (cells/µl), mean (SD) | Not done | 216.8 (150.1) | N/A |
| Total IgE (kU/L) | Not done | 248.3 (264,3) | N/A |
| FVC (L), mean (SD) | 3.77(1.65) | 3.72 (1.17) | 0.899 |
| FVC%, mean (SD) | 98.9(20.9) | 89.4 (17.4) | 0.083 |
| FEV1 (L), mean (SD) | 3.02 (1.54) | 2.66 (1.11) | 0.336 |
| FEV1%, mean (SD) | 92.9 (0.2) | 77.2 (23.5) | 0.021 |
| FEV1/FVC ratio | 0.76 (0.1) | 0.68 (0.14) | 0.045 |
| FEV1% change after BD, mean (SD) | Not done | 14.8 (13.2) | N/A |
| ACQ score, mean (SD) | Not done | 0.99 (0.58) | N/A |
FIGURE 8.
Plasma levels of miR-155. (A)Plasma levels of miR-155 were detected in in healthy (n=30), allergic rhinitis (AR, n=31), Mild-Mod asthmatic (n=29), and severe asthmatic (n=33) human patients by real-time PCR analysis. (B) Plasma levels of miR-155 were measured in asthmatics with mild-moderate asthma (n=29) or severe asthma (n=33), with or without cockroach allergy (CR- or CR+, respectively). (C) Plasma miR-155 in asthmatics with high or low eosinophils based on the median value in our population (≥200 cells/µl). (D) Proposed model for cockroach allergen-induced ROS generation and miR-155 secretion, which up-regulates COX-2 expression and subsequent Th2/Th17-associated allergic inflammation in allergic asthma.
DISCUSSION
This work is part of our overall mechanistic studies on cockroach allergen-induced allergic inflammation, with a specific focus on cockroach allergen-induced ROS generation and ROS-associated gene identification. ROS have been shown to be crucial in pollen (16) and HDM (60)-induced allergic sensitization and asthma. In particular, ROS induced by HDM cause oxidative DNA damage and asthma-associated pathophysiology (14, 60). Recent studies have suggested that ROS in epithelial cells are a critical mediator of IL-33-dependent activation of innate airway type 2 immune responses to common airborne allergens(20) (61). Similar findings have also been found for cockroach allergen through the activation of proteinase-activated receptor 2 (PAR-2), leading to the up-regulation of the DUOX-2/ROS pathway in airway epithelial cells (62). Furthermore, we have recently reported that cockroach allergen induces ROS production and oxidative activation of calmodulin-dependent protein kinase II (CaMKII) in mast cells, which leads to the exacerbation of lung inflammation (22). Interestingly, the increased ox-CaMKII in the airway epithelium of asthmatic patients has been linked to the severity of asthma (63). Observations made in this study demonstrated that cockroach allergen can induce ROS generation in airway epithelial cells. While the intracellular sources of the ROS are not clear, mitochondria are known to be a major source of ROS that are induced by external stimuli (64–66), and are associated with allergic inflammation in OVA-challenged mice (67). Indeed, we found that cockroach allergen-induced ROS in airway epithelial cells were significantly blocked by the mitochondria-specific antioxidant, MitoTEMPO. Furthermore, mitochondrial ROS was significantly increased in these cockroach allergen-treated airway epithelial cells. Thus, our studies provided further evidence that cockroach allergen can induce ROS production, particularly mitochondrial-derived ROS, which may serve as a critical mediator in regulating allergen-induced airway inflammation and asthma.
In this study, we have made a novel finding that COX-2 was the most significantly up-regulated gene related to cockroach allergen-induced oxidative stress with the use of the Human Oxidative Stress RT2 Profiler PCR Array. A total of 84 genes related to oxidative stress are represented on this array, including glutathione peroxidases (GPx), peroxiredoxins (TPx), other peroxidases, and genes associated with ROS metabolism. The array made it possible to analyze the expression of a focused panel of genes related to oxidative stress. Another strength was the use of human airway epithelial cells from an ALI culture system. Epithelial cells in the ALI system can fully differentiate into mature epithelial cells, as manifested by the formation of greater levels of mucociliary epithelium (51, 52), and faithfully mimic the in vivo physiological setting. Intriguingly, COX-2 was differential expression in the ALI-cultured human airway epithelial cells after exposure to cockroach allergen. To exclude the possibility that CRE-induced COX-2 expression may have been due to endotoxin present in the CRE, we used polymyxin to neutralize the effect of LPS present as contaminant on CRE. We found that airway epithelial cells treated with polymyxin-treated or untreated CRE showed similar results, suggesting that increased expression of COX-2 is due to cockroach allergen, but not LPS.
Furthermore, previous observations have suggested that ROS could induce COX-2 expression (23, 24) and that antioxidants could suppress COX-2 expression (69), Indeed, we found that cockroach allergen-induced COX-2 expression was significantly inhibited by antioxidants. Furthermore, given the increasingly recognized role of COX-2 in allergic inflammation in animal models and in humans with asthma (29–33, 38), it is tempting to speculate that COX-2 could be an important oxidative stress-associated gene might contribute to allergen-induced allergic inflammation. Thus, targeting of the regulation of COX-2 may yield therapeutic approaches for the treatment of allergic inflammation and asthma.
Our central finding is the epigenetic regulation of COX-2 by miR-155. miRNAs are small, non-coding RNAs that are important regulators of protein expression and cellular functions (68). Several miRNAs have been suggested to target COX-2 and modulate its expression (40–47). Of these, miR-155 has been shown to enhance COX-2 expression in human asthmatic airway smooth muscle cells (41). However, no evidence was provided to demonstrate a direct interaction between miR-155 and COX-2. Our studies provide evidence for a direct link between cockroach allergen-induced COX-2 expression and miR-155. We first showed that miR-155 regulates COX-2 expression in either miR-155 mimic or miR-155 antagomir-transfected NHBEs. NHBE cells with miR-155 mimic showed increased expression of COX-2, but with miR-155 antagomir displayed a reduced expression of COX-2. We then analyzed the binding of miR-155 to COX-2 using technology we developed to identify binding partners of miRNA by mixing biotinylated miRNA with cell lysates (56). We observed a significantly higher amount of COX-2 mRNA in isolated miR-155-mRNA complexes than in miR-control-mRNA complexes. Furthermore, we investigated whether miR-155 could regulate COX-2 activity using a luciferase reporter assay with a reporter plasmid containing the 3’UTR of COX-2 with miR-155 predicted binding sites. As expected, cells transfected with the reporter plasmid containing miR-155 binding sites showed significantly increased luciferase activity compared to those without binding sites. Lastly, we investigated the role of miR-155 in regulating COX-2 miRNA stability. While we recognize that miRNAs are generally considered to negatively regulate target mRNA, more published studies have now increasingly indicated that miRNA oscillates between suppression and stimulation in response to specific cellular conditions, sequences, and cofactors (71). Given that regulation of miRNA stability is an important regulatory mechanism for controlling gene expression, we specifically analyzed the effect of miR-155 on COX-2 miRNA stability. We found that COX-2 mRNA was much more stable in cells transfected with miR-155 compared to those transfected with a control mimic. These findings provide a novel epigenetic mechanism by which miR-155 regulates COX-2 activity and mRNA stability.
Most importantly, COX-2 regulation by miR-155 was also observed in our cockroach allergen-induced mouse model of asthma. We observed increased expression of ROS and COX-2 in the lung tissues, particularly airway epithelia of cockroach allergen-sensitized and challenged mice. Intriguingly, these increased epithelial ROS and COX-2 were not observed in miR-155−/− mice. These results further supported our in vitro findings that miR-155 regulates COX-2 expression. Furthermore, we observed an increased expression of ROS in CRE-challenged WT mice, but the increased ROS were significantly reduced in miR-155−/−mice, suggesting that miR-155 may regulate ROS generation. Although detailed mechanisms are unclear, it is possible that miR-155 may not only directly target on COX-2, but also can directly induce ROS production to promote ROS-induced lung inflammation. Thus, we found that ROS production and lung inflammation were significantly reduced in miR-155−/− mice, raising the possibility that miR-155 might be an important player connecting ROS production and inflammation. However, it is also likely that the reduced ROS may not be directly regulated by miR-155, but a feed forward circuit in the ROS generation. For example, the deletion of miR-155 may lead to a reduction of local inflammatory processes that leads to a secondary reduction of ROS generation.
It is well-documented that up-regulated miR-155 is associated with the development of allergic asthma (47, 72–74). Of these, Zhang et al reported that miR-155 was the most up-regulated miRNAs in the lungs of allergen-challenged mice compared with control mice (73). Furthermore, Malmhall et al has recently provided evidence that miR-155 is differentially expressed ex vivo in airways of allergic asthmatics compared to healthy controls, and suggested that miR-155 may participate in the local immune response in allergic asthma (74). Recent studies have suggested that miR-155 is a critical regulator of type 2 innate lymphoid cells (ILC2) (48) and is a novel target in allergic asthma (75). In addition, previous studies have demonstrated an increased miR-155 expression in activated T cells and that miR-155 over-expression increases the numbers of activated CD4+ T cells with increased Th2 and Th17-derived cytokines, suggesting that miR-155 may regulate Th2/Th17-associated inflammation. In accordance with previous findings, we found that miR-155 is up-regulated in the lung tissues of cockroach allergen-challenged mice, and miR-155 is critical in the cockroach allergen-induced Th2/Th17 cytokine production and lung inflammation. Taken together, our studies suggest a possible mechanism by which miR-155 regulates Th2/Th17 differentiation and activation, which may be mediated through the functional axis of COX-2-PGE2.
Finally, we showed the direct relevance of miR-155 to human asthma. We have previously demonstrated differential expression of plasma miR-155 in human subjects with asthma, allergic rhinitis, or neither (61). Building on these data, we recruited additional subjects, including those with severe asthma and cockroach allergy. We found that patients with severe asthma had higher levels of miR-155 when compared with mild-to-moderate asthmatics, allergic rhinitis, and non-asthmatic controls, suggesting that miR-155 may contribute to the severity of inflammation. It is interesting to note that plasma miR-155 levels were lower in subjects with allergic rhinitis compared to all other groups, including healthy controls. The underlying reason is not clear, but anti-inflammatory miRNA, such as miR-146a, are known to be up-regulated by inflammatory stimuli as a potential feedback mechanism to limit inflammation (75). Along these lines, there is emerging evidence that miR-155 expression can also be down-regulated by a number of stimuli (76–77). It is possible that mechanisms exist to limit miR-155 expression in allergic rhinitis, but that these mechanisms are overwhelmed as the extent and severity of inflammation increases, as could be the case in severe asthma. Further work will be needed to understand the mechanisms that govern miR-155 expression in allergic rhinitis and asthma.
As cockroach allergen is an important driver of allergic inflammation in asthma, we analyzed levels of plasma miR-155 in asthmatics with and without cockroach allergy. In severe asthmatics, miR-155 levels were higher in cockroach-allergic subjects compared to those without cockroach allergy. These data are in agreement with our observations in the mouse model, and support the possibility that miR-155 may be a driver of cockroach-induced allergic airway inflammation. However, there are several limitation for this study. For example, although an increased plasma miR-155 was found in severe asthmatics, this may not directly reflect the changes in the local environment in the airway and lung tissues. Furthermore, we hypothesize that exposure to cockroach allergen, either long duration or high exposure, played a role in inducing secretion of miR-155. Unfortunately, we do not yet have data on exposure to cockroach for these subjects, to know whether exposure level relates to miR-155 levels. In addition, we do not know whether there is an intrinsic defect in cells that makes them susceptible to overexpress miR-155, and this will be a topic of future study.
In summary, our findings provide evidence that cockroach allergen exposure can induce oxidative stress in airway epithelia and subsequent allergic inflammation and asthma. Specifically, we identified COX-2 as a pivotal gene related to oxidative stress in airway epithelial cells and suggested a novel mechanism by which cockroach allergen-enhanced expression of COX-2 is dependent upon miR-155. We speculate that inhibition of miR-155 may block ROS-induced COX-2 expression and subsequent COX-2-mediated allergic inflammation and asthma (Fig. 8D). More importantly, these studies allow us to solidify the ground work for future in-depth studies, with a focus on the regulation of COX-2 function by ROS and miR-155 via its receptors (e.g., EP2, EP4) and the mechanisms underlying COX-2-mediated epithelial cell activation and airway inflammation. Furthermore, it would be essential to explore the cellular sources of miR-155, which may serve as a critical mediator for cell-cell interactions. Taken together, our findings provide supporting evidence that COX-2 is a major gene related to cockroach-induced oxidative stress and further highlight a role for miR-155 in the pathogenesis of asthma through regulating the ROS-COX2 axis.
Supplementary Material
Acknowledgments
We gratefully acknowledge the assistance of Beverly Plunkett regarding the Air-Liquid Interface cultures of human airway epithelial cells. Additionally, we thank Dr. Allen Myers at the Johns Hopkins Bayview Histology Core Laboratory for providing isolated epithelial cells from central airways of human subjects. We also thank Dr. Neeraj Sharma, Johns Hopkins University, for his kind gift of NHBEs.
This work was supported by grants from the US National Institutes of Health (NIH) (RO1ES021739, R21 AI109062, R21 AI121768) and the National Science Foundation of China (NSFC) 81628001(to P Gao); the Doris Duke Charitable Foundation Clinician Scientist Development Award (to F Ishmael); and NSFC 81402840 and the National Science Foundation of Jiangsu Province (To L Qiu).
Abbreviations
- CRE
Cockroach extract
- HDM
House dust mite
- ROS
Reactive oxygen species
- NHBE
Humanbronchial epithelial cell
- COX-2
Cyclooxygenase-2
- PGE2
Prostaglandin E2
- miRNA-155
microRNA-155
- BALF
Bronchoalveolar lavage fluid
- AAV
Adeno-associated virus
Footnotes
Author contributions
L.Q., Y. Z. D.D., X.K., S. Z., K.L., C. H. S.K., Y.Z. performed experiments and analyzed data. L.Q. and D.D. wrote the manuscript. F.I. and P.G designed and supervised the study, and wrote the manuscript.
References
- 1.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, Mitchell H, McNiff-Mortimer K, Lynn H, Ownby D, Malveaux F. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. The New England journal of medicine. 1997;336:1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 2.Matsui EC, Wood RA, Rand C, Kanchanaraksa S, Swartz L, Curtin-Brosnan J, Eggleston PA. Cockroach allergen exposure and sensitization in suburban middle-class children with asthma. J Allergy Clin Immunol. 2003;112:87–92. doi: 10.1067/mai.2003.1588. [DOI] [PubMed] [Google Scholar]
- 3.Olmedo O, Goldstein IF, Acosta L, Divjan A, Rundle AG, Chew GL, Mellins RB, Hoepner L, Andrews H, Lopez-Pintado S, Quinn JW, Perera FP, Miller RL, Jacobson JS, Perzanowski MS. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat, and dog allergens in New York City. The Journal of allergy and clinical immunology. 2011;128:284–292. e287. doi: 10.1016/j.jaci.2011.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gruchalla RS, Pongracic J, Plaut M, Evans R, 3rd, Visness CM, Walter M, Crain EF, Kattan M, Morgan WJ, Steinbach S, Stout J, Malindzak G, Smartt E, Mitchell H. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. The Journal of allergy and clinical immunology. 2005;115:478–485. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Comhair SA, Bhathena PR, Dweik RA, Kavuru M, Erzurum SC. Rapid loss of superoxide dismutase activity during antigen-induced asthmatic response. Lancet. 2000;355:624. doi: 10.1016/S0140-6736(99)04736-4. [DOI] [PubMed] [Google Scholar]
- 6.Comhair SA, Bhathena PR, Farver C, Thunnissen FB, Erzurum SC. Extracellular glutathione peroxidase induction in asthmatic lungs: evidence for redox regulation of expression in human airway epithelial cells. FASEB J. 2001;15:70–78. doi: 10.1096/fj.00-0085com. [DOI] [PubMed] [Google Scholar]
- 7.Barnes PJ. Reactive oxygen species and airway inflammation. Free Radic Biol Med. 1990;9:235–243. doi: 10.1016/0891-5849(90)90034-g. [DOI] [PubMed] [Google Scholar]
- 8.Qu J, Li Y, Zhong W, Gao P, Hu C. Recent developments in the role of reactive oxygen species in allergic asthma. Journal of thoracic disease. 2017;9:E32–E43. doi: 10.21037/jtd.2017.01.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nadeem A, Siddiqui N, Alharbi NO, Alharbi MM. Airway and systemic oxidant-antioxidant dysregulation in asthma: a possible scenario of oxidants spill over from lung into blood. Pulm Pharmacol Ther. 2014;29:31–40. doi: 10.1016/j.pupt.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Nadeem A, Masood A, Siddiqui N. Oxidant--antioxidant imbalance in asthma: scientific evidence, epidemiological data and possible therapeutic options. Ther Adv Respir Dis. 2008;2:215–235. doi: 10.1177/1753465808094971. [DOI] [PubMed] [Google Scholar]
- 11.Comhair SA, Erzurum SC. Redox control of asthma: molecular mechanisms and therapeutic opportunities. Antioxid Redox Signal. 2010;12:93–124. doi: 10.1089/ars.2008.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HJ, Ryu JH, Kim CH, Lim JW, Moon UY, Lee GH, Lee JG, Baek SJ, Yoon JH. Epicatechin gallate suppresses oxidative stress-induced MUC5AC overexpression by interaction with epidermal growth factor receptor. Am J Respir Cell Mol Biol. 2010;43:349–357. doi: 10.1165/rcmb.2009-0205OC. [DOI] [PubMed] [Google Scholar]
- 13.Brussino L, Badiu I, Sciascia S, Bugiani M, Heffler E, Guida G, Malinovschi A, Bucca C, Rolla G. Oxidative stress and airway inflammation after allergen challenge evaluated by exhaled breath condensate analysis. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2010;40:1642–1647. doi: 10.1111/j.1365-2222.2010.03604.x. [DOI] [PubMed] [Google Scholar]
- 14.Bacsi A, Pan L, Ba X, Boldogh I. Pathophysiology of bronchoconstriction: role of oxidatively damaged DNA repair. Current opinion in allergy and clinical immunology. 2016;16:59–67. doi: 10.1097/ACI.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boldogh I, Bacsi A, Choudhury BK, Dharajiya N, Alam R, Hazra TK, Mitra S, Goldblum RM, Sur S. ROS generated by pollen NADPH oxidase provide a signal that augments antigen-induced allergic airway inflammation. The Journal of clinical investigation. 2005;115:2169–2179. doi: 10.1172/JCI24422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shalaby KH, Allard-Coutu A, O'Sullivan MJ, Nakada E, Qureshi ST, Day BJ, Martin JG. Inhaled birch pollen extract induces airway hyperresponsiveness via oxidative stress but independently of pollen-intrinsic NADPH oxidase activity, or the TLR4-TRIF pathway. J Immunol. 2013;191:922–933. doi: 10.4049/jimmunol.1103644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fukunaga M, Gon Y, Nunomura S, Inoue T, Yoshioka M, Hashimoto S, Ra C. Protease-mediated house dust mite allergen-induced reactive oxygen species production by neutrophils. International archives of allergy and immunology. 2011;155(Suppl 1):104–109. doi: 10.1159/000327492. [DOI] [PubMed] [Google Scholar]
- 18.Lin C-HH, Hong Y-CC, Kao S-HH. Aeroallergen Der p 2 induces apoptosis of bronchial epithelial BEAS-2B cells via activation of both intrinsic and extrinsic pathway. Cell & bioscience. 2015;5:71. doi: 10.1186/s13578-015-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Y, Bai C, Li K, Adler KB, Wang X. Role of airway epithelial cells in development of asthma and allergic rhinitis. Respiratory medicine. 2008;102:949–955. doi: 10.1016/j.rmed.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Uchida M, Anderson EL, Squillace DL, Patil N, Maniak PJ, Iijima K, Kita H, O'Grady SM. Oxidative stress serves as a key checkpoint for IL-33 release by airway epithelium. Allergy. 2017 doi: 10.1111/all.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu T, Zhou Y, Qiu L, Do DC, Zhao Y, Cui Z, Wang H, Liu X, Saradna A, Cao X, Wan M, Gao P. Aryl Hydrocarbon Receptor Protects Lungs from Cockroach Allergen-Induced Inflammation by Modulating Mesenchymal Stem Cells. Journal of immunology. 2015;195:5539–5550. doi: 10.4049/jimmunol.1501198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qu J, Do DC, Zhou Y, Luczak E, Mitzner W, Anderson ME, Gao P. Oxidized CaMKII promotes asthma through the activation of mast cells. JCI Insight. 2017;2:e90139. doi: 10.1172/jci.insight.90139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kale SL, Agrawal K, Gaur SN, Arora N. Cockroach protease allergen induces allergic airway inflammation via epithelial cell activation. Scientific reports. 2017;7:42341. doi: 10.1038/srep42341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barbieri SS, Eligini S, Brambilla M, Tremoli E, Colli S. Reactive oxygen species mediate cyclooxygenase-2 induction during monocyte to macrophage differentiation: critical role of NADPH oxidase. Cardiovascular research. 2003;60:187–197. doi: 10.1016/s0008-6363(03)00365-1. [DOI] [PubMed] [Google Scholar]
- 25.Onodera Y, Teramura T, Takehara T, Shigi K, Fukuda K. Reactive oxygen species induce Cox-2 expression via TAK1 activation in synovial fibroblast cells. FEBS Open Bio. 2015;5:492–501. doi: 10.1016/j.fob.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu Y-P, Y-B P, Peng B, Zhang Y-FF, Wang Y, Yu W-RR, Yao M, Fu X-JJ. Reactive Oxygen Species Mediated Prostaglandin E2 Contributes to Acute Response of Epithelial Injury. Oxidative medicine and cellular longevity. 2017;2017:4123854. doi: 10.1155/2017/4123854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Mari JF, Mifflin RC, Adegboyega PA, Saada JI, Powell DW. IL-1alpha-induced COX-2 expression in human intestinal myofibroblasts is dependent on a PKCzeta-ROS pathway. Gastroenterology. 2003;124:1855–1865. doi: 10.1016/s0016-5085(03)00399-8. [DOI] [PubMed] [Google Scholar]
- 28.Williams CS, Mann M, DuBois RN. The role of cyclooxygenases in inflammation, cancer, and development. Oncogene. 1999;18:7908–7916. doi: 10.1038/sj.onc.1203286. [DOI] [PubMed] [Google Scholar]
- 29.Herrerias A, Torres R, Serra M, Marco A, Pujols L, Picado C, de Mora F. Activity of the cyclooxygenase 2-prostaglandin-E prostanoid receptor pathway in mice exposed to house dust mite aeroallergens, and impact of exogenous prostaglandin E2. J Inflamm (Lond) 2009;6:30. doi: 10.1186/1476-9255-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sousa A, Pfister R, Christie PE, Lane SJ, Nasser SM, Schmitz-Schumann M, Lee TH. Enhanced expression of cyclo-oxygenase isoenzyme 2 (COX-2) in asthmatic airways and its cellular distribution in aspirin-sensitive asthma. Thorax. 1997;52:940–945. doi: 10.1136/thx.52.11.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rumzhum NN, Patel BS, Prabhala P, Gelissen IC, Oliver BG, Ammit AJ. IL-17A increases TNF-alpha-induced COX-2 protein stability and augments PGE2 secretion from airway smooth muscle cells: impact on beta2 -adrenergic receptor desensitization. Allergy. 2016;71:387–396. doi: 10.1111/all.12810. [DOI] [PubMed] [Google Scholar]
- 32.Deacon K, Knox AJ. Human airway smooth muscle cells secrete amphiregulin via bradykinin/COX-2/PGE2, inducing COX-2, CXCL8, and VEGF expression in airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2015;309:L237–249. doi: 10.1152/ajplung.00390.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Profita M, Sala A, Bonanno A, Riccobono L, Siena L, Melis MR, Di Giorgi R, Mirabella F, Gjomarkaj M, Bonsignore G, Vignola AM. Increased prostaglandin E2 concentrations and cyclooxygenase-2 expression in asthmatic subjects with sputum eosinophilia. J Allergy Clin Immunol. 2003;112:709–716. doi: 10.1016/s0091-6749(03)01889-x. [DOI] [PubMed] [Google Scholar]
- 34.Carey MA, Germolec DR, Bradbury JA, Gooch RA, Moorman MP, Flake GP, Langenbach R, Zeldin DC. Accentuated T helper type 2 airway response after allergen challenge in cyclooxygenase-1−/− but not cyclooxygenase-2−/− mice. American journal of respiratory and critical care medicine. 2003;167:1509–1515. doi: 10.1164/rccm.200211-1383OC. [DOI] [PubMed] [Google Scholar]
- 35.Li H, Edin ML, Bradbury AJ, Graves JP, DeGraff LM, Gruzdev A, Cheng J, Dackor RT, Wang P, Bortner CD, Garantziotis S, Jetten AM, Zeldin DC. Cyclooxygenase-2 inhibits T helper cell type 9 differentiation during allergic lung inflammation via down-regulation of IL-17RB. American journal of respiratory and critical care medicine. 2013;187:812–822. doi: 10.1164/rccm.201211-2073OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Church RJ, Jania LA, Koller BH. Prostaglandin E(2) produced by the lung augments the effector phase of allergic inflammation. J Immunol. 2012;188:4093–4102. doi: 10.4049/jimmunol.1101873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trebino CE, Stock JL, Gibbons CP, Naiman BM, Wachtmann TS, Umland JP, Pandher K, Lapointe JM, Saha S, Roach ML, Carter D, Thomas NA, Durtschi BA, McNeish JD, Hambor JE, Jakobsson PJ, Carty TJ, Perez JR, Audoly LP. Impaired inflammatory and pain responses in mice lacking an inducible prostaglandin E synthase. Proceedings of the National Academy of Sciences of the United States of America. 2003;100:9044–9049. doi: 10.1073/pnas.1332766100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao Y, Zhao C, Wang W, Jin R, Li Q, Ge Q, Guan Y, Zhang Y. Prostaglandins E2 signal mediated by receptor subtype EP2 promotes IgE production in vivo and contributes to asthma development. Scientific reports. 2016;6:20505. doi: 10.1038/srep20505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rebane A, Akdis CA. MicroRNAs: Essential players in the regulation of inflammation. J Allergy Clin Immunol. 2013;132:15–26. doi: 10.1016/j.jaci.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 40.Cornett AL, Lutz CS. Regulation of COX-2 expression by miR-146a in lung cancer cells. RNA. 2014;20:1419–1430. doi: 10.1261/rna.044149.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Comer BS, Camoretti-Mercado B, Kogut PC, Halayko AJ, Solway J, Gerthoffer WT. Cyclooxygenase-2 and microRNA-155 expression are elevated in asthmatic airway smooth muscle cells. Am J Respir Cell Mol Biol. 2015;52:438–447. doi: 10.1165/rcmb.2014-0129OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xia M, Duan ML, Tong JH, Xu JG. MiR-26b suppresses tumor cell proliferation, migration and invasion by directly targeting COX-2 in lung cancer. Eur Rev Med Pharmacol Sci. 2015;19:4728–4737. [PubMed] [Google Scholar]
- 43.Kwon Y, Kim Y, Eom S, Kim M, Park D, Kim H, Noh K, Lee H, Lee YS, Choe J, Kim YM, Jeoung D. MicroRNA-26a/-26b-COX-2-MIP-2 Loop Regulates Allergic Inflammation and Allergic Inflammation-promoted Enhanced Tumorigenic and Metastatic Potential of Cancer Cells. J Biol Chem. 2015;290:14245–14266. doi: 10.1074/jbc.M115.645580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu D, Wang D, Xu Z, Gao J, Liu M, Liu Y, Jiang M, Zheng D. Dysregulated expression of miR-101b and miR-26b lead to age-associated increase in LPS-induced COX-2 expression in murine macrophage. Age (Dordr) 2015;37:97. doi: 10.1007/s11357-015-9836-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen L, Wang X, Wang H, Li Y, Yan W, Han L, Zhang K, Zhang J, Wang Y, Feng Y, Pu P, Jiang T, Kang C, Jiang C. miR-137 is frequently down-regulated in glioblastoma and is a negative regulator of Cox-2. Eur J Cancer. 2012;48:3104–3111. doi: 10.1016/j.ejca.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 46.Zuo W, Wang ZZ, Xue J. Artesunate induces apoptosis of bladder cancer cells by miR-16 regulation of COX-2 expression. Int J Mol Sci. 2014;15:14298–14312. doi: 10.3390/ijms150814298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen P, Wang BL, Pan BS, Guo W. MiR-1297 regulates the growth, migration and invasion of colorectal cancer cells by targeting cyclo-oxygenase-2. Asian Pac J Cancer Prev. 2014;15:9185–9190. doi: 10.7314/apjcp.2014.15.21.9185. [DOI] [PubMed] [Google Scholar]
- 48.Plank MW, Maltby S, Tay HL, Stewart J, Eyers F, Hansbro PM, Foster PS. MicroRNA Expression Is Altered in an Ovalbumin-Induced Asthma Model and Targeting miR-155 with Antagomirs Reveals Cellular Specificity. PLoS One. 2015;10:e0144810. doi: 10.1371/journal.pone.0144810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sonkoly E, Janson P, Majuri ML, Savinko T, Fyhrquist N, Eidsmo L, Xu N, Meisgen F, Wei T, Bradley M, Stenvang J, Kauppinen S, Alenius H, Lauerma A, Homey B, Winqvist O, Stahle M, Pivarcsi A. MiR-155 is overexpressed in patients with atopic dermatitis and modulates T-cell proliferative responses by targeting cytotoxic T lymphocyte-associated antigen 4. J Allergy Clin Immunol. 2010;126:581–589. e581–520. doi: 10.1016/j.jaci.2010.05.045. [DOI] [PubMed] [Google Scholar]
- 50.Malmhall C, Alawieh S, Lu Y, Sjostrand M, Bossios A, Eldh M, Radinger M. MicroRNA-155 is essential for T(H)2-mediated allergen-induced eosinophilic inflammation in the lung. The Journal of allergy and clinical immunology. 2014;133:1429–1438. 1438 e1421–1427. doi: 10.1016/j.jaci.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 51.Yeh TH, Tsai CH, Chen YS, Hsu WC, Cheng CH, Hsu CJ, Lee SY. Increased communication among nasal epithelial cells in air-liquid interface culture. Laryngoscope. 2007;117:1439–1444. doi: 10.1097/MLG.0b013e318063e84f. [DOI] [PubMed] [Google Scholar]
- 52.Hill DB, Button B. Establishment of respiratory air-liquid interface cultures and their use in studying mucin production, secretion, and function. Methods Mol Biol. 2012;842:245–258. doi: 10.1007/978-1-61779-513-8_15. [DOI] [PubMed] [Google Scholar]
- 53.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 54.Panganiban RP, Wang Y, Howrylak J, Chinchilli VM, Craig TJ, August A, Ishmael FT. Circulating microRNAs as biomarkers in patients with allergic rhinitis and asthma. The Journal of allergy and clinical immunology. 2016;137:1423–1432. doi: 10.1016/j.jaci.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 55.Gao P, Zhou Y, Xian L, Li C, Xu T, Plunkett B, Huang SK, Wan M, Cao X. Functional effects of TGF-beta1 on mesenchymal stem cell mobilization in cockroach allergen-induced asthma. Journal of immunology. 2014;192:4560–4570. doi: 10.4049/jimmunol.1303461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Panganiban RP, Pinkerton MH, Maru SY, Jefferson SJ, Roff AN, Ishmael FT. Differential microRNA epression in asthma and the role of miR-1248 in regulation of IL-5. American journal of clinical and experimental immunology. 2012;1:154–165. [PMC free article] [PubMed] [Google Scholar]
- 57.Panganiban RP, W Y, Howrylak J, Chinchilli VM, Craig TJ, August A, Ishmael FT. Circulating microRNAs as biomarkers in allergic rhinitis and asthma. Journal of Allergy and Clinical Immunology. 2015 doi: 10.1016/j.jaci.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 58.Zhu W, Qin W, Atasoy U, Sauter ER. Circulating microRNAs in breast cancer and healthy subjects. BMC research notes. 2009;2:89. doi: 10.1186/1756-0500-2-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Witkos TM, Koscianska E, Krzyzosiak WJ. Practical Aspects of microRNA Target Prediction. Current molecular medicine. 2011;11:93–109. doi: 10.2174/156652411794859250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chan TK, Loh XY, Peh HY, Tan WN, Tan WS, Li N, Tay IJ, Wong WS, Engelward BP. House dust mite-induced asthma causes oxidative damage and DNA double-strand breaks in the lungs. The Journal of allergy and clinical immunology. 2016;138:84–96. e81. doi: 10.1016/j.jaci.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 61.Hristova M, Habibovic A, Veith C, Janssen-Heininger YM, Dixon AE, Geiszt M, van der Vliet A. Airway epithelial dual oxidase 1 mediates allergen-induced IL-33 secretion and activation of type 2 immune responses. The Journal of allergy and clinical immunology. 2016;137:1545–1556. e1511. doi: 10.1016/j.jaci.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nadeem A, Alharbi NO, Vliagoftis H, Tyagi M, Ahmad SF, Sayed-Ahmed MM. Proteinase activated receptor-2-mediated dual oxidase-2 up-regulation is involved in enhanced airway reactivity and inflammation in a mouse model of allergic asthma. Immunology. 2015;145:391–403. doi: 10.1111/imm.12453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sanders PN, Koval OM, Jaffer OA, Prasad AM, Businga TR, Scott JA, Hayden PJ, Luczak ED, Dickey DD, Allamargot C, Olivier AK, Meyerholz DK, Robison AJ, Winder DG, Blackwell TS, Dworski R, Sammut D, Wagner BA, Buettner GR, Pope RM, Miller FJ, Jr, Dibbern ME, Haitchi HM, Mohler PJ, Howarth PH, Zabner J, Kline JN, Grumbach IM, Anderson ME. CaMKII is essential for the proasthmatic effects of oxidation. Science translational medicine. 2013;5:195ra197. doi: 10.1126/scitranslmed.3006135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lambeth JD. NOX enzymes and the biology of reactive oxygen. Nature reviews. Immunology. 2004;4:181–189. doi: 10.1038/nri1312. [DOI] [PubMed] [Google Scholar]
- 65.Luo M, Guan X, Luczak ED, Lang D, Kutschke W, Gao Z, Yang J, Glynn P, Sossalla S, Swaminathan PD, Weiss RM, Yang B, Rokita AG, Maier LS, Efimov IR, Hund TJ, Anderson ME. Diabetes increases mortality after myocardial infarction by oxidizing CaMKII. The Journal of clinical investigation. 2013;123:1262–1274. doi: 10.1172/JCI65268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hart PC, Mao M, de Abreu AL, Ansenberger-Fricano K, Ekoue DN, Ganini D, Kajdacsy-Balla A, Diamond AM, Minshall RD, Consolaro ME, Santos JH, Bonini MG. MnSOD upregulation sustains the Warburg effect via mitochondrial ROS and AMPK-dependent signalling in cancer. Nature communications. 2015;6:6053. doi: 10.1038/ncomms7053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jaffer OA, Carter AB, Sanders PN, Dibbern ME, Winters CJ, Murthy S, Ryan AJ, Rokita AG, Prasad AM, Zabner J, Kline JN, Grumbach IM, Anderson ME. Mitochondrial-targeted antioxidant therapy decreases transforming growth factor-beta-mediated collagen production in a murine asthma model. American journal of respiratory cell and molecular biology. 2015;52:106–115. doi: 10.1165/rcmb.2013-0519OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5:522–531. doi: 10.1038/nrg1379. [DOI] [PubMed] [Google Scholar]
- 69.Valinezhad Orang A, Safaralizadeh R, Kazemzadeh-Bavili M. Mechanisms of miRNA-Mediated Gene Regulation from Common Downregulation to mRNA-Specific Upregulation. Int J Genomics. 2014;2014:970607. doi: 10.1155/2014/970607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ghio AJ, Carraway MS, Madden MC. Composition of air pollution particles and oxidative stress in cells, tissues, and living systems. Journal of toxicology and environmental health. Part B, Critical reviews. 2012;15:1–21. doi: 10.1080/10937404.2012.632359. [DOI] [PubMed] [Google Scholar]
- 71.Johansson K, Malmhäll C, Ramos-Ramírez P, Rådinger M. MicroRNA-155 is a critical regulator of type 2 innate lymphoid cells and IL-33 signaling in experimental models of allergic airway inflammation. The Journal of allergy and clinical immunology. 2017;139:1007. doi: 10.1016/j.jaci.2016.06.035. [DOI] [PubMed] [Google Scholar]
- 72.Okoye IS, Czieso S, Ktistaki E, Roderick K, Coomes SM, Pelly VS, Kannan Y, Perez-Lloret J, Zhao JL, Baltimore D, Langhorne J, Wilson MS. Transcriptomics identified a critical role for Th2 cell-intrinsic miR-155 in mediating allergy and antihelminth immunity. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:E3081–3090. doi: 10.1073/pnas.1406322111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zech A, Ayata CK, Pankratz F, Meyer A, Baudiss K, Cicko S, Yegutkin GG, Grundmann S, Idzko M. MicroRNA-155 modulates P2R signaling and Th2 priming of dendritic cells during allergic airway inflammation in mice. Allergy. 2015;70:1121–1129. doi: 10.1111/all.12643. [DOI] [PubMed] [Google Scholar]
- 74.Zhou H, Li J, Gao P, Wang Q, Zhang J. miR-155: A Novel Target in Allergic Asthma. Int J Mol Sci. 2016;17 doi: 10.3390/ijms17101773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Comer BS, Camoretti-Mercado B, Kogut PC, Halayko AJ, Solway J, Gerthoffer WT. MicroRNA-146a and microRNA-146b expression and anti-inflammatory function in human airway smooth muscle. American journal of physiology. Lung cellular and molecular physiology. 2014;307:34. doi: 10.1152/ajplung.00174.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Choi S, Kim J, Kim JH, Lee DK, Park W, Park M, Kim S, Hwang JY, Won MH, Choi YK, Ryoo S, Ha KS, Kwon YG, Kim YM. Carbon monoxide prevents TNF-alpha-induced eNOS downregulation by inhibiting NF-kappaB-responsive miR-155-5p biogenesis. Exp Mol Med. 2017;49:e403. doi: 10.1038/emm.2017.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang L, Liu L, Ying H, Yu Y, Zhang D, Deng H, Zhang H, Chai J. Acute downregulation of miR-155 leads to a reduced collagen synthesis through attenuating macrophages inflammatory factor secretion by targeting SHIP1. J Mol Histol. 2018;49:165–174. doi: 10.1007/s10735-018-9756-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.