Abstract
Background:
Prediction of rehospitalization in patients treated with antipsychotics is important for identifying patients in need of additional support to prevent hospitalization. Our aim was to identify factors that predict rehospitalization in patients treated with antipsychotics at discharge from a psychiatric hospital.
Methods:
Adult patients suffering from schizophrenia, psychotic or bipolar I disorders who had been hospitalized in a psychiatric hospital for ⩾7 days and were treated with oral antipsychotics at discharge were included. The main outcome was rehospitalization within 6 months after discharge. A prediction model for rehospitalization was constructed including: patient/disease and medication characteristics, patients’ beliefs about medicines, and healthcare-professional-rated assessment for all patients. The patients were stratified by diagnosis (schizophrenia and nonschizophrenia). Area under the receiver operating characteristic curve (AUCROC) was also assessed.
Results:
A total of 87 patients were included and 33.3% of them were rehospitalized within 6 months after discharge. The variables that predicted rehospitalization were duration of hospitalization, patients’ attitude towards medicine use, and healthcare-professional-rated assessment with an AUCROC of 0.82. Rehospitalization for patients with schizophrenia could be predicted (AUCROC = 0.71) by the Global Assessment of Functioning score, age, and harm score. Rehospitalization was predicted (AUCROC = 0.73) for nonschizophrenia patients with, for example rehospitalization predicted by the nurse.
Conclusions:
Rehospitalization was predicted by a combination of variables from the patient/disease and medication characteristics, patients’ attitude towards medicine use, and healthcare-professional-rated assessment. These variables can be assessed relatively easily at discharge to predict rehospitalization within 6 months.
Keywords: Rehospitalization, BMQ, antipsychotic adherence, psychotic disorder, health care professionals’ expectation, prediction models
Introduction
There is ample evidence for the effectiveness of antipsychotics in the treatment of psychotic and bipolar I disorders. However, relapse rates are high in patients discharged from hospital with antipsychotic medication, leading to episodes of acute psychosis/mania and (re)hospitalizations.1–15 Up to 34% of the patients have a relapse within 6 months after hospitalization for a psychotic episode.12 This has a high impact on quality of life of patients and may lead to considerable economic costs.1–15 About half of the patients with psychotic or bipolar I disorders are (partially) nonadherent with their antipsychotic treatment; either by not initiating the medication, skipping dosages, or discontinuing treatment.2,11–14,16 A 2.4 times greater probability of hospitalization has been reported in those who are less than 80% adherent to antipsychotic therapy.17
It would be useful to be able to early identify patients at higher risk for rehospitalization in order to provide these patients with additional support. Previous studies have shown that patient, disease and treatment characteristics including age, duration of hospitalization, and severity of disease can be predictors for rehospitalization, as well as type of treatment and early nonadherence with antipsychotic medication.18,19 Healthcare professionals may have insights into patients’ adherence, which may be used to predict future success of therapy.20 It is unknown whether patients’ attitude towards medication therapy is a predictor for relapse in patients being treated with antipsychotics. Patients’ attitude towards medication use has two important dimensions: necessity and concern. Necessity reflects the perceived need for use of the medication by the patient, while concern measures the fear of negative outcomes from use of the medication, such as side effects, and addiction.13,21
The aim of this study was to predict the risk of rehospitalization in patients treated with antipsychotic medication discharged from a psychiatric hospital, using patient, disease and treatment characteristics, patients’ beliefs and attitudes towards antipsychotic medication, and healthcare professionals’ expectations towards patients’ adherence and probability of rehospitalization. These factors were assessed at discharge.
Methods
Setting
This study was performed in nine departments of Altrecht Mental Health Care (Altrecht), a conglomeration of five psychiatric hospitals in The Netherlands serving a total population of 800,000 inhabitants.22 Date of discharge was considered as index date. The study period included the 6 months following the index date or until patients were rehospitalized (considered end of follow up) whichever came first. The study was approved by the Altrecht’s scientific board (2013–17/oz1309/ck) and performed in accordance with The Federation of Dutch Medical Scientific Societies’ code of conduct for the use of data in health research.
Design and study population
A prospective, observational study was performed in which patients were followed from discharge up to 6 months or until rehospitalization, whichever came first. The study population included adult patients (⩾18 years) with a psychotic or bipolar I disorder (according to DMS-IV TR) that were treated with oral antipsychotics at discharge (ATC: N05A excluding lithium) and who were hospitalized for 7 days or longer.12 The patients used only oral antipsychotics, thus the patients did not use depot antipsychotics. If patients were rehospitalized within 7 days of discharge, we considered this hospitalization as a part of the index hospitalization.12,18,23 Patients discharged between May 2013 and April 2014 were eligible for participation in the study and received information about the study from a nurse or a researcher (KE) prior to being discharged from Altrecht. Those patients who gave informed consent filled in general questions before discharge regarding sex, age, their community pharmacy, and the Beliefs about Medicines Questionnaire (BMQ-specific, Appendix 1). Besides the questions for the patients, the nurse and the physician involved in patients’ treatment both filled in a healthcare professionals’ questionnaire on patients’ expected adherence, probability of rehospitalization and therapeutic relationship, which is set out in Appendix 2.
Outcome
The main clinical outcome was (time to) psychiatric rehospitalization within 6 months of discharge. Patients were considered to be rehospitalized when the time between discharge and rehospitalization was at least 7 days.12,18,23
Patient and disease characteristics
Data on patient and disease characteristics were collected from the hospital files.14,24–26
Medication characteristics
Data on medication characteristics were obtained from the hospital files.27 Medication-related information from the patients’ questionnaire investigated were:
Whether patients picked up their medication at their community pharmacy themselves (yes/no);
If someone was always available to remind patients to take medication (yes/no/now and then);
If somebody else was giving patients their medication when they were not taking it (yes/no).
Patients’ attitude towards medicine use
The attitude towards antipsychotic medication was assessed with the BMQ-specific, which is divided into the necessity and the concerns subscales. The necessity subscale, consisting of five statements, measures patients’ beliefs about the necessity to take antipsychotic medication, while the concerns subscale, consisting of six statements, measures patients’ concerns about their antipsychotic medication (Appendix 1).21 The total scores of the two subscales were summed, divided by the total number of statements in the scale and then multiplied by five. Patients were divided into four different belief groups: accepting (necessity score 15–25, concerns score 5–15), indifferent (necessity score 5–15, concerns score 5–15), skeptical (necessity score 5–15, concerns score 15–25), and ambivalent (necessity score 15–25, concerns score 15–25).21,28 General beliefs about medication were measured using the BMQ-general scale consisting of the subscales harm and overuse. Both subscales consist of four statements. The scores of the four statements for harm and overuse were summed and used as a continuous variable.
Finally, initiation of antipsychotic medication after discharge (initiated within 7 days or >7 days) was assessed based on information from the patients’ community pharmacy medication history. Patients were expected to get their first antipsychotic prescription dispensed within 7 days post discharge. In The Netherlands, patients do not receive antipsychotic medication at discharge to use at home but are expected to pick up their medication at a community pharmacy. However, when the discharge was just before or during the weekend, the patient could get medication for a maximum duration of 3 days. Furthermore, if the patient refilled their antipsychotic medication before admission, and still had enough antipsychotic medication at home, this was taken into account. The information about initiation of antipsychotic medication was used to visualize the belief groups in Figure 1.
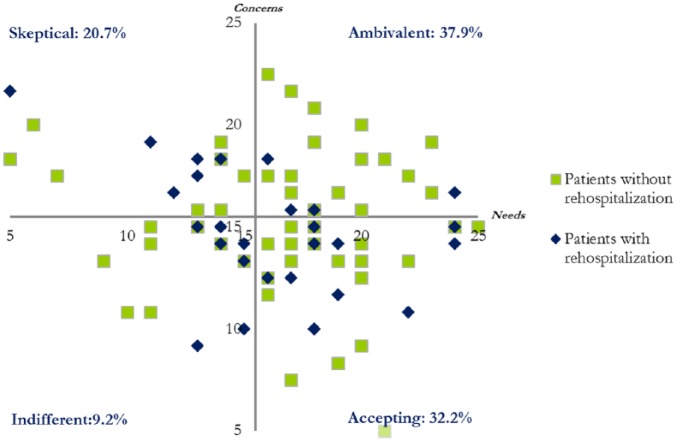
Figure 1.
This scatter plot shows the distribution of patient’s scores of the BMQ (Beliefs about Medicine Questionnaire) specific statements in the four belief groups: accepting, ambivalent, skeptical, and indifferent.
The x axis represents the scores of the necessity subscale and the y axis the scores of the concerns subscale.
Healthcare-professional-rated assessment
Furthermore, physicians and nurses (healthcare professionals) involved in patients’ treatment prior to discharge filled in a questionnaire including questions on:
Whether the healthcare professional had asked the patient during admission whether he/she was adherent to their antipsychotics (yes/no/do not know anymore);
Whether, during admission, they had discussed adherence to antipsychotic medication with the patient (yes/no/do not know anymore);
If they could predict whether the patient would use antipsychotic medication after discharge (yes/no/I do not know);
Estimating the patient’s adherence to antipsychotics after discharge (in %, scale 0–100%);
The prediction on risk on rehospitalization (scale 0–100%, categorized as: ⩽50% and >50%);
How they considered their patient–healthcare professional/therapeutic relationship (good or moderate/bad).
Data analysis
First, the association between the variables and rehospitalization were investigated in a univariate analysis using Cox proportional hazards. Second, the variables were analyzed using backward selection. Starting with all variables in the model for each group, variables were subsequently excluded from the model when p value ⩾ 0.20. The multivariate prediction model was also separately analyzed for patients with and without schizophrenia. Relative risks (RRs) were measured as hazard ratios with 95% confidence intervals (95% CI) using Cox proportional hazards. The data analysis was performed using SPSS for Windows, version 20.0, IBM Software, Chicago, USA. The area under the receiver operating characteristic (ROC) curve (AUCROC) was assessed for the multivariate prediction model by using the library ‘risksetROC’ in statistical software R version 3.1.2, University of Auckland in Auckland, New Zealand.29 A risk score was calculated for the multivariate prediction model by summing all regression coefficients and then adding 8. Subsequently, the risk score was categorized in tertiles to obtain three equally divided groups with proportion of patients rehospitalized.30 Finally, for the internal consistency of the different scales of the BMQ, Cronbach’s alpha test was performed.
Results
A total of 87 patients gave informed consent and were included in this study; 16 patients refused to participate. Patients’ mean age was 38.4 years [standard deviation (SD): 12.1], and most of them had a previous hospitalization (89.7%), as shown in Table 1.
Table 1.
Demographic and patient/disease characteristics at discharge.
| Characteristics | n | %/SD/range |
|---|---|---|
| Total | 87 | |
| Mean age, years (SD) | 38.4 | 12.1 |
| Sex (%) | ||
| Male | 52 | 59.8% |
| Diagnosis of psychotic disorder (%) | ||
| Brief psychotic disorder | 18 | 20.7% |
| Schizophrenia | 34 | 39.1% |
| Schizoaffective disorder | 13 | 14.9% |
| Bipolar disorder I | 22 | 25.3% |
| Duration of baseline hospitalization (days, median, range) | 48 | 7–371 |
| 7–29 days | 28 | 32.2% |
| 30–60 days | 31 | 35.6% |
| ⩾61 days | 28 | 32.2% |
| Number of antipsychotic agents used at discharge (%) | ||
| One antipsychotic agent | 69 | 79.3% |
| ⩾Two antipsychotic agents | 18 | 20.7% |
| Type of antipsychotic medication (%) | ||
| Second generation | 65 | 74.7% |
| First generation | 13 | 15.0% |
| Combination | 9 | 10.3% |
| Department at discharge (%) | ||
| Open unit | 73 | 83.9% |
| Closed unit | 14 | 16.1% |
| First admission (%) | ||
| Yes | 9 | 10.3% |
| No | 78 | 89.7% |
| Residential situation (%) | ||
| Alone | 40 | 46.0% |
| Living with others | 45 | 51.7% |
| Other/homeless | 2 | 2.3 |
| Mean GAF score (SD) | 46.0 | 11.7 |
| History of substance use | ||
| No | 64 | 73.6% |
| Yes | 23 | 26.4% |
SD, standard deviation; GAF, Global Assessment of Functioning scale.
The mean score on the necessity subscale of the BMQ-specific was 16.6 (SD: 4.2), 15.2 (SD: 3.3) on the concern subscale. Internal consistency of the subscales was variable; α = 0.81 for necessity, α = 0.57 for concerns, α = 0.62 for overuse, α = 0.57 for harm. Figure 1 shows the distribution of the patients in the four groups for the BMQ-specific scale. Most patients were either in the ambivalent (37.9%) or in the accepting (32.2%) group. 18.2% of the ambivalent patients were rehospitalized, 42.9% of the accepting, 50.0% of the skeptical, and 25.0% of the indifferent. A sum of 71.3% (62) of the patients refilled their oral antipsychotic medication within 7 days after discharge, 21.8%19 did not refill within 7 days and for 6.9%6 of the patients it was unknown. Among the patients that refilled antipsychotic medication within 7 days after discharge, 37.1% were ambivalent, 35.4% were accepting, 19.4% were skeptical, and 8.1% were indifferent. Among the patients that did not refill their antipsychotic medication within 7 days after discharge, 47.7% were ambivalent, 26.3% skeptical, 15.8% accepting, and 10.5% indifferent.
Rehospitalization
A total of 29 (33.3%) patients were rehospitalized within 6 months, with a median time to rehospitalization of 32 days (range: 12–181 days). A total of 12.6% of the patients were rehospitalized within 1 month after discharge, and 21.8% within 3 months.
The results of the univariate analysis for the association of the variables and rehospitalization are shown in Table 2. Of the patient/disease characteristics, only RR for duration of hospitalization (RR = 0.99; 95% CI: 0.98–0.998) and age (RR = 1.02; 95% CI: 0.99–1.05) had a p < 0.20. For the medication characteristics, patients that picked up their own medication at their community pharmacy had a higher risk of rehospitalization compared with patients that got their medication delivered or picked up by others (RR = 1.45; 95% CI: 0.87–2.39). Patients who were not reminded to take their antipsychotic medication (RR = 3.32, 95% CI: 1.13–9.78), and patients that were now and then reminded (RR = 2.41; 95% CI: 0.68–8.54) by someone else had a higher risk of rehospitalization compared with patients that were always reminded. Among the beliefs groups, skeptical patients had a threefold higher risk of rehospitalization than ambivalent patients (RR = 3.38; 95% CI: 1.20–9.50). Increase of 1 unit for the harm score gave an RR of 0.92 (95% CI: 0.81–1.04) and for the overuse score, an RR of 1.02 (95% CI: 0.90–1.15). Of the healthcare-professional-rated assessment variables, patients for whom a nurse predicted a risk of >50% for rehospitalization had a twofold higher risk of rehospitalization compared with patients with a nurse prediction of ⩽50% for rehospitalization (RR = 2.13; 95% CI: 1.03–4.42).
Table 2.
Univariate analysis for the variables of patient/disease and medication characteristics, patients’ attitude towards medicine use and healthcare-professional-rated assessment.
| Variables | n | % rehospitalized | HR (95% CI) |
|---|---|---|---|
| Overall | 87 | 33.3 | |
| Patient and disease characteristics | |||
| Duration of index hospitalization | 0.99 (0.98–1.00)* | ||
| Diagnosis of psychotic disorder | |||
| Schizophrenia | 34 | 44.1 | Reference |
| Schizoaffective disorder | 13 | 23.1 | 0.49 (0.14–1.71) |
| Brief psychotic disorder | 18 | 33.3 | 0.66 (0.26–1.70) |
| Bipolar disorder I | 22 | 22.7 | 0.44 (0.16–1.20)* |
| Sex | |||
| Male | 52 | 34.6 | Reference |
| Female | 35 | 31.4 | 0.99 (0.47–2.01) |
| Age (years) | 1.02 (0.99–1.05)* | ||
| Residential situation | |||
| Alone | 40 | 40.0 | Reference |
| Living with others | 45 | 26.7 | 0.62 (0.29–1.31) |
| Other/unknown | 2 | 50.0 | 1.13 (0.15–8.57) |
| History of substance use | |||
| No | 64 | 34.4 | Reference |
| Yes | 23 | 30.4 | 0.82 (0.35–1.92) |
| First admission | |||
| Yes | 9 | 33.3 | Reference |
| No | 78 | 33.3 | 1.03 (0.31–3.40) |
| GAF score | 1.01 (0.98–1.05) | ||
| Department at discharge | |||
| Open unit | 73 | 32.9 | Reference |
| Closed unit | 14 | 35.7 | 1.01 (0.38–2.64) |
| Medication characteristics | |||
| Number of AP used at discharge+ | |||
| One antipsychotic agent | 69 | 36.2 | Reference |
| ⩾Two antipsychotic agents | 18 | 22.2 | 0.56 (0.20–1.61) |
| Type of AP | |||
| First generation | 13 | 30.8 | 0.72 (0.25–2.06) |
| Second generation | 65 | 38.5 | Reference |
| Combination of both | 9 | 0.0 | NA |
| Number of comedications at discharge | 1.03 (0.99–1.15) | ||
| Patients themselves picked up medication at community pharmacy | |||
| No | 21 | 19.0 | Reference |
| Yes | 66 | 37.9 | 1.45 (0.87–2.39)* |
| Someone was always available to remind patients to take medication | |||
| Yes | 26 | 15.4 | Reference |
| No | 43 | 44.2 | 3.32 (1.13–9.78)** |
| Now and then | 18 | 33.3 | 2.41 (0.68–8.54)* |
| Somebody else was giving patients their medication when they were not taking it | |||
| Yes | 18 | 22.2 | Reference |
| No | 68 | 36.8 | 1.68 (0.59–4.84) |
| Unknown | 1 | 0.0 | NA |
| Patients’ attitude towards medication use | |||
| Belief groups | |||
| Ambivalent | 33 | 18.2 | Reference |
| Skeptical | 18 | 50.0 | 3.38 (1.20–9.50)** |
| Indifferent | 8 | 25.0 | 1.50 (0.30–7.44) |
| Accepting | 28 | 42.9 | 2.62 (0.98–7.00)* |
| BMQ-general | |||
| Harm score+ | 0.92 (0.81–1.04)* | ||
| Overuse score+ | 1.02 (0.90–1.15) | ||
| Healthcare-professional-rated assessment | |||
| Physician asked whether patient was adherent to AP | |||
| Yes | 62 | 37.1 | Reference |
| No | 24 | 25.0 | 0.66 (0.27–1.61) |
| Do not know anymore | 1 | 0.0 | |
| Nurse asked whether patient was adherent to AP | |||
| Yes | 64 | 37.5 | Reference |
| No | 22 | 22.7 | 0.58 (0.22–1.52) |
| Do not know anymore | 1 | 0.0 | NA |
| Physician discussed AP adherence during admission | |||
| Yes | 71 | 32.4 | Reference |
| No | 15 | 33.3 | 1.06 (0.40–2.79) |
| Do not know anymore | 1 | 100.0 | NA |
| Nurse discussed AP adherence during admission | |||
| Yes | 65 | 38.5 | Reference |
| No | 21 | 19.0 | 0.45 (0.16–1.30)* |
| Do not know anymore | 1 | 0.0 | NA |
| Physician predicted patient would use AP after discharge | |||
| Yes | 72 | 37.5 | Reference |
| No | 7 | 0.0 | NA |
| I do not know | 8 | 25.0 | 0.63 (0.15–2.65) |
| Nurse predicted patient would use AP after discharge | |||
| Yes | 73 | 35.6 | Reference |
| No | 7 | 42.9 | 1.28 (0.39–4.22) |
| I do not know | 7 | 0.0 | NA |
| AP adherence prediction by physician (%) | 1.04 (0.99–1.02) | ||
| AP adherence prediction by nurse (%) | 1.00 (0.99–1.02) | ||
| Rehospitalization prediction by physician (%) | |||
| Prediction ⩽50% | 60 | 35.0 | Reference |
| Prediction >50% | 27 | 29.6 | 0.77 (0.34–1.75) |
| Rehospitalization prediction by nurse (%) | |||
| Prediction ⩽50% | 58 | 25.9 | Reference |
| Prediction >50% | 29 | 48.3 | 2.13 (1.03–4.42)** |
| Therapeutic relationship according to physician | |||
| Good | 60 | 36.7 | Reference |
| Moderate/bad | 27 | 25.9 | 0.71 (0.30–1.66) |
| Therapeutic relationship according to nurse | |||
| Good | 63 | 31.7 | Reference |
| Moderate/bad | 24 | 37.5 | 1.18 (0.54–2.59) |
p < 0.2; **p < 0.05.
Continuous variable.
AP, antipsychotics; BMQ, Beliefs about Medicines Questionnaire; CI, confidence interval; GAF, Global Assessment of Functioning scale; HR, hazard ratio; NA, not applicable.
Table 3 shows the results of the multivariate analysis of the multivariate prediction model. Several variables remained in the multivariate prediction model predicting rehospitalization for all patients (Table 3). For example, duration of hospitalization gave an RR of 0.99 (95% CI: 0.97–1.00) per day. The diagnosis of bipolar disorder I resulted in the lowest RR of 0.12 (95% CI: 0.02–0.73) in the diagnosis category. Patients with a prior hospitalization had a lower risk of rehospitalization (RR of 0.70; 95% CI: 0.01–0.66) when compared with patients that were hospitalized for the first time. Number of comedications gave an RR of 1.29 (95% CI: 1.09–1.52) for each comedication used at discharge. Patients that had nobody to give them their medication when they were not taking it had an RR of 0.08 (95% CI: 0.10–0.64) compared with patients that received medication from somebody.
Table 3.
Results of the multivariate prediction models.
| Variables | |
|---|---|
| Duration of index hospitalization | 0.99 (0.97–0.998)** |
| Diagnosis | |
| Schizophrenia | Reference |
| Brief psychotic disorder | 0.83 (0.19–3.57) |
| Schizoaffective disorder | 0.89 (0.16–5.12) |
| Bipolar disorder I | 0.12 (0.02–0.73)** |
| First admission | |
| Yes | Reference |
| No | 0.70 (0.01–0.66)** |
| Department at discharge | |
| Open unit | Reference |
| Closed unit | 0.30 (0.05–1.77)* |
| Type of AP | |
| First generation | 0.15 (0.03–0.88)** |
| Second generation | Reference |
| Combination of both | NA |
| Number of comedications at discharge+ | 1.29 (1.09–1.52)** |
| Someone was always available to remind patients to take medication | |
| Yes | Reference |
| No | 11.89 (1.30–108.93)** |
| Now and then | 1.84 (0.19–18.21) |
| Somebody else was giving patients their medication when they were not taking it | |
| Yes | Reference |
| No | 0.08 (0.10–0.64)** |
| Unknown | NA |
| Belief groups | |
| Ambivalent | Reference |
| Skeptical | 6.30 (1.18–33.70)** |
| Indifferent | 7.23 (0.64–82.19)* |
| Accepting | 0.96 (0.18–5.20) |
| BMQ-general | |
| Harm score+ | 0.75 (0.58–0.98)** |
| Overuse score+ | 1.18 (0.98–1.42)* |
| Physician asked whether patient was adherent to AP | |
| Yes | Reference |
| No | 0.06 (0.07–0.55)** |
| Do not know anymore | NA |
| Nurse asked whether patient was adherent to AP | |
| Yes | Reference |
| No | 0.07 (0.11–0.43)** |
| Do not know anymore | NA |
| Therapeutic relationship according to physician | |
| Good | Reference |
| Moderate/bad | 3.27 (0.77–13.89)* |
| Rehospitalization prediction by nurse (%) | 1.04 (1.00–1.07)** |
| AUCROC (6 months) | 0.82 |
p < 0.2; **p < 0.05.
Continuous variable.
AP, antipsychotics; AUCROC, receiver operating characteristics for area under the curve; BMQ, Beliefs about Medicines Questionnaire; NA, not applicable.
Skeptical patients had higher risk of rehospitalization (RR = 6.30; 95% CI: 1.18–33.70) compared with ambivalent patients. Patients that had a moderate/bad relationship with their physician had a higher risk for rehospitalization (RR = 3.27; 95% CI: 0.77–13.89) compared with those that had a good relationship with their physician. When the nurse predicted rehospitalization, it gave an RR of 1.04 (95% CI: 1.00–1.07). AUCROC for the multivariate prediction model was 0.82.
Risk score of rehospitalization
The risk score was calculated for the multivariate prediction model. This model was transformed in a scoring rule based on the regression coefficient for the selected variables (Table 4). The total score (0–16.5) was assessed for all the patients and can be considered as a measure for prediction of rehospitalization at discharge. Patients were categorized in tertiles based on their score. Proportion of rehospitalized patients was assessed for the three categories being 20.6% in the patients with a risk score of 0.0 to 10.0, 20.6% in the patients with a risk score of 10.1–12.3, and 58.6% in the patients with a risk score of 12.4–16.5 (Table 7). Patients in the upper tertile had an RR of 3.34 (95% CI: 1.31–8.49) for rehospitalization and in the middle tertile, an RR of 0.96 (95% CI: 0.31–2.96) compared with patients in the lower tertile (Table 7).
Table 4.
Regression coefficient of the predictors obtained from model 1 + 2 + 3 + 4 with assigned score.
| Predictor | Regression coefficient = score |
|---|---|
| Duration of index hospitalization | −0.014 |
| Diagnosis | |
| Schizophrenia | Reference |
| Brief psychotic disorder | −0.113 |
| Schizoaffective disorder | −0.190 |
| Bipolar disorder I | −2.115 |
| First admission | |
| Yes | Reference |
| No | −2.66 |
| Department at discharge | |
| Open unit | Reference |
| Closed unit | −1.21 |
| Type of AP | |
| First generation | −1.88 |
| Second generation | Reference |
| Combination of both | NA |
| Number of comedications at discharge | 0.25 |
| Someone was always available to remind patients to take medication | |
| Yes | Reference |
| No | 2.48 |
| Now and then | 0.61 |
| Somebody else was giving patients their medication when they were not taking it | |
| Yes | Reference |
| No | −2.53 |
| Unknown | NA |
| Belief groups | |
| Ambivalent | Reference |
| Skeptical | 1.84 |
| Indifferent | 1.98 |
| Accepting | −0.043 |
| BMQ-general | |
| Harm score | −0.29 |
| Overuse score | 0.16 |
| Physician asked whether patient was adherent to AP | |
| Yes | Reference |
| No | −2.81 |
| Do not know anymore | NA |
| Nurse asked whether patient was adherent to AP | |
| Yes | Reference |
| No | −2.70 |
| Do not know anymore | NA |
| Therapeutic relationship according to physician | |
| Good | Reference |
| Moderate/bad | 1.19 |
| Rehospitalization prediction by nurse (%) | |
| Prediction ⩽50% | Reference |
| Prediction >50% | 0.034 |
The score is obtained by rounding each regression coefficient to nearest integer, summing them and adding 8 to the summed risk score.
AP, antipsychotic medication; BMQ, Beliefs about Medicines Questionnaire; NA, not applicable.
Table 7.
Distribution of patients rehospitalized within risk score category.
| Risk score category1 | Total n of patients | Patients rehospitalized (%)2 | Median time to rehospitalization (range) | HR (95% CI) |
|---|---|---|---|---|
| 0.0–10.0 | 29 | 20.6 | 24 (15–60) | Reference |
| 10.1–12.3 | 29 | 20.6 | 32 (21–181) | 0.96 (0.31–2.96) |
| 12.4–16.5 | 29 | 58.6 | 42 (12–165) | 3.34 (1.31–8.49)* |
| Overall | 87 | 33.3 | 32 (12–181) |
p < 0.05.
The calculated of the total risk score was rounded to nearest integer.
Proportion of patients rehospitalized within each risk score category.
CI, confidence interval; HR, hazard ratio.
Rehospitalization in patients with and without schizophrenia
The prediction models were analyzed for both patients with and without schizophrenia (Table 5 and 6). Rehospitalization was best predicted for patients with schizophrenia by Global Assessment of Functioning (GAF) score, age, and harm score (Table 5). The highest RR for rehospitalization was for age (RR = 1.07; 95% CI: 1.02–1.13). The prediction model had an AUCROC of 0.71.
Table 5.
Results of the multivariate prediction models for patients with schizophrenia.
| Variables | |
|---|---|
| GAF score | 1.06 (1.00–1.12)** |
| Age | 1.07 (1.02–1.13)** |
| Harm score | 0.79 (0.62–1.02)* |
| AUCROC (6 months) | 0.71 |
p < 0.2; **p < 0.05.
AUCROC, receiver operating characteristics for area under the curve; GAF, Global Assessment of Functioning scale.
Table 6.
Results of the multivariate prediction models for patients without schizophrenia.
| Variables | |
|---|---|
| GAF score | 0.96 (0.92–1.01)* |
| Residential situation | |
| Alone | Reference |
| Living with others | 0.26 (0.075–0.91)** |
| Other/unknown | 0.78 (0.085–7.24) |
| Rehospitalization prediction by nurse (%) | |
| Prediction ⩽50% | Reference |
| Prediction >50% | 3.82 (1.02–14.39)** |
| AP adherence prediction by physician (%) | 1.03 (1.00–1.06)** |
| AUCROC (6 months) | 0.73 |
p < 0.2; **p < 0.05.
AP, antipsychotics; AUCROC, receiver operating characteristics for area under the curve; GAF, Global Assessment of Functioning scale.
Rehospitalization was best predicted for patients without schizophrenia by GAF score, residential situation, and rehospitalization prediction by both the physician and the nurse (Table 6). The highest RR was for patients for whom the nurse predicted a rehospitalization >50% (RR = 3.82; 95% CI: 1.02–14.39) and adherence to antipsychotic predicted by the physician (RR = 1.03; 95% CI: 1.00–1.06). The prediction model had an AUCROC of 0.73.
Discussion
The aim of this study was to identify patients with psychotic or bipolar I disorders treated with antipsychotics at risk for rehospitalization within 6 months from discharge. Rehospitalization was best predicted by a combination of variables from patient/disease and medical characteristics, patients’ beliefs about medicines, and healthcare-professional-rated assessment, all variables that are relatively easily obtainable at discharge.
Compared with the literature
Skeptical patients had higher risk of rehospitalization compared with ambivalent patients. When the nurse predicted rehospitalization, it gave an RR of 1.04 (95% CI: 1.00–1.07). AUCROC for the multivariate prediction model was 0.82.
In our study, we found the strongest predictors to be having no one to remind patients to take medication, belief groups (indifferent or skeptical) about their antipsychotic medication, and patients having a moderate/bad relationship with their physician (according to the physician).
This is in line with Lang and colleagues, who found that hospitalization in patients with schizophrenia could be predicted with history of substance abuse, new starters of antipsychotic medication, adherence, and number of comedications, including anticholinergic use.19 Our results are also in line with Perkinson and colleagues who reported that caregivers’ rated assessment of medication adherence was correlated with how patients refilled their medication. They also measured necessity of treatment and the ones that believed need for treatment was low were more likely to be rehospitalized also when other questionnaires were used. This is in line with our results that patients indifferent or skeptical towards their medication were at a greater risk of rehospitalization.20,31
History of substance use did not remain in our prediction models, while it remained in the prediction model of Lang and colleagues. Our predictors may differ from the study of Lang and colleagues due to several differences in study design. We included variables related to patient/disease and medication characteristics, patients’ beliefs about medicines, and healthcare-professional-rated assessment while Lang and colleagues only included patient/disease and medication characteristics. Furthermore, Lang and colleagues included only patents with at least two refills for antispychotic drugs, included both in- and outpatients and had any hospitalization, general as well as psychiatric, as main outcome while we included patients that were discharged and had psychiatric rehospitalization as an outcome. Psychiatric patients have a higher prevalence of somatic disease, thus both higher somatic as well as psychiatric hospitalization rates are expected.27 Due to their inclusion criteria patients without any refill after discharge were missed and their results cannot be applied for these our patients. Besides this, their study population consisted of two different groups, namely inpatients and outpatients. The risk of (re)hospitalization for these patients could be different, because risk of hospitalization is highest within a month after discharge as seen in this study and also reported by Zilber and colleagues18
In other studies, physicians overestimated their patients’ adherence to pharmacotherapy. However, in our study as well in the study of Perkins and colleagues, healthcare professionals were able to predict adherence, as well as risk of rehospitalization.20,31–36 Of the healthcare professionals, nurses were better able to predict rehospitalization in patients without schizophrenia than physicians in our study. This could be because nurses have a more intensive contact with patients during the hospitalization than physicians and patients are more likely to share their thoughts about their disease and treatment with the nurses.
In our study, we found that the multivariate prediction model had the strongest ability for predicting rehospitalization (AUCROC = 0.82). It will give an overall reflection of patients’ disease and characteristics, and treatment, including antipsychotic medication, number of comedications, and patient–healthcare-professional-rated assessment. Furthermore, the patients’ attitude towards medicine use and the healthcare professionals’ questionnaires are short; thus, it takes little effort to complete these. The beliefs groups that remained in the prediction models were based on the BMQ-specific. Completing the questionnaires can be implemented in the patients’ discharge procedure to identify patients at a higher risk of rehospitalization at discharge. Future research is needed to assess whether stratification is needed for patients with and without schizophrenia.
Strengths
To the best of our knowledge, this is the first study where predictors of rehospitalization are identified combining patient/disease and medication characteristics, patients’ beliefs about medicines, and healthcare-professional-rated assessment. The questionnaires were completely filled in by everyone involved in this study. Patients filled in the questionnaire by themselves. If patients did not understand a question/statement, one of the researchers (KE) explained and assisted patients. For the first refill after discharge, stockpiling (antipsychotic refill before hospitalization) was taken into account. Another strength of this study is that psychiatric rehospitalizations in the whole region were included and not only rehospitalization in the five included hospitals. Both the physician and the nurse who were involved in patients’ treatment before discharge were involved in this study. Medication characteristics included information on number of comedications, antipsychotic initiation after discharge, whether patients refilled their medication themselves, if somebody else was giving patients their medication when they were not taking it. Thus, medication characteristics and medication use during and after hospitalization were taken into account. Even though other studies made prediction models, they did not calculate a risk score based on all the variables.
Limitations
Although this was a prospective study without any intervention in patients’ treatment, healthcare professionals might have spent more attention to antipsychotic adherence after discharge. This could have resulted in a better monitoring of adherence resulting in less rehospitalizations. Nonetheless, 33.3% of the patients were rehospitalized in the 6 months following discharge, which is comparable with what previous studies have reported.37–39 Patients were told at inclusion that there were no right or wrong answers, the results would not be discussed with their psychiatrist or anyone else, and the results would be processed anonymously in this study. Despite these facts, patients may have filled in socially desirable answers. Although the power for the prediction model in all the patients was 0.80, power decreased when patients were stratified by having diagnosis of schizophrenia or other diagnosis.
Conclusion
Rehospitalization was best predicted by a combination of variables from the patient/disease and medication characteristics, patients’ attitude towards medicine use, and healthcare-professional-rated assessment. These variables are relatively easily obtainable to predict rehospitalization within 6 months after discharge. Risk scores can be assessed at discharge to identify patients with a higher risk for rehospitalization.
Acknowledgments
The authors are thankful to the patients, Altrecht Mental Health Care, and the community pharmacies for their contribution in this study. Also, we thank Miss D Yazir for helping with the collection of the medication history, and Dr Md Jamal Uddin for helping with the statistical analyses.
Appendix 1. Basic questionnaire for the patients and patients’ attitudes towards medicine use (BMQ)
- (1) How do you receive your medication?
- I pick it up at the pharmacy (patients themselves)
- The pharmacy delivers my medication to my home
- My friends/family pick it up at the pharmacy for me
- Professionals/people from my assisted living facility pick it up from the pharmacy for me
- I get depot/Semap/Acemap from the nurses at Altrecht
- I get my oral medication from the nurses at Altrecht
- (2) What is your living situation?
- I live alone and am independent
- I live alone with housing counseling
- I live with my family/partner
- I live with other people and get assistance
- (3) Do people remind you to take your medication?
- Yes
- No
- Now and then
- (4) When you do not take your medication, do you receive your medication from someone else?
- Yes
- No
BMQ-specific [scored on a 5-point Likert scale; 1 (strongly disagree), 2 (disagree), 3 (uncertain), 4 (agree) or 5 (strongly agree)].
(5) My health, at present, depends on my medicines
(6) Having to take medicines worries me
(7) My life would be impossible without medication
(8) I sometimes worry about the long-term effects of my medicines
(9) Without my medicines, I would be very ill
(10) My medicines are a mystery to me
(11) My health in the future will depend on my medicines
(12) My medicines disrupt my life
(13) I sometimes worry about becoming too dependent on my medicines
(14) My medicines protect me from becoming worse
(15) These medicines have unpleasant side effects
BMQ-general [scored on a 5-point Likert scale 1 (strongly disagree), 2 (disagree), 3 (uncertain), 4 (agree) or 5 (strongly agree)].
(16) Physicians prescribe too many medicines
(17) People who take medicines should stop their treatment for a while, now and again
(18) Most medicines are addictive
(19) Natural remedies are safer than medicines
(20) Medicines do more harm than good
(21) All medicines are poisons
(22) Physicians place too much trust in medicines
(23) If physicians had more time with patients, they would prescribe fewer medicines
Appendix 2. Questionnaire for the healthcare professionals
- (1) How are you involved in the treatment of the patient (physician)?
- Clinical psychiatrist (during the last admission)
- Ambulatory psychiatrist
- Physician (not in training to become a specialist)
- Psychiatrist trainee
- Other: ………………………………… … … ….
(2) How do you estimate the patient’s antipsychotic adherence after discharge? (0% bad; 100% very good) …….%
- (3) Have you discussed adherence to antipsychotics with this patient during the admission?
- Yes
- No
- I do not know
- (4) Have you asked the patient during the admission whether he/she is adherent?
- Yes
- No
- I do not know
- (5) How do you assess your professional relationship with this patient?
- Good
- Moderate
- Bad
- (6) Predict: is this patient going to use his/her antipsychotic medication following discharge?
- Yes
- No
- I do not know
- (7) Predict: do you think that this patient will continue his/her antipsychotic medication during the 6 months after discharge?
- Yes
- No
- I do not know
(8) How long do you expect this patient to continue his/her antipsychotic medication after discharge? ……. months
(9) Do you think that this patient will be rehospitalized in the next 6 months? (0% no rehospitalization; 100% rehospitalization) …….%
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Heshu Abdullah-Koolmees, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands.
Helga Gardarsdottir, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands; Department of Laboratory and Clinical Pharmacy, University Medical Centre Utrecht, Utrecht, The Netherlands.
Lotte A. Minnema, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands
Kamjar Elmi, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands.
Lennart J. Stoker, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands Brocacef Hospital Pharmacy, Maarssen, The Netherlands.
Judith Vuyk, Altrecht Mental Health Care, Utrecht, The Netherlands.
Laurette E. Goedhard, Altrecht Mental Health Care, Utrecht, The Netherlands
Toine C. G. Egberts, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands Department of Laboratory and Clinical Pharmacy, University Medical Centre Utrecht, Utrecht, The Netherlands.
Eibert R. Heerdink, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, The Netherlands Department of Laboratory and Clinical Pharmacy, University Medical Centre Utrecht, Utrecht, The Netherlands; Altrecht Mental Health Care, Utrecht, The Netherlands.
References
- 1. Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 2008; 8: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Weiden PJ, Kozma C, Grogg A, et al. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv 2004; 55: 886–891. [DOI] [PubMed] [Google Scholar]
- 3. Law MR, Soumerai SB, Ross-Degnan D, et al. A longitudinal study of medication nonadherence and hospitalization risk in schizophrenia. J Clin Psychiatry 2008; 69: 47–53. [DOI] [PubMed] [Google Scholar]
- 4. dosReis S, Johnson E, Steinwachs D, et al. Antipsychotic treatment patterns and hospitalizations among adults with schizophrenia. Schizophr Res 2008; 101: 304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fenton WS, Kane JM. Clinical challenges in the psychopharmacology of schizophrenia. Schizophr Bull 1997; 23: 563–565. [DOI] [PubMed] [Google Scholar]
- 6. Sun SX, Liu GG, Christensen DB, et al. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin 2007; 23: 2305–2312. [DOI] [PubMed] [Google Scholar]
- 7. Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull 2008; 34: 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tiihonen J, Haukka J, Taylor M, et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry 2011; 168: 603–609. [DOI] [PubMed] [Google Scholar]
- 9. Jung SH, Kim WH, Choi HJ, et al. Factors affecting treatment discontinuation and treatment outcome in patients with schizophrenia in Korea: 10-year follow-up study. Psychiatry Invest 2011; 8: 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Robinson DG, Woerner MG, Alvir JM, et al. Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophr Res 2002; 57: 209–219. [DOI] [PubMed] [Google Scholar]
- 11. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry 2002; 63: 892–909. [DOI] [PubMed] [Google Scholar]
- 12. Laan W, Does Y, Sezgi B, et al. Low treatment adherence with antipsychotics is associated with relapse in psychotic disorders within six months after discharge. Pharmacopsychiatry 2010; 43: 221–224. [DOI] [PubMed] [Google Scholar]
- 13. Jonsdottir H, Friis S, Horne R, et al. Beliefs about medications: measurement and relationship to adherence in patients with severe mental disorders. Acta Psychiatr Scand 2009; 119: 78–84. [DOI] [PubMed] [Google Scholar]
- 14. Boden R, Brandt L, Kieler H, et al. Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Res 2011; 133: 36–41. [DOI] [PubMed] [Google Scholar]
- 15. Ohmori T, Ito K, Abekawa T, et al. Psychotic relapse and maintenance therapy in paranoid schizophrenia: a 15 year follow up. Eur Arch Psychiatry Clin Neurosci 1999; 249: 73–78. [DOI] [PubMed] [Google Scholar]
- 16. Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 2012; 73: 691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Valenstein M, Copeland LA, Blow FC, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care 2002; 40: 630–639. [DOI] [PubMed] [Google Scholar]
- 18. Zilber N, Hornik-Lurie T, Lerner Y. Predictors of early psychiatric rehospitalization: a national case register study. Isr J Psychiatry Relat Sci 2011; 48: 49–53. [PubMed] [Google Scholar]
- 19. Lang K, Meyers JL, Korn JR, et al. Medication adherence and hospitalization among patients with schizophrenia treated with antipsychotics. Psychiatr Serv 2010; 61: 1239–1247. [DOI] [PubMed] [Google Scholar]
- 20. Perkins DO, Gu H, Weiden PJ, et al. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry 2008; 69: 106–113. [DOI] [PubMed] [Google Scholar]
- 21. Verhoef TI, Redekop WK, Bouvy ML, et al. Beliefs about medicines in Dutch acenocoumarol and phenprocoumon users. Br J Clin Pharmacol 2014; 78: 422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Altrecht MHC. Annual Report 2013 of Altrecht/Jaarverslag. 2013: 19–94, www.altrecht.nl (2013, accessed 7 October 2017).
- 23. Reutfors J, Brandt L, Stephansson O, et al. Antipsychotic prescription filling in patients with schizophrenia or schizoaffective disorder. J Clin Psychopharmacol 2013; 33: 759–765. [DOI] [PubMed] [Google Scholar]
- 24. Olfson M, Mechanic D, Hansell S, et al. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv 2000; 51: 216–222. [DOI] [PubMed] [Google Scholar]
- 25. Gorwood P. Factors associated with hospitalisation of patients with schizophrenia in four European countries. Eur Psychiatry 2011; 26: 224–230. [DOI] [PubMed] [Google Scholar]
- 26. Hugenholtz GW, Stolker JJ, Heerdink ER, et al. Short-acting parenteral antipsychotics drive choice for classical versus atypical agents. Eur J Clin Pharmacol 2003; 58: 757–760. [DOI] [PubMed] [Google Scholar]
- 27. Abdullah-Koolmees H, Gardarsdottir H, Stoker LJ, et al. Prevalence of medication use for somatic disease in institutionalized psychiatric patients. Pharmacopsychiatry 2013; 46: 274–280. [DOI] [PubMed] [Google Scholar]
- 28. Aikens JE, Nease DE, Jr, Nau DP, et al. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann Fam Med 2005; 3: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Heagerty PJ, Zheng Y. Survival model predictive accuracy and ROC curves. Biometrics 2005; 61: 92–105. [DOI] [PubMed] [Google Scholar]
- 30. Bouvy ML, Heerdink ER, Leufkens HG, et al. Predicting mortality in patients with heart failure: a pragmatic approach. Heart 2003; 89: 605–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perkins DO, Johnson JL, Hamer RM, et al. Predictors of antipsychotic medication adherence in patients recovering from a first psychotic episode. Schizophr Res 2006; 83: 53–63. [DOI] [PubMed] [Google Scholar]
- 32. Byerly M, Fisher R, Whatley K, et al. A comparison of electronic monitoring versus clinician rating of antipsychotic adherence in outpatients with schizophrenia. Psychiatry Res 2005; 133: 129–133. [DOI] [PubMed] [Google Scholar]
- 33. Byerly MJ, Thompson A, Carmody T, et al. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatr Serv 2007; 58: 844–847. [DOI] [PubMed] [Google Scholar]
- 34. Remington G, Kwon J, Collins A, et al. The use of electronic monitoring (MEMS) to evaluate antipsychotic compliance in outpatients with schizophrenia. Schizophr Res 2007; 90: 229–237. [DOI] [PubMed] [Google Scholar]
- 35. Zeller A, Taegtmeyer A, Martina B, et al. Physicians’ ability to predict patients’ adherence to antihypertensive medication in primary care. Hypertens Res 2008; 31: 1765–1771. [DOI] [PubMed] [Google Scholar]
- 36. Miller LG, Liu H, Hays RD, et al. How well do clinicians estimate patients’ adherence to combination antiretroviral therapy? J Gen Intern Med 2002; 17: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry 2008; 7: 148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother 2011; 9: 11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stuffken R, van Hulten RP, Heerdink ER, et al. The impact of hospitalisation on the initiation and long-term use of benzodiazepines. Eur J Clin Pharmacol. 2005; 61(4): 291–5. [DOI] [PubMed] [Google Scholar]