INTRODUCTION
Chronic kidney disease (CKD) is a common condition, with an estimated prevalence in the UK of around 5–7%,1,2 and a GP recorded prevalence in the England Quality and Outcomes Framework (QOF) in 2017 of 4.1%,3 which is higher than the prevalence of coronary heart disease.
The majority of people with CKD are detected and managed in primary care rather than by kidney specialists. Early identification in primary care, particularly among populations with risk factors such as diabetes and hypertension, enables appropriate management of blood pressure, cardiovascular risk and lifestyle factors. There is evidence that progression of CKD can be delayed by such interventions,4 and that implementation of these interventions can be improved by use of quality improvement tools in primary care.5
However CKD as a long-term condition has not had an easy ride. Since its definition in 2002 there have been concerns about overdiagnosis, described as ‘when people without symptoms are diagnosed with a disease that ultimately will not cause them symptoms or early death’,6 and anxieties about the disclosure of early-stage CKD to patients, along with the work of reassurance and increased monitoring that this might entail.7,8 This debate within general practice has left some practitioners uncertain about the importance of naming, coding and managing CKD in primary care.
THE NATIONAL CHRONIC KIDNEY DISEASE AUDIT
This national audit, commissioned by the Healthcare Quality Improvement Partnership (HQIP) in 2014 as part of the National Clinical Audit and Patient Outcomes Programme, was designed to improve the identification and management of CKD in primary care. The audit included data from over 1000 practices in England and Wales, producing the largest sample of patients with CKD globally, the dataset for analysis of hospital outcomes included over 400 000 records of patients with CKD. Alongside data extraction to examine practice performance against NICE guidance and quality standards,9,10 an electronic quality improvement tool was developed. This provided in-consultation prompts, and practice lists of people who might benefit from attention to blood pressure management and other key interventions for CKD.
Part one of the audit report had a focus on findings relating to CKD identification, diagnostic coding, and management in primary care.1 The audit found high rates of regular testing among people with diabetes — no doubt a result of the reminders and incentives provided by QOF — this finding was in contrast to lower testing rates for those with hypertension in spite of a similar or higher prevalence of CKD among this population. Less than 30% of those with hypertension had urinary testing for albumin to creatinine ratio (ACR), a marker for higher risk of cardiovascular disease and more rapid CKD progression, and hence a reminder of the need for regular review and to manage blood pressure to tighter targets.
Across the 1000 audit practices, rates of diagnostic coding for CKD showed wide variation, with a range of 20% to 100% of biochemically identifiable cases. Of some concern was the finding that younger people (those aged <60 years) who had biochemical evidence of CKD had lower rates of CKD coding than those aged >60 years. These younger patients, particularly those with diabetes, have perhaps the most to gain from regular CKD review, an offer of treatment with statin, and control of blood pressure.
The second part of the audit, published in December 2017, looked at the outcomes of people with CKD, including emergency hospital admission, rates of acute kidney injury at hospital admission (AKI) and death.11
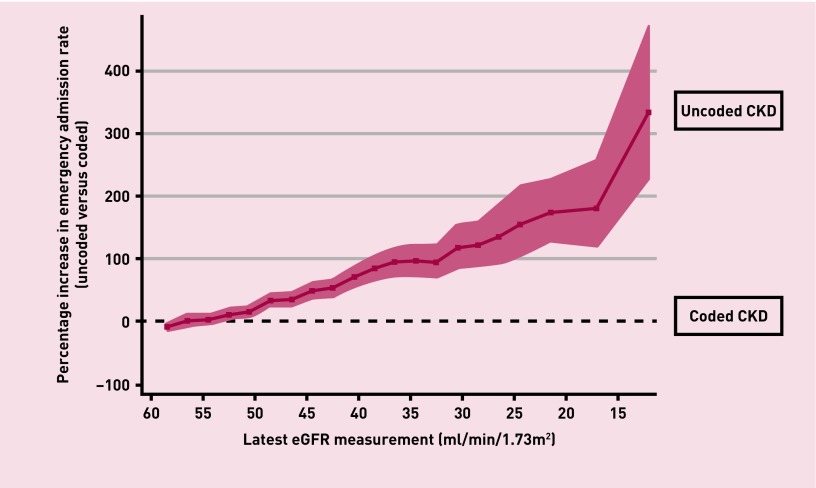
The rates of unplanned hospital admission, for all causes, increase sharply with a progressive fall in eGFR value such that patients with stage 4 CKD have around twice the unplanned hospital admission rate of those with stage 3 CKD. By using the linked data from primary and secondary care records the audit was also able to show that emergency hospital admission is more likely among people with biochemical evidence of CKD when this has not been previously coded in primary care. The magnitude of this difference in admission rates between coded and uncoded patients increases as kidney function declines, with twice the admission rates between coded and uncoded cases as the eGFR declines below 35ml/min (Figure 1).
Figure 1.
Comparison of emergency admissions between uncoded and coded patients with biochemical CKD stages 3–5 (using rate ratios). All rates are adjusted by age, sex, diabetes, hypertension, and cardiovascular disease.
Admission rates for acute kidney injury (AKI) showed a fourfold rise as CKD status declines from stage 3 to stage 4. Similar evidence was found to suggest that CKD coding is associated with lower rates of admission. Mortality rates showed a broadly similar pattern.
These observations of associations between CKD coding and unplanned hospital admissions is intriguing and important. For the present it needs treating with some caution, as the National Chronic Kidney (NCKD) database did not include data on all primary care coded comorbidities, and some important attributes that contribute to morbidity such as patient frailty, are currently not well captured by coded data. Further studies using a range of primary care and hospital linked data are needed to address these questions, and establish whether there is a causal link between improving rates of diagnostic coding and adverse events including emergency admission and death.
IMPLICATIONS FOR PRACTICE
The audit recommendations include a call to general practice to identify and test patients at risk, and where there is evidence of CKD stages 3–5 to improve the coding and regular review of these patients. There is good evidence, both from the national audit and from other studies, that coding is associated with improvements in the process of care. The benefits include managing blood pressure to target, the prescription of statins for primary prevention of cardiovascular disease, monitoring urinary proteinuria, and provision of flu and pneumococcal immunisation.12,13 Disease coding in primary care is a proxy for increased clinical scrutiny and informed clinical decision making with these patients, who often have a range of other comorbidities which increase their vulnerability to AKI and their likelihood of unplanned hospital admission. Although the national audit did not include data on medications that are potentially harmful to the kidneys such as non-steroidal anti-inflammatory medications (NSAID) there are important links between coding for CKD and safe prescribing. Some, but not all, GP computer systems link prescribing alerts to coded diagnoses — hence the benefits of these safety alerts are not available to uncoded patients.
ACHIEVING CHANGE
The national CKD audit highlights the wide variation between practices in their rates of CKD coding and the clinical management associated with best delivery of primary care. Many practices already use audit tools to monitor and improve their performance; others may need additional support or incentives to compare their performance with others and raise their game. Clinical commissioning groups and local health boards have an important role in providing the tools and resources to support this activity, which will provide direct benefits for patient care and are likely to result in decreased rates of hospital admission for this vulnerable group of patients.
Provenance
Commissioned; not externally peer reviewed.
Competing interests
The authors have declared no competing interests.
REFERENCES
- 1.Nitsch D, Caplin B, Hull SA, et al. National Chronic Kidney Disease Audit: National Report (Part 1) 2017. Healthcare Quality Improvement Partnership. 2017.
- 2.Iwagami M, Tomlinson LA, Mansfield KE, et al. Validity of estimated prevalence of decreased kidney function and renal replacement therapy from primary care electronic health records compared with national survey and registry data in the United Kingdom. Nephrol Dial Transplant. 2017;32(suppl 2):ii142–ii50. doi: 10.1093/ndt/gfw318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quality and Outcomes Framework. QOF 2016/17 results. NHS Digital; 2017. [Google Scholar]
- 4.Lv J, Ehteshami P, Sarnak MJ, et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ. 2013;185(11):949–957. doi: 10.1503/cmaj.121468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lusignan S, Gallagher H, Jones S, et al. Audit-based education lowers systolic blood pressure in chronic kidney disease: the Quality Improvement in CKD (QI CKD) trial results. Kidney Int. 2013;84(3):609–620. doi: 10.1038/ki.2013.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Treadwell J, McCartney M. Overdiagnosis and overtreatment: generalists--it’s time for a grassroots revolution. Br J Gen Pract. 2016. . [DOI] [PMC free article] [PubMed]
- 7.Blakeman T, Protheroe J, Chew-Graham C, et al. Understanding the management of early- stage chronic kidney disease in primary care: a qualitative study. Br J Gen Pract. 2012. . [DOI] [PMC free article] [PubMed]
- 8.Daker-White G, Rogers A, Kennedy A, et al. Non-disclosure of chronic kidney disease in primary care and the limits of instrumental rationality in chronic illness self-management. Soc Sci Med. 2015;131:31–39. doi: 10.1016/j.socscimed.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence . Chronic kidney disease: (partial update) early identification and management of chronic kidney disease in adults in primary and secondary care. NICE; 2014. [PubMed] [Google Scholar]
- 10.National Institute for Health and Care Excellence . Chronic kidney disease in adults: Quality standard. NICE; 2011. [PubMed] [Google Scholar]
- 11.Cleary F, Kim LG, Caplin B, et al. National Chronic Kidney Disease Audit. National Report (Part 2) 2017. Healthcare Quality Improvement Partnership; 2017. [Google Scholar]
- 12.Jain P, Calvert M, Cockwell P, McManus RJ. The need for improved identification and accurate classification of stages 3–5 Chronic Kidney Disease in primary care: retrospective cohort study. PloS One. 2014;9(8):e100831. doi: 10.1371/journal.pone.0100831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim LG, Cleary F, Wheeler DC, et al. How do primary care doctors in England and Wales code and manage people with chronic kidney disease? Results from the National Chronic Kidney Disease Audit. Nephrology, dialysis, transplantation. 2017 doi: 10.1093/ndt/gfx280. [DOI] [PMC free article] [PubMed] [Google Scholar]