Abstract
Introduction
Increasing pressure and limitations on the NHS necessitate simple and effective ways for maintaining standards of patient care. This quality improvement project aims to design and implement user-friendly and clear ward round stickers as an adjunct to surgical ward rounds to evidence standardised care.
Project design and strategy
Baseline performance was measured against the recommended standards by the Royal College of Physicians, General Medical Council and a study performed at the Imperial College London. A total of 16 items were studied. All members of staff in surgery department were informed that an audit on ward round entries would be implemented but exact dates and times were not revealed. In the first cycle, ward round sticker was implemented and results collected across three random days for use and non-use of sticker. Feedback was collected through the use of questionnaires. In the second cycle, the ward round sticker was redesigned based on feedback and results collected for use and non-use of sticker.
Results
Baseline performance noted in 109 ward round entries showed that checking of drug chart, intravenous fluid chart, analgesia, antiemetic, enoxaparin, thromboembolic deterrents ranged from 0% to 6%. With the introduction of ward round stickers in both cycles, there was noticeable improvement from baseline in all items; in ward round entries where stickers were not used, performance was similar to baseline.
Conclusion
This quality improvement project showed that the use of stickers as an adjunct to surgical ward round is a simple and effective way of evidencing good practice against recommended standards. Constant efforts need to be made to promote compliance and sustainability. Commitment from all levels of staff are paramount in ensuring standardised patient care without overlooking basic aspects.
Keywords: quality improvement, surgery, compliance, audit and feedback, checklists
Introduction
Surgical ward rounds are often brief.1 A study in a hospital in New Zealand found that surgical teams spent an average of 2 min 57 s per patient visit at the bedside.2 They are often led by a senior decision maker and the team also consists of foundation year one (FY1) and foundation year two (FY2) doctors. In addition to ward round, senior decision makers have other commitments such as theatre, endoscopy and clinic; whereas junior doctors are expected to review unwell patients, address any concerns that the nursing staff may have, prepare discharge letters—responsibilities which in the face of worsening rota gaps, render time available for ward rounds and documentation increasingly short.3
The General Medical Council set out guidelines for clinical documentation in Good Medical Practice 2013 that clinical records should be clear, accurate and legible and they should include (1) relevant clinical findings; (2) the decisions made and actions agreed, and who is making the decisions and agreeing the actions; (3) the information given to patients; (4) any drugs prescribed or other investigation or treatment and (5) who is making the record and when.4 In conjunction with these guidelines, there exist recommended standards by the Royal College of Physicians5 and a study performed at Imperial College London.6 With these in consideration, a study that assessed the reliability of a model where junior doctors document surgical consultations held between consultants and patients showed deficiencies in clinical findings, management decision and information given to patients including the need for an operation.7
The use of checklists at surgical ward rounds have been studied by numerous centres, with a randomised clinical trial of the impact of a surgical ward-care checklist showing significantly improved standardisation, evidence-based management of complications and quality of ward rounds.8 A qualitative study looking at attempts to decrease central line infections also highlighted the significance of checklist in changing cultural practice and improving safety.9
As such, to ensure that good patient care at recommended standards is not at the expense of the brevity of surgical ward round, an audited and evidenced way of achieving this is sought. Following informal self-auditing and comments from coroners, documenting surgical ward round with the aid of checklist was thought to be an area for quality improvement. The aim was to promote good quality surgical ward round using stickers containing a checklist as an aid to documentation and evidencing that certain basic aspects of patient care were checked, such as drug charts, intravenous fluid charts, observation charts and so on.
The objectives were: (1) to design a user-friendly, clear, unambiguous ward round sticker; (2) to gather feedback on the usefulness of the sticker; (3) to measure and compare quality of surgical ward round against recommended standards with or without sticker; (4) to implement and educate surgical teams on the use of ward round sticker as an adjunct to good patient care. We introduced a ward round sticker following a data collection exercise to ascertain base performance against recommended standards. This audit project underwent two plan, do, study, act (PDSA) cycles and the results are presented.
Project design and strategy
Recommended standards were adopted from recommendations by the Royal College of Physicians and a study performed at Imperial College London.
Ward round entries in the inpatient notes on the surgical Beech Ward that houses 63 inpatient beds at the Worcestershire Royal Hospital were examined over 3 random days in September 2016 and data on base performance prior to the use of ward round stickers were collected. Sixteen (16) items were measured as per recommended standards and achieving at least 95% of an item being measured was considered good.
Beech Ward houses patients under General Surgery, Colorectal Surgery, Upper GI and Bariatric Surgery, and Ear, Nose and Throat Surgery. Data were collected for all surgical patients on Beech Ward except Ear, Nose and Throat Surgery as the project was carried out at the General Surgery department level.
First PDSA cycle
A ward round sticker was designed and introduced in the first cycle. Clinical members of the general surgery department, including consultants and junior doctors, were made aware of the stickers via email. Members of the ward round teams comprising of a senior registrar, two senior house officers, two FY1 trainees, were also verbally informed by the first and/or second authors every weekday morning in January 2017 prior to ward round, after which there were no verbal reminders. Except for the first and second authors, no other members knew of the dates for data collection.
During its implementation, data were collected over three random weekdays in January 2017 for both usage and non-usage of ward round stickers. Data were collected from alternate surgical patient’s note in the ward in the same direction through all data collection days that is, smallest numerical bed number first, then every second surgical patient and so on. Feedback were gathered verbally as well as through questionnaires. Descriptive statistics were used to analyse the data.
Results were presented at the general surgery department governance meeting following completion of data collection. Feedback was taken into consideration for the next PDSA cycle.
Second PDSA cycle
Following feedback from the general surgery department governance meeting and verbal feedback from ward nurses, pharmacists and doctors, dominant points were that the sticker was too large to fit onto patients’ notes, the boxes gave limited space, and there should be a space to document outstanding investigations or pending actions. These were taken into consideration when the sticker was redesigned for the second cycle.
Similar to the first cycle, clinical members of the general surgery department, including consultants and junior doctors, were made aware of the stickers via email. Again, prior to ward round, members of the ward round teams were verbally informed by the first and/or second authors every weekday morning in March 2017 without further verbal reminders thereafter. Apart from the first and second authors, other members of ward round teams were not aware of dates for data collection.
During the second cycle, data were collected over three random weekdays in March 2017 for both usage and non-usage of stickers in the same manner as first cycle.
Results
Items measured
Sixteen items were identified to be important in complying with the recommended standards and these were measured: (1) date; (2) time; (3) led by—which indicates the person leading the ward round, usually the most senior decision maker of the team; (4) remarks; (5) observations; (6) on examination; (7) drugs; (8) intravenous fluid; (9) analgesia; (10) antiemetic; (11) enoxaparin; (12) TEDs—thromboembolic deterrent stockings; (13) impression or diagnosis; (14) plan; (15) signature; (16) bleep.
Baseline
To ascertain baseline performance, ward round documentation in patient notes were checked for the items measured. Every alternate patient’s notes were checked across 5 days in December 2016. To ensure that the data were collected without performance bias, the ward round team members were not informed of the data collection exercise.
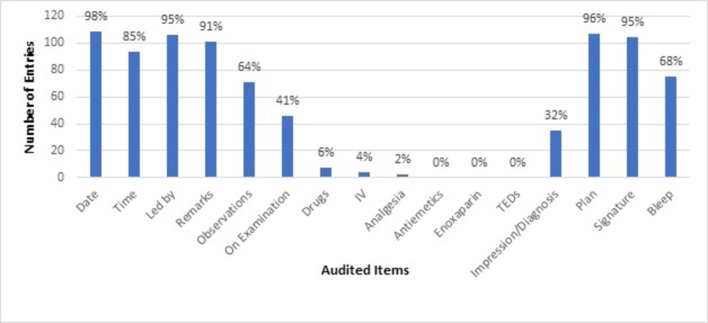
One hundred and nine (109) ward round entries were examined, and results are shown in figure 1. Results showed that there was no evidence in documentation to show that antiemetics, enoxaparin and TEDs were checked, and fewer than 10% of ward round involved checking drugs (6%), intravenous fluid (4%) and analgesia (2%). On the other hand, more than 90% of the ward round documentation contained date (98%), led by (95%), remarks (91%), plan (96%) and signature (95%).
Figure 1.
Baseline performance of 109 ward round entries. TEDs, thromboembolic deterrents.
First PDSA cycle
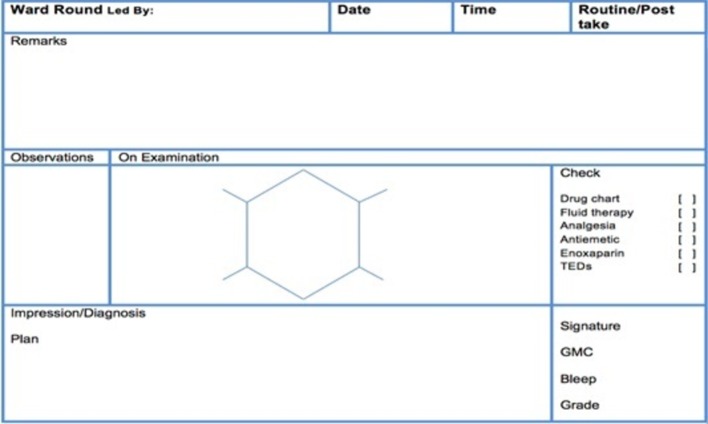
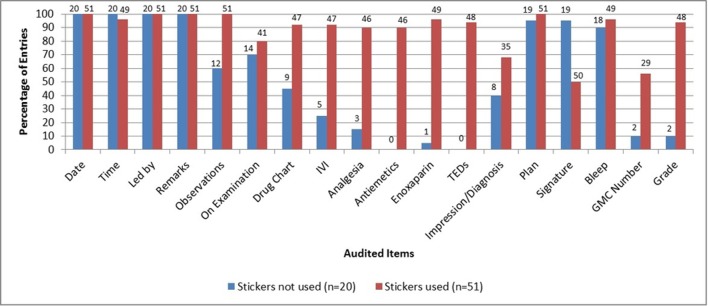
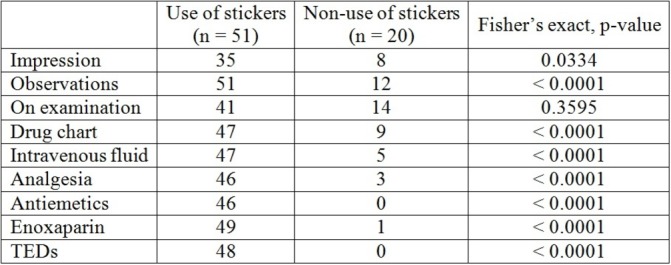
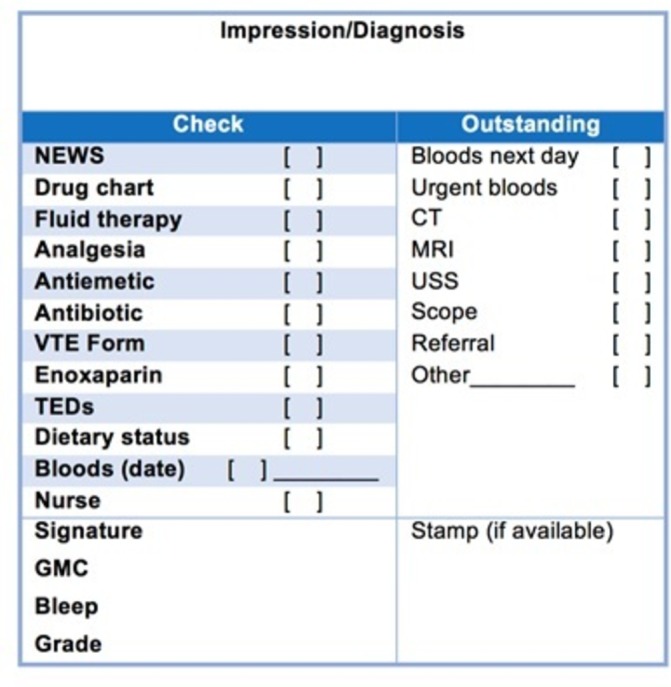
A total of 71 entries were examined. Out of these, 51 entries contained the ward round sticker and 20 did not. The ward round sticker used during this cycle is shown in figure 2. Results where ward round stickers were used in comparison to when they were not used are shown in figure 3. Questionnaire was distributed to doctors, nurses, pharmacists and dietitians who regularly used the inpatient notes, and responses and results are shown in figure 4.
Figure 2.
Ward round sticker in the first PDSA cycle. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
Figure 3.
Comparison when stickers were used (n=51) and when stickers were not used (n=20) during first PDSA cycle. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
Figure 4.
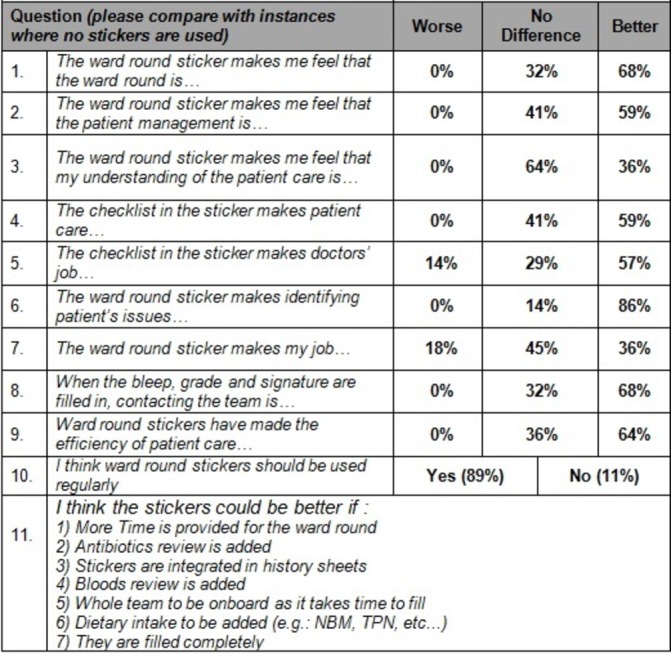
Summary of results from feedback questionnaire.
Results from the first cycle of audit without the use of ward round sticker demonstrated that performance in checking drugs, intravenous fluid, analgesia, TEDs, clexane and documenting impression/diagnosis was similar to baseline. On the other hand, there is a significant improvement in documentation and checking of these items when sticker was used (figure 5).
Figure 5.
Fisher’s exact p value of a number of measures during first PDSA cycle. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
From the feedback questionnaire (figure 4), 68% of respondents felt that use of ward round sticker made them feel that the ward round was better and 64% felt that efficiency of patient care was better. There was no overwhelming majority who felt that the sticker made patient care and patient management better (41% felt no difference vs 59% felt that it was better) although 86% of respondents found the ward round sticker made identifying patient’s issues better.
Second PDSA cycle
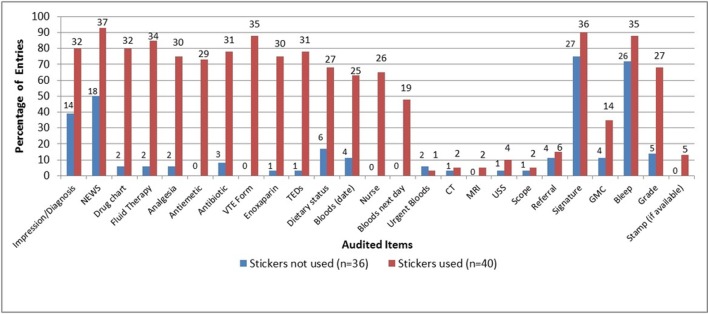
The ward round stickers were redesigned (figure 6) based on feedback. A total of 76 entries in notes were audited across three random days with the use of revised ward round sticker. Out of these, 40 entries contained the ward round sticker. The results were compared and shown in figure 7.
Figure 6.
Redesigned ward round sticker for second PDSA cycle following feedback. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
Figure 7.
Comparison when stickers were used (n=40) and not used (n=36) during second PDSA cycle. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
It was noted that without the use of stickers, documentation to evidence checking of eight items were below 10%—drug chart (6%), intravenous fluid (6%), analgesia (6%), antiemetic (0%), antibiotic (8%), venous thromboembolism (VTE) form (0%), enoxaparin (3%) and TEDs (3%). There was a significant difference (Fisher’s exact, p<0.0001, note figure 8) in these items measured between the use of stickers and non-use of stickers, emphasising the role of stickers in checking these items that are important aspects of basic care at ward round.
Figure 8.
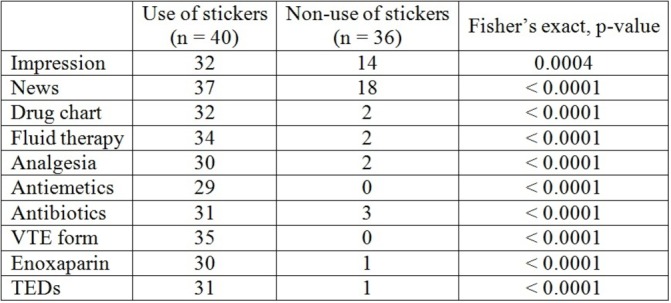
Fisher’s exact p value for a number of measures during second PDSA cycle. PDSA, plan, do, study, act; TEDs, thromboembolic deterrents.
Discussion and conclusion
Various studies exist in literature that demonstrate the effectiveness and advantages of ward round checklist, stickers or toolkits in improving patient care and evidencing good medical practice. In addition, lessons could be drawn from the positive outcomes in the study conducted by the Safe Surgery Saves Lives Study Group that concluded that checklist was associated with concomitant reductions in both rates of death and complications in patients undergoing non-cardiac surgery.10 The use of adjunct to ward rounds such as the stickers used in this audit demonstrated clearly that recommended standards could be met, hence evidencing good medical practice.
The ward round sticker provided a structured, standardised ward round practice where key elements would not be overlooked. Similar to a quality improvement programme in NHS Lanarkshire, ward round stickers in this audit were simple and acted as a safeguard aid memoir to ensure that perceived basic aspects of care were not missed while maintaining the standards.11 Results from this project have consistently shown that with the use of ward round stickers, there was a significantly clear evidence to show that key components such as VTE, analgesia, fluid therapy, antibiotic therapy, drug chart and so on were checked. Although there was no adequate data from our quality improvement project to show relationships between the use of checklist and respective patient outcomes, it was assumed that lack of documentation to evidence checking of aforementioned key components meant that they were potentially overlooked, thus falling short of recommended standards. In addition, it would be difficult in terms of study design, data collection and ethics to implement a quality improvement programme with data to robustly ascertain relationship between patient outcomes with the use of checklist or key components measured.
It is worth noting that data were not collected for surgical patients in outlier wards, as the number of outlier patients varied on a day-to-day basis ranging from none to fewer than 10 in total. Due to the variability in number and logistical reasons, it was thought that data collection should be limited to Beech ward only. One study identified response to a deteriorating patient and the care of outlier patients as error-prone processes,11 therefore perhaps future cycles in this quality improvement project should include data from outliers to identify areas for improving safety or standards unique to outlier patients, and whether checklist helps to maintain or improve standards of care.
Although the audit lead was not present at morning ward rounds where the stickers were to be used, the first and/or second authors formed part of the ward round teams, which might affect the uptake of stickers during the first and second PDSA cycles. It was difficult to determine from our results whether the presence of first and/or second authors had a significant impact on the uptake, as other factors contributing to engagement with the use of stickers included time and clinical commitment from senior decision makers, that is, senior registrars, designated scribe that could be a member other than the author(s), and self-awareness of all ward round members. It would be useful to see the effects on uptake if in future PDSA cycles the authors were excluded from ward rounds.
On one hand, successful implementation of a quality improvement project requires engagement from the management teams, senior clinicians, juniors and nurses. This audit project was implemented during a time when Worcestershire Acute Hospitals NHS Trust was under scrutiny based on poor performances according to care and quality commission standards, and it received attention and engagement from the senior management and clinician teams, hence providing strong encouragement for its introduction. Compliance would be limited by the number of ground staff that is, junior doctors, nurses available and lack of education. Education of junior medical staff and nurses was enforced through talks and presentations at junior doctors’ teaching sessions and regular reminders at nurses’ as well as juniors’ handovers. It is important to recognise that while there is a shortage of juniors and nurses, adjuncts and tools such as this are ever more important to ensure that safe standards are met at ward round, consequently in theory saving work hours that otherwise would be spent on rectifying overlooked aspects of patient care.
On the other hand, the sustainability of this quality improvement project requires continuous commitment from senior management teams, clinicians, juniors as well as local champions, as identified in other quality improvement projects.11 12 There was a drop in the use of ward round stickers between the first and second PDSA cycles (from 71% to 53%). Possible reasons included sampling error as random sampling method was used and members’ desensitisation to daily reminding to use of ward round stickers. Nevertheless, it highlights the importance of having a strategy for sustainability.
As discussed earlier, it was difficult from our results to measure the relationship between patient outcomes and the key components measured but lessons and results could be drawn from other similar quality improvement projects, especially involving data on impact to patient outcomes, to drive long-term compliance and engagement. Perhaps future PDSA cycles could capture concurrent data relating to incidences of VTE, drug errors, unnecessary fluid administration, antibiotics overuse, among others so that observations or assumptions could be drawn to use of ward round stickers.
Cost in printing the stickers, which were at £0.20 per sheet of two stickers (first PDSA cycle) and per sheet of four stickers (second PDSA cycle), was not insignificant due to volume, so this would need to be considered alongside other costs in the long-term, balanced with the perceived or measurable risks and impact to patient outcomes.
Following the completion of second cycle, implementation was expanded at the senior management level to include other departments—trauma and orthopaedics, ear, nose and throat surgery and gastroenterology—but the authors were not unable to collect data in those departments due to logistical limits, cost to time and limits posed by clinical commitments.
In addition to driving compliance and sustainability, further cycles of compliance measurement and improvement are needed to ensure that the objectives of this quality improvement project are met and maintained, perhaps with analyses to establish direct or indirect impact of ward round stickers on outcomes of hospital stay.
The findings from our quality improvement project showed that the use of ward round stickers as a checklist or aid memoir is a simple and effective way that could improve standards of patient care and serve as evidence that basic aspects of care were not overlooked. In order to drive compliance and sustainability, future cycles should include data collection and analyses, where possible, to relate the impact of ward round stickers on patient outcomes, as well as effects of continuous engagement from consultant body and senior management.
Acknowledgments
We would like to extend our sincerest gratitude to Mr Anthony Perry, consultant general and bariatric surgeon and Mr Steven John Robinson, consultant general and bariatric surgeon and department clinical audit lead, for their invaluable support and feedback to the project.
Footnotes
Contributors: JN planned the study. AA and JS collected the data. PW and AK provided advice and supervision. DN, SP and MZ provided support at the governance level. JN and AA worked towards writing and submitting the project.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: The audit was registered and approved by clinical audit lead at Worcestershire Acute Hospitals NHS Trust.
References
- 1. Force J, Thomas I, Buckley F. Reviving post-take surgical ward round teaching. Clin Teach 2014;11:109–15. 10.1111/tct.12071 [DOI] [PubMed] [Google Scholar]
- 2. Creamer GL, Dahl A, Perumal D, et al. Anatomy of the ward round: the time spent in different activities. ANZ J Surg 2010;80:930–2. 10.1111/j.1445-2197.2010.05522.x [DOI] [PubMed] [Google Scholar]
- 3. Fernandes D, Eneje P. Electronic printed ward round proformas: freeing up doctors’ time. BMJ Qual Improv Rep 2017;6:u212969.w5171–w5171. 10.1136/bmjquality.u212969.w5171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. General Medical Council. Good medical practice, 2013. [Google Scholar]
- 5. Royal College of Physicians, Royal College of Nursing. Ward rounds in medicine: principles for best practice. London: RCP, 2012. [Google Scholar]
- 6. Ahmed K, Anderson O, Jawad M, et al. Design and validation of the surgical ward round assessment tool: a quantitative observational study. Am J Surg 2015;209:682–8. 10.1016/j.amjsurg.2014.08.017 [DOI] [PubMed] [Google Scholar]
- 7. Fernando KJ, Siriwardena AK. Standards of documentation of the surgeon-patient consultation in current surgical practice. Br J Surg 2001;88:309–12. 10.1046/j.1365-2168.2001.01666.x [DOI] [PubMed] [Google Scholar]
- 8. Pucher PH, Aggarwal R, Qurashi M, et al. Randomized clinical trial of the impact of surgical ward-care checklists on postoperative care in a simulated environment. Br J Surg 2014;101:1666–73. 10.1002/bjs.9654 [DOI] [PubMed] [Google Scholar]
- 9. Dixon-Woods M, Leslie M, Tarrant C, et al. Explaining matching michigan: an ethnographic study of a patient safety program. Implement Sci 2013;8:70 10.1186/1748-5908-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491–9. 10.1056/NEJMsa0810119 [DOI] [PubMed] [Google Scholar]
- 11. Hale G, McNab D. Developing a ward round checklist to improve patient safety. BMJ Qual Improv Rep 2015;4:u204775–w2440. 10.1136/bmjquality.u204775.w2440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hassen YAM, Johnston MJ, Singh P, et al. Key Components of the Safe Surgical Ward: International Delphi Consensus Study to Identify Factors for Quality Assessment and Service Improvement. Ann Surg 2018. 10.1097/SLA.0000000000002718 [DOI] [PubMed] [Google Scholar]