Graphical abstract

Keywords: Double saddle emboli, Mobile saddle embolus, Free-floating thrombi
Highlights
-
•
Mobile main pulmonary artery emboli on transthoracic echocardiogram.
-
•
Large saddle embolus with mobile component.
-
•
Classic echocardiographic findings of massive pulmonary embolism.
-
•
Complex treatment decision of high-mortality free-floating right heart thrombi.
Introduction
Although free-floating right heart thrombi (FRHT) are a rare finding on transthoracic echocardiogram (TTE), they have been well reported in the literature.1, 2, 3 Patients with FRHT have a high mortality rate and can quickly become clinically unstable. This fact likely contributes to the rarity of discovery of FRHT. There have been a few reports of saddle embolus shown on TTE, but double saddle emboli with a mobile component has yet to be reported.4, 5, 6 Here we present a case of two distinct saddle emboli, one of which is highly mobile, found at the main pulmonary artery (MPA) by TTE.
Case Presentation
A 43-year-old man was admitted to the hospital with bilateral lower quadrant abdominal pain, nausea, and diarrhea. He had complained of 2–3 days of loose and more frequent stools followed by gradual-onset abdominal pain that started the day before admission. Computed tomography imaging of the abdomen showed an acute complicated sigmoid diverticulitis with a contained perforation. He was taken to surgery for an exploratory laparotomy with drainage of intra-abdominal abscess and sigmoid colectomy with end-to-end anastomosis. The patient did well in the perioperative period until he developed sudden-onset shortness of breath and hypoxia on postoperative day 2.
Computed tomography angiography of the chest was performed and showed a multilobar acute pulmonary embolism (PE). A large saddle embolus was discovered in the main pulmonary arterial bifurcation (Figure 1).
Figure 1.

PE protocol computed tomography angiography of the chest showing a large single saddle embolus in the MPA bifurcation.
Treatment was started with intravenous heparin. Ultrasound of the bilateral lower extremities showed an acute deep vein thrombosis within the left popliteal and posterior tibial veins. On the evening of postoperative day 3 he developed sinus tachycardia with a heart rate of 148, blood pressure of 107/67 mm Hg, and oxygen saturation of 80%. He was subsequently transferred to the surgical intensive care unit for closer monitoring. Cardiac examination revealed a regular tachycardia with a fixed wide S2. No murmurs or rubs were auscultated. He did have elevation of his jugular venous pressure noted to be at the angle of the jaw while sitting at 45°. A prominent parasternal heave was readily palpated. Pulmonary exam revealed conversational dyspnea, coarse breath sounds, and tachypnea. Electrocardiogram performed at this time showed sinus tachycardia with an incomplete right bundle branch block. The classic S1Q3T3 was present, with deep S wave in lead I and lead III displaying a Q wave and inverted T wave. ST depression of 1–2 mm was noted in the lateral precordial leads V4–V6. T wave inversions were present in the inferior leads II, III, and aVF indicating possible right ventricular (RV) strain.
Echocardiographic Imaging
Because of his clinical deterioration, an echocardiogram was ordered looking for right heart strain and assessment of left ventricular function. TTE revealed a nonmobile embolus attached to the MPA bifurcation. The echogenicity of this embolus gave it an organizing subacute appearance and distinguished it from the MPA bifurcation. A second large mobile embolus with the body measuring 1.13 cm × 3.81 cm in the MPA bifurcation was identified. The base of this embolus can be seen separate from and bouncing off the subacute embolus mentioned above (Video 1). This highly mobile embolus was less dense and appeared more acute. The proximal portion of the acute thrombus was serpentine in nature and freely moved in the MPA (Figure 2).
Figure 2.
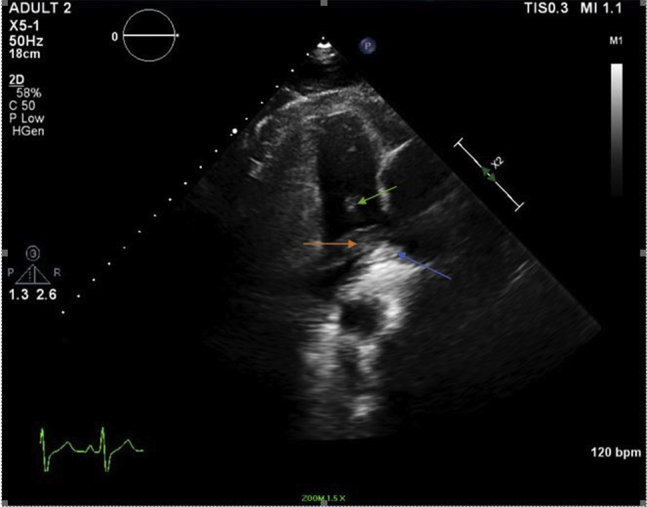
RV outflow view showing a subacute embolus (blue arrow) with a separate less echogenic acute mobile embolus (orange arrow). In the more proximal MPA, a mobile extension can be seen (green arrow).
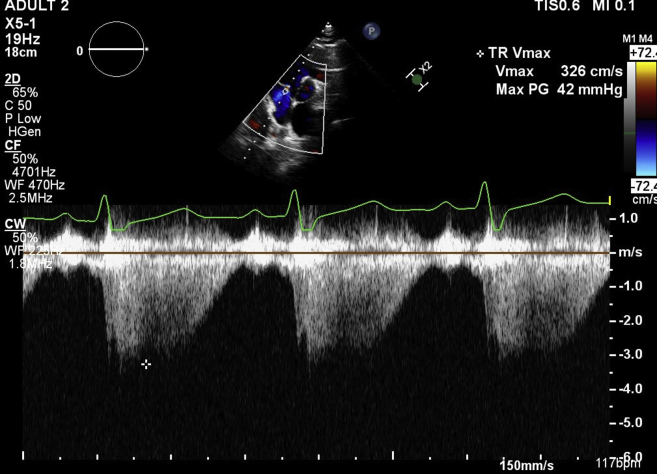
Extension of the acute thrombus was noticed into the right and left pulmonary arteries (Video 1). The MPA was found to be mildly dilated with a measurement of 2.8 cm. The right ventricle was severely dilated and had severely decreased systolic function with a hyperkinetic apical cap and akinesis of the mid to distal free wall (McConnell's sign)7 (Video 2). There was flattening of the interventricular septum with septal dyskinesis and paradoxical motion consistent with pressure overload in the right ventricle. The movement of the septum was seen impinging upon the left ventricle (Video 3). RV systolic pressure was elevated and estimated at 57 mm Hg with the right atrial pressure being elevated at 15 mm Hg (Figure 3).
Figure 3.
Short-axis view showing continuous wave (CW) spectral Doppler over the tricuspid valve with a max pressure gradient (PG) of 42 mm Hg.
Minimal pericardial effusion was noted. The left ventricle was hyperdynamic with an estimated ejection fraction of 70%. It appeared small and compressed by the dilated right ventricle and septal shifting.
Case Outcome
The acute, free-floating nature of this second discovered saddle embolus guided the treatment toward catheter-based ultrasound-assisted thrombolysis (USAT). The patient was transferred to a tertiary care center with expertise in catheter-based PE intervention. After intervention with USAT, the patient slowly improved, was weaned off oxygen completely, and was later discharged home from the tertiary care center on Apixiban. Laboratory testing did reveal a heterozygous prothrombin G20210A mutation.
Discussion
We present a case of a 43-year-old man diagnosed with postoperative massive double PE discovered on TTE at the bifurcation of the MPA. Unfortunately, despite appropriate anticoagulation, he had a second occurrence of an additional saddle embolus that was subsequently discovered on TTE. The uniqueness of this second layer of embolus was its mobility. Free-floating thrombi are usually trapped in the right heart and appear as elongated snake-like figures that are extremely mobile. This can be referred to as the “popcorn sign,” or a “popcorn thrombus.”8 The body of the second embolus has some mobility, but the serpentine extension found in the MPA is highly mobile and has features of thrombus in transit usually found in the right atrium and right ventricle. Rare case reports have shown fixed thrombus in the pulmonary arteries on TTE, but to date there have been no reported cases of mobile double-layered saddle embolus with video documentation by TTE.4, 9, 10, 11
Massive or submassive PEs caused by mobile thrombi convey a much higher degree of mortality. Mobile thrombi in the right heart are a substrate for impending transitive thrombi, which can quickly lead to deterioration and death. Patients with FRHT are found to have more significant clinical deterioration including lower blood pressure, higher likelihood of RV hypokinesis, and increased heart rate than when compared with PE not caused by free floating thrombi.12 Their prognosis also tends to be worse, despite being hemodynamically stable on presentation.12 The mortality rate in this subset of the population has been reported to be as high as 50%.3 The International Cooperative Pulmonary Embolism Registry, a registry of 2,454 patients, of which 1,113 had TTE, showed a 14-day and 3-month all-cause mortality of 21% and 29%, respectively.12 The emergent nature of PE with detection of mobile thrombi makes treatment decisions time critical and crucially important.
Treatment of PE from thrombus in transit and FRHT is not well studied and remains unclear. A series of 38 consecutive patients was studied by Chartier et al. who showed a mortality rate of 44.7% regardless of treatment modality.1 To date, there have been no case series or controlled trials addressing specific treatment for mobile emboli seen at the MPA bifurcation. Here a treatment strategy similar to FRHT etiology was applied. Available treatments include intravenous anticoagulant only, thrombolysis, surgical embolectomy, catheter embolectomy, or more novel treatments such as catheter-based USAT. USAT uses high-frequency and low-power ultrasound to increase the permeability of formed thrombus along with acoustic streaming to assist in thrombus penetration by thrombolytics.13
Systemic thrombolysis is often reported to be a first-line treatment over heparin alone, surgical intervention, or catheter embolectomy.12, 13, 14, 15 This is possibly due to the lack of difference in mortality between treatment strategies and the relatively less invasive nature of thrombolysis. Because of the lack of larger trials on treatment of this high-risk poor prognostic etiology, treatment is often anecdotal and depends on the experience of the clinician. The ULTIMA (Ultrasound Accelerated Thrombolysis of Pulmonary Embolism) trial has found intervention with USAT and unfractionated heparin to be superior to anticoagulation with unfractionated heparin alone in reversing RV dilatation, without a higher risk of major bleeding.13
Conclusion
Mobile thrombi in the MPA seen on TTE have yet to be reported in the literature. Our echocardiographic findings clearly show a mobile double-layered saddle embolus at the MPA bifurcation. This case shows the potential usefulness of TTE for guiding treatment decisions when there is a change in clinical status in patients with diagnosed MPA saddle pulmonary embolism. The discovery of a free-floating embolus in the MPA initiated expedited specialized treatment with catheter-based USAT. In a diagnosis that carries a poor prognosis and high risk of mortality, we were able to use clinical identification of initial treatment failure, aided by TTE, to achieve a positive outcome.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2017.09.011.
Supplementary Data
RV outflow view showing the double layer of emboli. Extension of the mobile embolus can be seen in the right pulmonary artery along with a proximal highly mobile serpentine component in the MPA.
A modified apical four-chamber view with focus on the right ventricle showing severe RV systolic dysfunction, akinesis of the mid to distal free wall, and hyperkinesis of the apical cap. The intraventricular septum can be seen impinging on the left ventricle.
Short-axis view at the midventricle showing left ventricular compression by impingement of the intraventricular septum. The large dilated right ventricle is also appreciated.
References
- 1.Chartier L., Béra J., Delomez M., Asseman P., Beregi J., Bauchart J. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999;99:2779–2783. doi: 10.1161/01.cir.99.21.2779. [DOI] [PubMed] [Google Scholar]
- 2.Kashif N. Floating thrombus in the right heart associated with pulmonary embolism: the role of echocardiography. Pak J Med Sci. 2015;31:233–235. doi: 10.12669/pjms.311.6219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mollazadeh R., Ostovan M.A., Abdi Ardekani A.R. Right cardiac thrombus in transit among patients with pulmonary thromboemboli. Clin Cardiol. 2009;32:E27–E31. doi: 10.1002/clc.20386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanjanauthai S., Couture L., Fissha M., Gentry M., Sharma G. Saddle pulmonary embolism visualized by transthoracic echocardiography. J Am Coll Cardiol. 2010;56:e21. doi: 10.1016/j.jacc.2009.10.097. [DOI] [PubMed] [Google Scholar]
- 5.Bilku R.S., Glennon P.E., Been M. Subacute massive pulmonary embolism diagnosed by transesophageal echocardiography. Circulation. 2007;116:e352–e353. doi: 10.1161/CIRCULATIONAHA.107.699132. [DOI] [PubMed] [Google Scholar]
- 6.Gabrielsen F., Schmidt A., Eggeling T., Hoeher M., Kochs M., Homback V. Massive main pulmonary artery embolism diagnosed with two-dimensional Doppler echocardiography. Clin Cardiol. 1992;15:545–546. doi: 10.1002/clc.4960150714. [DOI] [PubMed] [Google Scholar]
- 7.McConnell M.V., Solomon S.D., Rayan M.E., Come P.C., Goldhaber S.Z., Lee R.T. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78:469–473. doi: 10.1016/s0002-9149(96)00339-6. [DOI] [PubMed] [Google Scholar]
- 8.Driver S., Jouni H., McCully R.B. “Popcorn thrombus”: a case of massive intracardiac thromboembolism. Heart. 2014;100:520–521. doi: 10.1136/heartjnl-2013-304582. [DOI] [PubMed] [Google Scholar]
- 9.Barbetseas J., Bratsas A., Brill S., Chrysohoou C., Ioannidou M., Tzannos K. Main pulmonary artery thrombus. Hellenic J Cardiol. 2008;49:100–101. [PubMed] [Google Scholar]
- 10.Alpaslan M., Akgun G., Doven O., Oral D. Thrombus in the main pulmonary artery of a patient with thromboangiitis obliterans: observation by transthoracic echocardiography. Eur J Echocardiogr. 2001;2:139–140. doi: 10.1053/euje.2001.0071. [DOI] [PubMed] [Google Scholar]
- 11.Ulucay A., Aksoy M.F., Sahin E. Transthoracic echocardiography may show saddle pulmonary embolism. Neth Heart J. 2011;19:531. doi: 10.1007/s12471-011-0147-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torbicki A., Galie N., Covezzoli A., Rossi E., De Rosa M., Goldhaber S.Z. Right heart thrombi in pulmonary embolism: results from international cooperative pulmonary embolism registry. J Am Coll Cardiol. 2003;41:2245–2251. doi: 10.1016/s0735-1097(03)00479-0. [DOI] [PubMed] [Google Scholar]
- 13.Kucher N., Boekstegers P., Müller O.J., Kupatt C., Beyer-Westendorf J., Heitzer T. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014;129:479–486. doi: 10.1161/CIRCULATIONAHA.113.005544. [DOI] [PubMed] [Google Scholar]
- 14.Rose P.S., Punjabi N.M., Pearse D.B. Treatment of right heart thromboemboli. Chest. 2002;121:806–814. doi: 10.1378/chest.121.3.806. [DOI] [PubMed] [Google Scholar]
- 15.Kinney E.L., Wright R.J. Efficacy of treatment of patients with echocardiographically detected right-sided heart thrombi: a meta-analysis. Am Heart J. 1989;188:569–573. doi: 10.1016/0002-8703(89)90274-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
RV outflow view showing the double layer of emboli. Extension of the mobile embolus can be seen in the right pulmonary artery along with a proximal highly mobile serpentine component in the MPA.
A modified apical four-chamber view with focus on the right ventricle showing severe RV systolic dysfunction, akinesis of the mid to distal free wall, and hyperkinesis of the apical cap. The intraventricular septum can be seen impinging on the left ventricle.
Short-axis view at the midventricle showing left ventricular compression by impingement of the intraventricular septum. The large dilated right ventricle is also appreciated.