Abstract
Purpose:
We compared the effectiveness of three active vision therapy approaches for convergence insufficiency (CI).
Methods:
This randomized clinical trial included patients meeting the eligibility criteria and with symptomatic CI, who were allocated into three groups. In the home-based vision orthoptic therapy (HBVOT) group, patients performed the pencil push-up procedure 15 min/day for 5 days/week. In the office-based vision orthoptic therapy (OBVOT) group, patients underwent 60-min orthoptic therapy using a major amblyoscope twice weekly with additional home orthoptic therapy. In the augmented office-based vision orthoptic therapy (AOBVOT) group, patients performed orthoptic exercises using 3-diopter over-minus lenses and a base-out prism in addition to major amblyoscope therapy, and additional home reinforcement was prescribed during the same time period.
Results:
All 84 subjects (mean age, 26.8 ± 8.3 years) showed a statistically significant improvement in near exophoria, positive fusional vergence (PFV) at near, near point of convergence (NPC), stereoacuity, and Convergence Insufficiency Symptom Survey (CISS) scores at follow-up. Exophoria decreased by 64%, 68%, and 85% in the HBVOT, OBVOT, and AOBVOT groups, respectively (P = 0.2). PFV increased by 68%, 100%, and 100% in the HBVOT, OBVOT, and AOBVOT groups, respectively (P < 0.001). NPC decreased (improved) by 86%, 89%, and 96% in the HBVOT, OBVOT, and AOBVOT groups, respectively (P = 0.4). The CISS scores decreased by 75%, 96%, and 100% in the HBVOT, OBVOT, and AOBVOT groups, respectively (P = 0.003).
Conclusion:
Our results showed that in adults with CI, the augmented office-based orthoptic treatment was relatively more effective than the other treatments.
Keywords: Convergence Insufficiency, Orthoptic Therapy, Vision Therapy
INTRODUCTION
Convergence insufficiency (CI) is a common binocular visual problem characterized by exophoria that is greater at near distances than at far distances as well as an increased near point of convergence (NPC) and reduced positive fusional vergence (convergence amplitude) (PFV) at near distance. Population studies have estimated that the prevalence of CI is approximately 5% (range, 1.75 to 33%).[1,2,3,4]
The common symptoms of CI include discomfort after short periods of reading, computer work, or performing near activities, as well as eyestrain, frontal headache, blurred vision, diplopia, sleepiness, difficulty concentrating, tearing, and dull orbital pain. Thus, CI may interfere with the quality of life, especially during reading and near work.[1,2,3,4,5,6]
Although various treatments are prescribed, including base-out prism glasses, home-based pencil push-ups, office-based vision therapy/orthoptic therapy, and home-based computer vergence/accommodative therapy, there is a paucity of data and lack of consensus about the most appropriate treatment.[1,2,6,7,8,9,10,11,12,13,14] Home-based pencil push-ups are the most commonly prescribed treatment by both optometrists and ophthalmologists, but office-based vision therapy is more extensively studied and has been found more effective than is pencil push-up therapy.[7,8,10,11,12] In a 1999 randomized controlled study of 60 adult patients aged over 40 years with CI, Birnbaum et al found that office-based vision therapy with supplementary home therapy was successful in 61.9% of patients, whereas home-based vision therapy was successful in only 10.5% of patients.[7] Other studies showed that vergence therapy increased PFV and decreased symptoms in children with CI.[3,13,14]
In the present study, we evaluated three active vision therapies (home-based vision orthoptic therapy [HBVOT], office-based vision orthoptic therapy [OBVOT], and augmented office-based vision orthoptic therapy [AOBVOT]) for CI and investigated whether the augmented orthoptic treatments have a more objective or subjective effect in relieving the patients' symptoms and signs.
METHODS
This randomized clinical trial (RCT) was registered at ClinicalTrials.gov under the title “Comparison of three vision therapy approaches for convergence insufficiency” (NCT03431454). The study was approved by the Ethics Committee of the Shahid Beheshti University of Medical Sciences (SBMU) in Tehran, Iran, and was performed at Labbafinejad Hospital, which is affiliated with the SBMU. All newly diagnosed patients with CI were enrolled and randomly included in three groups. Written informed consent was obtained from the enrolled patients or from the legal guardians in case of children.
This single-masked randomized clinical trial (RCT) study was conducted during a 2-year period from January 2014 to January 2016. Data were collected by a pediatric ophthalmologist and certified orthoptist in private practice.
The eligible patients were aged between 15 and 35 years and had symptomatic CI diagnosed using the Convergence Insufficiency Symptom Survey (CISS) scoring system. CISS is a scoring system used to quantify the severity of symptoms associated with CI, and its findings are valid even when administered by an unmasked examiner. Although some reports indicate a low specificity for CISS scores, they are still used for the subjective evaluation of patients with CI.[15,16,17]
The CISS score was determined by the same examiner. A symptomatic score was an average score of 16 or higher on the CISS. Each response was scored between 0 and 4 points, with 4 representing the highest frequency of symptom occurrence (always) and 0 representing the lowest occurrence (not having that symptom). The highest possible score was 60 (most symptomatic).
The other inclusion criteria were best-corrected visual acuity ≥20/25, exophoria at near at least 4 prism diopters (Δ) greater than at distance, NPC more than 6.0 cm break, and insufficient PFV (failing Sheard's criterion or PFV ≤15 Δ base-out) at near distance.
The exclusion criteria were amblyopia (visual acuity worse than 20/30 in each eye), presence of manifest strabismus, history of ocular surgery, any systemic disorder, anisometropia of more than 1.5 diopters of myopia or hyperopia or significant refractive error, and nystagmus and usage of medications that may impair accommodation or convergence. Patients with ocular surface abnormalities or a history of ocular allergy or those who had previously been treated for CI were also excluded.
Demographic characteristics of the patients including age and sex were recorded. A comprehensive eye examination, including best-corrected visual acuity, refraction at far and near distances, and cycloplegic refraction with a mixture of one drop of tropicamide 1% and cyclopentolate 1%, as well as an examination of the anterior and posterior segments of the eye were conducted and the results recorded for each patient.
In addition, the following binocular sensory and motor tests were performed:
Cover/uncover (unilateral cover) test and alternate cover test with prism neutralization at distance and near were performed using an accommodative target.
Negative fusional vergence (blur/break, and recovery) at near was tested using the prism bar method.
PFV (blur/break, and recovery) at near was tested using the prism bar method.
NPC was evaluated using the standard push-up technique, which determined abnormalities longer than 10 cm.
Push-up accommodative amplitude measurement was performed for each eye separately and also both eyes together (monocular and binocular).
Monocular accommodative facility, positive and negative relative accommodation (PRA and NRA) (the ability to quickly achieve clear vision while alternately viewing 20/20 on a high contrast near chart using +2 diopter and −2 diopter lenses), was tested. The lenses were added binocularly and incrementally until blurring of vision occurred. Then, the plus lenses added for NRA testing and minus lenses for PRA testing were charted. NRA was evaluated before PRA to avoid any unwanted effect of accommodation on the results.
Stereoacuity was evaluated using a Titmus stereo test.
All tests at near were performed at 40 cm, and tests at distance were performed at 6 m.
The patients were randomly allocated to one of the three groups by using permuted-block randomization: HBVOT, OBVOT, and AOBVOT.
HBVOT
In this group, the patients were trained to perform the pencil push-up procedure. This procedure is done by holding a pencil with 20/60 size letters at arm's length in front of the eyes. The patient attempts to look at the pencil in the white background while moving it towards his/her nose.
The goal of the procedure was to move the pencil to within 2 to 3 cm of the brow, just above the nose on each push-up with a steady tenacious convergence and without disruption of fusion. Patients were instructed to perform the pencil push-up procedure for 15 min/day for 5 days/week. They recorded the closest distance at which they could maintain fusion after each 5 min of therapy. We did not supervise the patients at home when they performed orthoptic therapy and trusted they performed the therapy correctly.
OBVOT
OBVOT included 60 min of orthoptic therapy using the major amblyoscope performed twice weekly with additional home orthoptic therapy (pencil push-ups) prescribed for 15 min/day for 5 days/week (home reinforcement).
AOBVOT
In this group, the therapist performed the orthoptic exercise by using 3-diopter over-minus lenses (according to the patient's refraction) and a base-out prism, while the patient was performing a near task like reading a book, in addition to using a major amblyoscope. This orthoptic therapy was performed for 60 min twice weekly with additional home reinforcement.
Main Outcomes
Subjective outcome: improvement or decrease in symptoms based on the CISS score.
Objective outcomes: improvement in the amount of PFV, NPC, exophoria at far and near distances, and stereoacuity at near distance.
Follow-up visits were conducted by the therapist and another examiner twice weekly for 6 weeks, and thereafter, at 3 and 6 months after the completion of treatment. The data collected during each examination were recorded and analyzed.
Statistical Analysis
In this study, the mean, standard deviation, median, range, and frequency of data were calculated. To evaluate the difference between baselines, we used the Kruskal-Wallis and Chi-square tests, and to assess the improvement within the groups, we used the linear mixed model. To evaluate the differences between groups adjusted for the baseline values, we used an analysis of covariance. However, the relationship of CISS score change with exophoria and NPC was assessed using the Spearman correlation coefficient. As the last step, in order to consider the multiple comparisons, we used a Bonferroni correction. All statistical analyses were performed using SPSS Statistics software (Released 2013. Version 22.0. Armonk, NY: IBM Corp). P values less than 0.05 were considered statistically significant.
RESULTS
In total, 84 patients were enrolled in this study (28 in each group). The mean age of the patients was 26.8 ± 8.3 years (range, 15 to 35 years). Among them, 20 (24%) were male and 64 (76%) were female. The age of the patients was comparable in the three groups (P = 0.1). However, a difference was observed in sex between the three groups (P = 0.04).
All three groups showed a statistically significant improvement in near exophoria in all the follow-up examinations (all P < 0.001). No statistically significant difference was observed between the three groups at baseline in near exophoria (P = 0.6).
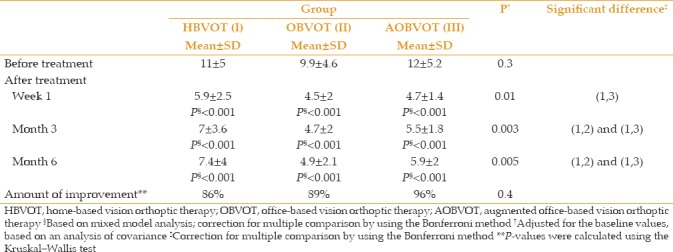
After adjusting for the baseline values, no statistically significant difference was observed between the three groups in near exophoria at 1 week and at 3 months (P = 0.3 and P = 0.2, respectively). In contrast, 6 months after treatment, a statistically significant difference was observed in near exophoria between the three groups (P = 0.02). This difference was due to the difference observed between the AOBVOT group and the HBVOT and OBVOT groups. However, no statistically significant difference was observed between the HBVOT and OBVOT groups at 6 months [Table 1]. Table 2 shows the far distance exophoria values of the three groups.
Table 1.
Near exophoria changes in the three groups
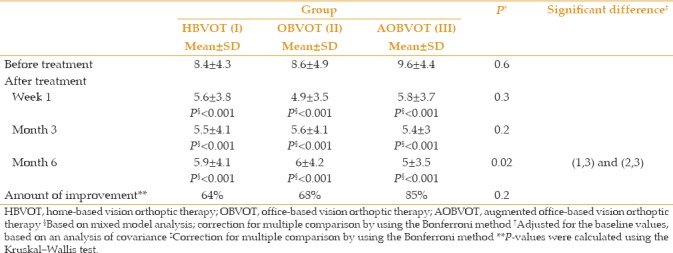
Table 2.
Distance exophoria before and after treatment in the study groups
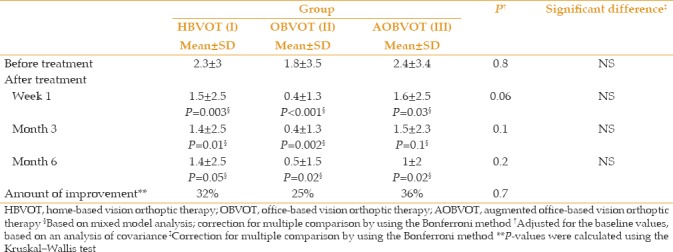
The amount of near exophoria decreased by 64%, 68%, and 85% in the HBVOT, OBVOT, and AOBVOT groups, respectively, at the end of the follow-up examinations (P = 0.2). The amount of far distance exophoria decreased by 32%, 25%, and 36% in the HBVOT, OBVOT, and AOBVOT groups, respectively, at the end of the follow-up examinations [Table 2].
All three groups showed a statistically significant improvement in near PFV in all the follow-up periods, except for the HBVOT group at 6 months, which was not statistically significant (P = 0.4). Six months after treatment, a statistically significant difference was observed in near PFV between the three groups. Post-hoc analysis revealed that this difference was due to the difference observed between the AOBVOT and OBVOT groups and the HBVOT group [Table 3]. The amount of PFV increased by 68% in the HBVOT group and by 100% in both the OBVOT and AOBVOT groups at the end of the follow-up examinations (P < 0.001). Table 4 shows the distance positive fusional vergence (PFV) before and after treatment in the study groups.
Table 3.
Near positive fusional vergence before and after treatment in the study groups
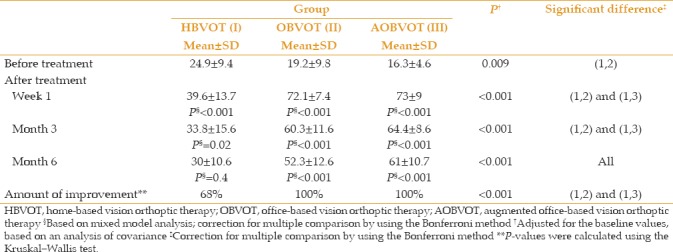
Table 4.
Distance positive fusional vergence before and after treatment in the study groups
A statistically significant difference was observed in NPC between the three groups. Post-hoc analysis revealed that this difference was due to the difference observed between the AOBVOT and OBVOT groups and the HBVOT group. The amount of NPC decreased by 86%, 89%, and 96% in the HBVOT, OBVOT, and AOBVOT groups, respectively, at the end of the follow-up examinations (P = 0.4) [Table 5].
Table 5.
Near point of convergence before and after treatment in the study groups
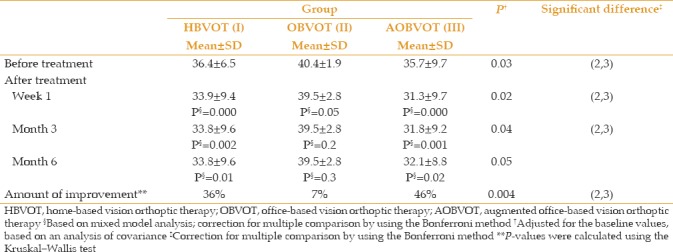
Statistically significant improvements in stereoacuity were observed, except for the improvement of stereoacuity in the OBVOT group, which was significant only up to 1 week (P = 0.05) but not at 3 months or 6 months (P = 0.2 and P = 0.3, respectively) [Table 6].
Table 6.
Stereoacuity before and after treatment in the study groups
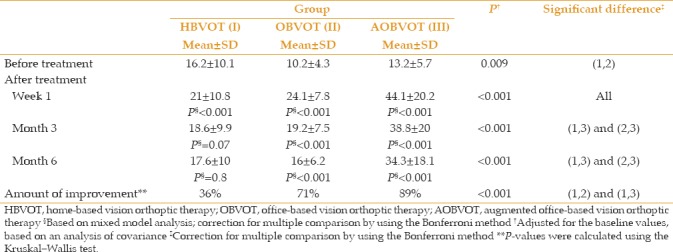
After adjusting for the baseline values, a statistically significant difference was observed between the three groups regarding the CISS at all the follow-up periods (all P < 0.001). In addition, post-hoc analysis revealed that all the pairwise differences in these periods were statistically significant (P < 0.001 for all the comparisons) [Table 7].
Table 7.
Convergence Insufficiency Symptom Survey scores before and after treatment in the study groups
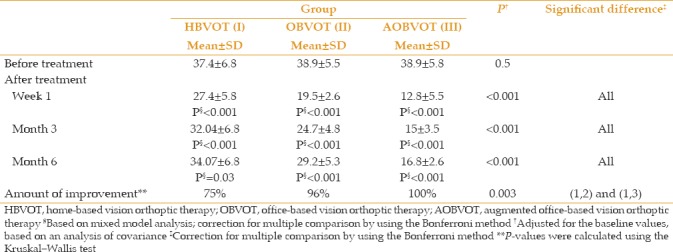
The number of CISS grades decreased in 75%, 96%, and 100% of the patients in the HBVOT, OBVOT, and AOBVOT groups, respectively, after the initiation of therapy (P < 0.003). Moreover, no statistically significant correlation was observed between the changes in all variables (near and far exophoria, NPC, PFV, and CISS) with age in the different groups.
DISCUSSION
There is a lack of consensus regarding the most appropriate treatment for CI. Many physicians consider patient cost as well as treatment effectiveness when deciding on a treatment. Pencil push-up therapy and home-based computer orthoptic treatment are far less expensive to the patient than are office treatments. This may play a greater role in the way physicians choose treatment modalities when they have a choice between treatments that have relatively similar effects.
Pencil push-ups and office-based orthoptics are the most routine treatment modalities.[7,8,9,10,11,12,13,14] Most ophthalmic practitioners and optometrists prescribe pencil push-up therapy as the initial treatment for CI.[1,7,8,10]
On the basis of the motor and sensory tests, the results of the present study demonstrate that in adult patients with CI, the augmented office-based orthoptic treatment was relatively more effective at the last follow-up examination than were the other treatment methods.
In a previous study, Scheiman et al showed that the most common treatment prescribed by optometrists was pencil push-up therapy (36%), followed by home-based vision therapy (22%), and office-based vision therapy (16%). For ophthalmologists, the most common treatment prescribed was pencil push-up therapy (50%), followed by home-based vision therapy (21%), and base-in prism (10%).[10]
In a RCT investigating the efficacy of vision therapy/orthoptics for the treatment of CI in young adults, Gallaway et al demonstrated that patients in the pencil push-up group did not demonstrate significant changes in the NPC and PFV at a near distance. Moreover, only 20% of the subjects in the home-based pencil push-up group showed symptom elimination according to the predescribed criterion.[12]
In our study, patients in the pencil push-up group demonstrated statistically and clinically significant changes in the clinical measures of NPC (86%) and PFV (68% improvement) at a near distance, even though these measures were lower than those in the other two groups.
Office-based vision therapy/orthoptics have been extensively studied.[8,9,10,11,12,13,14] Grisham reviewed the ophthalmic literature related to the treatment results for CI utilizing vision therapy training procedures for the years between 1940 and 1987. He evaluated 17 studies including 1931 patients, and reported a cure rate of 72%.[8]
In another study, Scheiman et al compared vision therapy/orthoptics, pencil push-ups, and placebo vision therapy/orthoptics as treatments for symptomatic CI in young adults with ages ranging from 19 to 30 years. In this study, vision therapy/orthoptics was the only treatment that produced clinically significant improvements in the NPC and PFV. All three groups demonstrated statistically significant changes in symptoms with 42% showing improvements with office-based vision therapy/orthoptics, 31% with office-based placebo vision therapy/orthoptics, and 20% with home-based pencil push-ups, thereby meeting their criteria for elimination of symptoms, which had been predetermined as a score of less than 21 at the 12-week visit. However, over half of the patients in this group (58%) were still symptomatic at the end of treatment, even though their symptoms were significantly reduced.[11] In our study, the CISS score decreased by 75%, 96.4%, and 100% in the HBVOT, OBVOT, and AOBVOT groups, respectively, after the initiation of therapy.
In the Convergence Insufficiency Treatment Trial, 221 children were randomly assigned to receive a 12-week program of home-based pencil push-ups, home-based computer vergence/accommodative therapy plus pencil push-ups, office-based vergence/accommodative therapy with home reinforcement, or office-based placebo therapy. After 12 weeks of treatment, the mean CISS score of the office-based vergence/accommodative therapy group was significantly lower than that of the other groups. The office-based vergence/accommodative therapy group also demonstrated significantly greater improvement in symptoms and clinical measures of NPC and PFV, and the predetermined criteria of success were achieved by a greater percentage of patients in this group than in the other groups. A successful or improved outcome was found in 73% of patients in the office-based vergence/accommodative therapy group, and the success rates in the other groups were less than 45%.[3]
In conclusion, results of the present study demonstrated that in young adults with CI, the augmented office-based orthoptic treatment in which patients received 3-diopter over-minus refraction (compared to the patients' refraction) and base-out prism was relatively more effective than were the other treatment methods such as pencil push-up therapy. Moreover, using multiple methods to improve convergence ability increases the effectiveness of orthoptic therapy (AOBVOT compared to OBVOT). Nevertheless, further large-scale studies with longer follow-up periods are warranted to evaluate these methods and findings.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Cooper J, Jamal N. Convergence insufficiency – A major review. Optometry. 2012;83:137–158. [PubMed] [Google Scholar]
- 2.Scheiman M, Mitchell GL, Cotter S, Kulp MT, Cooper J, Rouse M, et al. A randomized clinical trial of vision therapy/orthoptics versus pencil pushups for the treatment of convergence insufficiency in young adults. Optom Vis Sci. 2005;82:583–595. doi: 10.1097/01.opx.0000171331.36871.2f. [DOI] [PubMed] [Google Scholar]
- 3.Convergence Insufficiency Treatment Trial Study Group. Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Arch Ophthalmol. 2008;126:1336–1349. doi: 10.1001/archopht.126.10.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Porcar E, Martinez-Palomera A. Prevalence of general binocular dysfunctions in a population of university students. Optom Vis Sci. 1997;74:111–113. doi: 10.1097/00006324-199702000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Rouse MW, Hyman L, Hussein M, Solan H. Frequency of convergence insufficiency in optometry clinic settings. Convergence Insufficiency and Reading Study (CIRS) Group. Optom Vis Sci. 1998;75:88–96. doi: 10.1097/00006324-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Rouse MW, Borsting E, Hyman L, Hussein M, Cotter SA, Flynn M, et al. The Convergence Insufficiency and Reading Study (CIRS) group. Frequency of convergence insufficiency among fifth and sixth graders. Optom Vis Sci. 1999;76:643–649. doi: 10.1097/00006324-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Birnbaum MH, Soden R, Cohen AH. Efficacy of vision therapy for convergence insufficiency in an adult male population. J Am Optom Assoc. 1999;70:225–232. [PubMed] [Google Scholar]
- 8.Grisham JD. Visual therapy results for convergence insufficiency: A literature review. Am J Optom Physiol Opt. 1988;65:448–454. doi: 10.1097/00006324-198806000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Chin B, Faibish B, Hisaka C, Thal L, Tsuda K. A survey of the treatment of convergence insufficiency by optometrists in the greater San Francisco Bay area. J Beh Optom. 1995;6:91–2,109. [Google Scholar]
- 10.Scheiman M, Cooper J, Mitchell GL, de LP, Cotter S, Borsting E, et al. A survey of treatment modalities for convergence insufficiency. Optom Vis Sci. 2002;79:151–157. doi: 10.1097/00006324-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Scheiman M, Mitchell GL, Cotter S, Kulp MT, Cooper J, Rouse M, et al. A randomized clinical trial of vision therapy/orthoptics versus pencil pushups for the treatment of convergence insufficiency in young adults. Optom Vis Sci. 2005;82:583–595. doi: 10.1097/01.opx.0000171331.36871.2f. [DOI] [PubMed] [Google Scholar]
- 12.Gallaway M, Scheiman M, Malhotra K. The effectiveness of pencil pushups treatment for convergence insufficiency: A pilot study. Optom Vis Sci. 2002;79:265–267. doi: 10.1097/00006324-200204000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Convergence Insufficiency Treatment Trial Study Group. Long-term effectiveness of treatments for symptomatic convergence insufficiency in children. Optom Vis Sci. 2009;86:1096–1103. doi: 10.1097/OPX.0b013e3181b6210f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scheiman M, Cotter S, Rouse M, Mitchell GL, Kulp M, Cooper J, et al. Convergence Insufficiency Treatment Trial Study Group. Randomised clinical trial of the effectiveness of base-in prism reading glasses versus placebo reading glasses for symptomatic convergence insufficiency in children. Br J Ophthalmol. 2005;89:1318–1323. doi: 10.1136/bjo.2005.068197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borsting EJ, Rouse MW, Mitchell GL, Scheiman M, Cotter SA, Cooper J, et al. Validity and reliability of the revised convergence insufficiency symptom survey in children aged 9 to 18 years. Optom Vis Sci. 2003;80:832–838. doi: 10.1097/00006324-200312000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Rouse M, Borsting E, Mitchell GL, Cotter SA, Kulp M, Scheiman M, et al. Convergence Insufficiency Treatment Trial (CITT) Investigator Group. Validity of the convergence insufficiency symptom survey: A confirmatory study. Optom Vis Sci. 2009;86:357–363. doi: 10.1097/OPX.0b013e3181989252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horan LA, Ticho BH, Khammar AJ, Allen MS, Shah BA. Is the convergence insufficiency symptom survey specific for convergence insufficiency? A prospective, randomized study. Am Orthopt J. 2015;65:99–103. doi: 10.3368/aoj.65.1.99. [DOI] [PubMed] [Google Scholar]


