Abstract
Background
Observational studies suggest that diet may influence pancreatic cancer risk. We investigated the effect of a low-fat dietary intervention on pancreatic cancer incidence.
Methods
The Women’s Health Initiative Dietary Modification (WHI-DM) trial is a randomized controlled trial conducted in 48 835 postmenopausal women age 50 to 79 years in the United States between 1993 and 1998. Women were randomly assigned to the intervention group (n = 19 541), with the goal of reducing total fat intake and increasing intake of vegetables, fruits, and grains, or to the usual diet comparison group (n = 29 294). The intervention concluded in March 2005. We evaluated the effect of the intervention on pancreatic cancer incidence with the follow-up through 2014 using the log-rank test and multivariable Cox proportional hazards regression model. All statistical tests were two-sided.
Results
In intention-to-treat analyses including 46 200 women, 92 vs 165 pancreatic cancer cases were ascertained in the intervention vs the comparison group (P = .23). The multivariable hazard ratio (HR) of pancreatic cancer was 0.86 (95% confidence interval [CI] = 0.67 to 1.11). Risk was statistically significantly reduced among women with baseline body mass indexes (BMIs) of 25 kg/m2 or higher (HR = 0.71, 95% CI = 0.53 to 0.96), but not among women with BMIs of less than 25 kg/m2 (HR = 1.62, 95% CI = 0.97 to 2.71, Pinteraction = .01).
Conclusions
A low-fat dietary intervention was associated with reduced pancreatic cancer incidence in women who were overweight or obese in the WHI-DM trial. Caution needs to be taken in interpreting the findings based on subgroup analyses.
The World Cancer Research Fund/American Institute for Cancer Research reports found “limited suggestive” evidence associating red meat and foods containing saturated fatty acids with pancreatic cancer in 2012 (1,2). However, several recent prospective studies have shown a positive association between red meat and animal fat and risk of pancreatic cancer (3,4), as well as an inverse association between fruits, vegetables, and folate and risk of pancreatic cancer (5,6). In addition, adherence to the Healthy Eating Index 2005 and Mediterranean dietary pattern has been favorably associated with risk of pancreatic cancer (7–9). In light of the projected increasing trend of pancreatic cancer incidence and its high fatality rate (10), evaluating preventive strategies targeting diet is of great importance. However, thus far, no study has deliberately assessed the effect of dietary intervention on pancreatic cancer prevention due to the limited capacity of existing clinical trials to address this question.
The Women’s Health Initiative (WHI) dietary modification (DM) clinical trial was conducted between 1993 and 2005, with the primary goal of preventing breast and colorectal cancers (11,12). Although the low-fat dietary pattern used in this trial was not associated with statistically significant risk reduction of major cancer types (13–15), the intervention group reported a statistically significant reduction in total fat intake, to 29% of total energy on average, along with the reduction in intake of red meat and saturated fat and the modest increased intake of dietary fiber, fruits, vegetables, and whole grains (13,16), compared with the comparison group. During the postintervention period, the difference in dietary intake between two groups was preserved in spite of the attenuation (15). In addition, the DM was associated with a modest but statistically significant long-term weight reduction (16,17), as well as improved metabolic profile (17,18).
Because a high-fat diet, obesity, and metabolic syndrome are potential risk factors for pancreatic cancer (19,20), it is plausible that the WHI-DM intervention could influence risk of pancreatic cancer even though the convincing evidence for a link between diet and pancreatic cancer is still lacking. In a previous analysis on multiple cancer sites, the crude hazard ratio for pancreatic cancer was 0.75 (95% CI = 0.49 to 1.15) during the core intervention period (14). In the present report, we conducted an analysis to examine the effect of the WHI-DM trial specifically on pancreatic cancer risk, combining both the core intervention and the postintervention periods. We also evaluated how baseline adiposity influenced the association between dietary intervention and risk of incident pancreatic cancer.
Methods
Study Population
Details of the WHI clinical trial (NCT00000611) design were previously published (12). Briefly, 161 808 women age 50 to 79 years were recruited from 40 clinical centers throughout the United States between 1993 and 1998. Women were eligible for the WHI-DM trial if they were postmenopausal and reported a baseline total fat intake of 32% or higher of total energy (%Kcal), as assessed by the WHI food frequency questionnaire (FFQ) (21). Women were ineligible for the WHI-DM trial if they had self-reported type 1 diabetes, a prior cancer history within 10 years except for nonmelanoma skin cancer, medical conditions likely to cause death within three years, or had reported consuming 10 or more main meals per week prepared outside of the home (11–13,22).
Dietary Modification Intervention
Among 48 835 WHI-DM trial participants, 19 541 (40%) were randomly assigned to follow the low-fat dietary pattern (intervention) and 29 294 (60%) were assigned to continue their usual diet (comparison). Random assignment was based on a permuted-block algorithm with block size of five, 10, or 15 and stratified by clinical center and age group (50–54, 55–59, 60–69, and 70–79 years) (22). The WHI-DM was a behavior modification program to reduce total fat to 20% of daily energy intake and increase fruit and vegetable consumption to five or more daily servings, and grains to six or more daily servings. Caloric restriction or weight loss was not the intervention target. Participants received intensive behavioral modification involving 18 focus group sessions and one individual session in the first year, followed by quarterly maintenance sessions through March 31, 2005. DM intervention group participants were asked to monitor their food intake (12). DM comparison group participants received a copy of Dietary Guidelines for Americans (23) and other health-related materials, but were not asked to make specific diet changes or monitor their diet.
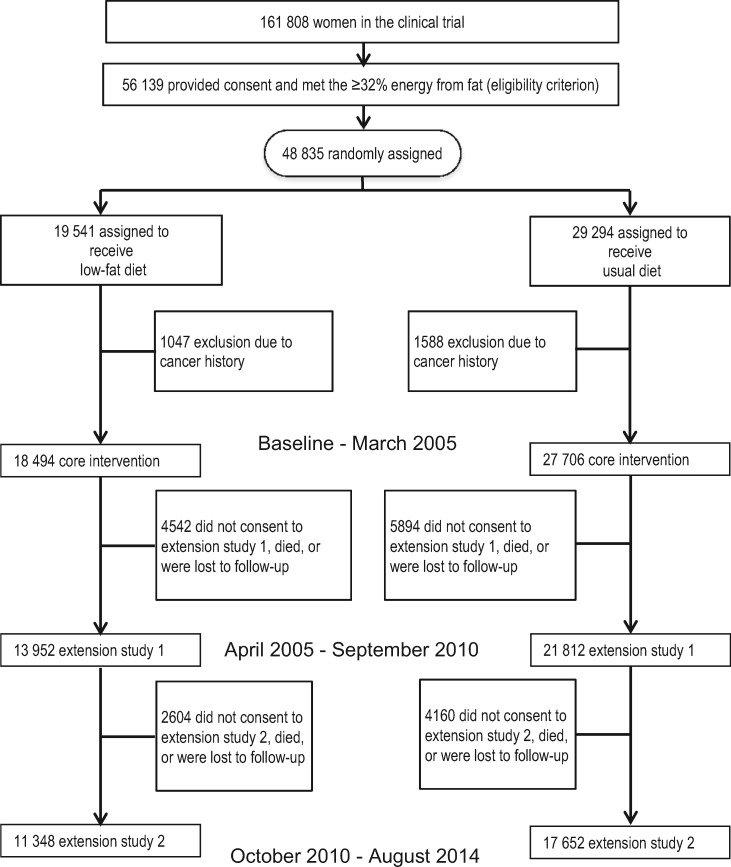
From the original 19 541 participants in the intervention and 29 294 participants in the comparison group, we excluded 1047 and 1588 participants, respectively, because of a history of cancer. As a result, we included 18 494 and 27 706 participants in the respective groups in the analysis (Figure 1).
Figure 1.
Flowchart of participants in the WHI-Dietary Modification Trial in the current analysis.
The WHI Extension Studies
Per protocol, the WHI-DM core intervention ended on March 31, 2005. A total of 76.8% women in the intervention and 80.2% women in the comparison group reconsented for extension study 1 and were followed up through 2010 (2005–2010) in the entire cohort. Our analysis included 13 952 and 21 812 women in the intervention and comparison groups, respectively, for the extension 1 study. In 2010, 81.3% (n = 11 348) in the intervention and 80.9% (n = 17 652) in the comparison group were reconsented for extension study 2 (2010–2015), with follow-up through August 29, 2014 (Figure 1). Throughout extension study 1, participants in the DM intervention group received a quarterly newsletter to offer tips for maintaining the dietary behaviors.
Data Collection
All participants provided information on sociodemographic features, medical history, medication use, smoking habit, alcohol use, physical activity, and family history of cancer at baseline. Study region (North east, South, Southwest, and West) was assigned to each participant. Trained research staff measured weight, height, and waist and hip circumference at the first clinical visit and annually throughout the core intervention trial (22). All reconsenting participants for extension studies completed annual data collection forms on medical history and lifestyle information (15). Average daily food consumption was assessed by self-administered WHI-FFQ at baseline, at year 1 after random assignment, and approximately every three years on a rotating basis for one-third of the women each year through March 2005.
Outcome Ascertainment
The primary outcome for this analysis was incident pancreatic cancer, which was initially ascertained through semi-annual self-administered questionnaires, and then confirmed through centralized review of medical records by trained adjudicators. Through August 29, 2014, 257 incident cases of pancreatic cancer were centrally adjudicated, and 81.7% of cases were pathologically confirmed.
Institutional review board (IRB) approval was obtained at each clinical center, and all participants provided written informed consent. The present analysis was approved by the WHI and the combined IRBs of Baylor College of Medicine and Michael E. DeBakey VA Medical Center.
Statistical Analysis
We used a Student’s t test or χ2 test to compare baseline characteristics of participants in the intervention and comparison groups. We compared age-adjusted incidence of pancreatic cancer based on the intent-to-treat principle. The time to event was defined as the number of days after enrollment to the diagnosis of pancreatic cancer, death, loss to follow-up, end of extension study 2 (August 29, 2014), end of extension study 1 (September 30, 2010), or core intervention period (March 31, 2005), respectively. We used a weighted log-rank test for differences in Kaplan-Meier estimated cumulative hazard for pancreatic cancer between the two groups, with weight defined using time since random assignment, with a weight of 0 at random assignment rising linearly to 1 at 10 years of follow-up and held constant at 1 thereafter. We used multivariable Cox proportional hazards regression analysis to estimate the hazard ratio (HR) and 95% confidence interval (CI) for risk of incident pancreatic cancer in association with intervention. The proportional hazards assumption was not violated for DM intervention and major exposure variables. An inspection of the Schoenfeld residuals for each model predictor was performed to check the proportional hazard assumption. The results showed that the slopes of major exposure variables by time (from baseline to five, 10, 15, and 20 years) were close to 0, thus confirming close adherence to proportional hazards.
We evaluated the following variables for their potential confounding effects on low-fat diet and pancreatic cancer: age, race, education, region, body mass index (BMI), waist to hip ratio (WHR), smoking, physical activity, nonsteroidal anti-inflammatory use, diabetes, pancreatitis, family history of cancer, alcohol use, baseline daily nutrient consumption estimates (total energy intake, percentage of energy from fat, carbohydrate, protein, saturated fat, monosaturated fat and polysaturated fat, folate fiber, and total sugar), baseline daily food assumption (saturated fat, red meat, vegetables, and fruits and grains), and hormone therapy and calcium/vitamin D (Ca/D) trial assignments. Baseline dietary and nutrient intake were energy-adjusted using the density method. We also tested whether the weight change variable mediated the inverse association between low-fat dietary pattern and pancreatic cancer. Absolute weight change (kg) between year 3 and baseline was categorized as weight loss (<–3.0 kg), weight maintenance (≥–3.0 kg and <3.0 kg) or weight gain (≥3 kg). Data on weight change were available for 86.2% of participants in the core intervention period.
We conducted stratified analyses according to baseline BMI status (25< vs ≥ 25 kg/m2), smoking status (never and former vs current), self-reported type 2 diabetes (yes vs no), family history of cancer (yes vs no), and weight change (weight loss and maintenance vs weight gain). We used Wald tests to test the statistical significance of interaction effect.
We performed sensitivity analyses by excluding participants with chronic pancreatitis or who were followed-up for less than two years to address the concern on reverse causality. We also excluded cases without pathological confirmation from the analysis. We alternatively used 25 and 30 kg/m2 as the cutoff points in the analysis, stratified by baseline BMI. Last, 6187 women died during the entire follow-up period in this trial. We addressed the potential competing risk of death by modeling death in the Cox proportional hazards regression model.
Analyses were carried out using SAS statistical software (version 9.4; SAS Institute Inc, Cary, NC). All tests were two-sided, with P values of less than .05 considered statistically significant.
Results
Table 1 shows that the baseline characteristics of the study participants in the two groups were well balanced. The majority of women were overweight or obese (>70.0%) or noncurrent smokers (>90.0%). This balance was largely maintained among participants in extension study 2. Women who remained in the extension study 2 were slightly more likely to be younger, be non-Hispanic Caucasian, or have a more advanced degree at baseline. Higher WHR (> median 0.8) was not associated with pancreatic cancer risk (adjusted HR = 1.04, 95% CI = 0.79 to 1.35) in the current data set (data not shown in tables).
Table 1.
Baseline characteristics of participants in the WHI Dietary Modification trial in the core intervention period and extension study 2*
| Characteristics | Core intervention period (ended in March 2005) |
Extension study 2 (ended in August 2014) |
||
|---|---|---|---|---|
| Intervention (n = 18 494) | Comparison (n = 27 706) | Intervention (n = 11 357) | Comparison (n = 17 665) | |
| Mean age at random assignment (SD), y | 62.2 (6.9) | 62.2 (6.9) | 61.3 (6.4) | 61.2 (6.4) |
| Race, % non-Hispanic white | 81.2 | 81.7 | 84.7 | 85.4 |
| College or postgraduate education, % | 67.5 | 67.2 | 71.3 | 71.0 |
| Region, % | ||||
| Northeast | 23.6 | 23.7 | 25.1 | 25.1 |
| South | 26.1 | 26.0 | 24.0 | 23.7 |
| Midwest | 20.6 | 20.6 | 21.7 | 21.7 |
| West | 29.7 | 29.7 | 29.2 | 29.5 |
| Body mass index, kg/m2 | ||||
| < 25 | 26.6 | 26.7 | 29.0 | 28.5 |
| 25–<30 | 35.5 | 35.6 | 35.7 | 36.5 |
| ≥30 | 37.9 | 36.7 | 35.3 | 35.0 |
| Waist to hip ratio (SD) | 0.82 (0.08) | 0.82 (0.08) | 0.81 (0.08) | 0.81 (0.08) |
| Smoking status, % | ||||
| Never smokers | 51.3 | 51.6 | 52.8 | 52.5 |
| Former smokers | 41.3 | 40.9 | 41.0 | 41.2 |
| Current smokers | 6.4 | 6.6 | 5.3 | 5.6 |
| Missing | 1.1 | 1.0 | 0.9 | 0.8 |
| Recreational physical activity, MET-hour (SD) | 10.1 (11.7) | 10.2 (12.1) | 10.6 (12.0) | 10.6 (12.2) |
| Regular NSAIDs user, % | 19.6 | 20.0 | 19.0 | 20.0 |
| Treated type 2 diabetes, % | 4.4 | 4.4 | 2.9 | 3.0 |
| Pancreatitis, % | 0.6 | 0.7 | 0.5 | 0.7 |
| 1st-degree family history of known cancers, % | 63.9 | 63.6 | 65.3 | 64.8 |
| Alcohol, >1 drink/d, % | 9.7 | 9.6 | 10.2 | 10.4 |
| Baseline daily nutrient consumption estimates (SD) | ||||
| Total energy intake, Kcal | 1791 (709) | 1791 (703) | 1798 (688) | 1797 (681) |
| Percentage energy from total fat | 37.7 (5.1) | 37.8 (5.0) | 37.5 (5.0) | 37.6 (4.9) |
| Percentage energy from carbohydrate | 45.6 (6.3) | 45.6 (6.2) | 45.7 (6.2) | 45.6 (6.1) |
| Percentage energy from protein | 16.5 (3.0) | 16.4 (3.0) | 16.5 (2.9) | 16.5 (2.9) |
| Percentage energy from mono-unsaturated fat | 14.4 (2.3) | 14.4 (2.3) | 14.3 (2.2) | 14.3 (2.2) |
| Percentage energy from saturated fat | 12.7 (2.5) | 12.6 (2.5) | 12.6 (2.5) | 12.6 (2.5) |
| Percentage energy from poly-unsaturated fat | 7.75 (2.0) | 7.76 (2.0) | 7.75 (1.9) | 7.75 (2.0) |
| Total folate equivalent, mcg/1000 Kcal | 278 (80) | 277 (78) | 279 (79) | 278 (77) |
| Total dietary fiber, g/1000 Kcal | 8.8 (2.4) | 8.8 (2.4) | 8.9 (2.4) | 8.9 (2.4) |
| Dietary total sugars, g/1000 Kcal | 53.6 (14.2) | 53.5 (14.2) | 53.6 (13.9) | 53.5 (13.9) |
| Baseline daily food consumption (SD) | ||||
| Saturated fat, g/1000 Kcal | 14.1 (2.8) | 14.1 (2.8) | 14.0 (2.8) | 14.0 (2.7) |
| Red meat, servings | 0.87 (0.60) | 0.87 (0.59) | 0.86 (0.58) | 0.86 (0.57) |
| Total vegetables, servings | 1.2 (0.7) | 1.2 (0.7) | 1.2 (0.7) | 1.2 (0.7) |
| Total fruits, servings | 0.94 (0.6) | 0.94 (0.6) | 0.95 (0.6) | 0.95 (0.6) |
| Total grain, servings | 4.75 (2.5) | 4.77 (2.5) | 4.80 (2.5) | 4.79 (2.4) |
| Vitamin D, mcg/1000 Kcal | 2.46 (1.2) | 2.45 (1.3) | 2.47 (1.3) | 2.46 (1.3) |
| HT trial assignment (active), % | 8.2 | 8.7 | 8.1 | 8.0 |
| Ca/D trial assignment (active), % | 24.8 | 27.0 | 27.4 | 29.2 |
Ca/D = calcium/vitamin D; HT = hormone therapy; MET = metabolic equivalent of task; NSAIDs = nonsteroidal antiinflammatory drugs; WHI = Women’s Health Initiative.
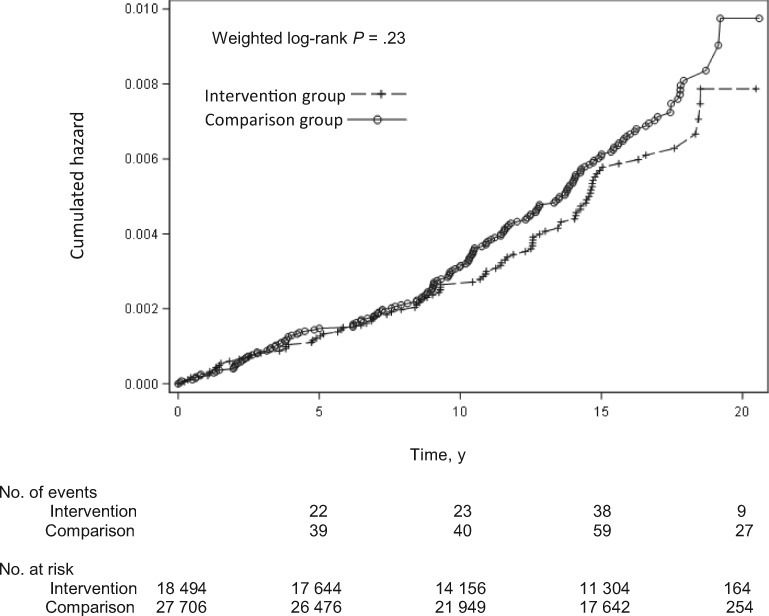
In intention-to-treat analyses including 46 200 women, we identified 92 cases of pancreatic cancer in the intervention group and 165 cases in the comparison group through August 2014, with an average follow-up duration of 14.7 years (SD = 4.3 years). The age-adjusted incidence rate of pancreatic cancer was lower in the intervention group compared with the comparison group (35, 95% CI = 28 to 48, vs 41, 95% CI = 35 to 48) per 100 000 person years, P = 0.23) (Figure 2). The multivariable hazard ratio for pancreatic cancer was 0.86 (95% CI = 0.67 to 1.11). In the selection of confounding factors, none of the variables was associated with both pancreatic cancer (Supplementary Table 1, available online) and random assignment (Table 1) at the P of less than .25 statistical significance level in univariate analyses. The stepwise addition of other variables to the model did not change the risk estimate by 10%. We, however, included age, race/ethnicity (non-Hispanic white, African American, Hispanic, Pacific Islander and Asian, and others), smoking status (never, former, and current smokers), and baseline BMI (<25, ≥25 and <30, ≥30 kg/m2 or continuous) in the multivariable models because they were potential risk factors for pancreatic cancer. The same pattern of statistically nonsignificant inverse association was observed during extension study 1 (average follow-up = 12.6 years) and the core intervention period (average follow-up = 8.5 years). Further adjustment for absolute weight change did not attenuate the association (Table 2). A similar finding was observed in sensitivity analyses excluding 303 women with a history of pancreatitis (multivariable HR = 0.85, 95% CI = 0.66 to 1.10) (data not shown) or excluding 47 cases without pathological confirmation (multivariable HR = 0.84, 95% CI = 0.63 to 1.11; data not shown). After excluding 841 women censored in the first two years of follow-up, the hazard ratio was 0.82 (95% CI = 0.62 to 1.07; data not shown in tables). The modeling of competing risk of death in the Cox regression model did not change the risk estimate. The hazard ratio was 0.86 (95% CI = 0.66 to 1.10).
Figure 2.
Kaplan-Meier estimated cumulative hazards for pancreatic cancer in the Women’s Health Initiative Dietary Modification Trial (1993–2014). The numbers of events and patients at risk in each group at various time points are given below the Kaplan-Meier curves. A two-sided weighted log-rank test was used to calculate the P value.
Table 2.
Incidence rate and risk of pancreatic cancer in the WHI Dietary Modification Trial across follow-up periods
| Follow-up period | Intervention |
Comparison |
Crude HR (95% CI) | Adjusted HR† (95% CI) | Adjusted HR‡ (95% CI) | ||
|---|---|---|---|---|---|---|---|
| No. of cases/ person-years | Age-standardized incidence rate* (95% CI) | No. of cases/ person-years | Age-standardized incidence rate* (95% CI) | ||||
| Extension study 2 (1993–2014) | 92/263 184 | 35 (28 to 48) | 165/403 080 | 41 (35 to 48) | 0.86 (0.66 to 1.10) | 0.86 (0.67 to 1.11) | 0.84 (0.65 to 1.09) |
| Extension study 1 (1993–2010) | 70/226 479 | 31 (24 to 39) | 129/344 313 | 37 (32 to 45) | 0.81 (0.60 to 1.08) | 0.82 (0.61 to 1.10) | 0.81 (0.60 to 1.08) |
| Core intervention (1993–2005) | 40/153 270 | 26 (19 to 36) | 61/230 012 | 27 (21 to 34) | 0.83 (0.56 to 1.24) | 0.83 (0.56 to 1.24) | 0.81 (0.55 to 1.22) |
Per 100 000 person-years. CI = confidence interval; HR = hazard ratio; WHI = Women’s Health Initiative.
HR adjusted for age (continuous), race/ethnicity (non-Hispanic white, Africa American, Hispanic, Pacific Islander and Asian, and other), smoking status (never, former, and current smokers), and baseline body mass index (<25, 25–<30, and ≥30 kg/m2).
HR adjusted for weight change (<–3, –3∼3, >3 kg) at year 3 compared with baseline additionally.
The association between DM intervention and pancreatic cancer risk differed according to baseline BMI status (Table 3). During follow-up through August 2014, the multivariable HR of pancreatic cancer was 0.71 (95% CI = 0.53 to 0.96) among women with a BMI of 25 kg/m2 or greater, but was 1.62 (95% CI = 0.97 to 2.71) among women with a BMI of less than 25 kg/m2 (Pinteraction = .01). We observed similar qualitative effect modification by BMI status when the follow-up was limited to extension study 1 or to the core intervention period (Table 3). In addition, we observed inverse associations between low-fat dietary pattern and pancreatic cancer among both overweight and obese women (Supplementary Table 2, available online).
Table 3.
The association between dietary intervention and risk of incident pancreatic cancer in the WHI Dietary Modification Trial, stratified by baseline BMI status across follow-up periods
| Follow-up period | Intervention | Comparison | Crude HR (95% CI) | Adjusted HR* (95% CI) | Pinteraction† |
|---|---|---|---|---|---|
| (No. of cases/noncases) | (No. of cases/noncases) | ||||
| Extension study 2 | |||||
| BMI < 25 kg/m2 | 30/4880 | 30/7309 | 1.52 (0.92 to 2.53) | 1.62 (0.97 to 2.71) | .01 |
| BMI ≥ 25 kg/m2 | 62/13 522 | 135/20 232 | 0.71 (0.52 to 0.96) | 0.71 (0.53 to 0.96) | |
| Extension study 1 | |||||
| BMI < 25 kg/m2 | 24/4886 | 27/7312 | 1.38 (0.80 to 2.40) | 1.48 (0.85 to 2.60) | .03 |
| BMI ≥ 25 kg/m2 | 46/13 538 | 102/20 265 | 0.66 (0.47 to 0.94) | 0.68 (0.48 to 0.96) | |
| Core intervention | |||||
| BMI < 25 kg/m2 | 15/4895 | 10/7329 | 1.89 (0.85 to 4.20) | 1.89 (0.85 to 4.22) | .02 |
| BMI ≥ 25 kg/m2 | 25/13 559 | 51/20 316 | 0.62 (0.38 to 1.00) | 0.62 (0.38 to 1.00) |
Hazard ratio adjusted for age (continuous), race/ethnicity (non-Hispanic white, African American, Hispanic, Pacific Islander and Asian, and other), smoking status (never, former, and current smokers), and baseline body mass index (continuous). BMI = body mass index; CI = confidence interval; HR = hazard ratio; WHI = Women’s Health Initiative.
P value for two-sided Wald test.
In further exploratory analyses, we did not observe statistically significant effect modification by weight change, smoking status, type 2 diabetes, or family history of cancer. The DM intervention was associated with a statistically nonsignificant reduced risk of pancreatic cancer among women who lost or maintained weight during follow-up, but not among women who gained weight (Pinteraction = .08) (Supplementary Table 3, available online).
Discussion
In a large randomized controlled WHI-DM trial conducted in postmenopausal women in the United States, an intervention emphasizing a lower-fat dietary pattern that incorporated higher intake of fruits, vegetables, and grains resulted in a statistically nonsignificant, moderate risk reduction in pancreatic cancer. However, there was a statistically significant risk reduction in pancreatic cancer among overweight or obese women in the intervention group that persisted even several years after the active intervention ceased.
Obesity is a well-known risk factor for pancreatic intraepithelial neoplasia (PanIN) and pancreatic cancer in Western countries (24,25). The interaction effect between the DM intervention and baseline BMI suggested that the dietary intervention mitigated obesity-associated sequelae that influence progression of pancreatic cancer. The DM intervention could have contributed to improved insulin resistance and immune function (26), suppressed chronic inflammatory tumor microenvironment, or changed the gut microbiome (27,28). Previous analyses showed that during the initial years, the DM intervention was associated with statistically significant decline in body weight (16) and percentage of fat mass, as measured by DXA scan (29). In our analysis, the risk reduction associated with intervention in overweight or obese women was the strongest during the core intervention period and attenuated with longer postintervention follow-up. However, we did not find that weight change mediated the inverse association between the DM trial and risk of pancreatic cancer. Nevertheless, the risk reduction of pancreatic cancer was seen only among women who lost or maintained weight, but not among women who gained weight. On the other hand, we observed a statistically nonsignificant but consistent trend of positive association between low-fat dietary pattern and risk of pancreatic cancer among women who had BMIs of less than 25 kg/m2. This observation pertains to a small number of cases (n = 60) and remains to be explained if it were true. It is less likely that this normal BMI was due to pancreatic cancer–associated weight loss because the median follow-up time for these cases was more than nine years. The distribution of known risk factors did not differ by BMI status either, albeit the rate of current smokers was higher in women who had normal BMIs (8.0%) than those who had higher BMIs (6.1%). Further biomarker study on metabolic phenotype may help us understand this observation if it’s true.
Experimental and epidemiological evidence support a favorable effect of the low-fat dietary intervention used in the WHI-DM intervention trial on pancreatic cancer development. In mice, a high-fat diet has been shown to activate oncogenic kras via ptgs 2, leading to pancreatic inflammation and fibrosis and development of PanIN and pancreatic ductal adenocarcinoma (30). A high-fat diet was associated with increased risk of pancreatic cancer in the National Institutes of Health–AARP Diet and Health Study (31), and saturated fat from animal sources in particular has been associated with an elevated risk of pancreatic cancer (32). The epidemiologic finding on fruit and vegetable consumption and pancreatic cancer is inconsistent (1,33–35). Nevertheless, a recent observational study (36) and a meta-analysis showed an inverse association between higher intake of fruits and/or vegetables, whole grains, and wheat and risk of pancreatic cancer (5,6,37). In addition, phytochemicals or food-bioactive compounds have been shown to inhibit pancreatic cancer growth in cell lines or genetically engineered murine models by modulating GSK-3β/NF-κB (38) and IGF1/Act/mTOR pathways (26,39). However, we were not able to determine the effect of DM intervention attributable to lower total/saturated fat intake or higher fruit/vegetable intake because the intervention was implemented as a dietary pattern.
The current analysis on dietary intervention and pancreatic cancer incidence in a large clinical trial is novel. Study strengths include a randomized design, a large, diverse population of postmenopausal women, a long follow-up period, and medical record confirmation of pancreatic cancer cases. Study limitations included post hoc analyses. Caution needs to be taken in interpreting the study findings based on the subgroup analyses. The observed associations might be explained by factors correlated with intervention but not accounted for in the analysis. The generalizability of the intervention effect in men and premenopausal women needs to be evaluated separately. Based on eligibility criteria, the study findings may not be generalizable to postmenopausal women with a total fat intake of less than 32% of total energy intake. The representativeness of the women in the DM trial thus may be limited. Finally, there was no adherence measure in the comparison group of the DM trial.
Dietary advice similar to the that applied in the WHI-DM intervention trial has been advocated for cancer prevention (40). However, the quality of US diets remains poor, with less than 20% of adults consuming the recommended amount of fruits and vegetables (41,42). In the Framingham Heart Study, the percentage of energy derived from total fat and protein increased in both men and women between 1991 and 2008 (43). We identified a potentially important opportunity for pancreatic cancer prevention through dietary intervention, specifically in overweight or obese postmenopausal women who had a higher percentage of energy intake from fat.
In summary, a statistically significant risk reduction in incidence of pancreatic cancer was seen in women with baseline BMIs of 25 kg/m2 or greater in the DM intervention group. Our observation supported the role of dietary factors in the development of obesity-related pancreatic cancer. Future studies should evaluate whether the preventive effect of diet on pancreatic cancer depends on different genetic, environmental, or metabolic backgrounds in the targeted populations.
Funding
This work was supported by the National Cancer Institute (5R01CA172880, PI: LJ) and Houston Veterans Affairs Health Services Research Center of Innovations (CIN13-413). The Women’s Health Initiative (WHI) program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, and US Department of Health and Human Services through contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118–32119, 32122, 42107-26, 42129-32, and 44221, and the Cancer Center Support Grant National Institutes of Health: National Cancer Institute (NCI) P30CA022453.
The study sponsor had no role in the design and conduct of the study, the data collection, analysis, and interpretation, the writing of the article, or the decision to submit for publication. The views expressed in this article are those of the authors and do not necessarily represent the views of the NCI or the Department of Veterans Affairs or other funders.
This trial is registered at clinicaltrials.gov as NCT00000611. The research protocol can be found at https://www.whi.org/researchers/studydoc/SitePages/Protocol%20and%20Consents.aspx.
We acknowledge the dedicated effort of the investigators and staff at the Women’s Health Initiative clinical centers, the WHI Clinical Coordinating Center, and the National Heart, Lung and Blood program office (listing available at http://www.whi.org). We also recognize the WHI participants for their commitment to the WHI program. For a list of all the investigators who have contributed to WHI science, please visit http://www.whiscience.org/publications/WHI_investigators_longlist.pdf. We thank Dr. Zhigang Duan (MD, MS, the University of Texas MD Anderson Cancer Center, Houston, TX) for his assistance with data analysis. We thank Dr. Margaret R. Spitz (MD, MPH, Baylor College of Medicine, Houston, TX) for her critical review of this manuscript.
Supplementary Material
References
- 1. World Cancer Research Fund/American Institute for Cancer Research. Pancreatic Cancer 2012 Report: Food, Nutrition, Physical Activity, and the Prevention of Pancreatic Cancer. Washington DC: AICR; 2012. [Google Scholar]
- 2. Norat T, Aune D, Chan D, Romaguera D.. Fruits and vegetables: Updating the epidemiologic evidence for the WCRF/AICR lifestyle recommendations for cancer prevention. Cancer Treat Res. 2014;159:35–50. [DOI] [PubMed] [Google Scholar]
- 3. Taunk P, Hecht E, Stolzenberg-Solomon R.. Are meat and heme iron intake associated with pancreatic cancer? Results from the NIH-AARP diet and health cohort. Int J Cancer. 2016;138(9):2172–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Larsson SC, Wolk A.. Red and processed meat consumption and risk of pancreatic cancer: Meta-analysis of prospective studies. Br J Cancer. 2012;106(3):603–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alsamarrai A, Das SL, Windsor JA, Petrov MS.. Factors that affect risk for pancreatic disease in the general population: A systematic review and meta-analysis of prospective cohort studies. Clin Gastroenterol Hepatol. 2014;12(10):1635–1644. [DOI] [PubMed] [Google Scholar]
- 6. Wu QJ, Wu L, Zheng LQ, Xu X, Ji C, Gong TT.. Consumption of fruit and vegetables reduces risk of pancreatic cancer: Evidence from epidemiological studies. Eur J Cancer Prev. 2015;25(3):196–205. [DOI] [PubMed] [Google Scholar]
- 7. Arem H, Reedy J, Sampson J, et al. The Healthy Eating Index 2005 and risk for pancreatic cancer in the NIH-AARP study. J Natl Cancer Inst. 2013;105(17):1298–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bosetti C, Bravi F, Turati F, et al. Nutrient-based dietary patterns and pancreatic cancer risk. Ann Epidemiol. 2013;23(3):124–128. [DOI] [PubMed] [Google Scholar]
- 9. Jiao L, Mitrou PN, Reedy J, et al. A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med. 2009;169(8):764–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM.. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–2921. [DOI] [PubMed] [Google Scholar]
- 11. The Women's Health Initiative Study Group. Design of the Women's Health Initiative clinical trial and observational study. Control Clin Trials. 1998;19(1):61–109. [DOI] [PubMed] [Google Scholar]
- 12. Ritenbaugh C, Patterson RE, Chlebowski RT, et al. The Women's Health Initiative Dietary Modification Trial: Overview and baseline characteristics of participants. Ann Epidemiol. 2003;13(9 suppl):S87–S97. [DOI] [PubMed] [Google Scholar]
- 13. Beresford SA, Johnson KC, Ritenbaugh C, et al. Low-fat dietary pattern and risk of colorectal cancer: The Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):643–654. [DOI] [PubMed] [Google Scholar]
- 14. Prentice RL, Thomson CA, Caan B, et al. Low-fat dietary pattern and cancer incidence in the Women's Health Initiative Dietary Modification Randomized Controlled Trial. J Natl Cancer Inst. 2007;99(20):1534–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thomson CA, Van HL, Caan BJ, et al. Cancer incidence and mortality during the intervention and postintervention periods of the Women's Health Initiative Dietary Modification Trial. Cancer Epidemiol Biomarkers Prev. 2014;23(12):2924–2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: The Women's Health Initiative Dietary Modification Trial. JAMA. 2006;295(1):39–49. [DOI] [PubMed] [Google Scholar]
- 17. Howard BV, Van HL, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: The Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):655–666. [DOI] [PubMed] [Google Scholar]
- 18. Neuhouser ML, Howard B, Lu J, et al. A low-fat dietary pattern and risk of metabolic syndrome in postmenopausal women: The Women's Health Initiative. Metabolism. 2012;61(11):1572–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Luo J, Margolis KL, Adami HO, LaCroix A, Ye W.. Obesity and risk of pancreatic cancer among postmenopausal women: The Women's Health Initiative (United States). Br J Cancer. 2008;99(3):527–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosato V, Tavani A, Bosetti C, et al. Metabolic syndrome and pancreatic cancer risk: A case-control study in Italy and meta-analysis. Metabolism. 2011;60(10):1372–1378. [DOI] [PubMed] [Google Scholar]
- 21. Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T.. Measurement characteristics of the Women's Health Initiative food frequency questionnaire. Ann Epidemiol. 1999;9(3):178–187. [DOI] [PubMed] [Google Scholar]
- 22. Anderson GL, Manson J, Wallace R, et al. Implementation of the Women's Health Initiative study design. Ann Epidemiol. 2003;13(9 suppl):S5–S17. [DOI] [PubMed] [Google Scholar]
- 23. US Department of Agriculture. Dietary Guideline for Americans. 3rd ed.Washington, DC: Department of Health and Human Services; 1990. [Google Scholar]
- 24. Stolzenberg-Solomon RZ, Schairer C, Moore S, Hollenbeck A, Silverman DT.. Lifetime adiposity and risk of pancreatic cancer in the NIH-AARP Diet and Health Study cohort. Am J Clin Nutr. 2013;98(4):1057–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rebours V, Gaujoux S, d'Assignies G, et al. Obesity and fatty pancreatic infiltration are risk factors for pancreatic precancerous lesions (PanIN). Clin Cancer Res. 2015;21(15):3522–3528. [DOI] [PubMed] [Google Scholar]
- 26. Mohammed A, Janakiram NB, Pant S, Rao CV.. Molecular targeted intervention for pancreatic cancer. Cancers (Basel). 2015;7(3):1499–1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Renehan AG, Zwahlen M, Egger M.. Adiposity and cancer risk: New mechanistic insights from epidemiology. Nat Rev Cancer. 2015;15(8):484–498. [DOI] [PubMed] [Google Scholar]
- 28. De R V, Galgani M, Santopaolo M, Colamatteo A, Laccetti R, Matarese G.. Nutritional control of immunity: Balancing the metabolic requirements with an appropriate immune function. Semin Immunol. 2015;(5):300–309. [DOI] [PubMed] [Google Scholar]
- 29. Carty CL, Kooperberg C, Neuhouser ML, et al. Low-fat dietary pattern and change in body-composition traits in the Women's Health Initiative Dietary Modification Trial. Am J Clin Nutr. 2011;93(3):516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Philip B, Roland CL, Daniluk J, et al. A high-fat diet activates oncogenic Kras and COX2 to induce development of pancreatic ductal adenocarcinoma in mice. Gastroenterology. 2013;145(6):1449–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thiebaut AC, Jiao L, Silverman DT, et al. Dietary fatty acids and pancreatic cancer in the NIH-AARP diet and health study. J Natl Cancer Inst. 2009;101(14):1001–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sanchez GV, Weinstein SJ, Stolzenberg-Solomon RZ.. Is dietary fat, vitamin D, or folate associated with pancreatic cancer? Mol Carcinog. 2012;51(1):119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heinen MM, Verhage BA, Goldbohm RA, van den Brandt PA.. Intake of vegetables, fruits, carotenoids and vitamins C and E and pancreatic cancer risk in The Netherlands Cohort Study. Int J Cancer. 2012;130(1):147–158. [DOI] [PubMed] [Google Scholar]
- 34. Koushik A, Spiegelman D, Albanes D, et al. Intake of fruits and vegetables and risk of pancreatic cancer in a pooled analysis of 14 cohort studies. Am J Epidemiol. 2012;176(5):373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vrieling A, Verhage BA, van Duijnhoven FJ, et al. Fruit and vegetable consumption and pancreatic cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2009;124(8):1926–1934. [DOI] [PubMed] [Google Scholar]
- 36. Jansen RJ, Robinson DP, Stolzenberg-Solomon RZ, et al. Fruit and vegetable consumption is inversely associated with having pancreatic cancer. Cancer Causes Control. 2011;22(12):1613–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lei Q, Zheng H, Bi J, et al. Whole grain intake reduces pancreatic cancer risk: A meta-analysis of observational studies. Medicine (Baltimore). 2016;95(9):e2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Johnson JL, de Mejia EG.. Flavonoid apigenin modified gene expression associated with inflammation and cancer and induced apoptosis in human pancreatic cancer cells through inhibition of GSK-3beta/NF-kappaB signaling cascade. Mol Nutr Food Res. 2013;57(12):2112–2127. [DOI] [PubMed] [Google Scholar]
- 39. Johnson J, de Mejia EG.. Dietary factors and pancreatic cancer: The role of food bioactive compounds. Mol Nutr Food Res. 2011;55(1):58–73. [DOI] [PubMed] [Google Scholar]
- 40. Pericleous M, Rossi RE, Mandair D, Whyand T, Caplin ME.. Nutrition and pancreatic cancer. Anticancer Res. 2014;34(1):9–21. [PubMed] [Google Scholar]
- 41. Johnston R, Poti JM, Popkin BM.. Eating and aging: Trends in dietary intake among older Americans from 1977–2010. J Nutr Health Aging. 2014;18(3):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vadiveloo M, Scott M, Quatromoni P, Jacques P, Parekh N.. Trends in dietary fat and high-fat food intakes from 1991 to 2008 in the Framingham Heart Study participants. Br J Nutr. 2014;111(4):724–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.