Abstract
Background
Effective handover is key in preventing harm. 1 In the Acute Surgical Receiving Unit of Ninewells Hospital, Dundee, large numbers of patients are transferred daily. However, lack of medical handover during transfer means important tasks are missed. Our aim was to understand and reflect on the current system and test changes to improve medical handover.
Aim
Our aim was to ensure that 95% of patients being transferred from the Acute Surgical Receiving Unit receive a basic medical handover within 2 months.
Methods
Initially, we collated issues that were missed when patients were transferred. These data coupled with questionnaire data from members of the team fed into the creation of a handover tool. We proposed to link our tool with the nursing handover, hence creating one unified handover tool. We completed six full Plan-Do-Study-Act (PDSA) cycles (two on communication to aide handover and four on the tool itself) to assess and develop our tool.
Results
By our final PDSA cycle, 84% (33/39) of the patients had a handover, meaning no tasks were missed during transfer. After 4 months, 9 out of 10 staff felt that the introduction of the handover sheet made the handover process smoother and 8 out of 10 felt that the handover sheet improved patient safety and quality of care.
Conclusions
Improving handover can be challenging. However, we have shown that a relatively simple intervention can help promote better practice. Challenges are still present as uptake was only 84%, so work still has to be done to improve this. A wider cultural change involving communication and education would be required to implement this tool more widely.
Keywords: quality improvement, hand-off, patient safety, teamwork, communication
Problem
Ninewells Hospital in Dundee is Scotland’s second largest hospital and one of the country’s main trauma centres; by virtue, large numbers of patients are transferred to and throughout the hospital daily, meaning numerous opportunities for incomplete and absent handover.
Between 1 November 2015 and 1 November 2016, an average of 923 patients visited the Accident and Emergency Department in Ninewells Hospital per week.2 A significant proportion of these patients would later be admitted to the Acute Surgical Receiving Unit (ASRU) for further investigation and treatment.
ASRU is a 30-bedded unit divided into an assessment bay and a short-stay ward. Patients admitted with acute surgical conditions from Accident and Emergency would be seen in the assessment bay and later admitted to the short-stay ward for further treatment and stabilisation. Once stable, patients would be moved to Ward 8, a 24-bedded general transition ward, for further investigation and treatment. We estimated that on average five patients transferred to Ward 8 per day.
At present, patients are transferred from ASRU in Ninewells Hospital to the general ward (Ward 8) without any formal, structured medical handover. This means that important information such as test requests, drug dosing, investigation requests, and so on, may be lost during the transfer process due to lack of communication, resulting in compromise of patient care.
The aim of this project is to implement an effective and efficient multidisciplinary handover of patients being transferred from ASRU to the general surgical ward (Ward 8) over a period of 2 months.
Background
Handover is one the most important aspects of patient care. It is at the point of handover where patients are at most risk of having an aspect of their care missed.1 3 The consequence of poor handover cannot be underestimated as severe harm can come even if a small, yet key, bit of information is missed.1
Furthermore, issues over poor handover practices are widespread, despite concerted efforts to improve practice.4 In recent years, as the European working time directive has come into effect, junior doctors are on average working less hours, resulting in shorter shifts and consequently more frequent handovers.5
The key aim of handover is the transfer of robust, reliable yet relevant information retaining to the patient care from one clinician to another. Its role in providing continuity of care is undeniable. However, for handover to be effective, defined practices must take place and all those involved should have the same aims and objectives.6
To best understand how to improve handover it is vital to understand why it is not always effective. There is a multitude of factors that can influence handover with the most significant being effectiveness of the clinician themselves. Effective handover skills require aptitude in understanding and prioritising clinical need, and also non-technical skills such as communication, situational awareness and teamwork. It is clear though that in busy hospital environments even the most seasoned clinicians can be under high levels of pressure, with suboptimal handover often occurring as a result.7
Optimising handover and ensuring it is efficient is key. With a greater awareness of the importance of handover, many hospitals have designated handover times allowing teams to hand over in a structured manner. However, patient transfers often complicate this as they often happen at any time of the day and very rarely involve any direct medical handover.1 8 This was the issue we found in our own department; it was not practical to effectively hand over these patients during the day due to work pressures.
Other than defined processes and supportive environments what else can be done to help the handover process? Often simple handover tools can be useful in supporting the handover process; however, their use needs to be carefully placed with their context. The well-publicised ‘SHARE’ guidelines recommended areas that any new handover tools should focus on to be as effective as possible.9 These guidelines focused on the standardisation associated with pro forma handover tools. It also highlighted the need for education of those involved as well as a discursive relationship with the team to ensure they buy into and engage with the tool. Furthermore, introduction of tools must be done so with quality improvement methodology to ensure adaptive implementation.10
Introduction of a new pro forma handover can often be viewed as simply ‘another piece of paperwork’, and simply imposing it on clinical team can often have insight on poor compliance and engagement.11 12 Therefore, the use of the SHARE guidelines is a key principle to ensure adoption of a new tool is vital in ensuring it becomes embedded in a clinical environment.
The themes of the SHARE guidelines very much fit with the ethos of how we approached our project. We understood that healthcare-based environments have an inordinate amount of paperwork. As we discuss later, we focused on engaging all the parties involved, gaining their feedback and developing a tool that would complement existing systems. We ensured all those involved were educated in its benefits and how to use it effectively. This allowed us to develop a tool aligned with the SHARE guidelines and maximise the most positive benefit with regard to handover.
NHS Tayside has a well-structured handover policy; this is most evident in the effective and structured Hospital at Night handover process. This system was created almost 10 years ago to minimise errors from poor handover at the beginning and end of shifts.13 Further to this, the health board trains and supports junior doctors in both the principles and practicalities of handover during their induction.14 Despite this, the hospital has hundreds of inter/intradepartmental transfers every day in which there is no formal handover process. This project highlights one of these specific examples within the surgical department and acts to improve it.
Around 10 patients are transferred from the receiving ward daily to each of the six other surgical wards. With current staffing levels it is impractical for one junior doctor to hand over to all the other medical teams downstream face to face. Previous attempts at introducing handover tools were not universally employed. Often medical staff were not aware when patients were moved and there was no protected time to hand over, unlike the current processes set in place with the Hospital at Night team.
Handover is most effective when all members of clinical team are involved and engaged in good handover practice,1 an ethos that drove this project.
Baseline measurement
A questionnaire was developed and sent out to Foundation Year 1 Doctors (FY1) who have worked on either ASRU or Ward 8 in the previous 6 months (n=26). This showed that 9 out of 15 responders have never received any form of handover related to patient transfers.
When asked about the commonly missed tasks for patients who are transferred from ASRU without a handover (table 1), antibiotic levels and prescribing were noted to be the most commonly missed by all of the respondents. Eight of the respondents suggested that the second most commonly missed tasks were requesting blood tests and the administration of medication doses. Seven of the respondents suggested that missing paperwork on transfer was another common issue, as were missed radiology requests and missed referrals to other specialties (six of the respondents). Senior reviews prior to transfer from ASRU, endoscopy requests and repeat troponin I blood tests were also commonly missed according to five of the respondents.
Table 1.
Commonly missed tasks between ASRU and Ward 8
| Task missed due to lack of handover | Frequency (%) |
| Antibiotic levels (gentamicin and vancomycin) and prescriptions | 15/15 (100) |
| Blood test request | 8/15 (53) |
| Medication doses | 8/15 (53) |
| Patient paperwork | 7/15 (47) |
| Radiology requests | 6/15 (40) |
| Referrals to other specialties | 6/15 (40) |
| Senior review | 5/15 (33) |
| Endoscopy requests | 5/15 (33) |
| Repeat troponin I blood test | 5/15 (33) |
ASRU, Acute Surgical Receiving Unit.
Design
Following analysis of the problem, it was clear that a structured handover which was efficient, informative and to the point was necessary to improve the quality of information passed over between the two wards and thus improve patient safety on transfer. We concluded that a simple, clear handover tool which is able to stand out from the large volume of patient notes would be key to improve the handover of patients being transferred from ASRU to Ward 8. There is a variety of standardised handover tools available; however, we identified that there were a number of specific tasks related to the surgical department that were not being handed over. Moreover, as we were incorporating this new tool with an already established nursing one, we decided to create our own bespoke tool that was best suited to ASRU.
This led to the development of a single-page handover sheet which included:
Patient name and Community Health Index Number.
Date and time of transfer.
Presenting complaint.
Provisional diagnosis.
A list of jobs which need to be completed after transfer.
The name, bleep number and signature of the doctor completing the handover form.
Steps were taken to ensure that the handover tool was simple, quick and easy to complete. None of the above sections (1–6) required more than a few words, with section 5 being presented as a list of jobs with tickboxes which can be used to indicate which commonly required jobs still need to be completed by the receiving team in Ward 8. Furthermore, the handover tool was printed on brightly coloured paper in order to make it stand out when placed among other papers in the transfer notes.
The handover tool was also accompanied by two separate instruction sheets detailing the guidelines for use of this new handover tool by both medical and nursing staff. These instruction sheets were placed on the wall in the doctors’ room and nursing station in order to allow users to quickly and easily access guidance for the new handover process.
Strategy
Our aim was to develop a handover tool so that 95% of patients being transferred from ASRU had a medical handover over a 2-month period. We undertook six Plan-Do-Study-Act (PDSA) cycles (see online supplementary file), four of which focused on the handover tool itself; with two cycles focusing on the use of a communication tool to support this (these both ran in parallel to cycles 2 and 3).
bmjoq-2017-000154supp001.docx (102KB, docx)
PDSA cycle 1: creating and introducing our tool
This cycle focused on creating and introducing the tool. As discussed, we collected data both from feedback and quantitative assessment of problems relating to handover. In collaboration with colleagues we created our first handover tool that would be attached to the already established nursing Situation, Background, Assess, emt Recommendation (SBAR) handover. The aim of the tool was to be simple, straightforward and easy to complete. This involved simple tickbox sections to focus on the issues that needed to be handed over.
Once complete we decided to introduce the tool over the course of one working day in ASRU. During this time, all six patients who transferred that day had a medical handover completed. Despite achieving a 100% compliance with using the handover tool, we felt this would be difficult to replicate as teams would change daily. However, it demonstrated the tool worked in principle. Issues included two forms having no patient identification on them as well as nursing staff leaving the forms in nursing notes and not directly giving them to the doctors involved. As a result, this led us to address effective communication of the new handover tool and introduce specific tools to do this, that is, a poster.
PDSA cycle 2: second 1-day trial with support of a communication tool
With a positive outcome from our first cycle, the second cycle focused on developing use of the tool. We decided to have a focus on communication with this cycle and developed a tool that was in the form of a simple poster that would be displayed in the clinical areas involved.
To compare directly with the previous cycle, we decided to once again test the tool over the course of 1 day. Of the five patients transferred, three had a completed form, with two patients not having any handover. This occurred as one of the nurses involved did not have an awareness of the trial and therefore did not prompt a handover to be completed. This highlighted the need for effective communication within the team to ensure full awareness and engagement. This cycle also highlighted an improvement for the tool, in that a documented date and time would be useful to plan jobs created from the tool. With regard to our communication tool in the form of a simple poster, feedback stated that though the poster was useful it was too complex and needed to be simplified.
PDSA cycle 3: 5-day trial with improved communication tool
At the outset of our third cycle it was clear that communication within the team was key to ensure the tool was effectively used. Because of this, we introduced a simplified communication tool in the form of a poster. This was placed in clinical areas in the relevant ward spaces and was eye catching and easy to understand. We also modified the handover tool to ensure it could be used contemporaneously with a date and time section.
We wanted to extend the use of the tool to over a 5-day period to assess how our tool coped with different clinical teams. To achieve this, we reached out to the nursing lead for ASRU who was keen and supportive of our improvement project. He was able to engage all of his nursing staff with our tool so different clinical teams were aware of the tool and how to use it.
In this cycle we achieved 83% (15/18 forms) of patients having a medical handover completed; however, seven of these forms (40%) were not handed over to the doctor when the patient arrived in the ward. Feedback highlighted that nursing staff were not always aware of the trial and that the communication tool was overlooked, despite being simplified. It was felt that more direct communication, either via email or from one-to-one contact, would be more effective. Another issue highlighted was that even though the tool handed over the need for gentamicin and vancomycin levels it did not have a facility for detailing the exact time for the level to be taken, which in itself could cause confusion.
PDSA cycle 4: 2-week trial (including out of hours) with a focus on direct communication
During this fourth cycle we decided to change our approach to how we communicated our tool. We decided that focus on direct communication with all the staff involved, either via email or one-to-one contact, would be a more effective way to ensure the whole team was engaged. We also edited the tool again with a specific vancomycin and gentamicin level section in which the time it was required could be clearly written.
For our final test we rolled out our tool over a 2-week period; this allowed us to test how robust the tool was with more clinical teams, and how effective it was in an out-of-hours setting. During normal clinical hours our tool was used 84% of the time (33/39 forms). This was a modest increase compared with our previous cycle but this was in context of the tool being used by far more clinical teams, indicating that this factor was not negatively impacting its use. During out of hours our tool was only used 37.5% of the time (three out of eight forms), highlighting the difficulties of using the tool in such environments with lower medical staffing. It was also noted that 15 out of the 39 handover forms (38%) were missing patient identification details, a key problem if they are going to be used as an effective mode of transferring patient information. A significant factor affecting use was that specific staff were not engaging with its use, most staff were completing it 100% of the time but some were not completing it at all. This highlighted that if this tool were ever to work effectively and be embedded, all the members of the team needed to be engaged. Therefore, we needed to ensure we were not simply imposing this on members of the team but communicating with them directly and gaining their feedback.
Results
After 4 months and four PDSA cycles, a second follow-up questionnaire was sent out to the FY1s working in ASRU and Ward 8, this time with 10 respondents. This questionnaire highlighted that:
Only 2 out of the 10 respondents never had a formal, structured handover over these 4 months compared with 9 out of 15 prior to the introduction of the handover tool.
Nine of the 10 respondents felt that the introduction of the handover tool made the handover process smoother.
Eight of the 10 respondents felt that the handover sheet improved patient safety and quality of care.
When asked about the commonly missed tasks for patients who are transferred from ASRU without a handover (table 2), the monitoring of antibiotic levels was still the most commonly missed task according to 5 of the 10 respondents. This does mean, however, that there has been an improvement from the previous 100% of respondents (15/15) who felt this was missed before the introduction of the handover tool.
Table 2.
Results from questionnaire after introduction of handover sheet
| Task | Frequency missed prior to introduction of handover sheet (%) | Frequency missed after introduction of handover sheet (%) |
Change (%) |
| Antibiotic levels (gentamicin and vancomycin) and prescriptions | 15/15 (100) | 5/10 (50) | −50 |
| Blood test request | 8/15 (53.3) | 4/10 (40) | −13.3 |
| Medication doses | 8/15 (53.3) | 1/10 (10) | −43.3 |
| Patient paperwork | 7/15 (46.7) | 1/10 (10) | −36.7 |
| Radiology requests | 6/15 (40) | 4/10 (40) | 0 |
| Referrals to other specialties | 6/15 (40) | 1/10 (10) | −30 |
| Senior review | 5/15 (33.3) | 1/10 (10) | −23.3 |
| Endoscopy requests | 5/15 (33.3) | 4/10 (40) | +6.7 |
| Repeat troponin I blood test | 5/15 (33.3) | 0/10 (0) | −33.3 |
Four of the 10 respondents thought that blood tests requested were being missed (down from the previous 8/15: 53.3%) as well as endoscopy requests (up from previous 5/15: 33.3%) and radiology requests (same as previous 6/15: 40%). Missed administration of drug doses, missing paperwork, missing senior reviews and missed referrals to other specialties were only reported by 1 of the10 respondents. This is an improvement from previous questionnaire: 8/15: 53.3% (missed administration of drug doses), 7/15: 46.7% (missing paperwork), 5/15: 33.3% (missed senior reviews) and 6/15: 40% (missed referrals to other specialties). Repeat (sixth hour) troponin I requests were never missed according to the 10 respondents, an improvement from the previous 5/15: 33.3% before the handover tool was introduced.
The above data are an accurate reflection of the data obtained from analysis of the handover tools completed during the trial period. In fact, at the end of the 2-month period, 84% (33/39) of the patients transferred between ASRU and Ward 8 had a completed handover. Figure 1 charts the trend of the proportion of completed handovers over the course of the four PDSA cycles highlighting the number of handovers at each stage.
Figure 1.
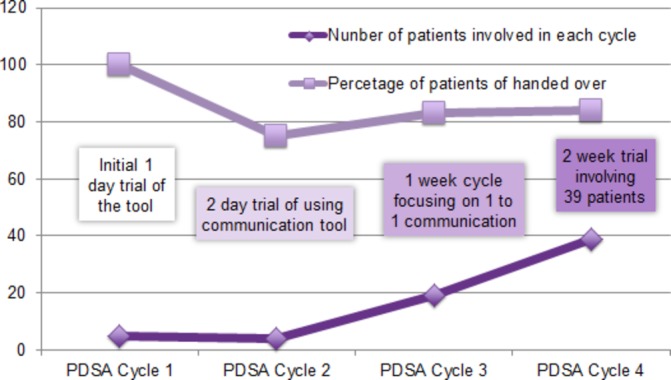
The percentage of completed handover at each Plan-Do-Study-Act (PDSA) cycle.
Lessons and limitations
The aim of this project was to improve the medical handover of patients being transferred from ASRU. As described, various strategies had been attempted in the past to try and improve this but never gained much traction or engaged the majority of staff. Our proposal was simple: to look at the processes involved and assess the barriers that prevented simple handovers from occurring.
One of the key issues was when patients were transferred to other wards and staff were not always necessarily aware, meaning by the time they had come to hand over the issue the patient and their notes had already left the ward. Furthermore, owing to the fact that between 8 and 10 patients could be transferred in 1 day the medical staff did not have the time practically to hand them over in person.
Our proposal was novel; as we aimed to use the already established nursing handover as a conduit to help facilitate improved medical handover. This meant that a truly multidisciplinary approach would need to be sought to engage all involved.
On the basis of this when we set out to create our tool, rather than to simply impose a premade tool, we worked with a number of parties within the multidisciplinary team, including, junior doctors, ward clerks, physician associates and nursing staff. We formed a draft which acted to complement and work with the current nursing handover. We went over the draft with the different team members mentioned at each PDSA cycle using their thoughts and feedback to adapt and improve the tool. Though this was quite time consuming we felt it worked to both optimise the tool and to engage each member of the team, allowing them to feel part of this change and therefore be more willing to enact it.
As stated, numerous hospital transfers occur within hospitals every day so the aim of the project was to perfect our own tool so it could be implemented throughout the surgical department. To this end, four PDSA cycles were vital in allowing us to assess, reflect and plan each step of the process as we went along.
A challenge we faced from the outset was embedding a change that required active action from a number of parties which included permanent nursing staff as well as daily rotational medical staff, thus requiring interface with a large number of people.
The biggest issue highlighted throughout each of the PDSA cycles was communication. The process involved a wide range of staff, ensuring everyone was aware of the process all of the time was difficult. This was shown in the Results section as many of the patients who had missed handovers were often due to the nursing staff not prompting doctors to complete the handover or the form not being handed to the doctor at the transfer ward. On review of these cases, the reason for non-completion was simply due to lack of awareness, highlighting that work needs to be done to improve communication between all members of the team.
We learnt early on that a simple communication tool, in the form of a poster, was not effective. Simple posters, even if they are relatively eye catching, are often overlooked in busy ward environments. Furthermore, often wards are littered with posters denoting guidelines, memorandums and protocols, meaning that a new addition to these already crowded displays often goes unnoticed. What we found out was that direct communication was far more effective. Emailing those involved or simply talking to staff on a one-to-one basis, explaining the project, its aims and the process involved, engaged team members far more. However, this is extremely labour intensive and it would therefore require a significant amount of effort from all involved to effectively embed the tool.
On reflection, the tool worked best when nursing staff were engaged. This underlines a key strength of this project. Every hospital has the factor of rotational medical staff affecting continuity; however, if nursing staff are engaged with any active change it appears to be more successful, as in this case.
What are the limitations of the project? Our target of 95% completed handover was ambitious and with the factors discussed it will always be difficult to ensure all patients get the handover required even if communication is optimised. This is further complicated by other factors such as transfers via theatre or high dependency. Moreover, this project looked at the transfer between two wards to demonstrate the principle of the tool in action. The next step is to upscale the use of the tool as numerous interward transfers happen every day in hospital in which there is a risk of loss of key information around a patient’s management. To do this, we plan to present our data to key clinical service managers; then on approval we work with individual ward teams to discuss how this could be implemented and potentially personalised to different services. This could involve ‘handover champions’ based in each unit that would support and develop the embedding of this tool into their clinical environments.
Another limitation of this project is assessing the impact of the tool directly. The project aimed to analyse and improve handover of a variety of tasks, meaning a simple objective measure of improvement is difficult to ascertain. Obvious measures to use are the rate of completed handover as well as feedback directly from staff involved. Even though feedback from staff has been extremely useful and demonstrated that the vast majority felt the tool made a positive impact, lack of quantifiable outcome data means the effect on patient safety and possible saved monetary costs are far harder to demonstrate.
Looking forward, there is still a significant amount of work to be done to take this tool forward. This project has shown that the principle of incorporating medical and nursing handover is an effective way of handing over important tasks that might otherwise be missed.
However, for this tool to be embedded and used, it needs to overcome the hurdles of wider implementation as well as the change of a 4-month rotation of junior doctors.
We plan to work with the current cohort of foundation doctors to fully bed in the tool over the coming months, so the tool will be robust enough to help augment and support new FY1s as they start. To do this, however, several more PDSA cycles and then subsequent extensions throughout the surgical department will need to occur to ensure it is robust and effective.
Conclusion
This project has shown that by integrating nursing and medical handover the transfer of important tasks can be improved. This fundamentally links in with our overarching aim of improving the rate of handover from the surgical receiving unit.
However, we did not reach our target of a handover rate of 95%, peaking at 84% in our final PDSA cycle. On reflection, we could have adjusted our target more as we went on as it became clear that even in optimal circumstances 95% may be difficult to reach.
Moreover, objectively measuring outcomes for this project was difficult. The rate of handover is one obvious measure; however, this in itself does not assess the impact of the intervention on patient safety. We only assessed the subjective feelings of those involved via feedback; although very insightful, it was not quantifiable, and for future assessment of this tool an objective measure to assess patient safety should be sought.
This project offers an easily reproducible intervention with regard to handover. In many departments, medical and nursing staff have different systems and procedures. Our project shows that if their combined effort is channelled a previous deficit can be filled without a huge burden on time and effort.
Therefore, this project can act as a clear example of how multidisciplinary working can positively affect the care of patients.
Acknowledgments
Special thanks to all the medical and nursing staff of both ASRU and Ward 8 who helped implement this tool and to VT for her support and guidance during this project.
Footnotes
NR and GM contributed equally.
Contributors: This project was planned and designed both equally by NR and GM. NR designed and produced the initial handover prototype in collaboration with the MDT. GM collected both the pre/postintervention questionnaire data as well as developing communication tools. Both GM and NR collected the live data of the handover process throughout the four PDSA cycles. VT provided support and guidance on how to complete and approach a quality improvement project as the hospital lead for patient safety and quality improvement; she also supported with the editing revisions of this submission. KC (Physician Associate in ASRU) was key in helping to implement this tool and collect data through the four PDSA cycles. NR drafted the majority of this revision with support from GM with the baseline measurement and results sections as well as the figures/tables.
Funding: This project received no direct funding from any internal or external bodies. The publishing costs were funded by NHS Tayside’s subscription to BMJ Open Quality as the manuscript was initially submitted in June 2017.
Competing interests: None declared.
Ethics approval: This was a quality improvement project and in line with NHS Tayside policy is exempt from ethical approval.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. The Royal College of Surgeons of England. Safe handover: guidance from the working time directive working party. London: RCS, 2017. [Google Scholar]
- 2. Information Services Division Scotland. NHS Performs - weekly update of emergency department activity and waiting times statistics. 2016. http://www.isdscotland.org/Health-Topics/Emergency-Care/Publications/data-tables.asp?id=1823#1823 (cited Jan 2017).
- 3. Farhan M, Brown R, Woloshynowych M, et al. The ABC of handover: a qualitative study to develop a new tool for handover in the emergency department. London: BMJ - Emergency Medicine Journal, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Horowitz LI, Krumholz HM, Green ML, et al. Transfers of patient care between house staff on internal medicine wards: a national survey. London: Archive Internal Medicine, 2006. [DOI] [PubMed] [Google Scholar]
- 5. Roughton VJ, Severs MP. The junior doctor handover: current practices and future expectations. London: Journal Royal College Physicians, 1996. [PMC free article] [PubMed] [Google Scholar]
- 6. The Royal College of Surgeons of England. Good Surgical Practice. London: RCSE, 2002. [Google Scholar]
- 7. Pezzolesi C, Manser T, Schifano F, et al. Human factors in clinical handover: development and testing of a ‘handover performance tool’ for doctors’ shift handovers. Int J Qual Health Care 2013;25:58–65. 10.1093/intqhc/mzs076 [DOI] [PubMed] [Google Scholar]
- 8. The Royal College of Physicians. Acute Care Toolkit 1: Handover. London: RCP, 2011. [Google Scholar]
- 9. Joint Commission Center for Transforming Healthcare Releases Targeted Solutions. Tool for Hand-Off Communications Joint Commission Perspectives.32. [PubMed] [Google Scholar]
- 10. Pucher PH, Johnston MJ, Aggarwal R, et al. Effectiveness of interventions to improve patient handover in surgery: A systematic review. Surgery 2015;158:85–95. 10.1016/j.surg.2015.02.017 [DOI] [PubMed] [Google Scholar]
- 11. Urbach DR, Govindarajan A, Saskin R, et al. Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med 2014;370:1029–38. 10.1056/NEJMsa1308261 [DOI] [PubMed] [Google Scholar]
- 12. Borchard A, Schwappach DL, Barbir A, et al. A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg 2012;256:925–33. 10.1097/SLA.0b013e3182682f27 [DOI] [PubMed] [Google Scholar]
- 13. Chalmers J. Hospital at night, operational policy manual. Dundee: NHS Tayside, 2006. [Google Scholar]
- 14. Sloan J, Tully V, Chandrashekar H. Handover of Care: NHS Education Scotland: Ninewells Hospital Dundee, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2017-000154supp001.docx (102KB, docx)


