Abstract
Objective
To investigate the effects of centralizing the acute stroke services in the Central Denmark Region (CDR).
Methods
The CDR (1.3 million inhabitants) centralized acute stroke care from 6 to 2 designated acute stroke units with 7-day outpatient clinics. We performed a prospective “before-and-after” cohort study comparing all strokes from the CDR with strokes in the rest of Denmark to discover underlying general trends, adopting a difference-in-differences approach. The population comprised 22,141 stroke cases hospitalized from May 2011 to April 2012 and May 2013 to April 2014.
Results
Centralization was associated with a significant reduction in length of acute hospital stay from a median of 5 to 2 days with a length-of-stay ratio of 0.53 (95% confidence interval 0.38–0.75, data adjusted) with no corresponding change seen in the rest of Denmark. Similarly, centralization led to a significant increase in strokes with same-day admission (mainly outpatients), whereas this remained unchanged in the rest of Denmark. We observed a significant improvement in quality of care captured in 11 process performance measures in both the CDR and the rest of Denmark. Centralization was associated with a nonsignificant increase in thrombolysis rate. We observed a slight increase in readmissions at day 30, but this was not significantly different from the general trend. Mortality at days 30 and 365 remained unchanged, as in the rest of Denmark.
Conclusions
Centralizing acute stroke care in the CDR significantly reduced the length of acute hospital stay without compromising quality. Readmissions and mortality stayed comparable to the rest of Denmark.
Stroke is one of the costliest health care conditions globally.1,2 In already overstretched health care budgets, efficient organization of stroke services is therefore essential to ensure high quality of care and the best possible outcomes for patients.
Organized stroke care provided by specialized multidisciplinary teams is associated with better quality and lesser risk of death and dependency.3–6 Furthermore, a higher patient volume at stroke units has been associated with improved quality of early stroke care, reduced length of stay, lower mortality, and reduced hospitalization costs.7–10 However, only a few studies have examined the effects of centralizing stroke care to fewer designated stroke units.11,12 Moreover, these studies may have been influenced by methodological limitations because they were conducted in selected urban populations without adjustment of clinical outcomes for stroke severity at stroke onset,2,13 and information on important aspects such as the use of acute reperfusion therapy rates14–17 and hospital readmissions has been missing.18,19 Increased funding may also have confounded the effects of centralization per se.20
The Central Denmark Region (CDR) implemented specialization and centralization of the acute stroke services in 2012 to ensure that all stroke patients would receive care in designated high-volume acute stroke units and to reduce overall costs.21 We investigated the effects of this reorganization.
Methods
System change
The acute stroke services reorganization in the CDR (≈1.3 million inhabitants in an area of 5,040 sq miles) implied that all acute stroke care was to be provided at only 2 designated acute stroke units in the CDR offering revascularization therapy (thrombolysis at both; endovascular therapy in 1 unit). Four other local hospitals with stroke units had provided acute stroke care before the reorganization, and patients would be admitted to the local hospital provided that they resided in its catchment area and were not candidates for acute revascularization therapy. For acute revascularization candidates, the reorganization meant no change. Three of the closed stroke units were “nonspecialized units” supervised by specialists in internal medicine. The reorganization reduced the total number of acute stroke beds in the CDR from 54 to 26.21 To meet treatment demand with only 2 dedicated stroke centers in the CDR, the centers established outpatient clinic for patients with suspected minor stroke (self-dependent although with neurologic symptoms) and TIA. The outpatient clinics were open 7 days a week during the daytime and staffed by an experienced neurovascular team. Patients needing in-hospital rehabilitation after the acute care could be transferred to a rehabilitation hospital unit or a local hospital 7 d/wk. The reorganization also implied setting up early-discharge home team care to improve patients' transition to stroke care in the community setting.
Centralization of the prehospital stroke code activation was part of the reorganization. In all suspected acute stroke cases, the general practitioner or prehospital service phoned an experienced neurologist who was available 24 h/d from either of the 2 high-volume acute stroke units. The stroke code was defined as acute focal neurologic deficits with no other obvious reasons than a possible cerebrovascular event. Regardless of whether patients were candidates for acute revascularization therapy, they were admitted directly to one of these units.
Outcomes
We investigated the effect of the reorganization from length of acute and total hospital stay, all-cause bed days, quality of and delays in acute stroke care, hospital readmissions, and mortality.
Admission length was counted as half rather than whole days when a patient died or was discharged from hospital on the day of admission. To ensure that the total length of the hospital stay included rehabilitation regardless of local organizational differences, admissions on the day after discharge were compiled in the total stay.
Nonacute hospital stay (total hospital stay - acute hospital stay) was defined as the total length of hospital stay spent in nonacute stroke care settings, including rehabilitation.
All-cause bed days were defined as the total number of days spent in hospital within the first year, including the total hospital stay of the initial stroke admission. To ensure that outpatient visits were not counted as part of all-cause bed days, only new admissions (acute/nonacute) ≥24 hours were included.
To be considered a readmission, at least 1 day was required between the day of discharge and the next admission date. Only acute admissions ≥24 hours were included. All admissions due to carotid artery surgery were excluded because they were considered part of the planned stroke care.
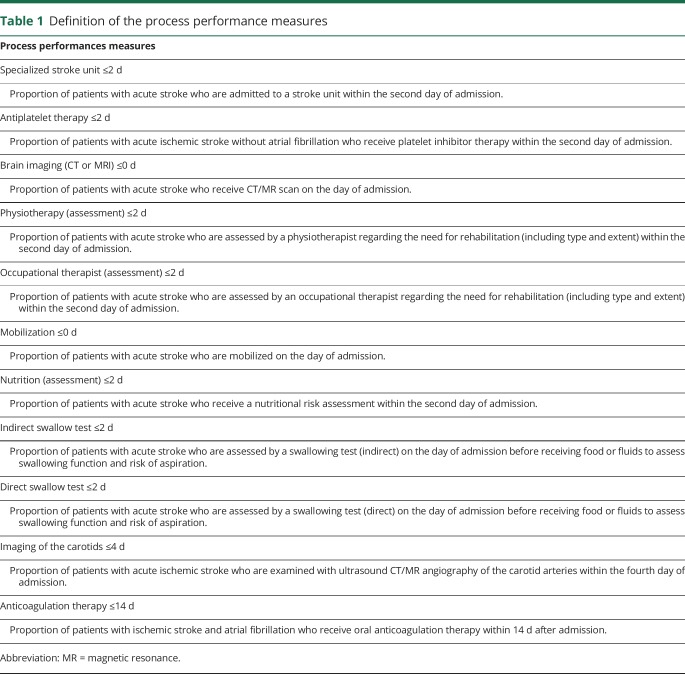
We evaluated quality of care using 11 clinical guideline-recommended process performance measures of acute stroke care (table 1). We defined “all-or-none” of the 11 measures as the proportion of stroke events involving all eligible measures for the individual patient. We evaluated the quality of the hyperacute phase from the ratio of all ischemic stroke events that received thrombolysis and the proportion of thrombolysed patients with a door-to-needle time <60 minutes. To evaluate hospital admission delay, we estimated the proportion of patients admitted within 4.5 hours from symptom onset.
Table 1.
Definition of the process performance measures
Study design
We conducted a prospective before-and-after cohort study using the rest of Denmark (≈4.3 million inhabitants) to compare for underlying general trends in stroke care and patient outcomes in a difference-in-differences (DID) approach. The “before” period was defined as the 12 months leading up to the reorganization (May 1, 2011–April 30, 2012), and the “after” period was defined as the 12-month period starting 1 year after initiation of the reorganization at which time the transition was considered to have been fully implemented (May 1, 2013–April 30, 2014).
We used the Danish Stroke Registry (DSR)22 to identify all stroke events. Reporting to the DSR is mandatory for all acute strokes (patients ≥18 years of age) at the hospital level. Given the Danish tradition of admitting almost all patients with acute stroke symptoms to hospital, virtually all acute stroke patients in Denmark are registered.23 The completeness of stroke event registration in the DSR exceeds 90%, and studies show that the DSR has a high validity.24 The DSR also provided information on baseline patient characteristics, length of acute hospital stay, and outcomes.
The Danish National Patient Register25 provided information on subsequent hospitalizations, including transfers from the acute stroke unit to in-hospital rehabilitation and readmissions.
The Danish Civil Registration System provided information on patients' vital status.26
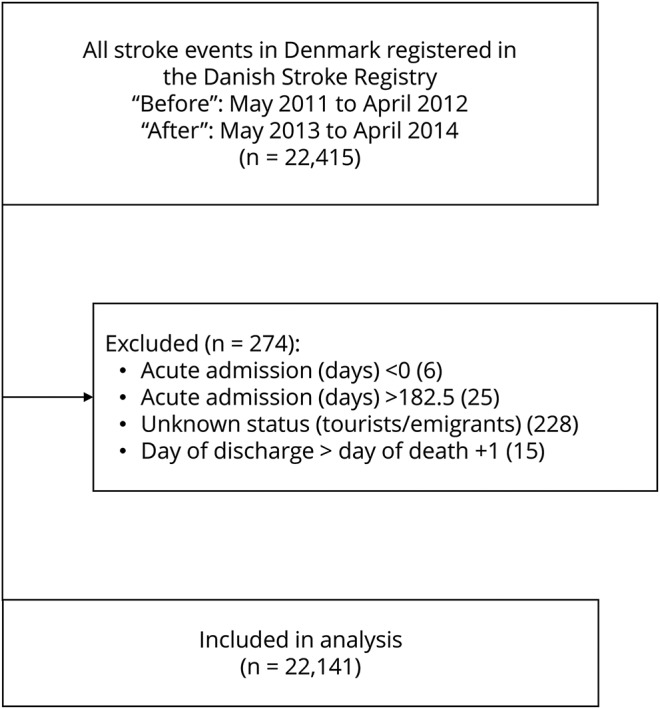
We restricted the population to individuals with stroke events with reliable data on length of acute hospital stay and a known vital status in the Danish Civil Registration System (figure).
Figure. Flowchart of the study population.
Statistical analysis
We compared outcomes from before and after the reorganization using regression methods based on the DID. The DID between the CDR and the rest of Denmark was estimated as an interaction term between period (before vs after) and region (CDR vs rest of Denmark).
The study was event based; i.e., individual patients could be included with several stroke episodes. Using multivariable models, we adjusted for age, sex, living arrangement, previous stroke, diabetes mellitus, atrial fibrillation, hypertension, smoking habits, alcohol use, stroke severity (Scandinavian Stroke Scale), and subtype of stroke. Missing information was encoded by an indicator variable and included in the analyses, except for patients with missing information on stroke severity, who were excluded from the multivariable models (missing information on stroke severity: 1,058 of 22,141 [4.8%]). Confidence intervals were based on robust standard errors adjusted for clustering within individual stroke units.
We determined the medians with interquartile range of the length of acute hospital stay, total hospital stay, and all-cause hospital bed day use within the first year. The data were severely right-skewed. We used a generalized linear model with a log-link and gamma distribution family to compare the length of stay ratios.
For readmissions, we compared hazard ratios (HRs) using multivariable Cox regression encountering the time of a potential readmission or death and analyzed mortality outcomes accordingly. We also calculated adjusted and unadjusted HRs.
For the clinical guidelines–recommended process performance measure, the time of admission and the rates and timing of thrombolysis were analyzed using binomial regression. Unadjusted risk ratios were calculated. We included only cases in which the health professionals caring for the individual patient had found the specific process measure to be relevant.
We used the Stata 13.0 package (StataCorp LP, College Station, TX) for all analyses.
Standard protocol approvals, registrations, and patient consents
The study was approved by the Danish Data Protection Agency (No. 1-16-02-213-15) and the Danish Clinical Registries. Under Danish law, registry-based studies require no ethics approval or patient consent.
According to Danish law, it is not possible to provide public access to the dataset, which is based on linkage of data from nationwide public registries. Access to Danish registry data can only be granted to individual researchers on seeking approval from the National Agency for Data Protection. It is therefore not possible to place the dataset in a public repository.
Results
After the exclusion of 1.2% of the identified stroke events, 22,141 cases remained in the study (figure). A total of 4,645 (21%) of all stroke events in Denmark occurred in the CDR during the study period. Of these, nonspecialized stroke units managed 603 (26%) events in the CDR before the reorganization.
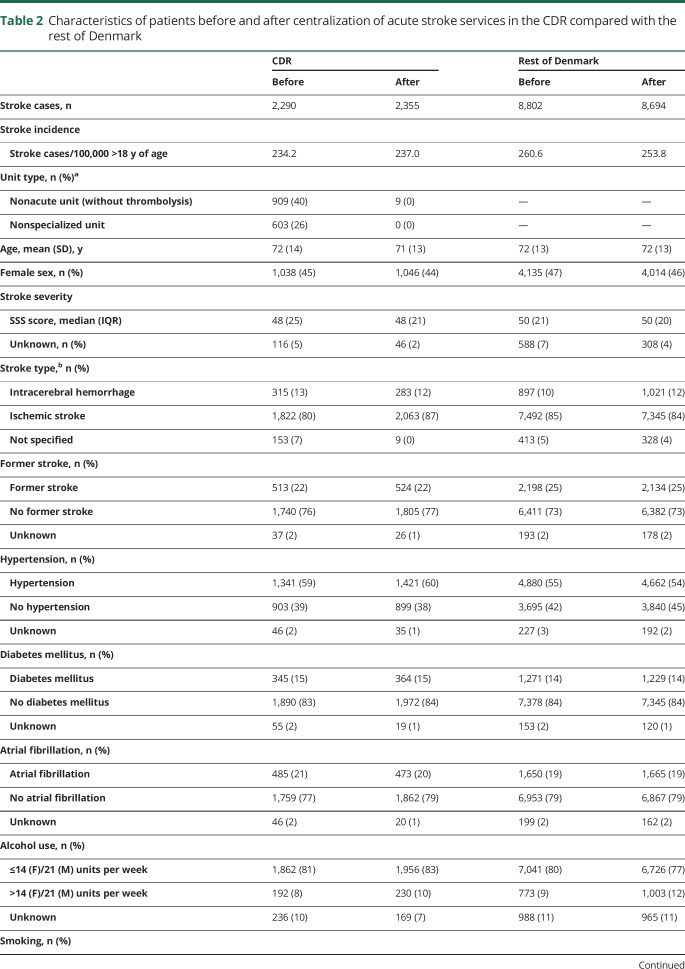
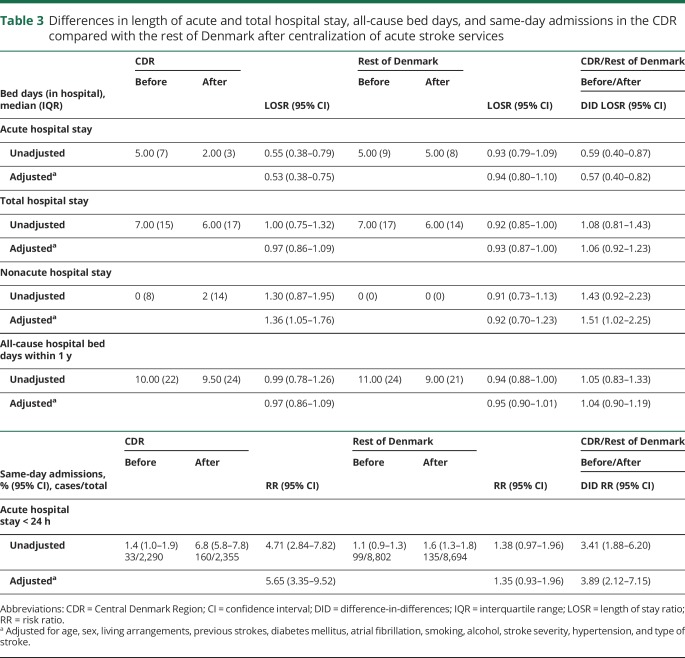
Baseline characteristics of the CDR patients compared with those recorded for the rest of Denmark in the before and after periods are shown in table 2. There were no substantial differences between the groups' baseline characteristics.
Table 2.
Characteristics of patients before and after centralization of acute stroke services in the CDR compared with the rest of Denmark
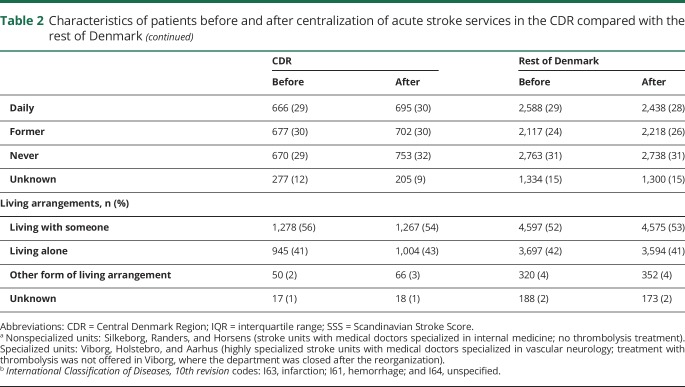
The study period saw a significant risk-adjusted reduction in the length of the acute hospital stay from a median of 5 to 2 days in the CDR (table 3). We saw no similar change in the rest of Denmark, for which the median acute hospital stay remained 5 days. Similarly, we observed a significant increase in the proportion of stroke events with a length of stay <24 hours (the majority being outpatients) in the CDR from 1.4% to 6.8%. In the rest of Denmark, this proportion increased only from 1.1% to 1.6%. The length of total stay, including rehabilitation and all-cause bed days, remained unchanged in the CDR and the rest of Denmark. The length of the total nonacute hospital stay, including rehabilitation, increased significantly in CDR but was unchanged in the rest of Denmark (table 3).
Table 3.
Differences in length of acute and total hospital stay, all-cause bed days, and same-day admissions in the CDR compared with the rest of Denmark after centralization of acute stroke services
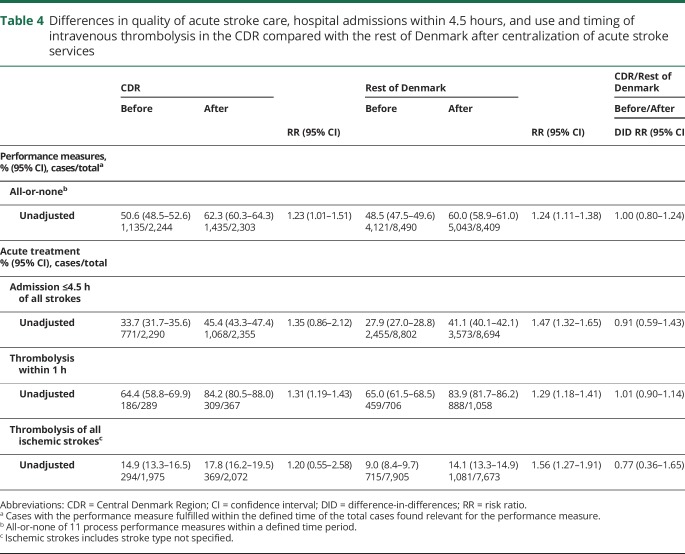
All-or-none of 11 process performance measures increased from 50.6% to 62.3% in the CDR, reflecting the proportion of stroke events for which all relevant process performance measures of acute stroke care were met. This corresponds to a similar increase from 48.5% to 60.0% in the rest of Denmark (table 4). Table 5 shows information on the included process performance measures.
Table 4.
Differences in quality of acute stroke care, hospital admissions within 4.5 hours, and use and timing of intravenous thrombolysis in the CDR compared with the rest of Denmark after centralization of acute stroke services
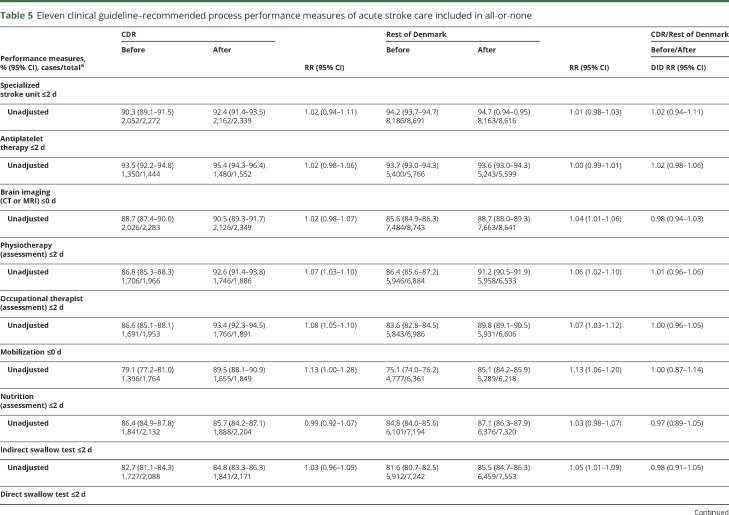
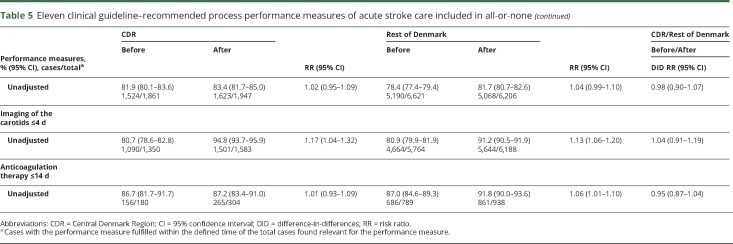
Table 5.
Eleven clinical guideline–recommended process performance measures of acute stroke care included in all-or-none
After the reorganization, the proportion of strokes admitted within 4.5 hours from stroke onset increased to 45.4% in the CDR and 41.1% in the rest of Denmark. The improvement in time delays for acute stroke service was comparable during this period (table 4).
Of all ischemic strokes, the rates of stroke cases receiving thrombolysis did not change significantly from 14.9% to 17.8% in the CDR in the study period, but we saw a significant increase from 9.0% to 14.1% in the rest of Denmark. Still, progress in the CDR and in the rest of Denmark did not differ significantly. The proportion of patients receiving thrombolysis within 1 hour of arrival rose significantly in the study period to ≈84% in both the CDR and in the rest of Denmark (table 4).
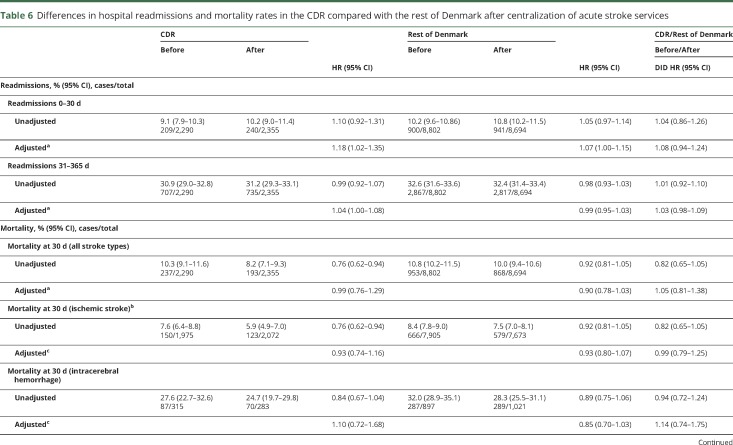
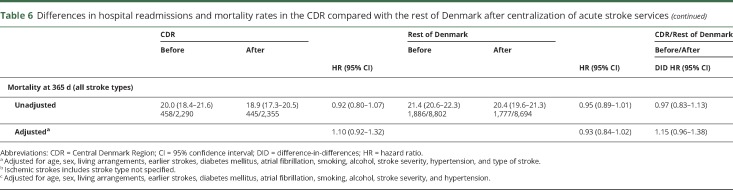
Readmissions within the first 30 days after discharge occurred in 10.2% in the “after” period of all strokes. Readmission risk increased significantly in the CDR, but this development was not significantly different from the trend seen in the rest of Denmark. Risk-adjusted readmissions on day 31 to 365 after discharge were unchanged in both CDR and the rest of Denmark (table 6).
Table 6.
Differences in hospital readmissions and mortality rates in the CDR compared with the rest of Denmark after centralization of acute stroke services
Mortality within 30 days after the reorganization dropped to 8.2% of all strokes and to 18.9% after 365 days. After risk adjustment, the HRs comparing before to after in the CDR showed no significant differences in mortality rates. The mortality rates in the rest of Denmark also remained unchanged.
The main analyses (length of the acute hospital stay, all-or-none of 11 process performance measures, and mortality within 30 days) were repeated after 1 other region in Denmark that was in the process of centralization was excluded from the control group. This sensitivity analysis did not change the results (data not shown).
Discussion
Centralization and specialization of the acute stroke services in CDR was associated with a significantly reduced length of the acute hospital stay from 5 to 2 days and more strokes patients handled via the same-day outpatient clinic, whereas the length of acute stay remained unchanged in the rest of Denmark in the study period. The dramatic reduction in the length of acute hospital stay was accompanied by a significant improvement in quality of care, an improvement that followed a trend seen in the rest of Denmark in the study period.
The reorganized stroke service could have caused potential risks of less use of acute revascularization as travel distances to stroke units became longer, but we recorded a nonsignificant increase in early stroke admissions within 4.5 hours and a nonsignificant increase in the rate of thrombolysis treatment. Furthermore, we found no indication of safety problems in that the 30-day readmission rates in the CDR rose only slightly, not significantly different from the general trend, with mortality remaining unchanged compared to controls from the rest of Denmark.
We used population-based national data on all stroke events registered in the DSR, which enjoys a high level of completeness and validity. The incidence of stroke cases included matched general estimates of stroke incidences27–30 in the CDR and the rest of Denmark, which allowed us to control for general trends in stroke care in Denmark. Findings from the CDR are generalizable to the rest of Denmark because the 5 Danish regions are sociodemographically and health-wise fairly homogeneous.31 Detailed registry information on stroke characteristics and outcomes allowed us to study the reorganization extensively by including endpoints not analyzed in previous studies of urban area centralization (England). The present study therefore extends the findings of these British studies.3,11,12
We analyzed all hospital readmissions within the entire country during the first year post stroke. This is an essential measure of quality and safety of care,2,18 although there is some controversy as to how readmissions should be interpreted.19 Unfortunately, the data did not allow us to calculate a reliable rate of recurrent stroke because such registration in the DSR is not mandatory in the early phase after a stroke event, when the risk is highest.
We evaluated mortality both in the early phase and after 1 year, and we adjusted the risk-adjusted mortality rates for important potential confounders, including stroke severity, a factor not included in mortality rate adjustments in a previous study.11 It was a limitation that, besides mortality, the data did not permit us to analyze other functional outcomes because we registered no other outcomes.
We report a significant reduction in acute hospital stays, partly because some of the mild strokes were managed in outpatient clinics. The reorganization has hence likely meant cost savings21 because shorter acute hospital stays for stroke patients result in lower hospital costs overall32 and because the outpatient setup is probably more cost-effective.33 The results of this centralization are therefore unlikely to have been confounded by financial investment, as may have been the case with the reorganization of stroke services in London.20 Nevertheless, because the total hospital stay remained unchanged, we observed an increase in the nonacute hospital stay, including rehabilitation. The explanation for this finding is not clear. A significantly increased use of days for rehabilitation could be an explanation, but delayed start of rehabilitation and waiting for rehabilitation or transfer to a nursing home due to bottleneck problems may also have played a role. A more specific cost-effectiveness analysis is needed to make final conclusions on any financial implications.
Before the reorganization, patients deemed eligible for thrombolysis were already taken directly to 1 of 2 designated acute stroke units offering revascularization therapy. A centralized model has previously shown to increase the likelihood of receiving thrombolysis.34 However, we saw a nonsignificant increase in the proportion of patients treated with thrombolysis. This development mirrored that seen in the rest of the country even though the proportion of patients receiving thrombolysis was initially significantly higher in the CDR than in the rest of Denmark and hence less likely to increase further. We therefore speculate that this takes place because all patients were preassessed and treated in a designated acute stroke unit regardless of whether they were found eligible for revascularization treatment. We also learned that the longer travel distances to a specialized stroke unit did not lead to fewer but actually more (nonsignificant) early stroke admissions (within 4.5 hours). We think specialized preassessment (telephone conferences between general practitioners or paramedics and stroke specialists in all cases of stroke suspicion) may have created a higher awareness of the urgency of stroke.
It is a limitation that the patients admitted to same-day treatment at outpatient clinics, which is likely the most cost-effective setup,33 could not be distinguished from hospitalized patients admitted for <24 hours. We therefore cannot describe the outcomes of these 2 groups.
There are no data on patients with TIA treated in the outpatient clinics in the study periods. Therefore, the effects of centralizing the TIA service in the CDR remain unknown.
We could not include patients with missing information on stroke severity in the multivariable models. However, because the prevalence of missing information was low (2%–7%), this is unlikely to have affected the results.
In this study, we used all stroke events from the rest of Denmark to account for general stroke care trends. Other parts of Denmark may also have reorganized their stroke treatment in this period. Collectively, this may have diluted the effect described here. One other region initiated a stepwise centralization model, but because only parts of this region were centralized in the “after” period, this region was included in the control group. However, a sensitivity analysis excluding this region from the data did not change the overall results.
Before the reorganization, some process indicators were significantly better in the CDR than in the rest of Denmark. Because there is a ceiling effect for most of the parameters analyzed, the DID may not fully illuminate the effects of reorganization for these measures.
Overall, the results showed significant effects from centralizing the stroke services in the CDR. We were able to organize the stroke services in a way likely to be more cost-effective while simultaneously maintaining or even improving high-quality care and overall safety for stroke patients from an entire region using specialized acute stroke units only. The improvements we detected were comparable to the general trend in Denmark during the period. The aim of reorganizing stroke care was to reduce costs by reducing the acute length of stay for stroke, managing some of the minor strokes in outpatient clinics, and drawing on early discharge home team care. These goals were met. Nevertheless, to make final conclusions on the financial implications, a more specific cost-effective analysis is needed.
Glossary
- CDR
Central Denmark Region
- DID
difference-in-differences
- DSR
Danish Stroke Registry
- HR
hazard ratio
Author contributions
S.H., S.P.J., D.D., and G.A. designed the study. S.H. and S.P.J. obtained approvals from the Danish Data Protection Agency and the Danish clinical registries. S.H., S.P.J., T.T., and H.H.H. handled the data management and statistical analysis. S.H. drafted the initial manuscript. S.H., P.v.W.-M., C.Z.S., N.H., A.T.M, T.H., M.S.P., N.R.d.M.A., D.D., and G.A. contributed to data collection. All authors made substantial contributions to the study design and interpretation of the findings, contributed to the drafting of the article or to critical revision of important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved. G.A. is the guarantor.
Study funding
This study was supported by the University of Aarhus, Denmark; the Lundbeck Foundation, Denmark; and the Laerdal Foundation, Norway.
Disclosure
S. Hastrup has served on the scientific advisory boards for AstraZeneca. She has received research grants from University of Aarhus and Lundbeck Foundation. S. Johnsen has received a research grant from Pfizer and has served as advisory board member for Pfizer, Bristol-Myer Squibb, and Bayer. He has also served as a speaker for Pfizer, Bristol-Myer Squibb, Bayer, Boehringer-Ingelheim, and St. Jude. He has received research grants from the Danish Research Council and TrygFonden. T. Terkelsen and H.H. Hundborg report no disclosures relevant to the manuscript. P. von Weitzel-Mudersbach received travel grants from Boehringer-Ingelheim and Bristol-Myer Squibb, and speaker honoraria from Bristol-Myer Squibb and Pfizer. C. Simonsen has received speaker honoraria from Bayer and Boehringer-Ingelheim. N. Hjort received travel funding from Bristol-Myer Squibb. A. Møller, T. Harbo, M. Poulsen, and N. Ruiz de Morales Ayudarte report no disclosures relevant to the manuscript. D. Damgaard received honoraria from serving on the scientific advisory board of Amgen Pharmaceuticals; received funding for 2 trips from Bayer Pharmaceuticals and 1 trip from Bristol-Myer Squibb Pharmaceuticals; received speaker honoraria from Bayer Pharmaceuticals, Boehringer-Ingelheim Pharmaceuticals, Bristol-Myer Squibb Pharmaceuticals, and Pfizer Pharmaceuticals; and served as primary investigator for a clinical trial sponsored by Boehringer-Ingelheim Pharmaceuticals and for a clinical trial sponsored by Bayer Pharmaceuticals. G. Andersen received speaker honorarium from Medtronic and research grants from TrygFonden, NovoNordisk Foundation, and Lundbeck Foundation. Go to Neurology.org/N for full disclosures.
References
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katzan IL, Spertus J, Bettger JP, et al. Risk adjustment of ischemic stroke outcomes for comparing hospital performance: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:918–944. [DOI] [PubMed] [Google Scholar]
- 3.Bray BD, Ayis S, Campbell J, et al. Associations between the organisation of stroke services, process of care, and mortality in England: prospective cohort study. BMJ 2013;346:f2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke 2011;42:3214–3218. [DOI] [PubMed] [Google Scholar]
- 5.Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013:CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Langhorne P, Fearon P, Ronning OM, et al. Stroke unit care benefits patients with intracerebral hemorrhage: systematic review and meta-analysis. Stroke 2013;44:3044–3049. [DOI] [PubMed] [Google Scholar]
- 7.Lin HC, Xirasagar S, Chen CH, Lin CC, Lee HC. Association between physician volume and hospitalization costs for patients with stroke in Taiwan: a nationwide population-based study. Stroke 2007;38:1565–1569. [DOI] [PubMed] [Google Scholar]
- 8.Saposnik G, Baibergenova A, O'Donnell M, et al. Hospital volume and stroke outcome: does it matter? Neurology 2007;69:1142–1151. [DOI] [PubMed] [Google Scholar]
- 9.Svendsen ML, Ehlers LH, Ingeman A, Johnsen SP. Higher stroke unit volume associated with improved quality of early stroke care and reduced length of stay. Stroke 2012;43:3041–3045. [DOI] [PubMed] [Google Scholar]
- 10.Tsugawa Y, Kumamaru H, Yasunaga H, Hashimoto H, Horiguchi H, Ayanian JZ. The association of hospital volume with mortality and costs of care for stroke in Japan. Med Care 2013;51:782–788. [DOI] [PubMed] [Google Scholar]
- 11.Morris S, Hunter RM, Ramsay AI, et al. Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014;349:g4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramsay AI, Morris S, Hoffman A, et al. Effects of centralizing acute stroke services on stroke care provision in two large metropolitan areas in England. Stroke 2015;46:2244–2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith EE, Shoba N, Dai D, et al. Risk score for in-hospital ischemic stroke mortality derived and validated within the Get With The Guidelines-Stroke program. Circulation 2010;122:1496–1504. [DOI] [PubMed] [Google Scholar]
- 14.Campbell BC, Meretoja A, Donnan GA, Davis SM. Twenty-year history of the evolution of stroke thrombolysis with intravenous alteplase to reduce long-term disability. Stroke 2015;46:2341–2346. [DOI] [PubMed] [Google Scholar]
- 15.Hacke W, Kaste M, Fieschi C, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke: the European Cooperative Acute Stroke Study (ECASS). JAMA 1995;274:1017–1025. [PubMed] [Google Scholar]
- 16.Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013;309:2480–2488. [DOI] [PubMed] [Google Scholar]
- 17.Schmitz ML, Simonsen CZ, Hundborg H, et al. Acute ischemic stroke and long-term outcome after thrombolysis: nationwide propensity score-matched follow-up study. Stroke 2014;45:3070–3072. [DOI] [PubMed] [Google Scholar]
- 18.Zhong W, Geng N, Wang P, Li Z, Cao L. Prevalence, causes and risk factors of hospital readmissions after acute stroke and transient ischemic attack: a systematic review and meta-analysis. Neurol Sci 2016;37:1195–1202. [DOI] [PubMed] [Google Scholar]
- 19.Oliver D. Readmission rates reflect how well whole health and social care systems function. BMJ 2014;348:g1150. [DOI] [PubMed] [Google Scholar]
- 20.Hill AM. Centralising acute stroke services: study confounded by financial investment. BMJ 2014;349:g5710. [DOI] [PubMed] [Google Scholar]
- 21.Douw K, Nielsen CP, Pedersen CR. Centralising acute stroke care and moving care to the community in a Danish health region: challenges in implementing a stroke care reform. Health Policy 2015;119:1005–1010. [DOI] [PubMed] [Google Scholar]
- 22.Mainz J, Krog BR, Bjornshave B, Bartels P. Nationwide continuous quality improvement using clinical indicators: the Danish National Indicator Project. Int J Qual Health Care 2004;16(suppl 1):i45–i50. [DOI] [PubMed] [Google Scholar]
- 23.Thorvaldsen P, Davidsen M, Bronnum-Hansen H, Schroll M. Stable stroke occurrence despite incidence reduction in an aging population: stroke trends in the Danish Monitoring Trends and Determinants in Cardiovascular Disease (MONICA) population. Stroke 1999;30:2529–2534. [DOI] [PubMed] [Google Scholar]
- 24.Wildenschild C, Mehnert F, Thomsen RW, et al. Registration of acute stroke: validity in the Danish Stroke Registry and the Danish National Registry of Patients. Clin Epidemiol 2013;6:27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish Civil Registration System: a cohort of eight million persons. Dan Med Bull 2006;53:441–449. [PubMed] [Google Scholar]
- 27.Thorvaldsen P, Kuulasmaa K, Rajakangas AM, Rastenyte D, Sarti C, Wilhelmsen L. Stroke trends in the WHO MONICA project. Stroke 1997;28:500–506. [DOI] [PubMed] [Google Scholar]
- 28.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thrift AG, Thayabaranathan T, Howard G, et al. Global stroke statistics. Int J Stroke 2017;12:13–32. [DOI] [PubMed] [Google Scholar]
- 30.Truelsen T, Piechowski-Jozwiak B, Bonita R, Mathers C, Bogousslavsky J, Boysen G. Stroke incidence and prevalence in Europe: a review of available data. Eur J Neurol 2006;13:581–598. [DOI] [PubMed] [Google Scholar]
- 31.Henriksen DP, Rasmussen L, Hansen MR, Hallas J, Pottegard A. Comparison of the five Danish regions regarding demographic characteristics, healthcare utilization, and medication use: a descriptive cross-sectional study. PLoS One 2015;10:e0140197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang YC, Hu CJ, Lee TH, et al. The impact factors on the cost and length of stay among acute ischemic stroke. J Stroke Cerebrovasc Dis 2013;22:e152–e158. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien E, Priglinger ML, Bertmar C, et al. Rapid access point of care clinic for transient ischemic attacks and minor strokes. J Clin Neurosci 2016;23:106–110. [DOI] [PubMed] [Google Scholar]
- 34.Lahr MM, Luijckx GJ, Vroomen PC, van der Zee DJ, Buskens E. Proportion of patients treated with thrombolysis in a centralized versus a decentralized acute stroke care setting. Stroke 2012;43:1336–1340. [DOI] [PubMed] [Google Scholar]