Graphical abstract
Keywords: Calcified amorphous tumor, Mitral annular calcification, Non-neoplastic mass
Highlights
-
•
Mitral annular calcifications (MACs) are chronic degenerative changes that occur mostly along the posterior mitral annulus.
-
•
Calcified amorphous tumors (CATs) constitute rare, non-neoplastic masses of the heart that histologically comprise calcium deposits, inflammatory cells, and fibrin elements.
-
•
Subgroups of cardiac CATs are echogenic spindle-shaped masses that arise from the mitral valve and are frequently related to bulky MACs in patients with end-stage renal disease; they are termed “MAC-related CATs.”
-
•
CATs have a wide variation of presenting symptoms, ranging from no symptoms to shortness of breath, obstruction, and systemic embolization, on the basis of the size and location of the CAT.
-
•
Awareness of MAC-related CATs is important, as they may lead to undesirable extra diagnostic and therapeutic management.
Introduction
Mitral annular calcifications (MACs), calcifications of the mitral annulus, are chronic degenerative changes that occur mostly along the posterior mitral leaflet. The incidence of MACs increases in the presence of end-stage renal disease (ESRD) and atherosclerosis risk factors such as hypertension, diabetes, and dyslipidemia. MACs can also be associated with liquefied necrosis or caseous calcification.1, 2
Calcified amorphous tumors (CATs) constitute rare non-neoplastic masses of the heart that are histologically composed of calcium deposits, inflammatory cells, and fibrin elements. The etiology of CATs is still unclear.3, 4, 5 Subgroups of cardiac CATs are echogenic spindle-shaped masses that arise from the mitral valve and are frequently related to bulky MACs in patients with ESRD; they are termed “MAC-related CATs.”5
Herein, we present a case of a CAT that arose from a MAC in a patient with ESRD and discuss the diagnostic features and management of this patient.
Case Presentation
A 75-year-old woman with a medical history of ESRD and hypertension presented to our outpatient clinic with dyspnea on exertion of a few months' duration. The patient had been maintained on regular hemodialysis for the previous 4 years and had a long-term history of hypertension and no recent history of loss of appetite, fever, or embolic event. She was afebrile and had a blood pressure of 160/80 mm Hg and a pulse rate of 75 beats/min.
Given the exacerbation of her dyspnea on exertion over the past few months, transthoracic echocardiography was performed, which revealed a mobile elongated calcified and spindle-shaped mass (1.3 × 0.3 cm) attached to the ventricular side of a large and bulky posterior MAC (Figure 1, Figure 2, Figure 3, Videos 1–3). Trivial functional mitral regurgitation was present, with no other valvular abnormalities. There was moderate left ventricular hypertrophy with preserved left ventricular systolic function and a left ventricular ejection fraction of 55%.
Figure 1.
Transthoracic echocardiography in the apical long-axis view shows a large bulky posterior MAC (arrow), associated with a linear calcified mass on the ventricular side of the MAC, suggestive of a CAT (arrowhead). AO, Aorta; LA, left atrium; LV, left ventricle.
Figure 2.
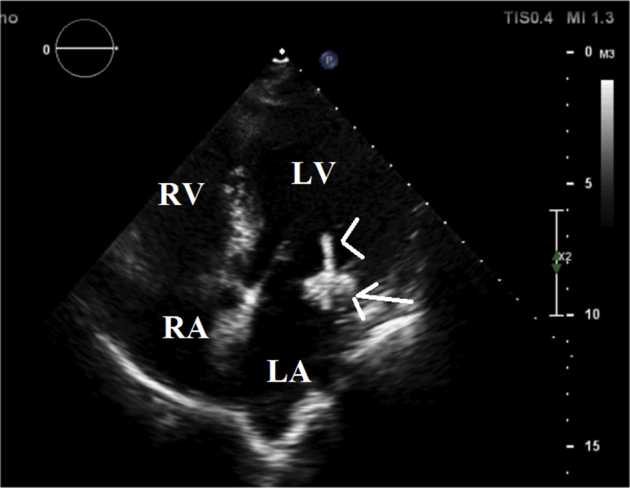
Transthoracic echocardiography in the four-chamber view shows a large bulky mass along the posterior mitral annulus suggestive of MAC (arrow), associated with a linear calcified mass on the ventricular side of the MAC, suggestive of a CAT (arrowhead). LA, Left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
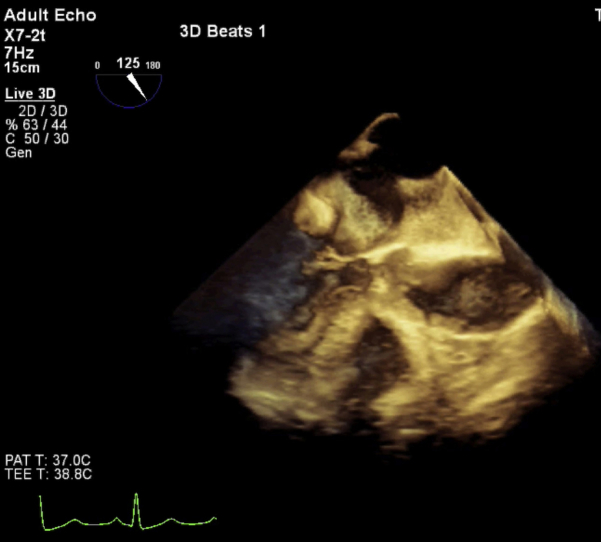
Figure 3.

Transthoracic echocardiography in the short-axis view shows posterior MAC, which is a large calcified bulky mass along the posterior mitral annulus (arrow). IVS, Interventricular septum; MV, mitral valve; RV, right ventricle.
Clinical data and laboratory tests did not suggest infectious endocarditis given the patient's three negative blood cultures, low erythrocyte sedimentation rate, C-reactive protein, and negative two- and three-dimensional transesophageal echocardiographic signs of infective endocarditis (Figure 4, Figure 5, Videos 4 and 5). Cardiac computed tomography supported the diagnosis (Figure 6, Figure 7).
Figure 4.
Three-dimensional transesophageal echocardiography (surgical view) illustrates a large bulky posterior mitral annulus (stars) with no evidence of vegetation. AML, Anterior mitral leaflet; AO, aorta; LAA, left atrial appendage; PML, posterior mitral leaflet.
Figure 5.
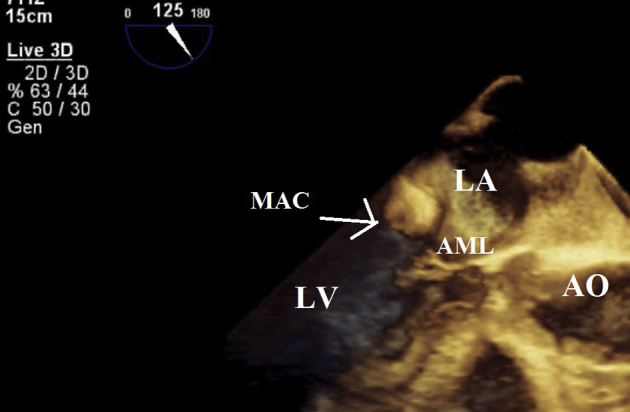
Three-dimensional transesophageal echocardiography in the long-axis view: bulky mass in the left atrial segment of the posterior leaflet. AML, Anterior mitral leaflet; AO, aorta; LA, left atrium; LV, left ventricle.
Figure 6.

Cardiac computed tomography in the long-axis view shows a large bulky posterior MAC (arrow), associated with a linear calcified mass on the ventricular side of the MAC and suggestive of a CAT (arrowhead). LA, Left atrium; LV, left ventricle.
Figure 7.

Cardiac computed tomography in the short-axis view shows posterior MAC with degenerative changes in the mitral valve. LV, Left ventricle; RV, right ventricle.
Considering the typical features of the mass insofar as it was an echogenic spindle-shaped mobile mass arising from a MAC (which typically occurs in patients with ESRD) and the patient's refusal to undergo surgery, a conservative approach and medical follow-up were chosen. Two-year follow-up was uneventful, and the patient's shortness of breath was diminished with antihypertensive therapy. Follow-up echocardiography showed no significant change in her data with respect to the size and features of the mass.
Discussion
We present a MAC-related CAT, which is a subset of CATs that appear as mobile masses arising from MACs and typically occur in patients with histories of ESRD.3 Kubota et al.6 proposed the expressive term “swinging CATs” for mobile lesions that arise from MACs. CATs are calcified masses in the endocardium or heart cavities and have been found in all chambers of the heart; nevertheless, they most frequently present on the mitral valve and the mitral annulus. Regarding the presence of calcification, CATs may be misdiagnosed with other calcified masses such as osteosarcomas, calcified myxomas, and vegetations.
In MAC-related CATs, it is vitally important that CATs be distinguished from mitral valve vegetations.1 The usual location for typical vegetations is the atrial aspect of the mitral valve with tissue texture echo density and/or associated abscess formation or valvular regurgitation.
The typical histologic features of CATs are calcified nodules, associated with inflammatory cells, and fibrin degeneration. Indeed, it has been suggested that mobile CATs that are related to the mitral annulus can be an atypical form of MACs. Interestingly, caseous calcification of the mitral annulus may be a dynamic process, and patients with MACs can progress to caseous calcification of the mitral annulus.7, 8
In a systematic review of English-language articles published up to 2014, Hemptinne et al.3 found 42 CAT cases with wide variations of the presenting symptoms ranging from no symptoms to shortness of breath, obstruction, and systemic embolization on the basis of the size and location of the CAT. Embolic events are not uncommon, especially in mobile CATs. However, high prevalence of cardiovascular risk factors also can contribute to cerebrovascular events in these patients. The growth rate is unknown, with reported fast growth in some patients with MAC-related CATs from 6 weeks to 1 year.
Although a large number of patients with MAC-related CATs have undergone surgical resection to confirm the diagnosis, recently a noninvasive approach and follow-up have also been suggested.3, 9 We opted for this approach with our patient. Two-year follow-up was uneventful and echocardiography showed no change with respect to the size and features of the mass.
In a recent study, Yılmaz et al.9 evaluated cardiac imaging findings in 12 patients with CATs and suggested that cardiac computed tomography and/or cardiac magnetic resonance imaging can support the diagnosis of CATs made by echocardiography. Cardiac computed tomography is useful to confirm the calcification of CATs, which can be large focal or diffuse calcifications of a mass. T1- and T2-weighted magnetic resonance images in patients with CATs show low signal intensity and no contrast enhancement. Yılmaz et al. reported that most of their patients were asymptomatic with advanced age, and the CATs were incidental findings. They proposed that surgery is not necessary in all patients and that asymptomatic patients with nonprogressive masses, especially in the elderly, can be followed up with echocardiography.
Conclusion
CATs are rare non-neoplastic masses of the heart that are histologically composed of calcium deposits, inflammatory cells, and fibrin elements. Mitral valves and annuli are the most frequent locations of CATs. MAC-related CATs, which are a subset of CATs, have a characteristic echocardiographic feature of echogenic spindle-shaped calcified masses attached to MACs and typically occur in patients with histories of ESRD.3
Awareness of MAC-related CATs is important because they may lead to undesirable extra diagnostic and therapeutic management. Surgical intervention has been suggested in most cases. Be that as it may, the risk/benefit ratio should be taken into account, as a mortality rate of 5% has been previously reported. The natural history, risk for embolic events, and management strategy of these masses have yet to be fully elucidated.5
Recently, a noninvasive follow-up approach for elderly asymptomatic patients has been proposed, but it needs more research data.
Footnotes
Conflicts of Interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.case.2017.02.004.
Supplementary Data
Transthoracic echocardiography in the apical long-axis view shows a large bulky posterior MAC, associated with a linear calcified mass on the ventricular side of the MAC and suggestive of a CAT.
Transthoracic echocardiography in the four-chamber view demonstrates a large bulky posterior MAC, associated with a linear calcified mass on the ventricular side of the MAC and suggestive of a CAT mimicking vegetation.
Transthoracic echocardiography in the short-axis view shows posterior MAC, which is a large calcified bulky mass along the posterior mitral annulus.
Three-dimensional transesophageal echocardiography (surgical view) illustrates a large bulky mass in the left atrial segment of the posterior leaflet of the mitral valve.
Three-dimensional transesophageal echocardiography, long-axis view, showing a bulky mass in the left atrial segment of the posterior leaflet.
References
- 1.Fujiwara M., Watanabe H., Iino T., Kobukai Y., Ishibashi K., Yamamoto H. Two cases of calcified amorphous tumor mimicking mitral valve vegetation. Circulation. 2012;125:e432–e434. doi: 10.1161/CIRCULATIONAHA.111.072793. [DOI] [PubMed] [Google Scholar]
- 2.Abramowitz Y., Jilaihawi H., Chakravarty T., Mack M.J., Makkar R.R. Mitral annulus calcification. J Am Coll Cardiol. 2015;66:1934–1941. doi: 10.1016/j.jacc.2015.08.872. [DOI] [PubMed] [Google Scholar]
- 3.Hemptinne Q., Canniere D., Vandenbossche J., Unger P. Cardiac calcified amorphous tumor: a systematic review of the literature. Int J Cardiol Heart Vasc. 2015;7:1–5. doi: 10.1016/j.ijcha.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho H.H., Min J.K., Lin F., Wong S.C., Bergman G. Calcified amorphous tumor of the heart. Circulation. 2008;117:e171–e172. doi: 10.1161/CIRCULATIONAHA.107.730838. [DOI] [PubMed] [Google Scholar]
- 5.Masuda S., Motoyoshi N., Ito K., Hayatsu Y., Akiyama M., Kawamoto S. Surgical removal of calcified amorphous tumor localized to mitral valve leaflet without mitral annular calcification. Surgical Case Rep. 2015;1:39. doi: 10.1186/s40792-015-0040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kubota H., Fujioka Y., Yoshino H., Koji H., Yoshihara K., Tonari K. Cardiac swinging calcified amorphous tumors in end-stage renal failure patients. Ann Thorac Surg. 2010;90:1692–1694. doi: 10.1016/j.athoracsur.2010.04.097. [DOI] [PubMed] [Google Scholar]
- 7.Deluca G., Correale M., Ieva R., Del Salvatore B., Gramenzi S., Di Biase M. The incidence and clinical course of caseous calcification of the mitral annulus: a prospective echocardiographic study. J Am Soc Echocardiogr. 2008;21:828–833. doi: 10.1016/j.echo.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Teoh J.K., Steeds R.P. Cardiac calcified amorphous tumour. Echo Res and Pract. 2015;2:I9–I10. doi: 10.1530/ERP-14-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yılmaz R., Demir A.A., Önür I., Yılbazbayhan D., Dursun M. Cardiac calcified amorphous tumors: CT and MRI findings. Diagn Interv Radiol. 2016;22:519–524. doi: 10.5152/dir.2016.16075. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography in the apical long-axis view shows a large bulky posterior MAC, associated with a linear calcified mass on the ventricular side of the MAC and suggestive of a CAT.
Transthoracic echocardiography in the four-chamber view demonstrates a large bulky posterior MAC, associated with a linear calcified mass on the ventricular side of the MAC and suggestive of a CAT mimicking vegetation.
Transthoracic echocardiography in the short-axis view shows posterior MAC, which is a large calcified bulky mass along the posterior mitral annulus.
Three-dimensional transesophageal echocardiography (surgical view) illustrates a large bulky mass in the left atrial segment of the posterior leaflet of the mitral valve.
Three-dimensional transesophageal echocardiography, long-axis view, showing a bulky mass in the left atrial segment of the posterior leaflet.