Abstract
Introduction:
The knee arthroplasty is the best option for patients with advanced osteoarthritis who have failed all other conservative options, but regrettably many patients fail to undergo surgery due to co-morbidities or other reasons. So, new alternative modes are always in demand for these patients.
Methods:
The ultrasound-guided radiofrequency ablation (RFA) of all the genicular nerves of knee joint was done in patients with grade III and IV osteoarthritis of knee joint, with severe pain (numerical rating scale (NRS) > 7) who had failed conservative management and intra-articular injections after a positive genicular nerve block with local anaesthetics. The demographics, pain intensity measured in NRS, Oxford Knee Score (OKS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and quality of life measured by 36-Item Short Form Health Survey (SF-36) questionnaire was measured at baseline and at regular intervals.
Results:
The average age of the patients was 61.50 ± 6.75 years. There was significant improvement in pain intensity at rest, movement and on weight bearing from 8.75 ± 0.5, 9.0 ± 0.0, and 9.0 ± 0.0 at baseline to 2.38 ± 0.51, 3.75 ± 0.46, and 4.13 ± 0.35 at 1 month and 3.13 ± 0.64, 4.38 ± 0.51, and 4.63 ± 0.51 at 6 months after the procedure, respectively (p value <0.05). The OKS had improved from 7.75 ± 1.25 at baseline to 28.88 ± 2.53 and 28.13 ± 1.80 at 1 and 6 months, respectively, after the procedure (p value <0.05). The WOMAC score had also improved significantly from 77.75 ± 4.34 at baseline to 38.38 ± 5.82 and 39.25 ± 5.12 at 1 and 6 months, respectively (p value <0.05). There was also significant improvement in the quality of life after the procedure (p value <0.05).
Conclusion:
Ultrasound-guided RFA of genicular nerves of knee joint is a good alternative option for patients who are having severe pain and disability from knee osteoarthritis and gives a long-lasting pain relief for more than 6 months.
Keywords: Knee osteoarthritis, genicular nerves, ultrasound guidance, radiofrequency ablation
Key points.
The literature on radiofrequency ablation of genicular nerves of knee for osteoarthritis of knee is limited. The earlier studies were done only on the three genicular nerves; whereas in our study, we had done the RF ablation on all the branches of the genicular nerves. This study will provide a level-IV evidence that ultrasound-guided radiofrequency ablation of the genicular nerves is safe and effective in treating knee pain from osteoarthritis of knee joint not responding to conservative modalities of treatment and who wish to avoid surgery.
Introduction
Osteoarthritis of knee joint is one of the most common disease conditions with advanced age and leads to considerable morbidity in terms of pain, stiffness, limitation in functions, disturbance in sleep and psychological disturbance.1–4
There are many options of treatment for knee osteoarthritis available. Among them, pharmacotherapy is useful for most of the patients with a few patients not tolerating them either because of adverse effects or co-morbidities of the patients.5 For these types of patients, there are other non-surgical interventions are accessible, which includes intra-articular steroid or hyaluronic acid or platelet-rich plasma, botulinum toxin, acupuncture, periosteal stimulation therapy, balneotherapy/spa therapy, biomechanical interventions (knee braces, knee sleeves and foot orthoses), cane (walking stick), crutches, electrotherapy/neuromuscular electrical stimulation, exercise (land and water based), strength training and weight management, etc.6–11 These therapies help in relieving the pain and other symptoms to a certain limited extent and are not much helpful in advanced osteoarthritis.6–11 Although knee arthroplasty is the best option for the patients with advanced disease, many patients cannot undergo surgery either because of multiple co-morbidities or the patients do not prefer to undergo surgery.12 Hence, there is always a search for new modalities of treatment for patients who are not a good candidate for surgery or refuse to undergo surgery. The radiofrequency neurotomy of the genicular branches is also used to alleviate pain from knee osteoarthritis. The earlier studies were mostly done with fluoroscopy guidance which depends on the virtual anatomical location of the genicular nerves and were regrettably done for three genicular nerves instead of seven genicular nerves.13–15 There are few recent studies, for instance, on ultrasound-guided radiofrequency neurotomy of genicular nerves showing good relief of knee pain; but sadly, in all these studies, also the neurotomy were done on three genicular nerves only.16–18 However, recently, the technique of blocking all the genicular nerves for acute knee pain with the help of ultrasound has been described in literature.19
In our case series, we had done radiofrequency ablation (RFA) of seven genicular nerves under ultrasound guidance in eight patients with severe pain from advanced knee osteoarthritis after two successive positive diagnostic genicular blocks.
Methods
This is a retrospective case series of eight patients with grade III or IV osteoarthritis of knee with severe pain (NRS > 7) in Asian Institute of Medical Sciences, Faridabad, India over a period of 12 months, from September 2014 to August 2015. These patients did not respond to conservative treatment with medications and non-invasive methods and also not a candidate for knee arthroplasty due to multiple co-morbidities. The patients had underwent ultrasound-guided RFA of all the genicular nerves following two successive positive diagnostic ultrasound-guided genicular nerve block given after a gap of 1 week. The procedures were performed only after obtaining a written informed consent for the procedure and its subsequent publication explaining the procedure, potential benefits and the risks associated with the procedure, such as anaesthesia dolorosa, deafferentation pain and motor weakness.
Diagnostic genicular nerve block
All patients were given diagnostic genicular block in the operation theatre under all aseptic conditions. The patient was positioned supine for all the injections except the posterior genicular nerve block when the patient was positioned prone. The monitoring was done as per American Society of Anesthesiologists (ASA) standard and an intra-venous cannulation was also done. The affected knee joint is cleaned with antiseptic solution and covered with sterile drapes. The genicular nerves were visualized with the help of high-frequency (6–13 Hz) linear USG probe (M-Turbo® Ultrasound System; SonoSite International, Washington, DC). A systemic scan was done on the superior, inferior, lateral, medial and posterior aspects of the knee joint and the genicular nerves are identified in the following way.
Superior medial genicular nerve
SMGN arises from nerve to vastus medialis which itself is a branch of the femoral nerve. To visualize SMGN, the ipsilateral hip was externally rotated to position the medial aspect of knee joint facing superiorly, and the USG transducer was aligned transversely over the medial femoral epicondyle and moved proximally to the level of adductor tubercle and insertion of adductor tendon. The target area was just proximal and anterior to the adductor tubercle, where the genicular nerve and vessels were found to be lying together. The needle was directed from anterior to posterior in the in-plane approach towards the nerve (Figure 1).
Figure 1.

Ultrasound image of the superomedial genicular nerve (SMGN) with the transducer is placed saggitally over the medial femoral epicondyle and to the level of adductor tubercle and insertion of adductor tendon. The needle is directed from lateral to medial along the in-plane approach.
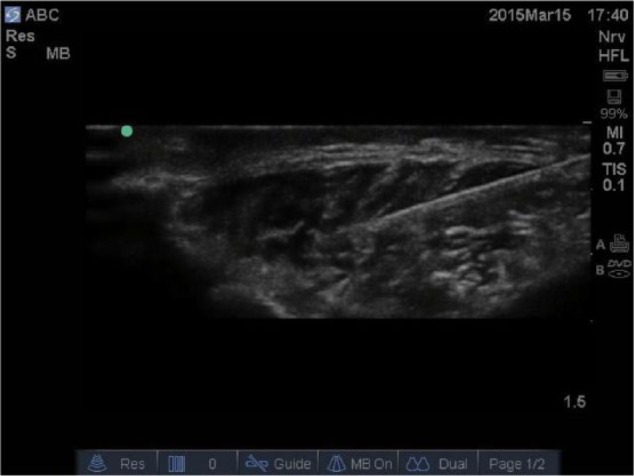
Superior lateral genicular nerve
The superior lateral genicular nerve (SLGN) is a branch of Nerve to Vastus lateralis which itself is a branch of femoral nerve supplying the superolateral and anterior aspect of knee joint capsule. To visualize the SLGN, the ipsilateral hip internally rotated to position the lateral aspect of knee joint facing superiorly and the USG transducer is aligned transversely over lateral aspect of femur at the junction of lateral epicondyle and shaft of femur. The SLGN and vessels are identified near the junction and the needle is directed in the in-plane from anterior to posterior direction (Figure 2).
Figure 2.

Ultrasound image of the superolateral genicular nerve (SLGN) with the ultrasound probe placed transversely over lateral aspect of femur at the junction of lateral epicondyle and shaft of femur. The needle is directed towards the nerve in the in-plane approach from anterior to posterior direction.
Middle genicular nerve
The middle genicular nerve (MGN) is a branch of Nerve Intermedius and gives the sensory innervation to the superior and anterior aspect of knee joint capsule. To visualize it, the knee was flexed with a pillow was placed under it, and the transducer was aligned transversely over the lower end of anterior aspect of femur just at the superior part of suprapatellar bursae. The needle was directed from lateral to medial direction towards the MGN, which was found between the fascia of the vastus intermedius, rectus femoris, suprapatellar bursae and vastus medialis and lateralis. (Figure 3).
Figure 3.

Ultrasound image of the middle genicular nerve (MGN) with the transducer positioned along the short axis of femur and with the radiofrequency needle directed in the in-plane approach towards it.
Inferior lateral genicular nerve
The inferior lateral genicular nerve (ILGN) is a branch of common peroneal nerve supplying the infero-lateral and anterior aspects of the knee joint. To visualize it, the hip was internally rotated and the knee was flexed. The USG transducer was aligned transversely over anterolateral aspect tibial condyle, and the needle is inserted using the in-plane technique from lateral to medial side of knee towards the ILGN which lies in close proximity to anastomotic branch of anterior tibial artery (Figure 4).
Figure 4.
Ultrasound image of the inferior lateral genicular (ILGN) with the ultrasound probe aligned transversely over anterolateral aspect tibial condyle and the needle is inserted through the in-plane technique from lateral to medial side of knee towards the inferior lateral genicular (ILGN) which lies in close proximity to anastomotic branch of anterior tibial artery.
Lateral retinacular nerve
Lateral retinacular nerve (LRN) is a branch of common peroneal nerve supplying the lateral aspect of knee joint. To visualize it, the hip was internally rotated and the knee was flexed. The transducer was aligned along the short axis of tibia at the lateral border of tibial condyle. The needle was inserted in the in-plane approach from the lateral to medial direction towards the LRN which lies underneath the lateral collateral ligament along with lateral inferior genicular artery (Figure 5).
Figure 5.

Ultrasound image of lateral retinacular nerve with the ultrasound transducer aligned along the short axis of tibia and the RF needle is directed in in-plane towards it.
Inferior medial genicular nerve
Inferior medial genicular nerve (IMGN) is derived from infra-patellar branch of saphenous nerve and runs in close proximity to inferior medial genicular artery in the junction between tibial condyle and shaft. To visualize the IMGN, the hip was externally rotated and knee is flexed. The USG transducer is aligned along the short axis of the tibia and medial collateral ligament. The needle was inserted in the in-plane approach from the anterior to the posterior direction towards the IMGN and artery, both of which lie just underneath the medial collateral ligament (Figure 6).
Figure 6.

Ultrasound image of inferior medial genicular nerve with the transducer along the short axis of tibia with the needle directed in-plane towards it.
Posterior genicular nerve plexus
The posterior genicular nerve plexus (PGN) supplies the posterior part of knee joint and is formed chiefly by articular branches of tibial nerve and rarely by the articular branches of obturator nerve. To visualize it, the patient was positioned prone and the probe was aligned transversely over posterior joint line. The popliteal artery was identified and the PGN usually lies deep into it. The needle was introduced in the in-plane approach from medial to lateral direction towards the nerve (Figure 7).
Figure 7.
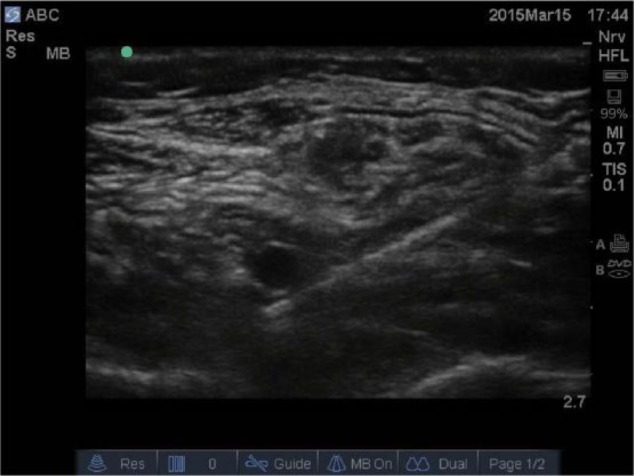
Ultrasound image of the posterior genicular nerve with the transducer transversely over posterior joint line and the radiofrequency needle is introduced in in-plane approach from medial to lateral direction.
A 22G 50 mm SonoPlex Stim cannulae (PAJUNK Medical Systems L.P., Norcross, GA, USA) was directed towards the genicular nerves under ultrasound guidance. The final position was confirmed by using nerve stimulator NS-100 (Inmed Equipments Pvt. Ltd., Vadodara, Gujarat, India) with elicitation of paraesthesia along the area of knee joint supplied by that respected genicular nerve by stimulation at 50 Hz current of <0.5 mV. The motor stimulation was done at 2 Hz and 2 mV current, which was negative at all instances. A volume of 2 mL of 2% lignocaine was injected, which was seen to encircle the nerves in all the patients. The block was considered successful or positive only if it had given a relief of more than 50% in pain intensity at all three occasions of rest, on walking and standing for more than 2 hour. The patients were considered for the therapeutic knee genicular RFA only if the patient had two positive successive diagnostic blocks, with a minimum gap of 1 week between the two procedures.
Therapeutic genicular nerve RFA
The therapeutic RFA of the genicular nerves was done using same technique as the USG guided diagnostic genicular nerve block. A 5-cm-long straight RF cannula with 5 mm active tip was advanced under USG guidance towards the nerve. The final position of the tip of the RF needle was as close to the nerve as possible. After negative aspiration of blood or fluid, 1 mL of 2% lignocaine was injected through the RF cannulae. For each genicular nerve, two conventional RF lesions were done for 90 s at 80° of temperature using the Cosman RFG-1B RF generator (Cosman Medical, Inc, Burlington, MA, USA). The patients were observed for 2 h immediately after the procedure for any immediate complications and relief of pain intensity.
Assessments
The patients were followed up for the next 6 months; with data collection before the procedure and at 1 and 6 months post-proceedure. The demographic data, previous treatment history and its duration and degree of relief and pain intensity in numerical rating scale (NRS) at rest, walking and movement were noted. The pain, physical stiffness and physical function were assessed by Oxford Knee Score (OKS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the quality of life by 36-Item Short Form Health Survey (SF-36). The pain intensity was measured by numerical rating scale (NRS), which is a 11-point scale indicating the pain in the past 24 h on a scale of 0 (no pain) to 10 (worst pain imaginable). Pain and physical function were assessed by OKS, which is a 12-point self-administered questionnaire with each item scored from 0 for worst symptom/outcome and 4 for no symptoms/best outcome. The pain, stiffness and physical function were also assessed by WOMAC score which is a 24-point scale with 5 items for pain, 2 items for stiffness and 17 items for physical function. Each item is a 5-point likert scale from 0 to 4. The scoring ranges are pain = 0–20, stiffness = 0–8 and physical function = 0–68, with higher score showing worst pain, stiffness and functional limitations.
Statistical analysis
The statistical analysis was done using the Statistical Package for the Social Sciences (SPSS) (version 17, SPSS Inc., Chicago, IL, USA) for Windows. The variables were expressed as mean and standard deviation. The paired t-test of the changes in variables with time was used to analyse the effectiveness of RFA. The factors responsible for more than 50% pain relief after the RFA was analysed by using the Chi-square test or Fisher’s exact test. The level of significance was set at p value of <0.05.
Results
Demographics
The average age of the patients was 61.50 ± 6.75 years, and out of them, five were male and three were female respectively. Half of the patients had pain in the right knee, while another half had pain in the left knee. Surprisingly, all the patients were obese and the average BMI was 31.97 ± 0.89. The duration of the knee pain was 55.50 ± 15.70 months. The patients were having either grade 3 or 4 of Kellgren and Lawrence system of knee osteoarthritis. The above demographic details and baseline medications of each patient are given in Table 1.
Table 1.
Showing demographic features and duration of pain and the medications with their doses.
| Serial no. | Age (years) | Sex | Knee pain side | BMI | Kellgren and Lawrence grade of OA | Duration of pain | Medications and their doses |
|---|---|---|---|---|---|---|---|
| 1 | 65 | Male | Right | 31.97 | 3 | 38 | Paracetamol 3 g/day Duloxetine 60 mg/day Etoricoxib 60 mg/day (for approximately 2–3 days/week) Tramadol 100–150 mg/day |
| 2 | 58 | Female | Left | 32.14 | 3 | 42 | Paracetamol 3 g/day Duloxetine 60 mg/day Tramadol 10–150 mg/day Etoricoxib 60 mg/day (for approximately 2–3 days/week) |
| 3 | 54 | Male | Left | 32.28 | 4 | 76 | Paracetamol 3 g/day Gabapentine 600 mg/day Tramadol 100–200 mg/day Etoricoxib 60 mg/day (for approximately 3–5 days/week) |
| 4 | 69 | Male | Right | 33.28 | 4 | 82 | Paracetamol 3 g/day Pregabalin 150 mg/day Tramadol 50–150 mg/day Etoricoxib 60 mg/day (for approximately 1–2 days/week) |
| 5 | 65 | Male | Right | 32.04 | 3 | 48 | Paracetamol 2 g/day Duloxetine 60 mg/day Tramadol 100–150 mg/day Diclofenac sodium 50 mg/day (for approximately 0–2 days/week) |
| 6 | 68 | Female | Left | 30.09 | 3 | 56 | Paracetamol 2 g/day Duloxetine 60 mg/day Tramadol 100–150 mg/day Diclofenac sodium 50 mg/day (for approximately 1–2 days/week) |
| 7 | 75 | Male | Right | 32.36 | 3 | 48 | Paracetamol 3 g/day Pregabalin 150 mg/day Tramadol 100–150 mg/day Etoricoxib 90 mg/day (for approximately 1–3 days/week) |
| 8 | 72 | Female | Left | 31.63 | 3 | 54 | Paracetamol 3 g/day Duloxetine 60 mg/day Tramadol 100–150 mg/day Etoricoxib 60 mg/day (for approximately 2–3 days/week) |
Previous treatment history
All patients had previously undergone conservative treatment and intra-articular injections of steroid, hyaluronic acid, platelet-rich plasma and so on. The details of each patient and the amount and duration of relief from each treatment were also given in detail in Table 2.
Table 2.
Showing the previous treatments used by the patients and the degree of relief.
| Intra-articular Synvisc-One | Intra-articular PRP | Intra-articular steroid | Physical therapy | Reduction of excess weight | Lateral wedged insoles | Appropriate footwear | Knee braces | |
|---|---|---|---|---|---|---|---|---|
| 1. | 1. First injection = 50% relief for 3 weeks 2. Second injection = 20% relief for 1 week |
Three injections of PRP with the relief of only 15–20% for 1–2 weeks | 20% relief for 1.5 weeks only | For 8 weeks with 10–15% relief | Tried with decrease of 4% weight and no pain relief | Tried but no relief | Tried but no relief | Not tried |
| 2. | One injection = 20% relief for 3 weeks | Not received | 20% relief in pain intensity in NRS for 1 week only | For 6 weeks with 15% relief | Tried with decrease of 8% of weight and no pain relief | 10% relief | Tried with no relief | Tried and got 10% relief |
| 3. | 1. First injection = 60% relief for 3 weeks 2. Second injection = 10% relief for 1 week |
Three injections of PRP with relief of only 10–20% for 2–3 weeks | 30% relief for 1 week only | For 8 weeks with only 10% relief | Tried with decrease of 4% weight and no relief in pain | Not tried | Tried with 10% relief | Tried but no relief |
| 4. | One injection = 20% relief for 1 week | Three injections of PRP with relief of only 15–20% for 2–3 weeks | 1. First injection = 30% relief for 3 weeks only 2. Second injection = no relief |
For 6 weeks with 10–15% relief | Tried with decrease of 15% weight and pain relief of 10–15% | Not tried | Tried but no relief | Tried with 5% relief |
| 5. | 1. First injection = 55% relief for 4 weeks 2. Second injection = 15% relief for 1 week |
Not received | 40% relief for 1 week only | For 6 weeks with no relief | Tried with decrease of 5% of weight and no pain relief | Not tried | Tried with 5% relief | Tried with 10% relief |
| 6. | Not received | Not received | 30% relief for 1 week only | For 8 weeks with only 10% relief | Tried with decrease of 10% weight and relief of 5% | Tried but 10% relief | Tried with 5% relief | Not tried |
| 7. | 1. First injection = 40% relief for 2 weeks 2. Second injection = 15% relief for 1 week |
Three injections of PRP with relief of only 10–20% for 2–3 weeks | Not received | For 8 weeks with only 15% relief | Tried with decrease of 3% weight and no relief in pain | Tried but no relief | Tried but no relief | Tried with 5% relief |
| 8. | One injection = 15% relief for 1 week | Three injections of PRP with relief of only 10% for 1–2 weeks | 20% relief in pain intensity in NRS for 1 week only | For 8 weeks with no relief | Tried with decrease of 7% weight and no relief in pain | Not tried | Tried with 5% relief | Tried with no relief |
PRP: platelet-rich plasma; NRS: numerical rating scale.
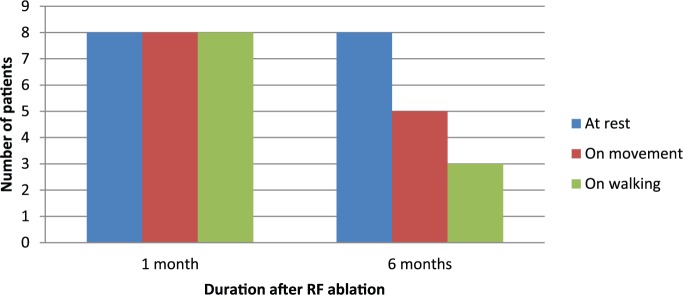
Pain intensity
The RF treatment resulted in significant improvement in the pain intensity at rest, on movement and on walking for up to 6 months (p value <0.05; Table 3). At 1 month, almost all patients had more than 50% improvement in pain intensity at rest, on movement and on walking. Interestingly, even at 6 months, eight, five and three patients had more than 50% relief in pain intensity on rest, on movement and on walking (Figure 8), respectively.
Table 3.
Showing pain intensity at rest, on movement and on walking.
| NRS at rest |
NRS on movement |
NRS on walking |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Before procedure | 1 month | 6 months | Before procedure | 1 month | 6 months | Before procedure | 1 month | 6 months | |
| 1 | 9 | 2 | 3 | 9 | 3 | 4 | 9 | 4 | 4 |
| 2 | 8 | 2 | 2 | 9 | 3 | 4 | 9 | 4 | 5 |
| 3 | 9 | 2 | 3 | 9 | 4 | 5 | 9 | 4 | 4 |
| 4 | 9 | 3 | 3 | 9 | 4 | 4 | 9 | 5 | 5 |
| 5 | 9 | 3 | 4 | 9 | 4 | 5 | 9 | 4 | 4 |
| 6 | 8 | 2 | 3 | 8 | 4 | 4 | 9 | 4 | 5 |
| 7 | 9 | 3 | 4 | 9 | 4 | 5 | 9 | 4 | 5 |
| 8 | 8 | 2 | 3 | 9 | 4 | 4 | 9 | 4 | 5 |
| Average | 8.63 ± 0.51 | 2.38 ± 0.51 | 3.13 ± 0.64 | 8.88 ± 0.35 | 3.75 ± 0.46 | 4.38 ± 0.51 | 9.0 ± 0.0 | 4.13 ± 0.35 | 4.63 ± 0.51 |
NRS: numerical rating scale.
Figure 8.
The number of patients with more than 50% relief after the RFA at 1 and 6 months.
Oxford Knee Score (OKS)
The OKS had improved significantly from 7.25 ± 1.03 before the procedure to 28.88 ± 2.53 at 1 month after the procedure and this improvement was maintained till 6 months when it was 28.13 ± 1.80 (Table 4).
Table 4.
Showing OKS and WOMAC score at baseline and 1 and 6 months.
| OKS |
WOMAC score |
|||||
|---|---|---|---|---|---|---|
| Before procedure | 1 month | 6 months | Before procedure | 1 month | 6 months | |
| 1 | 6 | 24 | 25 | 84 | 45 | 46 |
| 2 | 9 | 27 | 26 | 77 | 42 | 43 |
| 3 | 8 | 31 | 28 | 74 | 35 | 36 |
| 4 | 8 | 32 | 30 | 76 | 30 | 32 |
| 5 | 7 | 30 | 29 | 78 | 31 | 33 |
| 6 | 7 | 29 | 30 | 79 | 38 | 39 |
| 7 | 7 | 30 | 29 | 80 | 42 | 43 |
| 8 | 6 | 28 | 28 | 79 | 44 | 42 |
| Average | 7.25 ± 1.03 | 28.88 ± 2.53 | 28.13 ± 1.80 | 78.38 ± 2.97 | 38.38 ± 5.82 | 39.25 ± 5.12 |
WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; OKS: Oxford Knee Score.
WOMAC score
The pain, stiffness and physical function as measured by WOMAC score improved significantly from 78.38 ± 2.97 before the procedure to 38.38 ± 5.82 and 39.25 ± 5.12 at 1 and 6 months, respectively (p value <0.05; Table 4).
Quality of life
There was also significant improvement in the quality of life in both physical and mental health measured by SF-36 questionnaire from 23.32 ± 2.16 and 31.22 ± 4.35 to 49.68 ± 2.49 and 53.93 ± 3.23 at 1 month and 49.48 ± 2.11 and 51.63 ± 4.18 at 6 months, respectively (p value <0.05; Table 5).
Table 5.
Showing the quality of life as measured by SF-36 questionnaire at baseline and after 1 and 6 months of RFA ablation.
| Physical health |
Mental health |
|||||
|---|---|---|---|---|---|---|
| Baseline | 1 month | 6 months | Baseline | 1 month | 6 months | |
| 1 | 22.1 | 49.5 | 50.6 | 31.5 | 56.7 | 57.5 |
| 2 | 22.7 | 53.5 | 50.2 | 34.6 | 46.6 | 43 |
| 3 | 24.9 | 46.9 | 49.2 | 25 | 54.7 | 52 |
| 4 | 21.9 | 49.4 | 51.7 | 23.8 | 53.1 | 49.8 |
| 5 | 26.8 | 48.7 | 48.1 | 32.9 | 56.1 | 52.2 |
| 6 | 19.8 | 52 | 48.3 | 34 | 54.2 | 54.7 |
| 7 | 23.8 | 46.2 | 52.1 | 33.1 | 53.8 | 51.9 |
| 8 | 24.6 | 51.3 | 45.7 | 34.9 | 56.3 | 52 |
| Average | 23.32 ± 2.16 | 49.6 ± 2.49 | 49.48 ± 2.11 | 31.22 ± 4.35 | 53.93 ± 3.23 | 51.63 ± 4.18 |
SF-36: 36-Item Short Form Health Survey.
Complications and adverse effects
There were no immediate or delayed major complications. However, in two patients, there were hypoesthesia and in one patient there was numbness; but nevertheless, these did not cause much discomfort and improved by more than 50% during 6 months of time. There was no instance of increased pain, increased allodynia or hyperaesthesia, deafferentation pain, anaesthesia dolorosa and so on among the patients after the procedure.
Discussion
Our case series is the first reported case series in the literature where the RFA was done for all the seven genicular nerves.
The knee joint is innervated by articular branches of femoral, common peroneal, saphenous, tibial and obturator nerves.20,21 The RFA of these nerves had been attempted for last few years for relief of pain from knee osteoarthritis. In most of the previous studies, RFA was done by the aid of fluoroscopy, which relies on the virtual anatomical position of the nerve around the knee joint.13–15 The limitation of this technique is that only the ablation of the three genicular nerves was possible and recent studies had also showed that there are chances of injury to the vessels which accompany these nerves.22 However, recently, ultrasound-guided RFA of genicular nerves was also attempted, but these interventions were limited to the same three genicular nerves as fluoroscopy. But it had the advantage that the nerves can be seen directly via ultrasound during the procedure which increases the precision of the procedure and also the safety by avoiding the vessels which accompany the nerves and had the chance of injury with fluoroscopy.16–18,22
Recently, the blockade of the seven genicular nerves with ultrasound guidance had been described by Stanley K.H. Lam.19 He described the technique to block the four additional genicular nerves, that is, the MGN, LRN, PGN and ILGN.19 The added advantage of ablating these four additional nerves in our study had resulted in excellent and sustained relief in pain and symptoms for up to 6 months.
There are many interventions for knee pain described in the literature for patients with severe knee pain who either can not undergo surgery or not willing to undergo surgery. But most of these interventions are not effective in all the patients.10–12
In our study, the immediate pain relief was excellent with more than 50% relief in nearly all patients at rest, on movement and on walking. The relief was also maintained for 6 months at rest and on movement for most of the patients; whereas on walking, more than 50% relief was maintained in only three out of eight patients. Although many patients were not getting more than 50% relief in pain intensity till 6 months, the improvement was statistically significant at both 1 and 6 months after the procedure. There was also improvement in stiffness and function after the procedure as measured by OKS and WOMAC index, and it was maintained till 6 months. The quality of life also improved after the procedure and was maintained for next 6 months.
In our case series, all the patients get good and prolonged pain relief as compared to the previous studies where RFA of only three genicular nerves was attempted. In one of the previous studies, a few patients failed to get relief with the RFA.13 It is due to the fact that the knee joint is also innervated by articular branches of other nerves such as femoral, common peroneal, saphenous, tibial and obturator nerves apart from the genicular nerve that was ablated by the earlier techniques of the RFA.20,21 So, they had suggested that RFA of genicular nerves may not relieve the pain from knee joint in all the patients; but in our study, additional ablation of genicular nerves resulted in excellent and prolonged pain relief. So, the RFA of seven genicular nerves can be a good alternative for relief of pain and symptoms from knee osteoarthritis.
In our case series, no patient complained of transient pain during the RFA which had earlier occurred during fluroscopic guided RFA and was attributed to the stimulation of the periosteum and ligament insertion sites by the RF cannulae. In USG guidance, the precise position of the RF cannulae could be visualized, thus avoiding the injury to the nearby structures.13,22
Limitations
The limitations of the study include the following;
a) retrospective case-series
b) limited number of patients
c) limited follow-up
d) absence of control group
Conclusion
The ultrasound-guided RFA of the seven genicular nerves is a safe and effective method of treatment for patients suffering from severe pain from knee joint osteoarthritis. However, to generalize this statement, a larger randomized sham control study with larger sample size and prolonged follow-up is required.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil 2006; 85: S2–S14. [DOI] [PubMed] [Google Scholar]
- 2. Hopman-Rock M, Odding E, Hofman A, et al. Physical and psychosocial disability in elderly subjects in relation to pain in the hip and/or knee. J Rheumatol 1996; 23: 1037–1044. [PubMed] [Google Scholar]
- 3. Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001; 60: 91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilcox S, Brenes GA, Levine D, et al. Factors related to sleep disturbance in older adults experiencing knee pain or knee pain with radiographic evidence of knee osteoarthritis. J Am Geriatr Soc 2000; 48: 1241–1251. [DOI] [PubMed] [Google Scholar]
- 5. Bjordal JM, Ljunggren AE, Klovning A, et al. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ 2004; 329: 1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 2014; 5(3): 351–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jüni P, Hari R, Rutjes AW, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015; 10: CD005328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weiner DK, Rudy TE, Morone N, et al. Efficacy of periosteal stimulation therapy for the treatment of osteoarthritis-associated chronic knee pain: an initial controlled clinical trial. J Am Geriatr Soc 2007; 55: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 9. White A, Foster NE, Cummings M, et al. Acupuncture treatment for chronic knee pain: a systematic review. Rheumatology 2007; 46: 384–390. [DOI] [PubMed] [Google Scholar]
- 10. Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013; 72(7): 1125–1135. [DOI] [PubMed] [Google Scholar]
- 11. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014; 22: 363–388. [DOI] [PubMed] [Google Scholar]
- 12. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012; 64(4): 465–474. [DOI] [PubMed] [Google Scholar]
- 13. Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain 2011; 152: 481–487. [DOI] [PubMed] [Google Scholar]
- 14. Sari S, Ozlülerden P, Aydin ON, et al. Radiofrequency thermocoagulation on genicular nerves in chronic knee osteoarthritis: a pilot study for a new alternative therapy. Turk J Phys Med Rehab 2016; 62: 234–239. [Google Scholar]
- 15. Bellini M, Barbieri M. Cooled radiofrequency system relieves chronic knee osteoarthritis pain: the first case-series. Anaesthesiol Intensive Ther 2015; 47(1): 30–33. [DOI] [PubMed] [Google Scholar]
- 16. Wong J, Bremer N, Weyker PD, et al. Ultrasound-guided genicular nerve thermal radiofrequency ablation for chronic knee pain. Case Rep Anesthesiol. Epub ahead of print 16 October 2016. DOI: 10.1155/2016/8292450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Demİr Y, Güzelküçük Ü, Tezel K, et al. A different approach to the management of osteoarthritis in the knee: ultrasound guided genicular nerve block. Pain Med 2017; 18: 181–183. [DOI] [PubMed] [Google Scholar]
- 18. Kesikburun S, Yaşar E, Uran A, et al. Ultrasound-guided genicular nerve pulsed radiofrequency treatment for painful knee osteoarthritis: a preliminary report. Pain Physician 2016; 19(5): E751–E759. [PubMed] [Google Scholar]
- 19. Stanley KH Lam. Ultrasonography and Injection Techniques of the Genicular Nerves of the Knee Joint. In: Manoj Kumar Karmakar. (eds.) Musculoskeletal Ultrasound for Regional Anesthesia and Pain Medicine, 2nd edition Hong Kong: Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, 2014, pp. 797–818. [Google Scholar]
- 20. Hirasawa Y, Okajima S, Ohta M, et al. Nerve distribution to the human knee joint: anatomical and immunohistochemical study. Int Orthop 2000; 24: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med 1982; 10: 329–335. [DOI] [PubMed] [Google Scholar]
- 22. Kim SY, Le PU, Kosharskyy B, et al. Is genicular nerve radiofrequency ablation safe? A literature review and anatomical study. Pain Physician 2016; 19(5): E697–E705. [PubMed] [Google Scholar]