Abstract
Background:
Delayed anterior cruciate ligament (ACL) reconstruction may be associated with increased risk of subsequent knee joint damage and osteoarthritis (OA). The relationship between recurrent instability episodes and meniscal or cartilage damage after first-time ACL injury is unknown.
Purpose:
To assess the association between recurrent knee instability episodes and prevalence of meniscal lesions, cartilage damage, and OA after first-time ACL injury.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Six electronic databases were systematically searched using keywords and Medical Subject Heading terms. Studies selected were of English language, included original data, had a prospective design, and provided an outcome of recurrent instability and meniscal lesions, cartilage damage, or OA after first-time ACL injury. Adjusted odds ratios (ORs) were extracted or unadjusted ORs (95% CI) were calculated. PRISMA guidelines were followed, and 2 independent raters assessed study quality using Downs and Black criteria.
Results:
Of 905 potentially relevant studies, 7 were included. Sample sizes ranged from 43 to 541, and Downs and Black scores ranged from 2 to 12. Clinical and methodological heterogeneity precluded meta-analysis. Six studies reported a positive association between recurrent instability episodes and medial meniscal damage (OR range, 3.46 [95% CI, 1.24-9.99] to 11.56 [1.37-521.06]). The association between instability episodes and lateral meniscal or cartilage damage was inconsistent. No studies examined the association between instability episodes and OA.
Conclusion:
This systematic review provides preliminary evidence that recurrent instability episodes after first-time ACL injury may be associated with increased odds of medial meniscal damage. This highlights the importance of early diagnosis, education, and treatment for individuals with ACL injury, all of which must include a specific focus on the prevention and management of instability episodes. High-quality, prospective cohort studies are needed that assess the effects of diagnostic and treatment delay, recurrent instability episodes on secondary meniscal and cartilage damage, and OA after an initial ACL injury.
Keywords: injury prevention, knee, articular cartilage, meniscus, ACL
The incidence of knee osteoarthritis (OA) after anterior cruciate ligament (ACL) injury is high.43,47,51,54 This may be explained in part by the fact that an ACL-deficient knee is at increased risk for subsequent cartilage and meniscal damage.5,47 Recent systematic reviews that have investigated the relationship between time from ACL injury to ACL reconstruction (ACLR) and meniscal or cartilage damage18,46,57 have reported that prolonged time to ACLR is associated with increased risk of meniscal and cartilage damage. However, the link between prolonged time to ACLR and knee OA is less clear, with some studies identifying a positive association36,48 and others not.2,21,53 That said, few of these investigations have controlled for the number of recurrent instability episodes incurred after the initial ACL injury. The number of dislocations in the shoulder has been identified as a predictor of future glenohumeral OA,26 and this association may be paralleled in the knee.
Understanding the relationship between recurrent instability episodes and meniscal and/or cartilage damage in patients with ACL injury has significant implications for acute treatment pathways in terms of the secondary prevention of OA after ACL injury. Specifically, if an association between the number of recurrent instability episodes and meniscal or cartilage damage were identified, greater emphasis should be placed on the importance of avoiding conditions that are associated with instability episodes, regardless of primary treatment choice (surgical or nonsurgical). Surgery would be indicated for patients with, or at high risk of, recurrent instability episodes (participation in pivoting sports) to protect the meniscus and cartilage. Conversely, nonsurgical management in the form of rehabilitation, bracing, and lifestyle modification may be more appropriate for patients without, or at low risk of, instability episodes. Furthermore, this may influence timing of ACLR (especially in resource-limited health care environments) in that patients sustaining recurrent instability episodes might benefit by being prioritized for surgery over those who are better able to cope with their ACL-injured knee.
The purpose of this systematic review is to assess the relationship between recurrent knee instability episodes and the prevalence of meniscal lesions, cartilage damage, and OA after first-time ACL injury.
Methods
This review was conducted according to the 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement41 and was registered on the PROSPERO database (http://www.crd.york.ac.uk/prospero).
Data Sources and Search
Relevant studies were identified by searching 6 online databases, selected for their relevance to the topic, from inception to June 2016. These databases included MEDLINE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), EMBASE (Excerpta Medica databases), PubMed, Scopus, and the Cochrane Library. The Appendix outlines the combination of Medical Subject Heading and text words that were used for ACL, instability, meniscus, cartilage, and OA along with combinations of search terms that formed the final search strategy. Limits included English language and human ACL studies published in peer-reviewed journals. Articles were organized in an Excel sheet designed by VonVille.58 The number of references obtained from each search strategy for each database was recorded, and a running total was constructed. After accounting for duplication, the title and abstracts of all returned records were independently reviewed by 2 authors (1 orthopaedic surgeon and 1 medical student [M.S. and A.R.]) blinded to record authors and journal name. Prior to title and abstract review, these 2 authors independently screened a random sample of 86 titles and abstracts, in which they were blinded to authors and journal names, and reached moderate agreement regarding study relevance (Cohen kappa = 0.71) using an Excel workbook designed by VonVille.58 Finally, the same 2 authors independently reviewed the full text of all potentially relevant studies to determine final study selection. Consensus (first between the 2 reviewers and, if required, by a third author, an orthopaedic surgeon [D.O.]) regarding potentially relevant studies was reached on items where there was disagreement. The reference lists of selected studies were also hand-searched to identify relevant articles not found by this search strategy.
Study Selection
Studies were included if they investigated the relationship between an occurrence of recurrent instability after first-time ACL injury (yes/no or number of episodes) and prevalence of meniscal lesions, cartilage damage, and OA. Additional inclusion criteria included primary research with original data and analytic or interventional design. Exclusion criteria included animal studies and non-English or review articles.
Assessment of Study Quality
The methodological quality of included studies was appraised by 2 of 3 authors using the Downs and Black quality assessment tool.16 This checklist has been developed and recommended for use in systematic reviews of both randomized and nonrandomized studies.6 This tool consists of 27 questions that assess criteria for reporting, external validity, and internal validity (measurement and confounding). The highest score possible is 32.
Data Extraction and Synthesis
Data extraction was completed independently by 2 authors (1 orthopaedic surgeon and 1 medical student [M.S. and A.R.]) during the period July through September 2016 and was compared for accuracy using a Microsoft Excel spreadsheet designed by the authors for this purpose. Extracted data included study characteristics; patient demographics; definitions of recurrent instability episodes, meniscal lesions, and cartilage injuries; odds (odds ratio [OR] and 95% CI) of recurrent instability episodes, meniscal lesions, and cartilage damage; OA; and any functional outcomes. Covariates known to be potential risk factors for intra-articular knee injury, such as body mass index (BMI), activity level, time from injury to surgery (TFI), and sex, were also recorded.
For studies that did not report an OR, raw data were extracted to construct a 2 × 2 table with instability (yes/no) plotted against the outcome (yes/no), and Stata (StataCorp, 2013) was used to calculate an unadjusted OR with 95% CIs. In 1 study,49 1 cell of the 2 × 2 table contained zero. To allow calculation of an OR, each cell value was increased by 1, which is a described statistical technique to overcome this issue while biasing toward the null hypothesis.25
Results
Identification of Studies
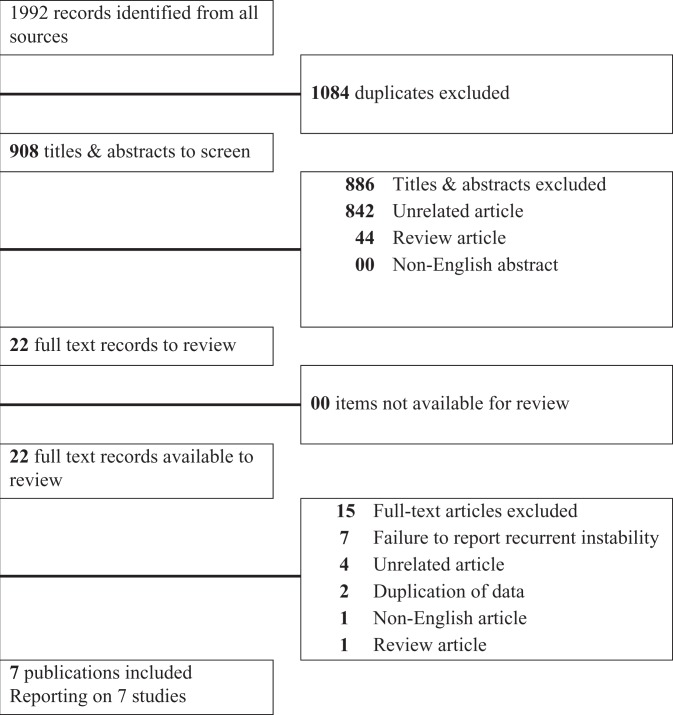
A summary of the study identification process is provided in Figure 1. The initial search strategy identified 1992 records; 1084 duplicates were removed, leaving 908 potentially relevant articles. Following removal of records that did not meet the inclusion criteria based on title and abstract review, the number of relevant articles was reduced to 22. After full-text review, 15 were excluded, leaving 7 studies for inclusion in the review.3,9,22,27,30,33,49 Articles were excluded at the full record review stage for the following reasons: failure to report recurrent instability (yes/no) in all patients (n = 7), unrelated article (n = 4), review article (n = 1), duplication of data (n = 2), and non-English article (n = 1). Of 2 papers by Kluczynksi et al,30,31 the earlier was selected because it presented the data in a nonstratified manner, which was consistent with the other studies in the review. Hand-searching of references of selected articles yielded no additional articles. Figure 1 provides a summary of the literature search and study selection process. Clinical and methodological heterogeneity (specifically involving the definition of recurrent instability episodes) precluded meta-analysis (Table 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for study selection process.
TABLE 1.
Summary of Findingsa
| Lead Author (Year) | Study Design | Level of Evidence | No. of Participants | Definition of Recurrent Instability | Definition of Meniscal and Cartilage Damage | OR of Any Tear (Medial, Lateral, Cartilage) With Recurrent Instability | OR of Medial Meniscal Tear With Recurrent Instability | OR of Lateral Meniscal Tear With Recurrent Instability | OR of Cartilage Injury With Recurrent Instability | Study Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|
| Anderson3 (2015) | Cohort study | 3 | 134 pediatric | Any instability episode subsequent to initial injury but before surgery | Operative reports and intraoperative images used to classify meniscal tears using the ISAKOS system. Chondral injuries were classified according to ICRS system. | Not reported, not calculable | OR 4.72; 95% CI, 1.43-15.6; P = .01 | OR 2.98; 95% CI, 0.99-8.96; P = .52 | Not reported, unadjusted calculated with Stata: OR 5.90; 95% CI, 1.78-20.09; P = .0004 | A delay in ACLR, history of any instability, and return to sports participation before reconstruction are associated with increased risk of meniscal and chondral injuries. |
| Funahashi22 (2014) | Cohort study | 3 | 71 pediatric | Reinjury indicated by significant encounters, which were characterized by new complaints of pain or swelling that were documented in record. The recording of instability or giving way was less consistent in the charts. | Operative reports used to classify meniscal injuries as present or not and reparable or not. Cartilage injuries were recorded as either present or not. | Not reported, unadjusted calculated with Stata: OR 4.57; 95% CI, 1.34-15.6; P = .015 | Not reported, unadjusted calculated with Stata: OR 3.21; 95% CI, 0.82-12.5; P = .093 | Not reported, unadjusted calculated with Stata: OR 1.56; 95% CI, 0.46-5.26; P = .47 | Not reported, unadjusted calculated with Stata: OR 2.70; 95% CI, 0.82-8.94; P = .10 | An increased number of significant encounters (≥5) was significantly associated with combined meniscal and cartilage injuries. |
| Lawrence33 (2011) | Cohort study | 3 | 70 pediatric | Subjective sense of instability noted as ≥1 episodes of “giving way” or “shifting” with activity | Operative reports and intraoperative images used to classify meniscal (required surgical intervention or not) and cartilage injuries (Outerbridge scores 0, 1 or 2, 3, 4) | Not reported, not calculable | OR 11.4; 95% CI, 1.31-99.1 | Reportedly no significant association, OR not calculable | Reportedly no significant association, OR not calculable | These data may influence many to favor early ACLR in this population. |
| Chen9 (2015) | Cohort study | 3 | 293 adults | Reinjury was defined as an explicit injury to the same knee introduced by joint instability after the initial injury and was recorded as “yes” or “no.” | Operative reports used to classify meniscal tears (full-thickness defect as determined by 2 surgeons) and cartilage (Outerbridge) injuries | OR 7.68; 95% CI, 3.24-18.22; P < .0001 | OR 10.9; 95% CI, 6.04-19.88; P < .0001 | OR 1.65; 95% CI, 0.98-2.76; P = .044 | OR 4.18; 95% CI, 2.09-8.35; P < .001 | An increased risk of meniscal tears (especially in the medial meniscus) was strongly associated with an active daily life and reinjury. |
| Kluczynski30 (2013) | Cohort study | 3 | 541 adults | No. of instability episodes subsequent to the initial injury but before surgery | Operative reports used to classify meniscal tears (no treatment or excision or repair) and cartilage (Outerbridge) injuries | Not reported, not calculable | Model 1: OR 3.53; 95% CI, 1.54-8.14. Model 2: OR 3.58; 95% CI, 1.55-8.28 | Reportedly no significant association, OR not calculable | Reportedly no significant association, OR not calculable | Data suggest focusing on number of instability episodes after the initial injury rather than the interval from injury to surgery as a more accurate predictor of subsequent medial meniscal tears. |
| Shelton49 (1997) | Case series | 4 | 43 adults (44 knees) | Buckling of the knee | Not defined | Not reported, unadjusted calculated with Stata: OR 14.63; 95% CI, 1.73-655.16 | Not reported, unadjusted calculated with Stata: OR 11.56; 95% CI, 1.37-521.06 | Not reported, unadjusted calculated with Stata: OR 4.68; 95% CI, 0.53-220.61 | Not reported, unadjusted calculated with Stata: OR 0.81; 95% CI, 0.039-51.57 | An athlete attempting to return to play early after an ACL injury is likely to experience recurrent buckling of the knee, which has significant potential for subsequent meniscal and cartilage injuries. |
| Indelicato27 (1985) | Case series | 4 | 100 adults | Episodes of buckling, giving out, or reinjury since the initial injury | Meniscal tears not defined; operative reports used to define cartilage defects as present (chondral fractures resulting in fragments) or not | Not reported, unadjusted calculated with Stata: OR 4.77; 95% CI, 1.42-18.32; P = .0038 | Not reported, unadjusted calculated with Stata: OR 3.46; 95% CI, 1.24-9.99; P = .0075 | Not reported, unadjusted calculated with Stata: OR 1.19; 95% CI, 0.48-3.01; P = .68 | Not reported, unadjusted calculated with Stata: OR 3.92; 95 % CI, 1.51-10.57, P = .0018 | Reinjury to the knee will likely enhance the incidence of meniscal tears and articular changes. |
aACLR, anterior cruciate ligament reconstruction; ICRS, International Cartilage Repair Society; ISAKOS, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine; OR, odds ratio.
Study Characteristics
Five of the 7 studies were considered cohort studies (level of evidence, 3)3,9,22,30,33 (Table 1). The other 2 were considered case series (level of evidence, 4).27,49 The median sample size was 100 (range, 43-541). Three of the studies investigated either pediatric or adolescent patient populations,3,22,33 while the 4 other studies involved adult patients.9,27,30,49 Four of the studies assessed the relationship between potential risk factors other than recurrent instability episodes and secondary intra-articular injury identified at the time of ACLR.3,9,30,33 No studies were found that assessed the association between recurrent instability episodes and OA.
The definition of recurrent instability varied among the studies (Table 1). Definitions included the following: any instability episode after first-time ACL injury and before surgery, reinjury (as indicated by significant encounters, which were characterized by new complaints of pain and swelling), subjective sense of instability (noted as 1 or more episodes of “giving way” or “shifting” with activity), explicit reinjury to the knee introduced by joint instability, and buckling episodes of the knee. Most authors dichotomized instability episodes as present or absent; however, 1 study established a cutoff of 5 or more significant clinical encounters (which the authors of that study attributed to recurrent instability episodes).22 The definition of meniscal and cartilage injury was not consistent but was more robust in studies that had higher Downs and Black scores in that established scoring criteria were used (Outerbridge; International Cartilage Repair Society; International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine) (Table 1).
Risk of Bias Within Studies
The median methodological quality for the 7 studies, based on Downs and Black criteria, was 9 out of 32 (range, 2-12), with only 3 studies scoring higher than 10 (Table 2). These scores indicate a risk of bias. Because the included studies were observational, 7 items (4, 8, 14, 19, 23, 24, and 27; totaling 10 points) were not applicable. The most consistent methodological weaknesses of the included studies were their observational design (lack of randomization, blinding, etc) and insufficient reporting of information about recruited patients as well as those lost to follow-up.
Table 2.
Downs and Black Scoring Chart
| Study Authors and Year | |||||||
|---|---|---|---|---|---|---|---|
| Anderson 2015 | Chen 2015 | Funahashi 2014 | Indelicato 1985 | Kluczynski 2013 | Lawrence 2011 | Shelton 1997 | |
| Study design | Cohort | Cohort | Cohort | Case series | Cohort | Cohort | Case series |
| Total score | 11 | 9 | 8 | 5 | 11 | 12 | 2 |
| Oxford level of evidence (2011) | 3 | 3 | 3 | 4 | 3 | 3 | 4 |
Risk of Bias Across Studies
A risk of bias was noted, because all included studies except 149 involved only patients who ultimately underwent ACLR. Underrepresented in this analysis are those patients with ACL injury who had not undergone ACLR.
Synthesis of Results
A summary of extracted data is provided in Table 1. All studies found that recurrent instability episodes were associated with some type of intra-articular damage diagnosed at time of surgery.
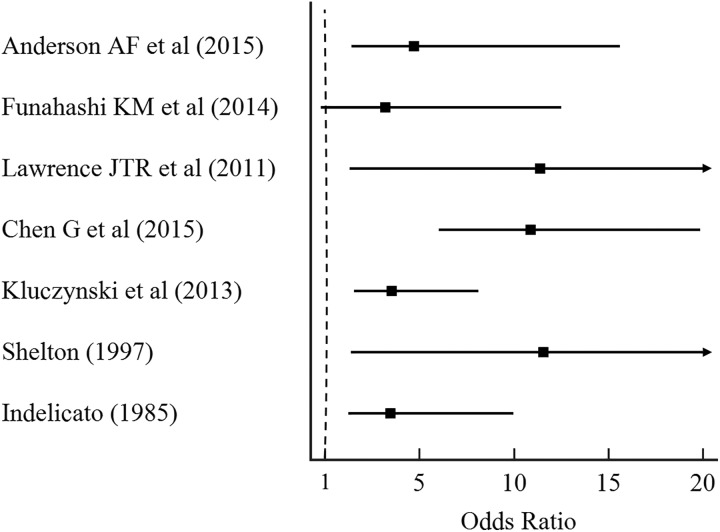
Adjusted OR (95% CI) for medial meniscal injury was reported in 4 of the 7 studies,3,9,30,33 and unadjusted ORs were calculable in the other 3 studies.22,27,49 Recurrent instability episodes were reportedly associated with medial meniscal tears in 6 of the 7 studies,3,9,27,30,33,49 with ORs from all 7 studies ranging from 3.21 (95% CI, 0.82-12.5) to 11.56 (95% CI, 1.37-521.06) (Figure 2). One study that recorded the actual number of instability episodes reported a linear relationship between number of instability episodes and medial meniscal tears (P = .01).30 One study reported that presence of instability episodes was predictive of having a high-grade (vs low-grade) medial meniscal tear.3 Another study found that the presence of instability episodes was predictive of necessity for meniscectomy.30 In this latter paper, sustaining more than 10 instability episodes reportedly doubled the odds of undergoing meniscectomy, although an OR was not reported.
Figure 2.
Odds ratios of medial meniscal injury with recurrent instability of individual studies.
Three of the 7 studies reported that recurrent instability episodes were associated with cartilage injury, with ORs ranging from 3.92 (95% CI, 1.51-10.57) to 5.90 (95% CI, 1.78-20.09).3,9,27 Two of the 7 studies reported that recurrent instability episodes were marginally associated with lateral meniscal injury, with ORs ranging from 1.65 (95% CI, 0.98-2.76) to 2.98 (95% CI, 0.99-8.96).3,9
Four studies examined the association between covariates (ie, TFI, sex, activity level, and BMI) and instability episodes on meniscal lesions and cartilage damage.3,9,30,33 One of these studies reported that instability episodes were associated with TFI and activity level.9 Another reported that TFI was associated with medial meniscal tears but that this association disappeared after adjustment for number of instability episodes.30
The only prospective study in the review reported rates of instability. Specifically, 60.3% (323/536) of patients awaiting ACLR had experienced 1 or more recurrent instability episodes, 13.1% (70/536) had experienced 1 episode, and 16.6% (89/536) had experienced more than 10 episodes; 39.7% (213/536) had not experienced an instability episode.30
Discussion
To our knowledge, this is the first systematic review examining the relationship between recurrent instability episodes and meniscal lesions or cartilage damage in individuals after a first-time ACL injury. The most important finding of this systematic review is that low-level evidence indicates that recurrent instability after first-time ACL injury is associated with increased odds of medial meniscal lesions. We found inconsistent evidence that recurrent instability is associated with lateral meniscal or cartilage damage in the same population.
This review brings to light the concept that instability episodes may be just as important in the development of medial meniscal damage, if not more so, than prolonged time from injury to surgery. This idea was first brought forward when Kluczynski et al30 controlled for instability episodes and found that time from injury to surgery was no longer predictive of medial meniscal damage. This finding sheds light on 2 areas of recent debate: timing of ACLR and early operative versus nonoperative management of patients with ACL injury.
Investigators have put forth considerable effort to determine the optimal period for ACLR. The majority, but not all, of these studies have found that with prolonged TFI, the likelihood of finding concomitant meniscal and cartilage damage during reconstruction increases.¶ Some authors, however, have reported acceptable results with delaying or avoiding ACLR, a finding that has garnered considerable debate.20,21,34,37 This dichotomy will be explored in several systematic reviews currently registered on PROSPERO, and the publication of these reviews will be a valuable addition to the literature on the topic. Whether prescribed treatment of an ACL tear involves reconstruction, delayed reconstruction, or rehabilitation, this review emphasizes that the goal of treatment should be to avoid further instability episodes. If nothing else, this systematic review highlights the importance of establishing an early diagnosis after an ACL tear, beginning timely care, and avoiding further instability episodes, with the aim of preventing secondary medial meniscal damage.
This information should affect the practice and management decisions of clinicians in several ways. Information regarding the number of instability episodes should be obtained early in the history of patients with ACL injury, as this may influence the likelihood of having medial meniscal damage. Educating the patient regarding the importance of avoiding subsequent instability episodes becomes an essential part of any treatment algorithm. Appropriately selecting surgical patients may be easier with this knowledge, because individuals with ACL deficiency who experience recurrent instability episodes may be at increased risk of secondary medial meniscal tears compared with such individuals who do not have recurrent instability. This finding may also increase the urgency of ACLR for patients experiencing recurrent instability episodes in resource-limited environments, as ACLR has been shown to reduce reinjury, secondary surgery, and meniscal tears.8 This effect is contingent upon the ACLR being able to eliminate recurrent instability episodes. For the long-term health of any ACL-deficient knee, avoidance of subsequent instability episodes should be a priority.
Although no long-term natural history study is available that reports on recurrent instability episodes in the ACL-deficient knee (as there is in the shoulder26), it is likely that knees with more recurrent instability episodes are at increased risk of developing OA. Failing to control for number of instability episodes may explain why prior studies have not found an association between delay to ACLR and OA.2,21,53,57 The association between medial meniscal loss and OA is clear,57 and this review demonstrates low-level evidence of the association between recurrent instability and medial meniscal injury. We recommend that future studies be designed to investigate the relationship between recurrent instability episodes and OA.
The role of the medial meniscus as a secondary restraint to anterior translation is further delineated by the findings of this review. The restraint against anterior translation of the tibia afforded by the medial meniscus has been described elsewhere.1,38,52 The role of recurrent instability in the development of varying types medial meniscal injury remains unclear. For example, it is not known whether recurrent instability increases the likelihood of occurrence of the medial meniscal ramp lesion, an entity described in recent literature.7,15 This review supports the assumption that in the setting of ACL deficiency, the medial meniscus, as a secondary restraint to anterior translation, is subject to an increased risk of injury.
Previous literature suggests that the lateral meniscus does not have a significant role in resisting anterior tibial translation. Levy et al35 performed a cadaveric study that involved sequential sectioning of the ACL and lateral meniscectomy. Their results suggest that the lateral meniscus does not act like a wedge resisting anterior translation in the same way that the medial meniscus does. In contrast, more recent literature suggests that the lateral meniscus may play a role in stabilizing the ACL-deficient knee during rotational loading. Shybut et al50 used a cadaveric model to show that an ACL-deficient knee with a posterior root tear of the lateral meniscus demonstrated significantly more rotational translation than an ACL-deficient knee with an intact lateral meniscus. With 5 of the studies in this review failing to identify an association between recurrent instability episodes and lateral meniscal tears,22,27,30,33,49 it may be that the more mobile lateral meniscus is less likely to be injured during recurrent instability episodes than the less mobile medial meniscus. This concept is supported by data showing lateral meniscal damage to be more common in an acute ACL injury and medial meniscal damage to be more common in a chronic ACL injury.12
Limitations
The findings of this systematic review are based on a synthesis and evaluation of the existing literature. As such, they are limited by the inadequacies and risk of bias of each individual study included. Prospective, well-designed, long-term studies are needed to further explore the implications of recurrent instability episodes on medial meniscal injury and OA.
The included studies in this review scored poorly on the Downs and Black questionnaire, which indicates a high risk of bias. Scores ranging from 2 to 12 indicate poor methodological quality, which must be kept in mind when the extracted data are analyzed.
Another limitation of this systematic review is the underrepresentation of patients who are treated nonsurgically, because most of the patients in these studies underwent ACLR. It is difficult to comment on the nonsurgical group, but it seems intuitive that conservatively managed patients who have recurrent instability episodes are similarly at higher risk for medial meniscal tears.
Because most of the studies included in this review were retrospective, definitively establishing the directionality of the association between the number of recurrent instability episodes and meniscal and cartilage damage is difficult. One could argue that knees with meniscal and cartilage damage may be more prone to further instability episodes or greater symptoms of pain and swelling, which then cause patients to seek treatment. Clarifying this issue will require prospective studies that examine images before and after the occurrence of recurrent instability episodes.
Recommendations
Information regarding the number of instability episodes should be obtained from patients with ACL injury, and education regarding the importance of avoiding subsequent instability episodes should be provided.
Conclusion
This systematic review has identified low-level evidence that recurrent instability after an initial ACL injury is associated with increased odds of medial meniscal damage. High-quality, prospective cohort studies are needed that further assess the effect of diagnostic and treatment delay, as well as recurrent instability episodes, on secondary meniscal and cartilage damage and OA after an initial ACL injury.
Appendix
Search Strategy
anterior cruciate ligament.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
(instability episode* or recurren* or re-injury or reinjury or subjective instability).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
(menisc* or cartilage or osteoarthritis or outcome*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
1 and 2 and 3.
Results
| Database | Date Searched | No. of Results |
|---|---|---|
| MEDLINE | June 7, 2016 | 321 |
| CINAHL | June 7, 2016 | 166 |
| EMBASE | June 7, 2016 | 363 |
| PubMed | June 7, 2016 | 552 |
| Scopus | June 7, 2016 | 505 |
| Cochrane Library | June 7, 2016 | 85 |
| Total | 1992 |
References
- 1. Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament–deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39(10):2187–2193. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC. Long-term results of anterior cruciate ligament reconstruction using bone–patellar tendon–bone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy. 2012;28(8):1114–1123. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 4. Anstey DE, Heyworth BE, Price MD, Gill TJ. Effect of timing of ACL reconstruction in surgery and development of meniscal and chondral lesions. Phys Sportsmed. 2012;40(1):36–40. [DOI] [PubMed] [Google Scholar]
- 5. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966–2973. [DOI] [PubMed] [Google Scholar]
- 6. Centre for Reviews and Dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. Layerthorpe, York, UK: York Publishing Services; 2008. [Google Scholar]
- 7. Chahla J, Dean CS, Moatshe G, et al. Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop J Sports Med. 2016;4(7):2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chalmers PN, Mall NA, Moric M, et al. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292–300. [DOI] [PubMed] [Google Scholar]
- 9. Chen G, Tang X, Li Q, Zheng G, Yang T, Li J. The evaluation of patient-specific factors associated with meniscal and chondral injuries accompanying ACL rupture in young adult patients. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):792–798. [DOI] [PubMed] [Google Scholar]
- 10. Chhadia AM, Inacio MCS, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39(9):1894–1899. [DOI] [PubMed] [Google Scholar]
- 11. Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87(12):1639–1642. [DOI] [PubMed] [Google Scholar]
- 12. Cipolla M, Scala A, Gianni E, Puddu G. Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees: classification, staging and timing of treatment. Knee Surg Sports Traumatol Arthrosc. 1995;3(3):130–134. [DOI] [PubMed] [Google Scholar]
- 13. de Roeck NJ, Lang-Stevenson A. Meniscal tears sustained awaiting anterior cruciate ligament reconstruction. Injury. 2003;34(5):343–345. [DOI] [PubMed] [Google Scholar]
- 14. Demiraq B, Aydemir F, Danis M, Ermutlu C. Incidence of meniscal and osteochondral lesions in patients undergoing delayed anterior cruciate ligament reconstruction. Acta Orthop Traumatol Turc. 2011;45(5):348–352. [DOI] [PubMed] [Google Scholar]
- 15. DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 16. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40(9):2128–2133. [DOI] [PubMed] [Google Scholar]
- 18. Fabricant PD, Lakomkin N, Cruz AI, Spitzer E, Lawrence JTR, Marx RG. Early ACL reconstruction in children leads to less meniscal and articular cartilage damage when compared with conservative or delayed treatment. J ISAKOS. 2016;1:10–15. [Google Scholar]
- 19. Fok AWM, Yau WP. Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):928–933. [DOI] [PubMed] [Google Scholar]
- 20. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 21. Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346:F232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Funahashi KM, Moksnes H, Maletis GB, Csintalan RP, Inacio MC, Funahashi TT. Anterior cruciate ligament injuries in adolescents with open physis: effect of recurrent injury and surgical delay on meniscal and cartilage injuries. Am J Sports Med. 2014;42(5):1068–1073. [DOI] [PubMed] [Google Scholar]
- 23. Ghodadra N, Mall NA, Karas V, et al. Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg. 2013;26(3):185–193. [DOI] [PubMed] [Google Scholar]
- 24. Granan L, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med. 2009;37(5):955–961. [DOI] [PubMed] [Google Scholar]
- 25. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 Updated March 2011 http://handbook.cochrane.org/. Accessed June 30, 2016. [Google Scholar]
- 26. Hovelius L, Saeboe M. Neer Award 2008: Arthropathy after primary anterior shoulder dislocation—223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg. 2009;18(3):339–347. [DOI] [PubMed] [Google Scholar]
- 27. Indelicato PA, Bittar ES. A perspective of lesions associated with ACL insufficiency of the knee: a review of 100 cases. Clin Orthop Relat Res. 1985;198:77–80. [PubMed] [Google Scholar]
- 28. Joseph C, Pathak SS, Aravinda M, Rajan D. Is ACL reconstruction only for athletes? A study of the incidence of meniscal and cartilage injuries in an ACL-deficient athlete and non-athlete population: an Indian experience. Int Orthop. 2008;32(1):57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kennedy J, Jackson MP, O’Kelly P, Moran R. Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. J Bone Joint Surg Br. 2010;92(3):362–366. [DOI] [PubMed] [Google Scholar]
- 30. Kluczynski MA, Marzo JM, Bisson LJ. Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med. 2013;41(12):2759–2765. [DOI] [PubMed] [Google Scholar]
- 31. Kluczynski MA, Marzo JM, Rauh MA, Bernas GA, Bisson LJ. Sex-specific predictors of intra-articular injuries observed during anterior cruciate ligament reconstruction. Orthop J Sports Med. 2015;3(2):2325967115571300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Krutsch W, Zellner J, Baumann F, Pfeifer C, Nerlich M, Angele P. Timing of anterior cruciate ligament reconstruction within the first year after trauma and its influence on treatment of cartilage and meniscus pathology. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):418–425. [DOI] [PubMed] [Google Scholar]
- 33. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. [DOI] [PubMed] [Google Scholar]
- 34. Levy BA, Krych AJ, Dahm DL, Stuart MJ. Treating ACL injuries in young moderately active adults. BMJ. 2013;346:F963. [DOI] [PubMed] [Google Scholar]
- 35. Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71(3):401–406. [PubMed] [Google Scholar]
- 36. Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(12):2595–2603. [DOI] [PubMed] [Google Scholar]
- 37. Lohmander LS, Roos HP, Roos EM, Ranstam J, Frobell RB. Authors’ response to editorial by Levy and colleagues on treating ACL injuries in young moderately active adults. BMJ. 2013;346:F2082. [DOI] [PubMed] [Google Scholar]
- 38. Lorbach O, Kieb M, Herbort M, Weyers I, Raschke M, Engelhardt M. The influence of the medial meniscus in different conditions on anterior tibial translation in the anterior cruciate deficient knee. Int Orthop. 2015;39(4):681–687. [DOI] [PubMed] [Google Scholar]
- 39. Magnussen RA, Pedroza AD, Donaldson CT, Flanigan DC, Kaeding CC. Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: is patient age an important factor? Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2029–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Michalitsis S, Vlychou M, Malizos KN, Thriskos P, Hantes ME. Meniscal and articular cartilage lesions in the anterior cruciate ligament–deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):232–239. [DOI] [PubMed] [Google Scholar]
- 41. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 42. Murrell GAC, Maddali S, Horovitz L, Oakley SP, Warren RF. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med. 2001;29(1):9–14. [DOI] [PubMed] [Google Scholar]
- 43. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
- 44. Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1438–1444. [DOI] [PubMed] [Google Scholar]
- 45. Ralles S, Agel J, Obermeier M, Tompkins M. Incidence of secondary intra-articular injuries with time to anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(6):1373–1379. [DOI] [PubMed] [Google Scholar]
- 46. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 47. Sanders TL, Pareek A, Kremers HM, et al. Long-term follow-up of isolated ACL tears treated without ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):493–500. [DOI] [PubMed] [Google Scholar]
- 48. Seon JK, Song EK, Park SJ. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006;30(2):94–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shelton WR, Barrett GR, Dukes A. Early season anterior cruciate ligament tears: a treatment dilemma. Am J Sports Med. 1997;25(5):656–658. [DOI] [PubMed] [Google Scholar]
- 50. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. [DOI] [PubMed] [Google Scholar]
- 51. Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2009;18(3):304–311. [DOI] [PubMed] [Google Scholar]
- 52. Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–408. [DOI] [PubMed] [Google Scholar]
- 53. Streich NA, Zimmermann D, Bode G, Schmitt H. Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency: a retrospective matched-pair long-term follow-up. Int Orthop. 2011;35(4):607–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Suter LG, Smith SR, Katz JN, et al. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adulthood. Arthritis Care Res (Hoboken). 2017;69(2):201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tandogan RN, Taser O, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):262–270. [DOI] [PubMed] [Google Scholar]
- 56. Tayton E, Verma R, Higgins B, Gosal H. A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay. Knee Surg Sports Traumatol Arthrosc. 2009;17(1):30–34. [DOI] [PubMed] [Google Scholar]
- 57. van Meer BL, Meuffels DE, van Eijsden WA, Verhaar JA, Bierma-Zeinstra SM, Reijman M. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review. Br J Sports Med. 2015;49(15):975–983. [DOI] [PubMed] [Google Scholar]
- 58. VonVille H. Excel workbooks for systematic reviews. http://libguides.sph.uth.tmc.edu/excel_workbook_home. Accessed June 9, 2016.
- 59. Yoo JC, Ahn JH, Lee SH, Yoon YC. Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med. 2009;37(8):1478–1483. [DOI] [PubMed] [Google Scholar]
- 60. Yuksel HY, Erkan S, Uzun M. The evaluation of intraarticular lesions accompanying ACL ruptures in military personnel who elected not to restrict their daily activities: the effect of age and time from injury. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1139–1147. [DOI] [PubMed] [Google Scholar]