Abstract
Acute oesophageal necrosis (AON), also known as ‘black oesophagus’, is a rare condition characterised by the necrosis of the oesophagus usually involving the distal part. It has been associated with various conditions, and the pathogenesis is thought to involve hypovolaemia combined with decreased function of oesophageal protective mucosal barriers and may be compounded by the effect of gastric secretions on oesophageal mucosa. The hallmark of this condition is characteristic circumferential black discolouration of the distal oesophagus that may extend proximally. We present a case of a man who presented with haematemesis associated with cocaine abuse. Oesophagogastroduodenoscopy confirmed black oesophagus. The patient was managed with intravenous fluids, packed red blood cell transfusions, proton pump inhibitors and sucralfate suspension; however, he failed to recover. We have also reviewed the previous reported cases of AON in association with cocaine use.
Keywords: gastroenterology, endoscopy
Background
Acute oesophageal necrosis (AON), also termed ‘black oesophagus’ and ‘acute necrotising oesophagitis’, is characterised by diffuse circumferential black appearance of oesophageal mucosa on endoscopy that usually affects the distal oesophagus and stops abruptly at the gastro-oesophageal junction.1–5 It is a rare disease with a prevalence of up to 0.2% in some autopsy series.6 7 In endoscopy series, its prevalence has ranged from 0.001% to 0.2% of cases.7–11 The aetiology of AON is multifactorial. It arises in a setting of tissue hypoperfusion due to haemodynamic compromise, impaired local protective mechanisms that may be due to some underlying illness and topical chemical injury due to gastric fluid regurge.12 The patient usually presents with signs of upper gastrointestinal (GI) bleeding like haematemesis and melena. Other symptoms like epigastric pain, nausea, vomiting, dysphagia, chest pain and syncope may also be present.3 Associated multiple comorbidities are usually present. Physical examination findings are usually related to an underlying medical condition. Tachycardia, hypotension, shock, fever, cachexia, hypoxia and abdominal tenderness are some of the signs that can be present, but none of these are specific for this condition.3 Diagnosis is made by endoscopy. A biopsy is required to rule out infectious and other causes of oesophageal necrosis. Management classically involves treatment of the underlying illness, intravenous fluids, packed red blood cell transfusion, keeping the patient nil per oral, proton pump inhibitors (PPIs) and sucralfate suspension.3 The outcome depends to a large extent on the comorbidities that the patient has.
Case presentation
A 50-year-old man was brought to the emergency department in an unresponsive state by a friend. He had three episodes of haematemesis in the 6 hours prior to presentation. He also had multiple episodes of vomiting prior to that. The patient had a history of alcohol abuse, hypertension, fatty liver and coronary artery disease. The patient also had a long history of gastro-oesophageal reflux disease for which he was taking antacids occasionally. His home medications included PPIs and aspirin. The patient did not have any history of melena or haematochezia.
On further questioning, the patient’s friend mentioned that the patient regularly used cocaine and the current episode of vomiting and haematemesis started after cocaine use. The patient would also drink four to five cans of beer per day.
Initial physical examination revealed a patient in distress. He looked lethargic and pale. He was hypotensive with a blood pressure of 85/60 mm Hg, a pulse of 122/min, respiratory rate of 20 bpm and oxygen saturation of 95%. Abdominal examination revealed mild hepatomegaly and mild tenderness on deep palpation of the epigastrium. Neurological examination revealed a Glasgow Coma Scale (GCS) score of 7/15. However, there were no signs of an upper motor neuron lesion. The rest of his systemic examination was unremarkable.
Investigations
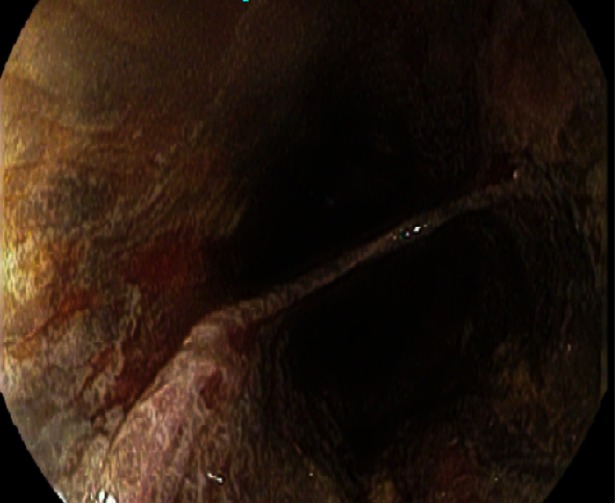
Pertinent laboratory studies included an Hb of 8.2 g/dL, mean corpuscular volume of 100 fL, platelet count of 124×109/L and white blood cell count of 12 x 109/L. His creatinine was at 1.1 mg/dL and urea nitrogen 41 mg/dL. Serum potassium was 3.0 mmol/L while serum sodium level was within normal limits at 145 mmol/L. His serum protein level and serum albumin were low at 4.8 g/dL and 2.9 g/dL, respectively. His total bilirubin was also raised with 6.9 mg/dL with raised SGOT and SGPT of 979 IU/L and 1312 IU/L, respectively. His abdominal ultrasound performed showed mild hepatomegaly while chest X-ray was normal. Oesophagogastroduodenoscopy was performed. It showed circumferential necrotic, friable oesophagus that extended from 21 cm to 40 cm from the incisors (figure 1). There was associated friable red mucosa (figure 2).
Figure 1.
Oesophagoscopy showing necrotic, friable oesophagus that extended from 21 cm to 40 cm from the incisors.
Figure 2.
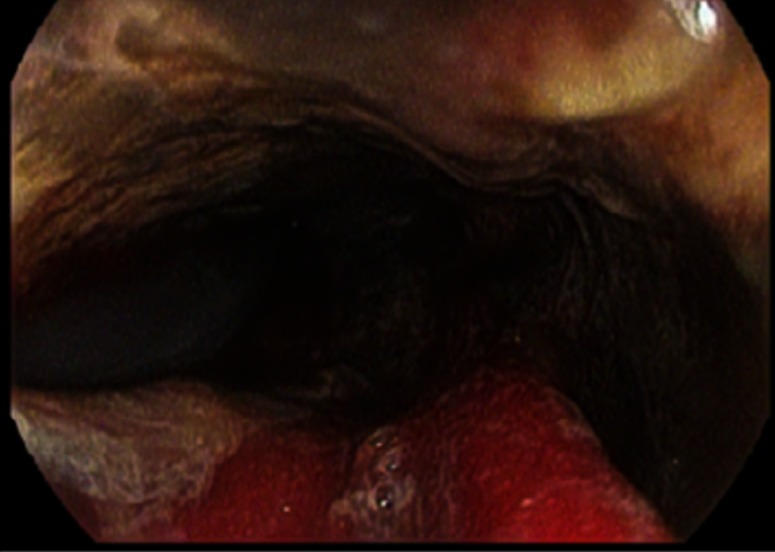
Oesophagoscopy demonstrating the associated friable red mucosa along the necrotic area.
Differential diagnosis
On presentation, our suspicion was bleeding oesophageal varices as the patient was a known alcoholic. Other possibilities included acute gastritis, Mallory-Weiss tear or Boerhaave syndrome.
Treatment
The patient was resuscitated with intravenous fluids and was given two blood transfusions. After the diagnosis of black oesophagus, he was subsequently given intravenous PPIs and sucralfate for the management of black oesophagus.
Outcome and follow-up
The patient was shifted to the intensive care unit where he was constantly monitored. However, the patient’s condition worsened and gradually his GCS score went from 7/15 at the time of admission to 3/15. The patient subsequently expired 12 hours after admission secondary to multiorgan failure.
Discussion
AON, also commonly called ‘black oesophagus’ and ‘acute necrotising oesophagitis’, was first described by Goldenberg in 1990.13 14 It is a condition in which the oesophagus, usually the distal portion, develops necrosis of the mucosa. Rarely, it can have widespread oesophageal involvement and extend to the proximal portion as well.3 It is a life-threatening condition with a high mortality rate. It is considered to be under-reported, in part due to decreased awareness of this condition as a differential of upper GI bleeding and in part due to the self-resolving nature of black oesophagus in some cases.3
We performed a comprehensive review of all the case reports and case series of black oesophagus through PubMed, with no time filter and no language barrier. The search terms included ‘black esophagus’, ‘acute esophageal necrosis’ and ‘necrotizing esophagitis’. We found a total of four previous case reports reporting AON in association with cocaine abuse. We reviewed these reported cases and summarised the patient characteristics in table 1.
Table 1.
Characteristics of the reported cases of AON in association with cocaine use reported so far
| Authors | Age/sex | Presentation | Underlying condition/comorbidities | Endoscopic findings | Management | Outcome/complications |
| Shafa et al15 | 25/M | DKA, melena, acute anaemia and dysphagia | Insulin-dependent DM and HTN. Alcoholic, cocaine and cannabis user | Circumferential necrosis throughout the oesophagus and a mid-oesophageal stricture 5 cm in length | Gastrostomy tube and supportive therapy | Recovered strictures |
| Altenburger et al16 | 45/F | Found unresponsive | Cocaine and alcohol abuse | On autopsy examination, the oesophagus was black with ischaemic necrosis | Died | |
| Pineo and Pineo17 | 30/M | Epigastric pain of 1-day duration, haematemesis and weakness | Cocaine, bupropion and amphetamine overdose | Oesophageal necrosis | PPI, intravenous opioids and nasogastric tube insertion for presumptive small bowel obstruction | Died |
| Singh et al18 | 49/M | Dysphagia, haematemesis, acute renal failure, severe GERD | Achalasia, CHF, anaemia, heavy alcohol, tobacco, cocaine use | Necrotic appearing friable areas of spontaneous bleeding | NPO, intravenous PPI twice daily, 100 U of botulinum toxin injected at LOS | Recovered |
AON, acute oesophageal necrosis; CHF, congestive heart failure; DKA, diabetic ketoacidosis; DM, diabetes mellitus; GORD, gastro-oesophageal reflux disease; HTN, hypertension; LOS, lower oesophageal sphincter; PPI, proton pump inhibitor.
Although the exact aetiology of AON is not known, it is hypothesised that decreased blood flow due to haemodynamic compromise combined with backflow of gastric contents due to gastric outlet obstruction or vomiting, and decreased protective mucosal barriers can all contribute to black oesophagus.3 As such, the pathogenesis is likely multifactorial. This is also supported by the different conditions in which black oesophagus has been reported. Many patients have some comorbidities like hypertension, diabetes and dyslipidaemia along with development of black oesophagus. This has given rise to the theory that patients who develop black oesophagus have some previous predisposition to develop oesophageal necrosis, and this is then precipitated by acute events in such patients. The acute event may be a hypotensive episode compromising blood flow to the already vulnerable lower oesophagus. Or in some cases, it may be episodes of vomiting with gastric contents damaging the oesophageal mucosa.3 Atherosclerotic vessel disease is one of the more frequently reported associated comorbidities with black oesophagus. This may explain why this condition is much more common among men as compared with women and in an age group that is more likely to have atherosclerotic vessel disease.3 The distal oesophagus is the most frequently involved region and there are several factors that may play a role in this. The distal oesophagus has a relatively weaker blood supply and poorer anastomosis as compared with the rest of the oesophagus. The distal oesophagus is also more exposed to gastric contents in cases of gastric acid reflux. Cocaine use has previously been associated with acute oesophageal necrosis. Four (n=4) cases have previously been described in association with cocaine use.15–18 Cocaine is known to cause serious vasoconstriction, and it is thought that a cocaine overdose may have precipitated AON by compromising the blood supply to the oesophagus, especially in predisposed patients.
AON is usually diagnosed on endoscopy in patients presenting with upper GI bleeding. Black discolouration of the oesophagus is characteristic.3 19 A biopsy is required to rule out infectious causes of AON, which include Klebsiella pneumoniae, Candida albicans, cytomegalovirus and herpes simplex virus.8 11 On histology, absence of viable epithelium, necrosis of mucosa extending into submucosa, heavy leucocytic infiltrates and inflammatory changes may be seen.14 The role of angiography has not been defined clearly for diagnostic or therapeutic purposes in AON.12
Management of black oesophagus is primarily focused on supportive measures and treating the underlying condition associated with it.3 Supportive measures like intravenous fluids and packed red blood cells in case of acute anaemia are usually given to the patient. The mainstay of therapy is PPIs that suppress gastric acid secretion and avoid further injury to the oesophagus. The patient is kept nil per oral, and after 24 hours, sucralfate suspension is administered to prevent oesophageal injury due to its protective function on oesophageal mucosa. Nasogastric tube is strongly advised against as it may rupture the oesophagus.3
The most serious complication of black oesophagus is oesophageal perforation and has been reported to occur in 7% of the patients.3 Such patients usually deteriorate very rapidly and have a high mortality rate. Duodenal ulcers may occur more frequently with black oesophagus as they may have a common blood supply from the coeliac trunk and in case of some pathology or event, they may be simultaneously affected.3 Oesophageal stricture formation is a late sequelae of black oesophagus.
The mortality of black oesophagus has variously been reported to be between 30% and 50%. However, ultimately the outcome of black oesophagus depends more on the associated underlying comorbidity.3
Learning points.
Acute oesophageal necrosis should be considered in any patient with upper gastrointestinal bleeding having multiple comorbid conditions.
Though multiple aetiologies are associated with acute oesophageal necrosis, cocaine use can also precipitate it.
Diagnosis is obtained with endoscopy having characteristic findings. The passing of nasogastric tube is forbidden to avoid its dreaded complication of oesophageal perforation.
Treatment should be aimed at underlying illness. Prompt supportive therapy with fluids, packed red blood cells, followed by treatment with proton pump inhibitors, sucralfate and keeping patient nil per oral can help the patient.
Footnotes
Contributors: WU and KS did the literature search. HMAA and AR wrote the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Moretó M, Ojembarrena E, Zaballa M, et al. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy 1993;25:534–8. 10.1055/s-2007-1009121 [DOI] [PubMed] [Google Scholar]
- 2.Obermeyer R, Kasirajan K, Erzurum V, et al. Necrotizing esophagitis presenting as a black esophagus. Surg Endosc 1998;12:1430–3. 10.1007/s004649900875 [DOI] [PubMed] [Google Scholar]
- 3.Gurvits GE, Cherian K, Shami MN, et al. Black esophagus: new insights and multicenter international experience in 2014. Dig Dis Sci 2015;60:444–53. 10.1007/s10620-014-3382-1 [DOI] [PubMed] [Google Scholar]
- 4.Geller A, Aguilar H, Burgart L, et al. The black esophagus. Am J Gastroenterol 1995;90:2210-2. [PubMed] [Google Scholar]
- 5.Brennan JL. Case of extensive necrosis of the oesophageal mucosa following hypothermia. J Clin Pathol 1967;20:581–4. 10.1136/jcp.20.4.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Etienne JP, Roge J, Delavierre P, et al. [Esophageal necrosis of vascular origin]. Sem Hop 1969;45:1599–606. [PubMed] [Google Scholar]
- 7.Postlethwait RW, Musser AW. Changes in the esophagus in 1,000 autopsy specimens. J Thorac Cardiovasc Surg 1974;68:953. [PubMed] [Google Scholar]
- 8.Lacy BE, Toor A, Bensen SP, et al. Acute esophageal necrosis: report of two cases and a review of the literature. Gastrointest Endosc 1999;49:527–32. 10.1016/S0016-5107(99)70058-1 [DOI] [PubMed] [Google Scholar]
- 9.Augusto F, Fernandes V, Cremers MI, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004;36:411–5. 10.1055/s-2004-814318 [DOI] [PubMed] [Google Scholar]
- 10.Julián Gómez L, Barrio J, Atienza R, et al. [Acute esophageal necrosis. An underdiagnosed disease]. Rev Esp Enferm Dig 2008;100:701–5. [DOI] [PubMed] [Google Scholar]
- 11.Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002;56:213–7. 10.1016/S0016-5107(02)70180-6 [DOI] [PubMed] [Google Scholar]
- 12.Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol 2010;16:3219–25. 10.3748/wjg.v16.i26.3219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990;98:493–6. 10.1016/0016-5085(90)90844-Q [DOI] [PubMed] [Google Scholar]
- 14.Gurvits GE, Shapsis A, Lau N, et al. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007;42:29–38. 10.1007/s00535-006-1974-z [DOI] [PubMed] [Google Scholar]
- 15.Shafa S, Sharma N, Keshishian J, et al. The black esophagus: a rare but deadly disease. ACG Case Rep J 2016;3:88–91. 10.14309/crj.2016.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altenburger DL, Wagner AS, Li S, et al. A case of black esophagus with histopathologic description and characterization. Arch Pathol Lab Med 2011;135:797–8. 10.1043/2010-0128-C.1 [DOI] [PubMed] [Google Scholar]
- 17.Pineo CE, Pineo TZ. Acute oesophageal necrosis in a young man with cocaine and alcohol abuse. BMJ Case Rep 2016;2016:bcr2016216138 10.1136/bcr-2016-216138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh D, Singh R, Laya AS. Acute esophageal necrosis: a case series of five patients presenting with "black esophagus". Indian J Gastroenterol 2011;30:41–5. 10.1007/s12664-011-0082-z [DOI] [PubMed] [Google Scholar]
- 19.Manno V, Lentini N, Chirico A, et al. Acute esophageal necrosis (black esophagus): a case report and literature review. Acta Diabetol 2017;54:1061–3. 10.1007/s00592-017-1028-4 [DOI] [PubMed] [Google Scholar]