Abstract
Essentials.
Delayed‐onset heparin‐induced thrombocytopenia can lead to severe thrombocytopenia in the setting of recent major vascular surgery.
Intravenous immunoglobulin (IVIG) can be used as a supplementary treatment when platelet count fails to improve with conventional treatment.
When platelet counts are severely low, benefits of using IVIG can outweigh the risks of thromboembolic events.
Delayed onset heparin induced thrombocytopenia (HIT), is characterized by a late nadir due to persistent platelet‐activating IgG antibodies. It typically begins or worsens 5 or more days after heparin is discontinued with complications such as thrombosis up to 3 weeks after exposure to heparin.1–3 In 50% of cases, the platelet count can decrease to very low numbers (<20 000/μL), which is not usual for typical HIT. Here we report 2 cases of post‐operative delayed onset HIT manifesting as severe thrombocytopenia that persisted despite cessation of heparin and initiation of argatroban. Key Clinical Question: Is intravenous immunoglulin beneficial in severe refractory delayed‐onset HIT?
Keywords: heparin; immunoglobulins, intravenous; thrombocytopenia; thrombosis
1. INTRODUCTION
Patients with type II immune mediated heparin‐induced thrombocytopenia (HIT) develop antibodies to platelet factor 4 (PF4) and develop a clinical syndrome characterized by a drop in platelet count and a prothrombotic state causing venous or arterial thrombosis.1, 2 Delayed‐onset HIT is usually suspected when the platelet count fall begins after stopping heparin. Delayed‐onset HIT is also suspected with worsening thrombocytopenia after heparin cessation and is considered an “autoimmune‐like HIT”.3, 4, 5, 6 The platelet count nadir usually occurs between 10 and 17 days post‐immunizing heparin exposure. In some cases, the thrombocytopenia can persist for several weeks. It is commonly reported after major surgical interventions.4, 6, 7 These patients are typically challenging to manage due to the persistence of their HIT antibodies and as such, their platelets remain low, leaving them at risk of thrombotic and bleeding complications. It is postulated that trauma and the inflammatory state prime an immune response toward the immunogenic cationic PF4+ anionic heparin complex.8 HIT commonly occurs postoperatively, likely due to the combined effect of the release of PF4 from activated platelets during surgery and the concomitant administration of heparin.6 As such, vascular and cardiac patients have higher rates of platelet factor‐4 heparin antibody seroconversion and HIT after large intraoperative doses of therapeutic heparin or prophylactic post‐operative heparin.2, 9, 10, 11 This case series aims to identify whether there is an indication for IVIG in patients with prolonged and severe thrombocytopenia not responding to conventional HIT treatments.
2. CASE 1
A 49‐year‐old female presented with acute new onset severe bilateral claudication and occluded bilateral popliteal and tibioperoneal arteries with a large thrombus along the anterior wall of the proximal to mid‐descending thoracic aorta. Heparin at 18 units/kg/hour was started and she underwent successful thromboembolectomies of both lower extremities and thoracic endovascular aortic aneurysm repair (TEVAR) with stent graft placement. Her arterial thrombi were thought to be precipitated by multiple risk factors, including the use of combined oral contraceptive pills, and heterozygosity for the prothrombin gene PG20210 mutation.
On hospital day 8, the patient's platelet count dropped from 243 000/μL to 122 000/μL with a positive clinical 4T score of 6. Heparin was stopped and an argatroban drip was started. Heparin‐induced antiplatelet antibodies and PF4 antibodies ELISA screen were positive at 2.79 OD and 95‐97% SRA at 0.1 and 0.5 IU/mL UFH, respectively. Despite changing heparin to argatroban, platelets continued to decline. The worsening thrombocytopenia despite being having stopped heparin suggested a diagnosis of delayed onset HIT. Intravenous immunoglobulin 1 g/kg/day and methylprednisolone 1 g/kg/day were given on days 11 and 12, when platelet count fell to 11 000/μL. On day 12, the patient was found to have a symptomatic catheter associated non‐occlusive right internal jugular deep vein thrombosis. The central catheter was not heparin coated.
Platelet count recovered to 81 000/μL on day 14, but began to decline again the following day (Figure 1). Repeat HIT studies on day 15 remained strongly positive by ELISA with an optic density of 3.14 and SRA of 91 and 100% with 0.1 and 0.5 IU/mL UFH, respectively. Repeat computed tomography angiography on day 15 showed an aortic endograft thrombus. Platelets nadired at 5000/μL on day 18, but recovered after another dose of IVIG, reaching 150 000/μL at discharge on day 20 (Figure 1).
Figure 1.
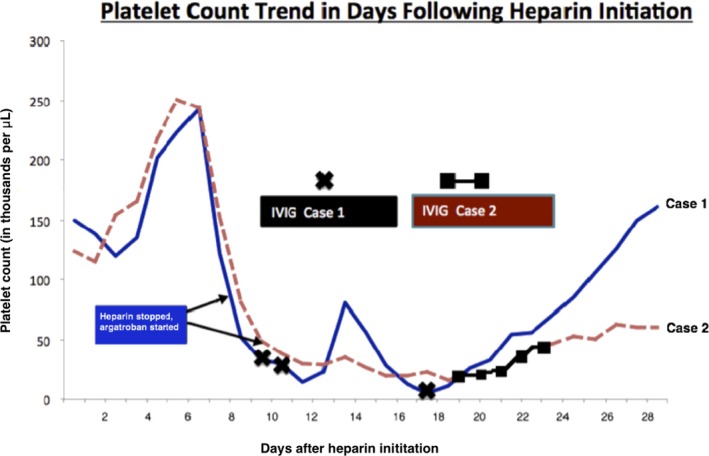
Platelet count trend with interventions versus days post heparin initiation for both cases
3. CASE 2
An 84‐year‐old female presenting with acute chest and back pain was found to have a large descending aortic aneurysm with impending rupture. She underwent a TEVAR. Prophylactic unfractionated heparin was started. On postoperative day (POD) 9, the platelet count dropped to 81 000/μL. HIT was diagnosed with a 4T score of 7, positive HIT ELISA with an optical density of 2.805, and a positive SRA with 100% serotonin release at 0.1 and 0.5 IU/mL UFH. Heparin was discontinued and argatroban initiated. She was subsequently found to have new deep venous thromboses in the right internal jugular and right posterior tibial veins.
The platelet count continued to decline despite avoidance of heparin products. A platelet count of 31 000/μL triggered testing for DIC, which showed hyperfibrinolysis. A workup, performed 12 hours after holding argatroban, revealed a low fibrinogen level of 75 mg/dL and normal activity of factors VII, VIII and X. Mixing studies were negative, thus excluding the presence of a factor inhibitor. Due to intermittent epistaxis and hemoptysis, she received 2 units of fresh frozen plasma on POD 17. On POD 19, platelets nadired at 16 000/μL. Given this severe thrombocytopenia and prior bleeding manifestations, she was started on a 5‐day course of IVIG (1 g/kg/day) and methylprednisolone (1 g/kg/day) (Figure 1). Due to persistently low platelets (Figure 1), repeat HIT studies were performed on POD 22, revealing an optical density of 2.46 and positive SRA with 100% serotonin release at 0.1 and 0.5 IU/mL UFH. Her platelets began to recover by POD 26, at which time argatroban was switched to fondaparinux (off label treatment for HIT). Platelets further rose to above 100 000 upon follow‐up, one week later.
4. DISCUSSION
4.1. Clinical presentation of delayed HIT
Severe thrombocytopenia is not typically seen in HIT, however it has been described in 50% of patients with delayed onset HIT.6 In these cases, platelet counts will usually recover slowly. There are also persistently high titers of platelet‐activating IgG induced by heparin as seen in this case (up to 20 days after heparin administration).6, 7 In a published case‐series of such patients, there was greater heparin‐dependent and independent platelet activation at serial dilutions seen in cases than in control patients with typical HIT. These delayed onset HIT patients were also found to have more thrombosis and other complications including disseminated intravascular coagulation (25% of cases).7 The strong activation of platelets seen in serologic testing even in the absence of therapeutic heparin is a characteristic feature of delayed onset HIT.5, 6 Although our laboratory did not perform serotonin release functional assays in the absence of heparin, our suspicion of delayed onset HIT remained elevated due to persistent HIT that worsened after heparin cessation.
4.2. IVIG in the setting of delayed onset HIT
As soon as HIT is suspected, heparin should be discontinued and an alternative anticoagulant should be initiated. Alternative agents include direct thrombin inhibitors, namely argatroban and bivalirudin.12, 13 Guidance on the utilization of IVIG with HIT is scant; however, there are several reports of it being associated with successful results. Many of the published cases in the literature interestingly involve severe thrombocytopenia (below 25 000/μL) that was refractory to conventional therapy4, 9, 14, 15, 16, 17, which is suspicious for delayed onset HIT. Of particular interest, in 2014, Warkentin and Sheppard described a case where IVIG was used in a second lifetime episode of HIT after cardiac surgery with subsequent improvement in platelet counts after two rounds of IVIG, similar to our first case.9
We experienced success with using IVIG/methylprednisolone for delayed onset HIT, when platelet count severely dropped to below 20 000/μL during the postoperative period. Platelet counts began to improve the subsequent day, with one of our patients requiring additional IVIG after platelet count dropped again, due to persistence of antibodies. Case 1 did experience a catheter‐associated thrombosis and aortic endograft thrombosis after IVIG was initially infused. However, it is unclear whether these were recognized adverse reactions to IVIG versus HIT. Otherwise, we found no additional adverse reactions to systemic IVIG. Our cases support the growing evidence that IVIG is a helpful supplemental treatment to increase platelet count and interfere with activation of heparin‐PF4 antibodies in cases of severe persistent HIT, also supported through in vitro analyses.4, 18, 19 In these cases, the benefits of IVIG outweigh the thromboembolic risks. Methylprednisolone may also have provided a benefit, difficult to distinguish from IVIG.
5. CONCLUSION
Further studies should investigate IVIG as an additional treatment to aid recovery of platelets when bleeding risk is high and while awaiting recovery from severe thrombocytopenia as a result of delayed onset HIT. Biologically, there is some interest in proposing IVIG as the treatment of delayed HIT due to persistent platelet‐activating IgG antibodies as the underlying cause, as was presumed in these cases. However, cases should be selected cautiously since IVIG can also increase thromboembolic risk.
AUTHOR CONTRIBUTIONS
K. Doucette: primary author, writing and interpretation. C.B. Destefano: writing, interpretation and editing. N.A. Jain: interpretation and editing. A.L. Cruz: interpretation editing. V. Malkovska: interpretation and editing. K. Fitzpatrick: interpretation and editing.
RELATIONSHIP DISCLOSURES
None of the authors have any disclosures relevant to this paper.
Doucette K, DeStefano CB, Jain NA, Cruz AL, Malkovska V, Fitzpatrick K. Treatment of refractory delayed onset heparin‐induced thrombocytopenia after thoracic endovascular aortic repair with intravenous immunoglobulin (IVIG). Res Pract Thromb Haemost. 2017;1:134–137. 10.1002/rth2.12009
REFERENCES
- 1. Warkentin TE. Heparin‐induced thrombocytopenia: pathogenesis and management. Br J Haematol 2003;121:535–55. [DOI] [PubMed] [Google Scholar]
- 2. Warkentin TE, Kelton JG. A 14‐year study of heparin‐induced thrombocytopenia. Am J Med 1996;101:502–7. [DOI] [PubMed] [Google Scholar]
- 3. Rice L, Attisha WK, Drexler A, Francis JL. Delayed‐onset heparin‐induced thrombocytopenia. Ann Intern Med 2002;136:210–5. [DOI] [PubMed] [Google Scholar]
- 4. Tvito A, Bakchoul T, Rowe JM, Greinacher A, Ganzel C. Severe and persistent heparin‐induced thrombocytopenia despite fondaparinux treatment. Am J Hematol 2015;90:675–8. [DOI] [PubMed] [Google Scholar]
- 5. Warkentin TE, Greinacher A. Management of heparin‐induced thrombocytopenia. Curr Opin Hematol 2016;23:462–70. [DOI] [PubMed] [Google Scholar]
- 6. Kopolovic I, Warkentin TE. Progressive thrombocytopenia after cardiac surgery in a 67‐year‐old man. CMAJ 2014;186:929–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Warkentin TE, Kelton JG. Delayed‐onset heparin‐induced thrombocytopenia and thrombosis. Ann Intern Med 2001;135:502–6. [DOI] [PubMed] [Google Scholar]
- 8. Lubenow N, Hinz P, Thomaschewski S, et al. The severity of trauma determines the immune response to PF4/heparin and the frequency of heparin‐induced thrombocytopenia. Blood 2010;115:1797–803. [DOI] [PubMed] [Google Scholar]
- 9. Warkentin TE, Sheppard JA. Serological investigation of patients with a previous history of heparin‐induced thrombocytopenia who are reexposed to heparin. Blood 2014;123:2485–93. [DOI] [PubMed] [Google Scholar]
- 10. Pouplard C, May MA, Iochmann S, et al. Antibodies to platelet factor 4‐heparin after cardiopulmonary bypass in patients anticoagulated with unfractionated heparin or a low‐molecular‐weight heparin: clinical implications for heparin‐induced thrombocytopenia. Circulation 1999;99:2530–6. [DOI] [PubMed] [Google Scholar]
- 11. Selleng S, Selleng K, Wollert HG, et al. Heparin‐induced thrombocytopenia in patients requiring prolonged intensive care unit treatment after cardiopulmonary bypass. J Thromb Haemost 2008;6:428–35. [DOI] [PubMed] [Google Scholar]
- 12. Greinacher A. Heparin‐induced thrombocytopenia. J Thromb Haemost 2009;7(suppl 1):9–12. [DOI] [PubMed] [Google Scholar]
- 13. Warkentin TE, Pai M, Sheppard JI, Schulman S, Spyropoulos AC, Eikelboom JW. Fondaparinux treatment of acute heparin‐induced thrombocytopenia confirmed by the serotonin‐release assay: a 30‐month, 16‐patient case series. J Thromb Haemost 2011;9:2389–96. [DOI] [PubMed] [Google Scholar]
- 14. Frame JN, Mulvey KP, Phares JC, Anderson MJ. Correction of severe heparin‐associated thrombocytopenia with intravenous immunoglobulin. Ann Intern Med 1989;111:946–7. [DOI] [PubMed] [Google Scholar]
- 15. Grau E, Linares M, Olaso MA, Ruvira J, Sanchis J. Heparin‐induced thrombocytopenia–response to intravenous immunoglobulin in vivo and in vitro. Am J Hematol 1992;39:312–3. [DOI] [PubMed] [Google Scholar]
- 16. Winder A, Shoenfeld Y, Hochman R, Keren G, Levy Y, Eldor A. High‐dose intravenous gamma‐globulins for heparin‐induced thrombocytopenia: a prompt response. J Clin Immunol 1998;18:330–4. [DOI] [PubMed] [Google Scholar]
- 17. Padmanabhan A, Jones CG, Pechauer SM, et al. Intravenous immunoglobulin for treatment of severe refractory heparin‐induced thrombocytopenia. Chest 2017. 10.1016/j.chest.2017.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Greinacher A, Liebenhoff U, Kiefel V, Presek P, Mueller‐Eckhardt C. Heparin‐associated thrombocytopenia: the effects of various intravenous IgG preparations on antibody mediated platelet activation–a possible new indication for high dose i.v. IgG. Thromb Haemost 1994;71:641–5. [PubMed] [Google Scholar]
- 19. Lei BZ, Shatzel JJ, Sendowski M. Rapid and durable response to intravenous immunoglobulin in delayed heparin‐induced thrombocytopenia: a case report. Transfusion 2017;57:919–23. [DOI] [PubMed] [Google Scholar]


