Graphical abstract
Keywords: Pericardial effusion, Coronary perforation, Angiosarcoma, Multimodal imaging
Highlights
-
•
Coronary artery perforation was related to angiosarcoma with prior radiation therapy.
-
•
Pericardial effusion must make a neoplastic origin suspicious, even from coronary arteries.
-
•
Angiosarcomas are rare complications of radiotherapy that must be considered in case of complex situations.
Introduction
The occurrence of pericardial effusions involves numerous etiologies, which require the use of multimodal imaging to adapt the management. Here, we report a rare case of secondary effusion due to a coronary perforation caused by an angiosarcoma induced by mediastinal radiotherapy.
Case Presentation
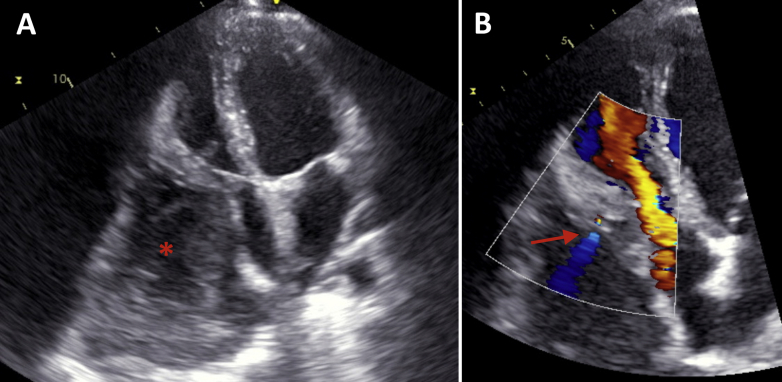
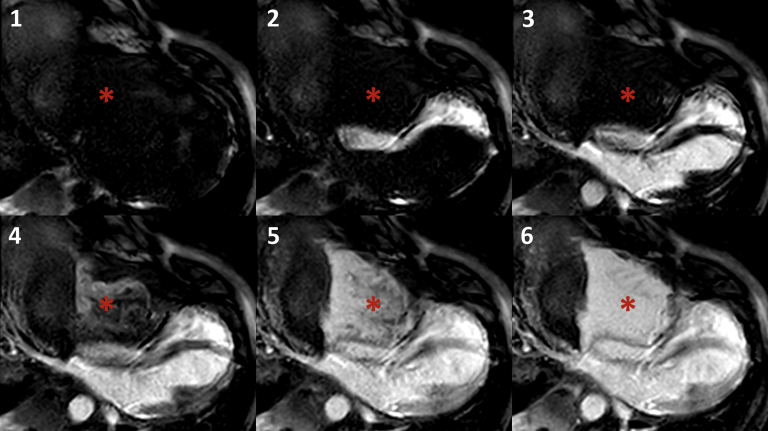
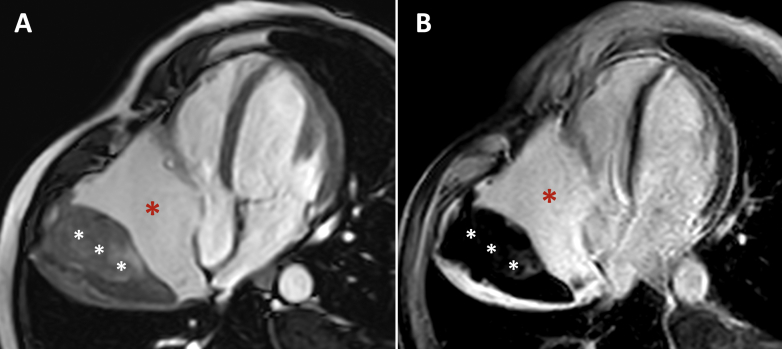
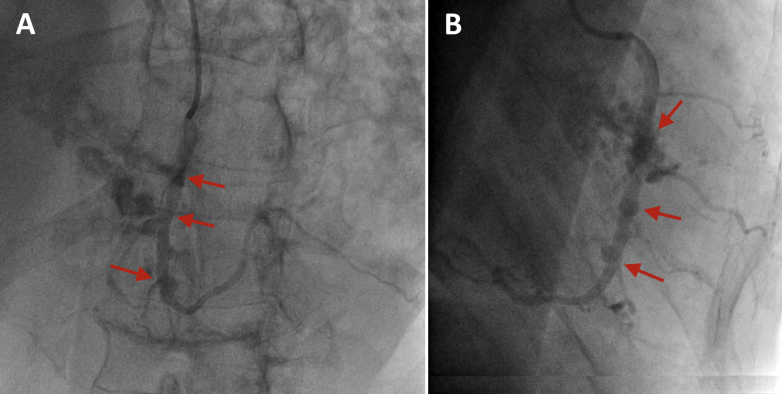
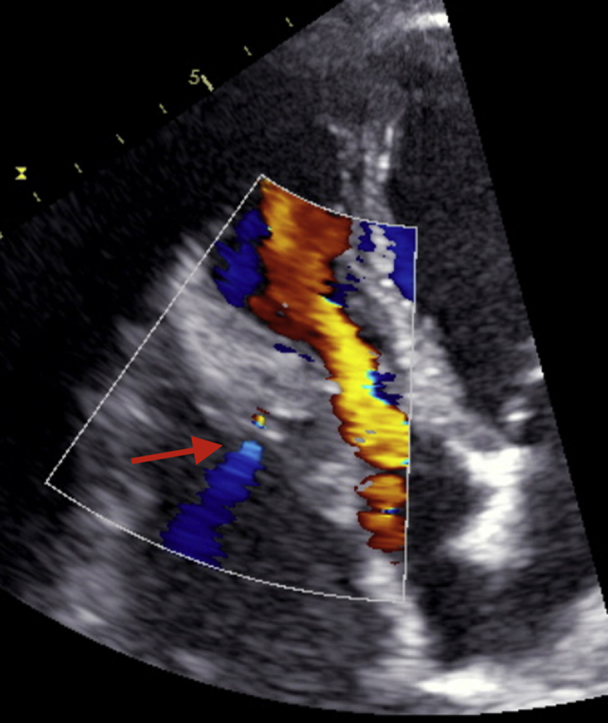
A 53-year-old man was admitted to our institution with congestive heart failure (New York Heart Association functional class III) and anemia. He had a medical history of multiple myeloma, for which several sessions of radiotherapy targeted to isolated plasmacytomas for analgesic reasons in the thoracic spine (D6, D8, and D10) had been performed. He underwent three sessions of 30 Gy divided into 10 fractions. The last session was performed 1 year previously. At admission, transthoracic echocardiography found a voluminous pericardial effusion with small color flow along the right ventricular free wall, suggesting a fistula between the heart cavity and the effusion (Figure 1, Video 1). There was an irregular mass extending along the back of the pericardium suggesting pericardial thrombus (Figure 1, red star), which we initially thought may have been paraneoplastic. Cardiac magnetic resonance imaging was not able to detect perforation of the right ventricular free wall, but perfusion imaging confirmed connection to the pericardial space (Figure 2, Video 2), with the presence of thrombus on the back in contrast-enhanced sequences (Figure 3). Coronary angiography found three fistulas between the right coronary artery and the pericardium (Figure 4, Video 3). Percutaneous treatment of the fistulas by a covered stent was considered but not pursued because of the volume of the pericardial effusion, which required surgical management. Consequently, surgical indication was retained, and the patient underwent pericardial drainage associated with the removal of the first and the second segments of the right coronary artery, completed by a coronary artery bypass with a saphenous graft. During the procedure, the surgeon found inflammatory tissue with multiple small perforations of the right atrial free wall, explaining why coronary blood inflow was constant. Unfortunately, the patient died 2 days later because of acute right heart failure, which was attributed to the ischemia induced by the coronary resection. The anatomic and pathologic exploration of the excised coronary artery revealed an angiosarcoma of the right coronary artery (Figure 5).
Figure 1.
Transthoracic echocardiography. (A) Apical four-chamber view showing pericardial effusion (red star) at the side portion of the right atrium and right ventricular free wall leading to a compressive effect on the tricuspid annulus. (B) Apical four-chamber view with color Doppler showing color spark (red arrow) along the right ventricular free wall.
Figure 2.
Perfusion by cardiac magnetic resonance. Perfusion sequences (four-chamber view) from images 1 to 6 showing dynamic enhancement of the pericardial effusion at the same time as the myocardium (red star).
Figure 3.
Cardiac magnetic resonance. (A) Four-chamber view cine magnetic resonance imaging showing pericardial effusion (red star) along the base of the right ventricular free wall and the back of the right atrium with thrombus (white stars). (B) Four-chamber view, late gadolinium enhancement images showing thrombus (in black, white stars) at the back of the pericardial effusion.
Figure 4.
Coronary angiography. (A) Left anterior oblique view showing fistulas of the second segment of the right coronary artery (red arrows). (B) Right anterior oblique view showing fistulas of the second segment of the right coronary artery (red arrows).
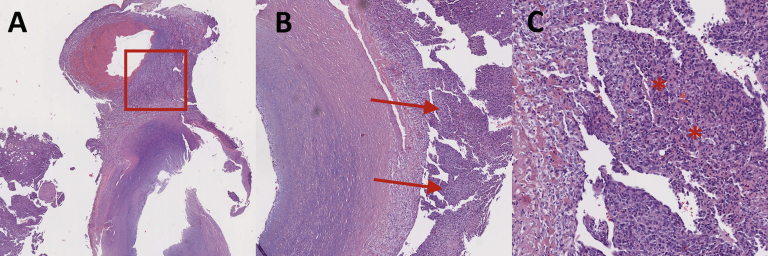
Figure 5.
Pathology. Right coronary artery cross-section determined on Hematoxylin and Eosin–stained section showing proliferation of atypical cells from the vessel, suggesting angiosarcoma. (A) Magnification 2.5× (red square). (B) Magnification 5× (red arrows). (C) Magnification 10× (red stars).
Discussion
In this case, it is legitimate to think that the angiosarcoma, which led to the fistula between the coronary artery and the pericardium, was induced by the previous thoracic radiotherapy. At the time of the surgery, we did not suspect the diagnosis of angiosarcoma or indeed a tumoral process; rather, we initially thought that the perforation was due to fragility of the artery induced by radiotherapy. Improvement in therapeutics for thoracic cancers has shifted neoplastic prognoses to cardiac prognoses, particularly in patients with histories of thoracic radiotherapy.1 Radiation-induced soft tissue sarcoma is a classical complication of thoracic radiotherapy,2 but heart involvement, particularly coronary artery involvement, is rare and unrecognized. However, coronary angiosarcoma has also been reported in the absence of prior radiotherapy, and we cannot exclude the possibility of a metachronous tumor.
Conclusion
The presence of a pericardial effusion must make a neoplastic origin suspicious, particularly in patients with a history of cancer. Although cases are rare, a local origin, from the pericardium or, as in this case, from the coronary artery, is always possible.
Footnotes
Conflicts of Interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.case.2017.04.003.
Supplementary Data
Transthoracic echocardiography. Apical four-chamber view with color Doppler showing color spark along the right ventricular free wall.
Perfusion by cardiac magnetic resonance. Perfusion sequences (four-chamber view) showing dynamic enhancement of the pericardial effusion at the same time as the myocardium.
Coronary angiography. Left anterior oblique view showing fistulas of the second segment of the right coronary artery.
References
- 1.Lee M.S., Finch W., Mahmud E. Cardiovascular complications of radiotherapy. Am J Cardiol. 2013;112:1688–1696. doi: 10.1016/j.amjcard.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 2.Huang J., Mackillop W.J. Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer. 2001;92:172–180. doi: 10.1002/1097-0142(20010701)92:1<172::aid-cncr1306>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography. Apical four-chamber view with color Doppler showing color spark along the right ventricular free wall.
Perfusion by cardiac magnetic resonance. Perfusion sequences (four-chamber view) showing dynamic enhancement of the pericardial effusion at the same time as the myocardium.
Coronary angiography. Left anterior oblique view showing fistulas of the second segment of the right coronary artery.