Abstract
Background
Appropriate testing of people at risk for HIV is an important piece of the HIV care continuum. We analyzed HIV testing patterns of patients tested for gonorrhea and chlamydia (GC/CT) at a large urban health care system in New York City.
Methods
We retrospectively studied HIV and GC/CT testing from 2010 to 2015. Data were collected from a clinical laboratory database and linked to electronic health records. Patients were older than age 13 years, not known to be HIV positive, and had had a GC/CT test. The main outcome was the proportion of patients who had both HIV and GC/CT testing performed at the same encounter.
Results
We analyzed 85 768 patients with 139 404 GC/CT testing encounters. Most of the testing encounters (88% for men and 94% for women) were in the outpatient setting. Same-day HIV testing improved from 59% in 2010 to 70% in 2015 for male patients, and from 41% to 51% for female patients. In multivariate regression, male sex was associated with receipt of an HIV test (odds ratio [OR], 2.49; P < .001). Emergency department (OR, 0.22; P < .0001) and inpatient (OR, 0.10; P < .0001) locations were negatively associated with receipt of HIV testing. Among patients with HIV and GC/CT testing at the same encounter, 37 were HIV positive.
Conclusions
Concurrent HIV testing of patients being evaluated for GC/CT increased from 2010 to 2015. However, many patients failed to receive HIV testing, especially in emergency and inpatient settings. There continue to be missed opportunities for diagnosis of HIV among individuals with ongoing high-risk behavior.
Keywords: emergency department, HIV, sexually transmitted diseases, testing
Early diagnosis and linkage to treatment has a significant impact on the morbidity and mortality of HIV-infected individuals [1, 2]. Diagnosis and treatment also lead to reduced risk of HIV transmission [3]. These data have led to recommendations to expand HIV testing. In 2006, the Centers for Disease Control and Prevention (CDC) recommended opt-out testing for all individuals [4], and the US Preventive Service Task Force (USPSTF) recommended routine testing in 2013 [5]. To further encourage testing, New York State passed legislation in 2010 requiring that all individuals between 13 and 64 years of age be offered at least 1 HIV test in emergency department (ED), inpatient, and primary care settings [6]. In 2014, New York updated the law to eliminate the need for written consent. The implementation of this testing law has been projected to contribute to a decline in HIV incidence and prevalence in the coming decade [7].
Each of these recommendations also includes provisions for retesting of individuals with ongoing risk of HIV acquisition, such as those with high-risk sexual behavior or sexually transmitted infections (STIs). Previous studies show that the presence of a recent STI and/or attendance at an STI clinic are significant predictors of future HIV infection [8–10]. Thus, in addition to routine annual testing, retesting of individuals at higher risk may further identify HIV-infected individuals, who can then be linked to care.
In response to the New York State mandate, our hospital implemented an electronic health record (EHR) prompt in September 2011 to remind providers to offer 1-time HIV testing in the ED and at outpatient primary care practices. However, this prompt did not incorporate retesting of patients at continued risk for HIV acquisition, such as those with suspected STIs. We aimed to evaluate the trend in HIV testing during encounters for STI testing within our health care system from 2010 to 2015 and to define factors associated with having an HIV test performed.
METHODS
Design and Setting
This is a retrospective cohort study of HIV testing of individuals >13 years of age who were tested for gonorrhea and chlamydia infection (GC/CT) at New York Presbyterian Hospital–Weill Cornell (NYPH-WC) between 2010 and 2015. NYPH-WC consists of a large urban academic hospital and affiliated outpatient practices in New York City. The study was approved by the Weill Cornell Medicine Institutional Review Board.
Data Collection
Study patients were identified by querying the NYPH-WC laboratory database for GC/CT and HIV tests performed during the study period. For GC/CT, we collected all nucleic acid amplification tests from urine and vaginal, urethral, rectal, or pharyngeal sites. All encounters with GC/CT tests that were collected were analyzed, including those tests that the laboratory was unable to perform (labeled “no result”). This is because the provider’s decision to order the test would motivate concurrent HIV testing, regardless of whether the test was performed by the laboratory. We collected HIV antibody, HIV viral load, and CD4 cell count results to determine if patients had known HIV. For every test performed, we also collected participant age, sex, participant location at sample acquisition, date of test, and test result. To categorize settings, we obtained the list of all outpatient appointment dates, location, department, provider, and visit diagnosis. In the 114 cases where no specific encounter location was available, we assigned these to an outpatient site rather than in the emergency department or hospital. We manually reviewed 30 of these encounters to ensure that no inpatient or ED encounters occurred during that time. We defined patients as being primary care patients if they had had primary care appointments at the same institution within 1 year of the encounter. We excluded patients that were known or likely to have preexisting HIV, which included those with (1) a positive HIV antibody or viral load, (2) an HIV diagnosis on the outpatient appointment diagnosis list, (3) an appointment location in the HIV clinic, or (4) >1 CD4 cell count and HIV viral load. The remainder of testing encounters were considered to be for patients who were at risk for HIV and were included in the analysis. We reviewed the charts of a random sampling of 100 laboratory testing encounters each from ED, inpatient, and outpatient sites to confirm the validity of this classification.
Data Analysis
Each GC/CT testing encounter was treated as a unique observation. Our primary outcome was performance of an HIV test at the same encounter as a GC/CT test. Analyses were conducted separately for men and women because of differences in how providers might perceive the risk of HIV acquisition and different GC/CT testing patterns between those groups. Descriptive statistics were performed using the proportion of encounters that met the outcome and 95% confidence intervals. The trends in proportion over time were plotted. Bivariate logistic regressions were conducted using year of visit, age, visit location, whether the participant was engaged in primary care at NYPH-WC, whether the participant had a prior negative HIV antibody test, and the result of GC/CT testing as predictors. Multivariate logistic regression analysis using robust covariance accounting for participant-level clustering was then performed to generate odds ratios associated with the outcome of receiving an HIV test on the same day. Additional predictor variables were selected as candidates for inclusion in the multivariate model if they were significant on bivariate testing (alpha level of 0.25) [11]. A secondary analysis was also conducted of the outcome of receiving an HIV test within 30 days before or 1 year after the GC/CT test. This was to allow for providers who may not have performed an HIV test if one was recently available in the EHR and those who may have referred patients to another provider for HIV testing. Statistical analyses were performed in R, version 3.3.1, and STATA, version 14 [12–14].
RESULTS
Description of Study Population and Encounters
A total of 85 788 patients received GC/CT testing during the study period. We excluded 4 individuals due to missing sex, 81 who were out of the specified age range, and 2934 who were known or suspected to be HIV-infected. We analyzed data from a total of 11 889 men, seen for 17 249 GC/CT testing encounters, and 70 880 women, seen for 122 155 GC/CT testing encounters. The majority of the testing encounters, 88% for men and 94% for women, were in the outpatient setting. Table 1 shows characteristics of GC/CT testing encounters over the study period.
Table 1. .
Characteristics of GC/CT Testing Encounters From 2010 to 2015
| Female (n = 122 155) | Male (n = 17 249) | |
|---|---|---|
| Mean patient age (SD), y | 34 (8.7) | 34 (12.8) |
| Encounter location, No. (%) | ||
| Emergency department | 4203 (3.4) | 1679 (9.7) |
| Inpatient | 2877 (2.4) | 353 (2) |
| Outpatient | 115 075 (94.2) | 15 217 (88.2) |
| Primary care patient,a No. (%) | 49 246 (40) | 13 331 (77.3) |
| Prior HIV test,b No. (%) | ||
| Previously HIV tested | 43183 (35.3) | 5503 (31.9) |
| Not previously HIV tested | 78972 (64.7) | 11 746 (68.1) |
| GC/CT test result, No. (%) | ||
| GC positive | 65 (<0.1) | 105 (0.6) |
| CT positive | 1150 (0.9) | 380 (2.2) |
| GC and CT positive | 25 (<0.1) | 25 (0.2) |
| GC and CT negative | 119 569 (97.9) | 16 247 (94.2) |
| No result available | 1346 (1.1) | 492 (2.9) |
Abbreviations: CT, Chlamydia trachomatis; GC, Neisseria gonorrhoea.
aPrimary care patients were those patients with primary care appointments at the same institution within 1 year of the encounter.
bAs patients with known HIV infection were excluded, all “previously HIV tested” patients tested HIV negative.
Change in HIV Testing Over Study Period (2010–2015)
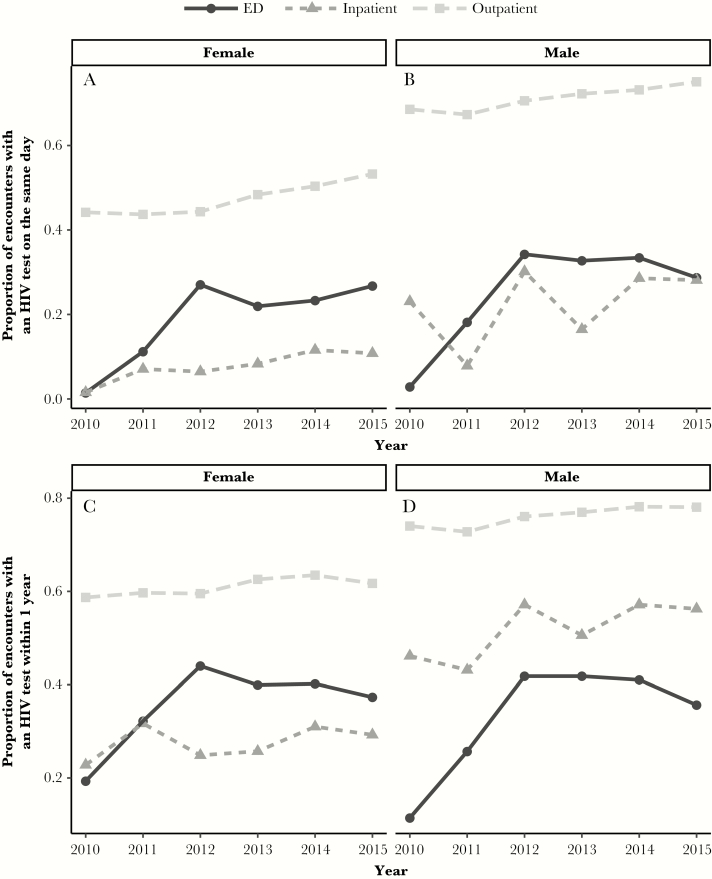
For male patients, 59% of GC/CT testing encounters in 2010 resulted in an HIV test on the same day, and this increased to 70% in 2015. For female patients, 41% of GC/CT testing encounters in 2010 resulted in an HIV test on the same day, which increased to 51% in 2015. Although HIV testing improved over time in all subgroups, there was significant variation by encounter location, with higher testing frequency at outpatient sites compared with ED and inpatient sites. Figure 1, A and B, shows the change over time in proportion of GC/CT encounters with an HIV test on the same day, stratified by sex and by encounter location.
Figure 1. .
Proportion of gonorrhea and chlamydia testing encounters with HIV test by location. A and B, Proportion of encounters in which patients received an HIV test on the same encounter. C and D, Proportion of encounters in which patients received an HIV test within 1 year after the encounter. Abbreviation: ED, emergency department.
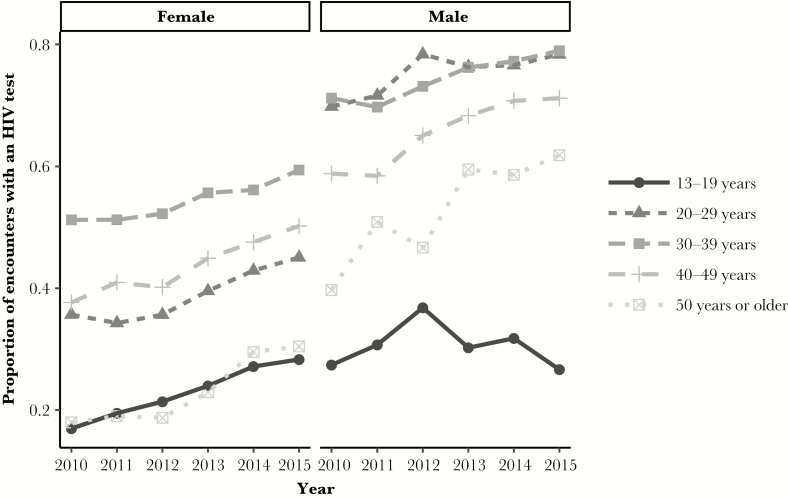
For both male and female patients, the proportion of GC/CT testing encounters that resulted in an HIV test was lowest in the youngest and oldest age groups (<20 years and >50 years). Figure 2 shows the change in HIV testing over time stratified by sex and by age group.
Figure 2. .
Proportion of gonorrhea and chlamydia testing encounters with concurrent HIV test by age. Proportion of encounters in which patients received an HIV test on the same day. Age is measured in years at the time of the encounter.
Factors Associated With HIV Testing
Results of logistic regression analysis are shown in Table 2. Male sex was most strongly associated with receipt of an HIV test, with an adjusted odds ratio of 2.94 (P < .001). Study year was also strongly associated with an adjusted odds ratio of 1.13 (P < .001). Encounters in the ED, inpatient setting, a prior negative HIV test, and patients with known primary care engagement at our institution were all associated with a lower odds ratio of receiving an HIV test at a given encounter.
Table 2. .
Multivariate Logistic Regression for Odds of Receiving an HIV Test at the Same Encounter as GC/CT Testing
| Adjusted Odds Ratio | 95% Confidence Interval | P Value | |
|---|---|---|---|
| Study year | 1.116 | 1.108–1.126 | <.001 |
| Age, y | 1.002 | 1.001–1.004 | <.001 |
| Male sex | 2.799 | 2.677–2.928 | <.001 |
| Encounter location | |||
| Emergency room | 0.219 | 0.204–0.236 | <.001 |
| Inpatient | 0.102 | 0.089–0.116 | <.001 |
| Outpatient | Ref | Ref | |
| Primary care patient | 0.842 | 0.818–0.866 | <.001 |
| Prior HIV test results | |||
| Previously HIV negative | 0.800 | 0.778–0.823 | <.001 |
| Not previously tested | Ref | Ref |
Logistic regression with robust covariances for participant-level clustering. Study year defined as a continuous variable, with 2010 as year 0. Primary care patients were those patients with primary care appointments at the same institution within 1 year of the encounter.
Abbreviations: CT, Chlamydia trachomatis; GC, Neisseria gonorrhoea.
Receipt of HIV Testing Within 1 Year of GC/CT Test
Expanding the interval of HIV testing to include tests performed within 30 days before and up to 1 year after GC/CT increased the proportion of encounters with an HIV test. For male patients, the proportion of encounters with HIV tests using a 1-year interval was 65% in 2010, compared with 59% using a same-day interval. In 2015 for male patients, the proportion receiving an HIV test in a 1-year interval was 74%, compared with 70% using a same-day interval. For female patients, the proportion increased to 56% (1-year interval) from 41% (same-day interval) in 2010, and to 60% (1-year interval) from 52% (same-day interval) in 2015. Inpatient encounters were most sensitive to changes in the time frame. This was driven by HIV tests performed several days into a hospitalization. Figure 1C and D, shows the proportion of encounters receiving HIV testing within 1 year after GC/CT testing over time, stratified by sex and location.
HIV and GC/CT Diagnoses
There were relatively few HIV diagnoses across the cohort. Over the 5-year study period, there were 31 positive HIV antibody tests among 11 515 HIV testing encounters in men (0.27%) and 6 positive HIV tests among 56 138 HIV testing encounters in women (0.01%). Diagnoses of GC/CT were more common than those of HIV: 510 positive tests over 17 249 testing encounters for men (2.9%) and 1240 positive GC/CT tests over 122 155 testing encounters for women (1.0%). Of the bacterial STIs diagnosed, chlamydia was the most common, accounting for 405 of the 510 diagnoses in men (79%) and 1175 of the 1240 positive tests in women (95%). Among patients who tested positive for STI, the HIV diagnoses were more common than in the whole cohort: 2 of 288 encounters in male patients (0.69%) with both positive GC/CT and HIV testing were HIV positive, and 2 of 470 encounters in female patients (0.42%).
DISCUSSION
Our study shows that the frequency of HIV testing within our institution for patients being tested for GC and CT has improved since New York State legislation mandating the offer of an HIV test. Despite this, there were frequent missed opportunities for HIV testing, especially in the ED, where less than one-third of patients tested for GC/CT received an HIV test on the same day. Even after expanding the testing interval to allow for testing performed within the next 12 months at the same institution, more than half of patients in the ED and 27%–40% of outpatients did not receive an HIV test after performance of GC/CT testing.
In New York State, providers in ED, inpatient, and primary care settings are required to offer 1-time HIV testing for individuals aged 13–64 years, except when previous testing offers have been documented or when a life-threatening emergency prevents the offer. Expanding testing within these parameters has been shown, using simulation modeling, to potentially reduce the number of HIV infections by 16.9% from 2010 to 2020, though this reduction assumes perfect implementation [7].
Data regarding the implementation of the New York testing law suggest that the frequency of HIV testing is improving [15–19]. Survey data from 2011 to 2012 showed that only 25% of New York residents aged 18–64 years who had sought medical care in the past year were offered an HIV test at that visit, with 60% of those accepting the offer [17]. By the end of our study, we found substantial increases in HIV testing. Our study population may have had an increased opportunity to be tested for HIV compared with the general population because our population was already interacting with the health care system for GC/CT testing.
In contrast to an overall improvement in HIV testing, we show that the trend varies by subgroups. For example, men were more likely to receive an HIV test. This may be because GC/CT testing is frequently ordered for asymptomatic women as part of routine gynecological exams or prenatal testing. In contrast, GC/CT testing for men may be reserved for those with known sexual risk or with symptoms. If this is the case, providers may be more inclined to offer a concurrent HIV test.
Individuals aged 13–20 years were less likely to receive HIV testing and had little increase in testing over time, and actually decreased in the last year of data. This is especially relevant given the importance of incident HIV in adolescent men, even as overall HIV incidence is declining. National and local surveillance data show that persons aged 20–29 years have the highest rate of reported HIV diagnoses [20, 21]. Earlier testing of individuals with ongoing sexual activity may be useful for diagnosing cases earlier and linking them to care and linking HIV-negative adolescents to appropriate prevention. Notably, the New York State law does not mandate parental consent for individuals <18 years of age, so this should not be a barrier to testing in the adolescent population.
Our data show that emergency departments present opportunities to improve HIV testing, even when accounting for subsequent testing via referral within the same health care network. There are multiple challenges to increasing testing in this setting, including personnel limitations, hospital efforts to minimize ED wait times, the need for a private space to provide testing and counseling, and the cost of coordinating follow-up for individuals with positive tests [22]. The availability of rapid point-of-care testing mitigates some of these difficulties, but unfortunately these testing methods have not been universally implemented, even in high-prevalence areas [16]. Electronic health record alerts can also serve to reinforce compliance, but a study by our ED providers suggests that overly frequent or onerous alerts may lead to frustration among providers [23].
Although the legislative mandate clearly describes recommendations for those who have never been HIV tested, the interval for retesting populations at ongoing risk is less clear. The missed opportunities for testing found in our study may be partly because individuals were not subject to the mandate. This would be true if the individual had a documented prior HIV test, even though the risk of acquisition in the setting of ongoing sexual risk behavior might warrant retesting. Data on the optimal interval of retesting and interventions to promote HIV testing for those at ongoing risk would help to improve the use of HIV testing in these settings.
Consistent with the decreasing incidence of HIV infection in New York City, we observed very few new HIV diagnoses in our analysis [20]. However, the diagnosis of HIV in the subset of patients with diagnosed GC/CT was substantially more common, likely reflecting the higher risk status of this group. If incidence continues to decline, in line with the New York State HIV elimination agenda, new testing strategies may need to evolve to account for local prevalence and risk of acquisition, even among patients with apparent sexual risk factors.
The strength of our analysis includes a large longitudinal data source that captures testing practices within a multilocation health care system. However, our analysis is limited in several ways. The use of institutional laboratory data did not allow us to capture tests performed outside our institution or point-of-care tests that were not sent to our laboratory. However, although 1 clinic used point-of-care testing, this was not in widespread use at the time of the study. We had limited patient-level data and were not able to assess the impact of factors such as race, insurance status, or type of sexual activity on receipt of an HIV test. Importantly, we were not able to separate tests done for routine screening during well-visits with tests done for symptoms of STI. Our analysis was based on tests performed and cannot account for tests that may have been offered and declined by patients. However, we feel that the outcome of tests performed rather than tests offered is more in line with the public health goal of expanded testing. Although our population likely included individuals engaging in condomless sex due to the suspicion of STI, our analyses were not able to account for other behavioral methods to prevent HIV acquisition such as pre-exposure prophylaxis, serosorting, and antiretroviral coverage among HIV-infected partners. Finally, because data before the passage of the New York State testing law were not available, we cannot confirm a causal association between the law and improvements in testing.
In conclusion, we found in a longitudinal analysis that HIV testing patterns at a large urban multilocation health care center for patients tested for GC or CT improved over time but missed significant opportunities for continued testing expansion. Strategies to target appropriate risk-based HIV retesting of patients with suspected STIs, especially in EDs and among adolescent patients, may help to reduce missed opportunities for testing. Education of providers in the settings studied regarding the importance of retesting individuals at ongoing risk for HIV (particularly adolescents), implementation of point-of-care testing for HIV, and further research with stakeholders to determine the perceived barriers to HIV testing are some of the possible interventions that could be taken to decrease these missed opportunities. The yield of HIV testing strategies is partly dependent on local prevalence and risk, and we expect optimal strategies to change over time as we continue efforts to curb the HIV epidemic.
Acknowledgments
Financial support. This work was funded by the National Center for Advancing Translational Sciences (UL1TR000457) and the National Institute of Mental Health (T32MH073553 to S.N.K.). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Chou R, Selph S, Dana T, et al. Screening for HIV: systematic review to update the 2005 U.S. Preventive Services Task Force recommendation. Ann Intern Med 2012; 157:706–18. [DOI] [PubMed] [Google Scholar]
- 2. Lundgren JD, Babiker AG, Gordin F, et al. ; Insight Start Study Group Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 2015; 373:795–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cohen MS, Chen YQ, McCauley M, et al. ; HPTN 052 Study Team Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006; 55(RR-14):1–17; quiz CE1–4. [PubMed] [Google Scholar]
- 5. Moyer VA; US Preventive Services Task Force Screening for HIV: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2013; 159:51–60. [DOI] [PubMed] [Google Scholar]
- 6. An Act to Amend the Public Health Law in relation to HIV testing, NY S 8227, A11487. Chapter 308 (2010). Available at: http://public.leginfo.state.ny.us/navigate.cgi?NVDTO. Accessed 20 May 2017. [Google Scholar]
- 7. Martin EG, MacDonald RH, Smith LC, et al. Mandating the offer of HIV testing in New York: simulating the epidemic impact and resource needs. J Acquir Immune Defic Syndr 2015; 68(Suppl 1):S59–67. [DOI] [PubMed] [Google Scholar]
- 8. Desai S, Nardone A, Hughes G, et al. HIV incidence in an open national cohort of men who have sex with men attending sexually transmitted infection clinics in England. HIV Med 2017; 18:615–22. [DOI] [PubMed] [Google Scholar]
- 9. Kelley CF, Vaughan AS, Luisi N, et al. The effect of high rates of bacterial sexually transmitted infections on HIV incidence in a cohort of black and white men who have sex with men in Atlanta, Georgia. AIDS Res Hum Retroviruses 2015; 31:587–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Graves SK, Little SJ, Hoenigl M. Risk profile and HIV testing outcomes of women undergoing community-based testing in San Diego 2008–2014. Sci Rep 2017; 7:42183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hosmer DW, Lemeshow S, Sturdivant RX.. Applied Logistic Regression. 3rd ed Hoboken, NJ: Wiley; 2013. [Google Scholar]
- 12. StataCorp. Stata Statistical Software. Release 14. College Station, TX: StataCorp LLC; 2015. [Google Scholar]
- 13. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 14. Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag New York; 2009. [Google Scholar]
- 15. Kennedy BS, Kern A, Ricci J, et al. Compliance with a New York State 2010 HIV testing law: is there racial/ethnic bias in HIV testing? Experience of Monroe County, New York, 2012. Ethn Dis 2016; 26:91–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Egan DJ, Cowan E, Fitzpatrick L, et al. Legislated human immunodeficiency virus testing in New York State emergency departments: reported experience from emergency department providers. AIDS Patient Care STDS 2014; 28:91–7. [DOI] [PubMed] [Google Scholar]
- 17. Leung SYJ, Sinclair AH, Battles HB, et al. HIV test offers and acceptance: New York State findings from the behavioral risk factor surveillance system and the national HIV behavioral surveillance, 2011–2012. J Acquir Immune Defic Syndr 2015; 68(Suppl 1):S37–44. [DOI] [PubMed] [Google Scholar]
- 18. Newton-Dame R, Wang JJ, Kim MS, Edelstein ZR, Cutler B, Tsoi BW. Evaluating the 2010 New York State HIV testing law in NYC ambulatory practices using electronic health records. J Acquir Immune Defic Syndr 2015; 68(Suppl 1):S15–20. [DOI] [PubMed] [Google Scholar]
- 19. Lazariu V, Parker MM, Leung SY, et al. New York State 2010 HIV testing law: an evaluation of testing rates using laboratory data. J Acquir Immune Defic Syndr 2015; 68(Suppl 1):S10–4. [DOI] [PubMed] [Google Scholar]
- 20. HIV Epidemiology and Field Services Program. HIV Surveillance Annual Report, 2016. New York: New York City Department of Health and Mental Hygiene; 2017. [Google Scholar]
- 21. Centers for Disease Control and Prevention. HIV Surveillance Report. Volume 27. Atlanta, GA: Centers for Disease Control and Prevention; 2015. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Accessed 20 Sept 2017. [Google Scholar]
- 22. Schnall R, Clark S, Olender S, Sperling JD. Providers’ perceptions of the factors influencing the implementation of the New York State mandatory HIV testing law in two urban academic emergency departments. Acad Emerg Med 2013; 20:279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schnall R, Liu N, Sperling J, et al. An electronic alert for HIV screening in the emergency department increases screening but not the diagnosis of HIV. Appl Clin Inform 2014; 5:299–312. [DOI] [PMC free article] [PubMed] [Google Scholar]