We report a novel form of autosomal dominant variant Glanzmann thrombasthenia (GT) with, unlike all previously reported cases, the proband showing compound heterozygosity for two ITGB3 variants. Expression studies in CHO cells of the two previously undescribed ITGB3 variants, and studies in megakaryocytes cultured from peripheral blood-derived CD34+ cells, show that gain-of-function ITGB3 variants exert a dominant effect over normal or loss-of-function ITGB3 variants, leading to the clinical picture of autosomal dominant GT.
Classical GT is a rare autosomal recessive disorder characterized by the absence of platelet aggregation with normal platelet number and volume, usually associated with severe mucocutaneous bleeding. GT is caused by variants in the ITGA2B and ITGB3 genes that encode, respectively, for the αIIb and the β3 subunits of integrin αIIbβ3, the most abundant platelet surface receptor.1 Integrin αIIbβ3 is exposed on resting platelets in an inactive conformation and it assumes an active conformation, able to bind its ligands, upon platelet activation by a mechanism named inside-out signaling. In turn, ligand-binding triggers outside-in signaling, with phosphorylation of the β3 cytoplasmic tail, and activation of Src-family kinases and Focal Adhesion Kinase (FAK), leading to cytoskeletal remodeling and consequently to platelet aggregation.2
Recently, an autosomal dominant form of GT, associated with platelet dysfunction, mild macrothrombocytopenia, and mild to severe hemorrhagic manifestations, has been included as a new entity in the list of hereditary platelet disorders.3 Autosomal dominant GT is caused by gain-of-function variants of ITGA2B or ITGB3 that generate a constitutively activated αIIbβ3 locked in a high affinity state.
We recently showed that constitutively activated αIIbβ3 is associated with αIIbβ3 internalization and to an altered cytoskeletal reorganization that is the main effector of platelet dysfunction.4 Abnormal cytoskeletal remodeling is also responsible for the macrothrombocytopenia, due to impaired proplatelet formation with the generation of a reduced number of abnormally large proplatelet tips.5
Here we describe a novel case of variant GT which phenotypically seemed to be autosomal dominant, but in which we found co-inheritance of two previously undescribed heterozygous ITGB3 variants, a genotype suggesting the classic form of GT. Expression studies in CHO cells, however, showed that one of these is a gain-of-function variant, exerting a dominant effect over both the normal and the dysfunctional β3, thus explaining the autosomal dominant GT phenotype of the family.
Platelet diameter and ultrastructure were assessed by transmission electron microscopy,6 while platelet volume distribution was evaluated on blood smears.7 Platelet function was assessed by impedance aggregometry, while αIIbβ3 expression and activation and αvβ3 expression were assessed by flow cytometry.6 To identify DNA variants, all exons of ITGA2B and ITGB3 were analyzed by Sanger sequencing.8 Megakaryocytes were cultured from CD34+ cells separated from peripheral blood5 and proplatelet formation was studied by immunofluorescence.4,5 To evaluate the functional impact of the novel variants, mutant β3 expression vectors were generated by site-directed mutagenesis9 and transfected into CHO cells stably expressing αIIb.4 αIIbβ3 expression, activation and internalization, and actin polymerization were assessed by flow cytometry.4,6 For the adhesion assay, CHO cells or platelets were layered onto fibrinogen-coated glass coverslips, May-Grunwald-Giemsa staining was performed, and samples were analyzed by optical microscopy.4,6 FAK phosphorylation was assessed by western blotting.5 Data are expressed as means±Standard Deviation. Additional details on methods and statistical analyses are provided in the Online Supplementary Appendix.
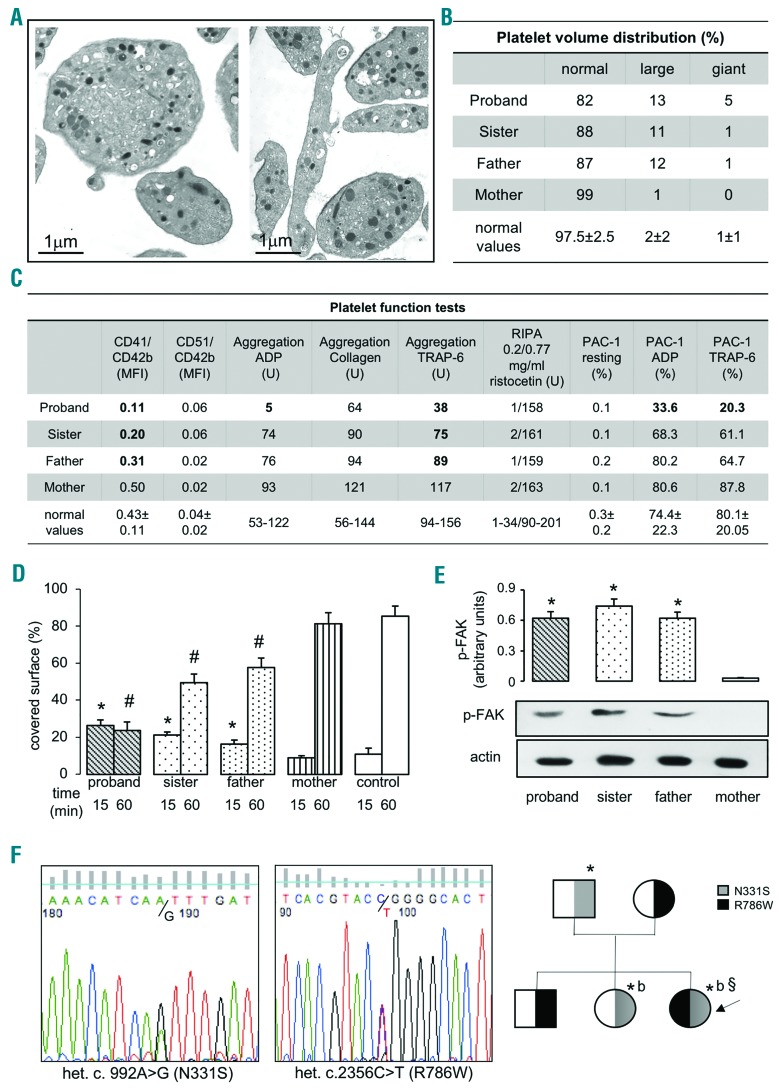
The proband was a 27-year old Danish woman with a lifelong mild bleeding history, with large skin bruises which occurred spontaneously or after minor trauma, prolonged bleeding from minor wounds and after tooth extraction [ISTH-Bleeding Assessment Tool (ISTH-BAT) bleeding score: 5]. Her platelet count was mildly reduced (64–90×109/L) and mean platelet volume (MPV) increased (13 fL, normal 8–12). Electron microscopy and analysis of May-Grünwald-stained blood smears showed increased mean platelet diameter, and platelet anisocytosis (Figure 1A and B). Platelet aggregation was impaired in response to all stimuli, except ristocetin, with low-normal response to collagen. αIIbβ3 surface expression was reduced, and PAC-1 binding induced by platelet stimulation, a measure of αIIbβ3 activation, impaired (Figure 1C). Her father and sister also showed macrothrombocytopenia (father: platelets 95×109/L, MPV 12.8 fL; sister: platelets 91×109/L, MPV 12.7 fL), but while her sister showed spontaneous subcutaneous hematomas (ISTH-BAT bleeding score: 3), her father did not show any bleeding symptoms but reported a family history of bleeding diathesis. Her mother and brother did not show any bleeding symptoms or macrothrombocytopenia. Platelet function of the family members is summarized in Figure 1C. Platelets from the proband, her father and her sister showed increased early spreading on fibrinogen, but reduced spreading at later time points4 (Figure 1D), together with FAK phosphorylation in unstimulated platelets (Figure 1E).
Figure 1.
Platelet morphology and genetic analysis. (A) Representative images of the proband’s platelets analyzed by transmission electron microscopy showing heterogeneity of platelet size and shape and the presence of large platelets (mean platelet volume: 4.23±1.23 vs. 2.58±0.72 μm; P<0.0001). Some of the largest platelets showed internal membrane complexes and heterogeneous granule distribution. (B) Distribution of platelet volumes; 100 platelets were evaluated for each blood smear. Normal values are expressed as mean±Standard Deviation. (C) All the tests carried out on platelets of the family members. Abnormal values are in bold. CD41 and CD51 expression has been corrected for platelet volume by calculating the ratio MFI clone/MFI CD42b. The brother was not available for further studies. Normal values are expressed as mean±SD, except for multiplate multiple electrode aggregometry for which reference ranges are shown. (D) Spreading of platelets after 15 or 60 minutes (mins) of adhesion to fibrinogen-coated plastic coverslips (*significantly increased vs. control 60 mins; #significantly decreased vs. control 60 mins; P=0.05). (E) Focal Adhesion Kinase (FAK) phosphorylation of platelets in suspension; densitometric analysis was performed using the Image J software (*significantly increased vs. mother; P<0.05 vs. mother). (F) Sequencing analysis of DNA from the proband, showing the two heterozygous nucleotide substitutions: c. 992A>G in exon 7 of ITGB3 leading to N331S and c.2356C>T in exon 15 of ITGB3 leading to R786W. Pathogenicity was predicted using the Sift and PolyPhen softwares. PolyPhen assigned “probably damaging” with a score of 1/1 to R786W and with a score of 0.097/1 to N331S. Sift assigned “deleterious” with a score of −3.653 (cut off: −2.5) to R786W and “Neutral” with a score of −2.191 to N331S. Pedigree of the family. and ○: male and female family members, respectively. Heterozygous for R786W: [Image]; heterozygous for N311S: [Image]; compound heterozygous for the two variants: [Image]. The arrow indicates the proband, compound heterozygous for the two variants. *Macrothrombocytopenia, reduced αIIbβ3 expression. b: bleeding. §Defective aggregation and αIIbβ3 activation.
Based on the clinical and platelet phenotype, we suspected autosomal dominant GT.3,4
Surprisingly, DNA analysis of the proband showed compound heterozygosity for two novel ITGB3 missense variants: c.2356C>T leading to R786W, affecting the β3 cytoplasmic tail, and c. 992A>G leading to N331S, affecting the β-I-like domain of the β3 globular head (Figure 1F), while heterozygosity for R786W was found in the mother and brother, and heterozygosity for N331S in the father and sister (Figure 1F). These novel variants were not present in the ExAC control dataset or in 50 healthy control subjects, nor in the disease-associated databases ClinVar and Ensembl. The identification of compound heterozygosity for two ITGB3 variants did not seem to support the diagnosis of autosomal dominant GT.
To solve the dilemma, we assessed the functional impact of the two novel ITGB3 variants by expressing them in αIIb-bearing CHO cells, either alone (CHO-N331S and CHO-R786W), or in combination (CHO-N331S/R786W), thus replicating the proband’s phenotype, or together with wild-type β3 (CHO-N331S/WT and CHO-R786W/WT), thus replicating the phenotype of the other family members.
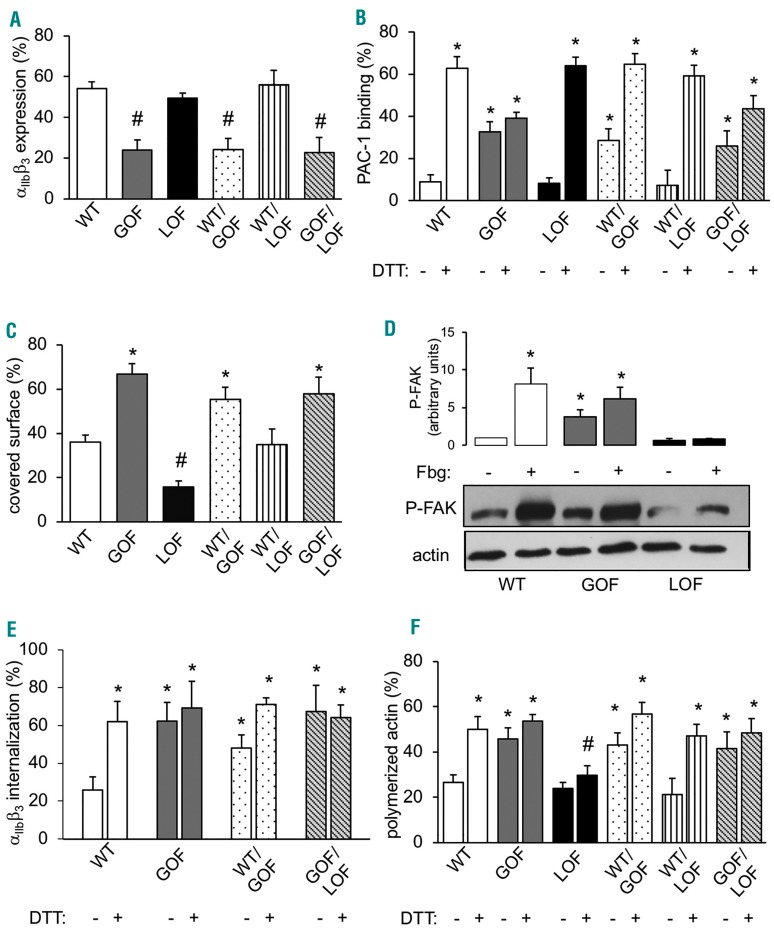
Expression studies revealed that R786W is a loss-of-function variant that does not affect αIIbβ3 expression (Figure 2A) or activation (Figure 2B), but causes impaired αIIbβ3 outside-in signaling, as shown by reduced CHO cell spreading (Figure 2C) and FAK phosphorylation on fibrinogen (Figure 2D). In contrast, N331S is a gain-of-function variant, inducing PAC-1 binding under resting conditions (Figure 2A) and triggering constitutive outside-in signaling, as shown by accelerated spreading on fibrinogen (Figure 2C) and by FAK phosphorylation under resting conditions (Figure 2D). Moreover, N331S impaired αIIbβ3 expression (Figure 2B) and enhanced αIIbβ3 internalization in unstimulated CHO cells (Figure 2E). This is in accordance with the platelet phenotype of family members expressing the N331S variant. In agreement with previous data showing that gain-of-function variants of β3 alter cytoskeletal reorganization, polymerized actin was increased in CHO cells expressing N331S and it did not increase further after treatment with dithiothreitol (Figure 2F).
Figure 2.
αIIbβ3 expression and function in CHO cells. (A) αIIbβ3 expression measured by flow cytometry in CHO cells expressing wild-type (WT) β3 and/or gain-of-function (GOF) or loss-of-function (LOF) β3 variants in different combinations (#significantly decreased vs. WT; n=8; P<0.05). (B) PAC-1 binding measured by flow-cytometry in CHO cells expressing WT β3 and/or gain-of-function (GOF) or loss-of-function (LOF) β3 variants in different combinations. Full αIIbβ3 activation was obtained by incubation with DTT (25 mM) (*significantly increased vs. WT resting; n=8; P<0.01). (C) Spreading of WT and mutant β3-expressing CHO cells after 15 minutes of adhesion to fibrinogen-coated plastic coverslips (*significantly increased vs. WT; #significantly decreased vs. WT; n=5; P<0.05). (D) Focal Adhesion Kinase (FAK) phosphorylation of WT and mutant integrin β3-expressing CHO cells in suspension (-) and after adhesion to fibrinogen (+). Densitometric analysis was performed using the Image J software (*significantly increased vs. WT-; n=5; P<0.05). (E) Internalized αIIbβ3 in WT CHO cells and mutant CHO cells expressing wild-type αIIbβ3 and N331S β3, alone or in combination with WT or R786W β3, treated or not with dithiothreitol (DTT) (*significantly increased vs. WT resting; n=3; P<0.05). (F) Polymerized actin (F-actin) content of WT and of different mutant β3-expressing CHO cells measured by flow cytometry before and after stimulation with DTT (25 mM) (*significantly increased vs. WT; #significantly decreased vs. WT; n=5; P<0.05).
Of note, when co-expressed with normal β3 or R786W, N331S exerted a dominant-negative effect producing impaired αIIbβ3 surface expression, increased internalization, PAC-1 binding under resting conditions, accelerated spreading and increased actin polymerization (Figure 2A–F).
We previously showed that gain-of-function β3 mutants exert a dominant effect over normal β3 thus being the main effector of platelet dysfunction in heterozygous variant GT.4 Here, we show that a gain-of-function mutation in the β-I-like domain of β3 can exert its dominant-negative effect even when associated with a loss-of-function β3 mutant on the second allele, giving rise to the clinical picture of autosomal dominant GT despite compound heterozygosity.
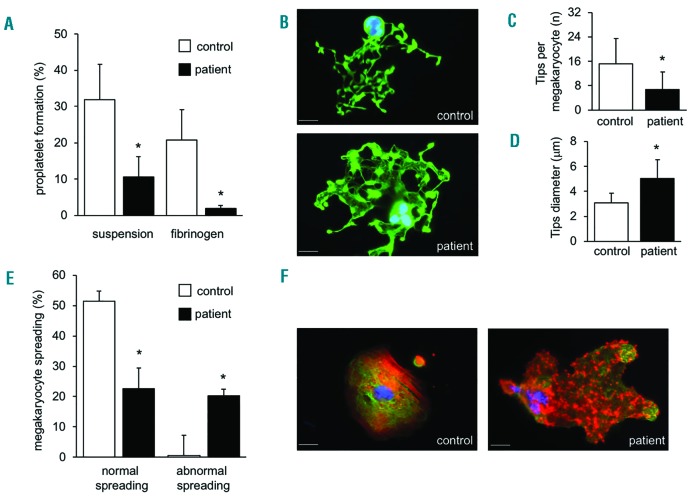
In agreement with previous observations, megakaryocytes cultured from peripheral blood-derived CD34+ cells showed normal maturation (CD41+ cells: controls 12.6+4.1%, patient 10.4+2.3%), but severely impaired proplatelet formation (Figure 3A and B), with tips decreased in number and larger in size than those of controls (Figure 3C and D). Moreover, megakaryocytes adhered normally to fibrinogen (control 43.6±10.1%, patients 45.1±13.2%) but displayed abnormal spreading, with disordered actin distribution5 (Figure 3E and F). The present observations strengthen our previous conclusion that the expression of a constitutively active αIIbβ3 in megakaryocytes leads to impaired proplatelet formation.5
Figure 3.
Megakaryocyte spreading and proplatelet formation. (A) Proplatelet formation from megakaryocytes at day 14 of culture in suspension or after 16 hours (h) of adhesion to fibrinogen (*P<0.05 vs. control). (B) Representative images of proplatelet formation. Microtubules were stained green with a rabbit anti-human β1-tubulin antibody and a secondary AlexaFluor488 conjugated antibody; nuclei were stained blue with Hoechst. (C) Number of proplatelet tips generated by megakaryocytes (*P<0.05 vs. control). (D) Diameter of proplatelet tips generated by megakaryocytes (*P<0.05 vs. control). (E) Spreading of megakaryocytes after 6 h of incubation on immobilized fibrinogen. Two populations of megakaryocytes were visible: half of the population spread regularly, while half showed abnormal spreading, with disordered distribution of actin and focal adhesion points more evident than stress fibers. (F) Representative image of megakaryocytes spreading on fibrinogen. Microtubules were stained green with a rabbit anti-human β1-tubulin antibody and a secondary AlexaFluor488 conjugated antibody; actin was stained red with TRITC-phalloidin, nuclei were stained blue with Hoechst. Scale bar=20 μm.
N331S is, to our knowledge, the first ITGB3 gain-of-function variant associated with macrothrombocytopenia that affects the globular head of β3 while all the previously described gain-of-function variants involved the EGF3,10 βTD6,11 and cytoplasmic12,13 domains of β3. Previous mutagenesis studies showed that the introduction of an N339S aminoacid substitution in the a7-helix of the β-I-like domain of β3 (the same domain affected by the N331S variant of our patient) causes αIIbβ3 activation, suggesting that asparagines located in this domain may have a primary role in keeping the integrin in a resting state.14
R786W affects the third-last aminoacid of the β3 cytoplasmic tail. Significantly, R786 is the arginine of the COOH-terminal RGT sequence crucial for triggering FAK phosphorylation and outside-in signaling,15 thus R786W causes impaired outside-in signaling.
This is the first case of variant GT associated with macrothrombocytopenia caused by co-inheritance of a loss-of-function and a gain-of-function ITGB3 variant. The gain-of-function variant is the main cause of the phenotype, dominating over the loss-of-function mutant β3 and explains macrothrombocytopenia and reduced αIIbβ3 expression. The heterogeneity of the platelet and bleeding phenotype within this family is in line with previous reports of autosomal dominant GT, including cases with normal10 or defective6,11–13 aggregation, and constitutively activated10,12 or inactive6 αIIbβ3 under resting conditions. For instance, a near normal or only slightly defective aggregation in response to collagen has been previously described in autosomal-dominant GT.6
In conclusion, starting from an apparent mismatch between genotype and phenotype, we confirm the central role of gain-of-function β3 variants in determining platelet dysfunction and macrothrombocytopenia in GT.
Supplementary Material
Acknowledgments
The authors thank Prof. Sisse Rye Ostrowsky (Department of Clinical Immunology, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark) for flow cytometry analysis of patients’ platelets and Dr. Paquita Nurden for electron microscopy preparations.
Footnotes
Funding: this work was supported in part by grants to PG from Telethon foundation (protocol # GGP10155 and protocol #GGP15063) and by a fellowship to EF from Fondazione Umberto Veronesi.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Gresele P, Bury L, Falcinelli E. Inherited platelet function disorders: algorithms for phenotypic and genetic investigation. Semin Thromb Hemost. 2016;42(3):292–305. [DOI] [PubMed] [Google Scholar]
- 2.Coller BS. αIIbβ3: structure and function. J Thromb Haemost. 2015;13 Suppl 1:S17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nurden AT, Pillois X, Fiore M, Heilig R, Nurden P. Glanzmann thrombasthenia-like syndromes associated with macrothrombocytopenias and mutations in the genes encoding the αIIbβ3 integrin. Semin Thromb Hemost. 2011;37(6):698–706. [DOI] [PubMed] [Google Scholar]
- 4.Bury L, Falcinelli E, Chiasserini D, Springer TA, Italiano JE, Jr, Gresele P. Cytoskeletal perturbation leads to platelet dysfunction and thrombocytopenia in variant forms of Glanzmann thrombasthenia. Haematologica. 2016;101(1):46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bury L, Malara A, Gresele P, Balduini A. Outside-in signalling generated by a constitutively activated integrin αIIbβ3 impairs proplatelet formation in human megakaryocytes. PLoS One. 2012;7(4):e34449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gresele P, Falcinelli E, Giannini S, et al. Dominant inheritance of a novel integrin β3 mutation associated with a hereditary macrothrombocytopenia and platelet dysfunction in two Italian families. Haematologica. 2009;94(5):663–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balduini CL, Cattaneo M, Fabris F, et al. Inherited thrombocytopenias: a proposed diagnostic algorithm from the Italian Gruppo di Studio delle Piastrine. Haematologica. 2003;88(5):582–592. [PubMed] [Google Scholar]
- 8.Bafunno V, Bury L, Tiscia GL, et al. A novel congenital dysprothrombinemia leading to defective prothrombin maturation. Thromb Res 2014;134(5):1135–1141. [DOI] [PubMed] [Google Scholar]
- 9.Sebastiano M, Momi S, Falcinelli E, Bury L, Hoylaerts MF, Gresele P. A novel mechanism regulating human platelet activation by MMP-2-mediated PAR1 biased signaling. Blood. 2017;129(7):883–895. [DOI] [PubMed] [Google Scholar]
- 10.Ghevaert C, Salsmann A, Watkins NA, et al. A nonsynonymous SNP in the ITGB3 gene disrupts the conserved membrane-proximal cytoplasmic salt bridge in the αIIbβ3 integrin and cosegregates dominantly with abnormal proplatelet formation and macrothrombocytopenia. Blood. 2008;111(7):3407–3414. [DOI] [PubMed] [Google Scholar]
- 11.Vanhoorelbeke K, De Meyer SF, Pareyn I, et al. The novel S527F mutation in the integrin β3 chain induces a high affinity αIIbβ3 receptor by hindering adoption of the bent conformation. J Biol Chem. 2009;284(22):14914–14920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kashiwagi H, Kunishima S, Kiyomizu K, et al. Demonstration of novel gain-of-function mutations of αIIbβ3: association with macrothrombocytopenia and Glanzmann thrombasthenia-like phenotype. Mol Genet Genomic Med. 2013;1(2):77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jayo A, Conde I, Lastres P, et al. L718P mutation in the membrane-proximal cytoplasmic tail of β3 promotes abnormal αIIbβ3 clustering and lipid microdomain coalescence, and associates with a thrombasthenia-like phenotype. Haematologica. 2010;95(7):1158–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng M, Foo SY, Shi ML, et al. Mutation of a conserved asparagine in the I-like domain promotes constitutively active integrins αLβ2 and αIIbβ3. J Biol Chem. 2007;282(25):18225–18232. [DOI] [PubMed] [Google Scholar]
- 15.Arias-Salgado EG, Lizano S, Sarkar S, Brugge JS, Ginsberg MH, Shattil SJ. Src kinase activation by direct interaction with the integrin beta cytoplasmic domain. Proc Natl Acad Sci USA. 2003; 100(23): 13298–13302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.