Abstract
Objective
This study examined the relationship between sleep duration, sleep quality and food consumption among adolescents.
Design
Cross-sectional study.
Setting
Data from the 2014 and 2015 Korea Youth Risk Behavior Web-based Survey were used.
Participants
Participants aged 12–18 years (n=118 462 (59 431 males and 59 031 females)) were selected.
Primary and secondary outcome measures
Sleep duration, sleep quality and the frequencies of fruits, soda, soft drinks, fast food, instant noodle, confectionaries, vegetables and milk consumption.
Results
Short sleep durations (<6 hours) were associated with higher soft drinks and confectionaries intake than longer sleep durations (9+ hours) (adjusted ORs (AORs) (95% CIs) for ≥5 times a week for soft drinks: 1.73 (1.57 to 1.91) and confectionaries: 1.32 (1.20 to 1.46); p<0.001). Poor sleep quality, with 7–8 hours of sleep, was associated with a lower intake of fruits, vegetables and milk (AORs (95% CIs) for ≥5 times a week for fruits: 0.71 (0.65 to 0.77); vegetables: 0.66 (0.58 to 0.75); and milk: 0.80 (0.74 to 0.86); each p<0.001), and higher intake of soda, soft drinks, fast food, instant noodle and confectionaries (AORs (95% CIs) for ≥5 times a week for soda: 1.55 (1.40 to 1.70); soft drinks: 1.58 (1.43 to 1.73); fast food: 1.97 (1.65 to 2.35); instant noodle: 1.55 (1.37 to 1.76); and confectionaries: 1.30 (1.18 to 1.43); each p<0.001) than good sleep quality of the same duration.
Conclusion
Short sleep durations and poor sleep quality might be associated with higher consumption of unhealthier foods, such as sugar-sweetened beverages, fast food, instant noodle and confectionaries, and associated with lower consumption of fruits, vegetables and milk.
Keywords: sleep duration, sleep quality, food consumption, food frequency, sugar-sweetened beverages, fast food, fruits, vegetables, adolescents, Korean
Strengths and limitations of this study.
Our study was conducted on a representative population of Korean adolescents.
We considered numerous socioeconomic status variables as confounding factors to investigate the independent relationship between sleep status and food consumption.
We considered sleep duration and sleep quality in explaining sleep status.
Our study was based on secondary data, and it has some limitations in providing specific information.
Because the data were collected based on a self-reported questionnaire, the precision of the information may be low.
Introduction
Sufficient sleep in adolescents is important to maintain good health status and school performance. According to the National Sleep Foundation,1 approximately 8–10 hours of sleep a night is best for adolescents. However, sleep durations for adolescents have been declining.2 The reasons for decreasing sleep durations and reduced sleep quality among adolescents have been suggested to be associated with increased use of the internet and social media and earlier school start times.3 4 Inadequate sleep durations or quality could lead to poor school performance, physical health problems such as atopic conditions, headaches, mental health problems and unhealthy behaviours.4–7
One of the outcomes of sleep deprivation among adolescents is obesity,8 which has become a serious public health problem worldwide.9 The fundamental factor leading to obesity is an energy imbalance between the calories consumed and the calories expended10; therefore, dietary factors are closely related to the prevalence of obesity11 12 and are considered as a potential link between sleep deprivation and obesity in adolescents. According to previous studies, the intake of fruits, vegetables and milk has a positive association, and the intake of sweets, snacks and fast food has negative association with sleep duration.13–15 In short, adolescents who get less sleep may be more likely to consume more calories in the form of fast foods, sweets and snacks and fewer micronutrients than adolescents who get more sleep. Previous studies demonstrated that one of the possible reasons for sleep deprivation in association with the consumption of higher energy foods might be changes in hormones such as decreased leptin and increased ghrelin levels, which can lead to an increase in appetite.16 17 In summary, sleep deprivation in adolescents might affect dietary habits as a factor of health problems including obesity.
In Korea, the prevalence of childhood obesity in males and females was 15.3% and 11.1% in 2016, respectively, and it increased steadily since 2010.18 Lee, who performed a study using the Korea Youth Risk Behavior Web-based Survey (KYRBWS), reported that <7 hours of sleep per night in high school students was associated with increased cracker consumption.19
Meanwhile, studies of sleep deprivation should consider sleep duration and sleep quality. However, few studies have investigated the relationship between sleep duration, along with sleep quality, and the intake of various foods while also adjusting for the numerous confounding factors among adolescents in population-based datasets. Lee used KYRBWS data, which is population-based datasets containing numerous variables, but she did not consider the sleep quality.19 The aim of our study was to identify the associations between sleep duration, sleep quality and food intake among adolescents by using KYRBWS datasets. We used the data of the participants’ level of recovery from fatigue after sleeping as sleep quality.
Materials and methods
Data collection
The Institutional Review Board (IRB) of the Centers for Disease Control and Prevention of Korea (KCDC) approved this study (2014-06EXP-02-P-A). Written, informed consent was obtained from each participant prior to the survey. Because this web-based survey was performed at schools and included a large number of participants, informed consent from their parents was exempted. This consent procedure was approved by the IRB of KCDC.
This was a cross-sectional study using data from the KYRBWS, covering only Korea and using statistical methods based on a designed sampling method and adjusted, weighted values. The results from the KYRBWS conducted in 2014 and 2015 were analysed. The data were collected by the KCDC.
Participants
The survey consists of 125 questions assessing demographic characteristics and health-related behaviours. Korean adolescents from 7th to 12th grade completed the self-administered questionnaire voluntarily and anonymously. Using 43 regions (considering administrative districts, geographic accessibility, the number of schools and population size) and the school participants attended, the mother population was stratified into 129 levels to identify the sample distribution. Groups were then selected using stratified, two-stage (schools and classes) clustered sampling based on data from the Education Ministry. Sampling was weighted by statisticians, who performed a poststratification step and considered non-response rates and extreme values. Detailed methods are described at the KYRBWS website (https://yhs.cdc.go.kr/new/pages/main.asp).
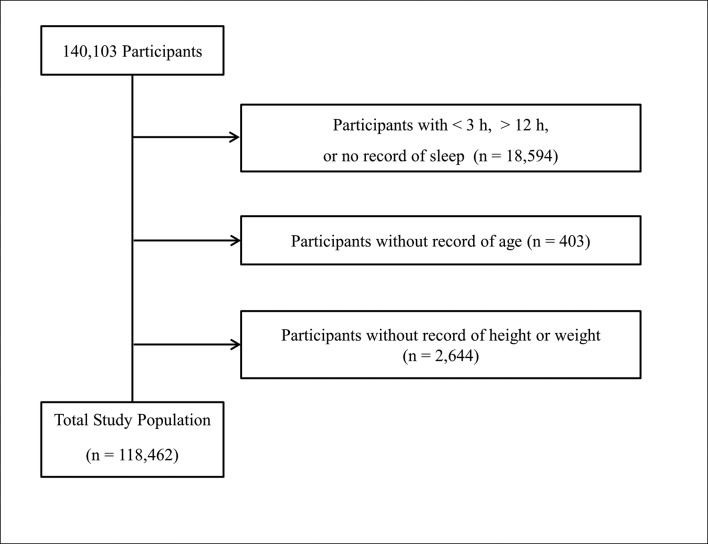
Of a total of 140 103 participants, we excluded the following participants from analysis in this study; participants who slept less than 3 hours or more than 12 hours per night or who had no sleep records (18 594 participants); participants who did not give their age (403 participants); and participants without height or weight data (2644 participants). Finally, 118 462 participants (84.5% of total participants; 59 431 males; 59 031 females; 12–18 years old) were included in this study (figure 1).
Figure 1.
A schematic illustration of the participant selection. From a total of 140 103 participants, those getting <3 hours or >12 hours of sleep per night or with no sleep records (n=18 594), without a record of their age (403) or without height or weight data (2644) were excluded. The data for the 118 462 participants from whom complete records were obtained were analysed.
Patients and Public involvement
Patients and public were not involved in the design and development of this research.
Sleep duration and sleep quality
The times at which participants fall asleep and wake up were recorded to within 10 min. The participants were asked the time they fall asleep and the time they wake up for the seven most recent days classified into weekdays and weekends. Sleep duration was calculated by subtracting the time they fall asleep from the time they wake up. The mean daily sleep duration was calculated by adding weekday and weekend sleep durations with weights of 5/7 and 2/7, respectively. Sleep duration was divided into five groups: <6 hours (less than 6 hours), ≥6 hours and <7 hours (6 hours), ≥7 hours and <8 hours (7 hours), ≥8 hours and <9 hours (8 hours) and ≥9 hours (9+ hours). The participants were asked about their recovery from fatigue after sleeping for the seven most recent days (quality of sleep). The answer options were very good, good, moderate, poor and very poor. We regrouped answers into three groups of sleep quality to simplify the categories: good (very good and good), moderate and poor (poor and very poor). We analysed the association between sleep quality and food consumption only in the 7-hour and 8-hour groups as sleep duration was closely related to its quality (online supplementary S1 table).
bmjopen-2018-022848supp001.pdf (191.1KB, pdf)
Food intake frequency
The KCDC collected the participants’ certain food intake frequencies in the seven most recent days. The foods were fruits (not fruit juice), soda, soft drinks (including sports drinks, coffee-based beverages and fruit drinks; excluding soda), fast food (such as pizza, hamburgers or chicken), instant noodle, confectionaries, vegetables and milk. The data were divided into four groups: ≥5 times a week, 3–4 times a week, 1–2 times a week and 0 times a week.
Health examination and socioeconomic status
The participants were asked their weight (kg) and height (cm). Obesity levels were categorised into four groups according to the Centers for Disease Control and Prevention guidelines regarding body mass index (BMI; kg/m2) for children and teens20 as follows: obese: ≥95th percentile; overweight: ≥85th percentile and <95th percentile; healthy weight: ≥5th percentile and <85th percentile; and underweight: <5th percentile. The region of residence was divided into three groups by administrative district: large city, small city and rural area. Subjective self-assessments of health were divided into five groups, from very good to very bad. The stress level of participants was divided into five groups: severe, moderate, mild, a little and no stress. Self-reported economic level was grouped into five levels, from the highest to lowest. Parent educational level was divided into four groups: graduated college or higher, graduated high school, graduated middle school or below, unknown and no parents. The participants who did not know the educational level of their parents or who had no parents were not excluded as this could have increased the number missing values for participants of relatively lower economic levels.
Statistical analysis
Differences in the general characteristics according to sleep duration were calculated using linear regression analysis with complex sampling for age. The rate differences in relation to sex, region of residence, economic level, educational level of parents, stress level, food consumption and quality of sleep were compared using χ2 tests with Rao-Scott corrections.
Adjusted ORs (AORs) for sleep duration in relation to food consumption were calculated using multinomial logistic regression analysis with complex sampling for adjusted covariates (age, sex, obesity, region of residence, stress level, economic level and educational level of parents).
AORs for sleep quality in relation to food consumption were calculated using multinomial logistic regression analysis with complex sampling for adjusted covariates in the 7-hour and 8-hour groups.
Two-tailed analyses were conducted. P values lower than 0.05 were considered to indicate significance, and 95% CIs were calculated. The weighted values recommended by the KYRBWS were applied, and all results are presented as weighted values. The results were analysed using SPSS V.21.0.
Results
Analysis of the general characteristics of the study participants shows that an older age, being female, reporting being healthy, living in a large city, feeling severe or moderate stress, being at a lower economic level and having higher parental educational levels were associated with shorter sleep durations (all p values <0.001, table 1).
Table 1.
General characteristics of participants according to sleep duration
| Factors | Total | Sleep duration | P values | ||||
| <6 hours | 6 hours | 7 hours | 8 hours | 9+ hours | |||
| Number | |||||||
| n | 118 462 | 27 409 | 29 773 | 30 254 | 20 743 | 10 283 | |
| % | 100 | 23.1 | 25.1 | 25.5 | 17.5 | 8.7 | |
| Mean age (year, SD) | 15.0 (1.7) | 16.1 (1.5) | 15.5 (1.6) | 14.7 (1.6) | 13.9 (1.5) | 14.0 (1.6) | <0.001* |
| Sex (%) | <0.001† | ||||||
| Male | 50.2 | 41.8 | 47.7 | 52.3 | 57.1 | 59.5 | |
| Female | 49.8 | 58.2 | 52.3 | 47.7 | 42.9 | 40.5 | |
| Obesity (%) | <0.001† | ||||||
| Underweight | 6.1 | 5.9 | 6.2 | 6.0 | 6.2 | 6.9 | |
| Healthy | 78.8 | 80.3 | 79.5 | 78.1 | 77.8 | 76.5 | |
| Overweight | 11.3 | 10.8 | 10.8 | 11.8 | 11.8 | 11.8 | |
| Obese | 3.8 | 3.0 | 3.5 | 4.1 | 4.2 | 4.8 | |
| Region (%) | <0.001† | ||||||
| Large city | 44.7 | 49.4 | 46.6 | 43.3 | 40.6 | 39.0 | |
| Small city | 47.3 | 44.5 | 46.4 | 48.1 | 49.8 | 50.1 | |
| Rural area | 8.0 | 6.1 | 7.1 | 8.6 | 9.6 | 10.9 | |
| Stress (%) | <0.001† | ||||||
| Severe | 8.9 | 13.7 | 9.3 | 7.1 | 5.7 | 7.1 | |
| Moderate | 27.3 | 34.4 | 29.1 | 25.0 | 21.4 | 21.7 | |
| Mild | 43.8 | 39.9 | 45.1 | 45.8 | 44.8 | 42.8 | |
| A little | 16.6 | 10.1 | 14.3 | 18.8 | 23.0 | 21.9 | |
| No | 3.3 | 1.9 | 2.3 | 3.3 | 5.2 | 6.6 | |
| Economic level (%) | <0.001† | ||||||
| Highest | 8.1 | 7.3 | 6.9 | 7.9 | 9.5 | 11.1 | |
| Middle high | 26.5 | 26.7 | 25.5 | 25.7 | 28.1 | 27.7 | |
| Middle | 48.3 | 46.9 | 48.9 | 49.5 | 48.3 | 46.3 | |
| Middle low | 14.0 | 15.2 | 15.2 | 13.9 | 11.8 | 11.9 | |
| Lowest | 3.2 | 3.9 | 3.5 | 3.0 | 2.3 | 3.0 | |
| Educational level, father (%) | <0.001† | ||||||
| Unknown | 19.7 | 12.8 | 16.0 | 21.9 | 26.6 | 28.5 | |
| Middle school | 2.7 | 2.6 | 2.8 | 2.8 | 2.4 | 2.6 | |
| High school | 29.2 | 28.8 | 30.5 | 30.3 | 27.5 | 26.9 | |
| College or over | 48.4 | 55.8 | 50.8 | 45.0 | 43.6 | 42.0 | |
| Educational level, mother (%) | <0.001† | ||||||
| Unknown | 18.9 | 12.0 | 15.2 | 21.0 | 25.8 | 28.1 | |
| Middle school | 2.3 | 2.3 | 2.5 | 2.3 | 2.0 | 2.2 | |
| High school | 37.1 | 39.1 | 39.3 | 37.1 | 33.7 | 31.8 | |
| College or over | 41.7 | 46.7 | 43.0 | 39.6 | 38.5 | 37.9 | |
*Linear regression analysis with complex sampling. Significance at p<0.05.
†χ2 test with Rao-Scott correction. Significance at p<0.05.
Higher frequencies of instant noodle, fruits, vegetables and milk intake were associated with longer sleep durations, while higher frequencies of soda, soft drinks, fast food, and confectionaries intake were associated with shorter sleep durations (all p values <0.001, table 2).
Table 2.
Food consumption of participants according to sleep duration
| Factors | Sleep duration | P values | |||||
| Total | <6 hours | 6 hours | 7 hours | 8 hours | 9+ hours | ||
| Fruits (%) | <0.001* | ||||||
| ≥5 times a week | 33.4 | 33.4 | 31.9 | 32.5 | 35.6 | 35.8 | |
| 3–4 times a week | 28.9 | 28.2 | 29.0 | 29.2 | 29.4 | 28.0 | |
| 1–2 times a week | 29.5 | 30.1 | 30.8 | 29.9 | 27.0 | 27.9 | |
| 0 times a week | 8.3 | 8.3 | 8.3 | 8.4 | 8.0 | 8.7 | |
| Soda (%) | <0.001* | ||||||
| ≥5 times a week | 8.0 | 8.3 | 8.1 | 8.0 | 7.7 | 8.0 | |
| 3–4 times a week | 18.2 | 17.2 | 18.8 | 18.8 | 18.2 | 17.4 | |
| 1–2 times a week | 48.9 | 48.0 | 49.0 | 49.8 | 49.0 | 48.0 | |
| 0 times a week | 24.9 | 26.5 | 24.2 | 23.4 | 25.1 | 26.6 | |
| Soft drinks (%) | <0.001* | ||||||
| ≥5 times a week | 13.9 | 16.3 | 14.5 | 13.1 | 12.0 | 11.6 | |
| 3–4 times a week | 25.9 | 26.7 | 26.5 | 26.0 | 24.7 | 24.0 | |
| 1–2 times a week | 44.1 | 42.2 | 43.9 | 44.8 | 45.6 | 44.6 | |
| 0 times a week | 16.1 | 14.7 | 15.0 | 16.1 | 17.7 | 19.8 | |
| Fast food (%) | <0.001* | ||||||
| ≥5 times a week | 2.5 | 2.8 | 2.6 | 2.2 | 2.2 | 2.7 | |
| 3–4 times a week | 11.9 | 12.6 | 12.8 | 11.7 | 10.6 | 10.7 | |
| 1–2 times a week | 59.8 | 60.0 | 60.7 | 60.5 | 58.8 | 56.2 | |
| 0 times a week | 25.8 | 24.6 | 23.8 | 25.5 | 28.3 | 30.3 | |
| Instant noodle (%) | <0.001* | ||||||
| ≥5 times a week | 4.6 | 4.4 | 4.3 | 4.8 | 4.8 | 5.4 | |
| 3–4 times a week | 17.6 | 15.0 | 16.9 | 18.6 | 19.7 | 18.6 | |
| 1–2 times a week | 51.6 | 49.8 | 51.9 | 52.4 | 52.6 | 51.3 | |
| 0 times a week | 26.2 | 30.8 | 26.9 | 24.2 | 22.9 | 24.6 | |
| Confectionaries (%) | <0.001* | ||||||
| ≥5 times a week | 10.7 | 12.2 | 11.1 | 9.9 | 9.7 | 9.7 | |
| 3–4 times a week | 26.4 | 27.1 | 26.9 | 26.4 | 25.5 | 24.4 | |
| 1–2 times a week | 45.4 | 44.3 | 45.6 | 45.9 | 45.9 | 45.6 | |
| 0 times a week | 17.6 | 16.5 | 16.5 | 17.8 | 18.9 | 20.3 | |
| Vegetables (%) | <0.001* | ||||||
| ≥5 times a week | 56.6 | 57.3 | 55.4 | 55.4 | 57.8 | 58.7 | |
| 3–4 times a week | 24.1 | 23.8 | 24.5 | 25.1 | 23.2 | 22.6 | |
| 1–2 times a week | 15.7 | 15.0 | 16.4 | 16.1 | 15.6 | 14.9 | |
| 0 times a week | 3.6 | 4.0 | 3.7 | 3.4 | 3.4 | 3.8 | |
| Milk (%) | <0.001* | ||||||
| ≥5 times a week | 41.9 | 36.7 | 38.4 | 42.9 | 48.4 | 50.4 | |
| 3–4 times a week | 20.0 | 20.3 | 20.4 | 20.2 | 19.6 | 18.2 | |
| 1–2 times a week | 22.4 | 24.3 | 24.0 | 22.2 | 19.4 | 18.6 | |
| 0 times a week | 15.7 | 18.7 | 17.3 | 14.8 | 12.5 | 12.8 | |
*χ2 test with Rao-Scott correction. Significance at p<0.05.
Short sleep durations (<6 hours) were associated with a higher intake of soft drinks (AOR (95% CI) for ≥5 times a week: 1.73 (1.57 to 1.91); p<0.001) and with a higher intake of confectionaries (AOR (95% CI) for ≥5 times a week: 1.32 (1.20 to 1.46); p<0.001). Soda and fast food intake showed an increasing trend in the group getting <6 hours of sleep. However, it was not definite. Fruits, instant noodle, vegetables and milk intake did not show an evident association with getting <6 hours of sleep per night despite the significant association with sleep duration overall (table 3). Unadjusted model was also analysed (online supplementary S2 table).
Table 3.
Adjusted ORs of sleep duration for food consumption using multiple logistic regression analysis with complex sampling (reference of food frequency=0 times a week)
| Factors | AOR (95% CI) of sleep duration | P values | ||||
| <6 hours | 6 hours | 7 hours | 8 hours | 9+ hours | ||
| Fruits (%) | <0.001* | |||||
| ≥5 times a week | 1.07 (0.97 to 1.18) | 0.97 (0.89 to 1.06) | 0.95 (0.87 to 1.04) | 1.03 (0.94 to 1.12) | 1 | |
| 3–4 times a week | 1.04 (0.94 to 1.15) | 1.05 (0.96 to 1.16) | 1.05 (0.95 to 1.15) | 1.11 (1.00 to 1.22) | 1 | |
| 1–2 times a week | 0.98 (0.89 to 1.08) | 1.02 (0.92 to 1.12) | 1.03 (0.94 to 1.13) | 1.02 (0.92 to 1.12) | 1 | |
| Soda (%) | <0.001* | |||||
| ≥5 times a week | 1.27 (1.14 to 1.41) | 1.29 (1.17 to 1.42) | 1.27 (1.16 to 1.40) | 1.08 (0.97 to 1.19) | 1 | |
| 3–4 times a week | 1.08 (1.00 to 1.17) | 1.25 (1.17 to 1.34) | 1.29 (1.21 to 1.38) | 1.13 (1.05 to 1.22) | 1 | |
| 1–2 times a week | 1.00 (0.94 to 1.07) | 1.12 (1.06 to 1.18) | 1.20 (1.14 to 1.27) | 1.09 (1.03 to 1.16) | 1 | |
| Soft drinks (%) | <0.001* | |||||
| ≥5 times a week | 1.73 (1.57 to 1.91) | 1.57 (1.44 to 1.71) | 1.38 (1.26 to 1.50) | 1.16 (1.06 to 1.28) | 1 | |
| 3–4 times a week | 1.36 (1.25 to 1.47) | 1.36 (1.37 to 1.46) | 1.28 (1.19 to 1.38) | 1.15 (1.07 to 1.24) | 1 | |
| 1– 2 times a week | 1.16 (1.09 to 1.25) | 1.22 (1.15 to 1.30) | 1.18 (1.11 to 1.26) | 1.14 (1.07 to 1.22) | 1 | |
| Fast food (%) | <0.001* | |||||
| ≥5 times a week | 1.12 (0.95 to 1.32) | 1.15 (0.99 to 1.34) | 0.95 (0.82 to 1.11) | 0.86 (0.74 to 1.00) | 1 | |
| 3–4 times a week | 1.18 (1.08 to 1.29) | 1.31 (1.20 to 1.28) | 1.22 (1.12 to 1.32) | 1.07 (0.99 to 1.17) | 1 | |
| 1–2 times a week | 1.12 (1.05 to 1.19) | 1.22 (1.15 to 1.28) | 1.22 (1.15 to 1.28) | 1.13 (1.07 to 1.19) | 1 | |
| Instant noodle (%) | <0.001* | |||||
| ≥5 times a week | 1.09 (0.96 to 1.24) | 1.03 (0.91 to 1.17) | 1.07 (0.95 to 1.20) | 0.98 (0.87 to 1.11) | 1 | |
| 3–4 times a week | 0.93 (0.86 to 1.01) | 1.06 (0.98 to 1.14) | 1.15 (1.07 to 1.23) | 1.17 (1.08 to 1.26) | 1 | |
| 1– 2 times a week | 0.92 (0.86 to 0.98) | 1.04 (0.98 to 1.10) | 1.09 (1.03 to 1.16) | 1.11 (1.04 to 1.18) | 1 | |
| Confectionaries (%) | <0.001* | |||||
| ≥5 times a week | 1.32 (1.20 to 1.46) | 1.28 (1.17 to 1.41) | 1.10 (1.00 to 1.20) | 1.06 (0.97 to 1.17) | 1 | |
| 3–4 times a week | 1.20 (1.11 to 1.29) | 1.22 (1.13 to 1.31) | 1.16 (1.08 to 1.24) | 1.10 (1.02 to 1.18) | 1 | |
| 1–2 times a week | 1.09 (1.12 to 1.17) | 1.15 (1.07 to 1.23) | 1.11 (1.04 to 1.18) | 1.08 (1.01 to 1.16) | 1 | |
| Vegetables (%) | <0.001* | |||||
| ≥5 times a week | 0.96 (0.85 to 1.10) | 0.95 (0.83 to 1.07) | 1.04 (0.92 to 1.17) | 1.07 (0.94 to 1.22) | 1 | |
| 3–4 times a week | 0.92 (0.80 to 1.05) | 0.98 (0.86 to 1.12) | 1.15 (1.02 to 1.30) | 1.10 (0.96 to 1.25) | 1 | |
| 1–2 times a week | 0.91 (0.79 to 1.05) | 1.02 (0.90 to 1.17) | 1.17 (1.03 to 1.33) | 1.15 (1.01 to 1.33) | 1 | |
| Milk (%) | <0.001* | |||||
| ≥5 times a week | 0.99 (0.91 to 1.07) | 0.91 (0.85 to 0.98) | 0.92 (0.85 to 0.99) | 0.97 (0.89 to 1.04) | 1 | |
| 3–4 times a week | 1.06 (0.97 to 1.15) | 1.04 (0.96 to 1.13) | 1.09 (1.00 to 1.18) | 1.09 (1.00 to 1.19) | 1 | |
| 1–2 times a week | 1.01 (0.93 to 1.09) | 1.05 (0.97 to 1.14) | 1.06 (0.98 to 1.14) | 1.03 (0.95 to 1.12) | 1 | |
*Significance at p<0.05.
bmjopen-2018-022848supp002.pdf (234.6KB, pdf)
Sleep quality was also associated with the frequency of food intake. Poor quality of sleep was associated with a lower intake of fruits, vegetables and milk (AOR (95% CI) for ≥5 times a week for fruits: 0.71 (0.65 to 0.77); vegetables: 0.66 (0.58 to 0.75); and milk: 0.80 (0.74 to 0.86); each p<0.001). Poor sleep quality was also related with a higher intake of soda, soft drinks, fast food, instant noodle and confectionaries (AOR (95% CI) for ≥5 times a week for soda: 1.55 (1.40 to 1.70); soft drinks: 1.58 (1.43 to 1.73); fast food: 1.97 (1.65 to 2.35); instant noodle: 1.55 (1.37 to 1.76); and confectionaries: 1.30 (1.18 to 1.43); each p<0.001, table 4).
Table 4.
Adjusted ORs of quality of sleep for food consumption using multiple logistic regression analysis with complex sampling (reference of food frequency=0 times a week) in 7-hour and 8-hour groups
| Factors | Quality of sleep | P values | ||
| Good | Moderate | Poor | ||
| Fruits (%) | <0.001** | |||
| ≥5 times a week | 1 | 0.81 (0.74 to 0.89) | 0.71 (0.65 to 0.77) | |
| 3–4 times a week | 1 | 0.93 (0.85 to 1.01) | 0.79 (0.72 to 0.87) | |
| 1–2 times a week | 1 | 1.00 (0.92 to 1.09) | 0.90 (0.82 to 0.99) | |
| Soda (%) | <0.001** | |||
| ≥5 times a week | 1 | 1.27 (1.16 to 1.40) | 1.55 (1.40 to 1.70) | |
| 3–4 times a week | 1 | 1.25 (1.16 to 1.33) | 1.35 (1.25 to 1.45) | |
| 1–2 times a week | 1 | 1.14 (1.08 to 1.20) | 1.15 (1.08 to 1.22) | |
| Soft drinks (%) | <0.001** | |||
| ≥5 times a week | 1 | 1.24 (1.15 to 1.35) | 1.58 (1.43 to 1.73) | |
| 3–4 times a week | 1 | 1.21 (1.13 to 1.29) | 1.36 (1.26 to 1.46) | |
| 1–2 times a week | 1 | 1.09 (1.03 to 1.16) | 1.10 (1.03 to 1.18) | |
| Fast food (%) | <0.001** | |||
| ≥5 times a week | 1 | 1.26 (1.07 to 1.49) | 1.97 (1.65 to 2.35) | |
| 3–4 times a week | 1 | 1.28 (1.19 to 1.38) | 1.49 (1.37 to 1.62) | |
| 1–2 times a week | 1 | 1.11 (1.06 to 1.17) | 1.18 (1.11 to 1.25) | |
| Instant noodle (%) | <0.001** | |||
| ≥5 times a week | 1 | 1.29 (1.14 to 1.45) | 1.55 (1.37 to 1.76) | |
| 3–4 times a week | 1 | 1.27 (1.19 to 1.36) | 1.31 (1.22 to 1.42) | |
| 1–2 times a week | 1 | 1.14 (1.09 to 1.20) | 1.11 (1.05 to 1.18) | |
| Confectionaries (%) | <0.001** | |||
| ≥5 times a week | 1 | 1.13 (1.03 to 1.23) | 1.30 (1.18 to 1.43) | |
| 3–4 times a week | 1 | 1.12 (1.04 to 1.19) | 1.08 (1.01 to 1.17) | |
| 1–2 times a week | 1 | 1.05 (0.99 to 1.12) | 1.00 (0.93 to 1.07) | |
| Vegetables (%) | <0.001** | |||
| ≥5 times a week | 1 | 0.97 (0.86 to 1.10) | 0.66 (0.58 to 0.75) | |
| 3–4 times a week | 1 | 1.14 (1.00 to 1.30) | 0.78 (0.68 to 0.89) | |
| 1–2 times a week | 1 | 1.30 (1.14 to 1.49) | 0.98 (0.85 to 1.12) | |
| Milk (%) | <0.001** | |||
| ≥5 times a week | 1 | 0.89 (0.83 to 0.95) | 0.80 (0.74 to 0.86) | |
| 3–4 times a week | 1 | 1.01 (0.941.09) | 0.86 (0.79 to 0.93) | |
| 1–2 times a week | 1 | 0.99 (0.92 to 1.06) | 0.91 (0.84 to 0.99) | |
*Significance at p<0.05.
Discussion
We found that shorter sleep durations were associated with higher frequencies of consuming soft drinks and confectionaries than longer sleep durations. Additionally, poor sleep quality, with 7–8 hours of sleep per night, was associated with a lower frequency of fruits, vegetables and milk intake, and a higher frequency of soda, soft drinks, fast food, instant noodle and confectionaries intake. These results are consistent with the results from previous studies in regard to the association between sleep duration and food consumption.13–15 19 Furthermore, we demonstrated an association between sleep quality and the intake of various foods.
Along with these outcomes, sleep duration in association with sleep quality might affect one’s appetite and even be related to health problems such as obesity21 and diabetes.22 A short sleep duration or poor sleep quality is associated with appetite-related hormonal changes such as lower leptin and higher ghrelin levels in previous studies. These results were also associated with greater energy intake and a higher BMI.16 17 Baron et al21 reported that people who fall asleep later sleep less and consume more calories than people who fall asleep earlier. Moreover, consuming calories after 20:00 was associated with a higher BMI. Rudnicka et al22 reported that shorter sleep durations in children were associated with a higher prevalence of risk factors for type 2 diabetes, such as increases in the fat mass index, insulin resistance and fasting glucose level. Meanwhile, Doo et al23 reported that participants with shorter sleep durations and a higher consumption of dietary antioxidant vitamins had a lower risk of obesity than those with a lower consumption of dietary antioxidant vitamins. In summary, a short sleep duration in association with poor sleep quality could affect dietary habits and appetite, which could result in health problems. Nevertheless, people who sleep for shorter durations can reduce the risks of health problems by consuming foods rich in micronutrients such as vitamins.
Although nutrient profiles were not available in our study, sugar-sweetened beverages, such as soda and soft drinks, confectionaries, fast food and instant noodle have higher energy levels but less micronutrients than fruits, vegetables and milk. Sugar-sweetened beverages contain mainly liquid calories provided by sugars and have very few of other nutrients. A potential biological mechanism for sugar-sweetened beverages leading to obesity is that liquid calories may result in decreased satiety, leading to the consumption of more sugar-sweetened beverages with subsequent weight gain.24
Fast food, confectionaries and instant noodle contain high energy densities, with calories derived from carbohydrates and fats and with minimal amounts of other nutrients. Nevertheless, humans have a weak innate ability to recognise energy density, so humans fail to downregulate the consumption of most of these foods accordingly.25 Obesity is one of the risk factors of type 2 diabetes, because it is related to an increase in insulin resistance.26 In fact, previous studies reported that sugar-sweetened beverage and fast food consumption were associated with changes in bodyweight and increased insulin resistance.24 27 Hence, consumption of these foods could be a potential mechanistic link between sleep duration in association with quality and health problems, including obesity and type 2 diabetes in adolescents.
However, food intake might affect sleep duration and sleep quality. Fruits, vegetables and milk are sources of vitamins and minerals. Grandner et al28 reported that sleep symptoms such as difficulty falling asleep, difficulty maintaining sleep, non-restorative sleep, and daytime sleepiness were associated with a lower intake of calcium, potassium, selenium, vitamin C, vitamin D, alpha-carotene and lycopene. Although mechanistic links between vitamin intake and sleep quality are unclear, previous studies have verified the relationship between sleep duration and vitamin intake.29 30 In addition, Grandner et al reported that sleep symptoms associated with poor sleep quality were associated with a higher intake of salt,28 and fast food and instant noodle intake are associated with salt intake. In accordance with the Korean food composition table, the sodium content of cooked hamburger is 498 mg/100 g and that of cheese pizza is 447 mg/100 g. Instant noodle seasoning contains 2225 mg of sodium in one portion (10.5 g).31 Excessive salt (and therefore sodium) intake leads to elevated blood pressure, whereas calcium and potassium lower blood pressure.32 Fereidoun and Pouria reported that providing 0.05 g/kg of salt to participants resulted in poor sleep quality.33 According to a study by Javaheri et al34, poor sleep quality in adolescents was associated with prehypertension. The findings of previous studies and those of our study show that consuming foods with high levels of salt and low levels of other micronutrients might result in reduced sleep durations and poor sleep quality.
The limitations of our study are as follows. First, our study was based on data collected by the KYRBWS, and as secondary data, it has some limitations in providing specific information. For example, the dataset did not have information on nutrient contents or the quantity of food consumed to go along with intake frequency data. In addition, data on other confounding factors such as school examination periods or the timing of food intake across the 24 hours were not present. Second, because the data were collected based on a self-reported questionnaire including weight and height, the precision of the information may be low such as BMI have possibility of underestimation by self-reported questionnaire.35 Third, the validity of questionnaires of sleep duration, sleep quality and food intake frequencies is unclear. Hence, the responses on the questionnaire may not represent the usual sleep duration, sleep quality or food intake frequency of each participant. To collect usual sleep duration, sleep quality and food intake data, the validity and reliability of the questionnaire should be evaluated in a further study. Finally, because of the cross-sectional design, the causal relationship between sleep duration, sleep quality and food intake frequency is unclear. Longitudinal, randomised, controlled studies should be conducted to determine the causal relationship.
Nevertheless, our findings provide valuable information for the following reasons. First, our study was conducted on a representative population of Korean adolescents. Second, we considered numerous socioeconomic status variables as confounding factors to investigate the independent relationship between sleep status and food consumption. Third, we considered sleep duration and sleep quality in explaining sleep status. Finally, we investigated the intake frequency of various foods to show the relationship between sleep status and food consumption.
Conclusion
A short sleep duration was related to a higher frequency of soft drinks and confectionaries intake. Additionally, poor sleep quality with a normal sleep duration was related to a lower frequency of fruits, vegetables and milk intake, and a higher frequency of soda, soft drinks, fast food, instant noodle and confectionaries intake in adolescents. Hence, we demonstrate that short sleep durations and poor sleep quality might be associated with unhealthy food consumption, such as consuming more sugar-sweetened beverages, fast food, instant noodle and confectionaries, and fewer fruits, vegetables and milk. Further studies with a longitudinal, randomised, controlled design are needed to elucidate the specific causal relationship between sleep status and food consumption in adolescents.
Supplementary Material
Acknowledgments
We would like to thank the survey participants and examiners of the Division of Chronic Disease Surveillance in the Korea Centers for Disease Control & Prevention for participating in this survey and providing the data.
Footnotes
Contributors: CM wrote the manuscript. H-JK designed the study. I-SP performed the data processing. BP performed the data interpretation. J-HK analysed the data. SS, as co-corresponding author, gave statistical techniques and reviewed the manuscript. HGC, as corresponding author, conceptualised the study and wrote and reviewed the manuscript. HGC and SS are equally contributed in this study.
Funding: This research was supported by Hallym University Research Fund.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Centers for Disease Control and Prevention of Korea.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. National Sleep Foundation. Teens and Sleep. https://sleepfoundation.org/sleep-topics/teens-and-sleep (accessed 8/29 2017).
- 2. Keyes KM, Maslowsky J, Hamilton A, et al. . The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics 2015;135:460–8. 10.1542/peds.2014-2707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med 2010;11:735–42. 10.1016/j.sleep.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 4. Ming X, Koransky R, Kang V, et al. . Sleep insufficiency, sleep health problems and performance in high school students. Clin Med Insights Circ Respir Pulm Med 2011;5:CCRPM.S7955–9. 10.4137/CCRPM.S7955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meldrum RC, Restivo E. The behavioral and health consequences of sleep deprivation among U.S. high school students: relative deprivation matters. Prev Med 2014;63:24–8. 10.1016/j.ypmed.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 6. Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics 2007;119(Suppl 1):S29–37. 10.1542/peds.2006-2089F [DOI] [PubMed] [Google Scholar]
- 7. Wolfson AR, Carskadon MA. Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev 2003;7:491–506. 10.1016/S1087-0792(03)90003-7 [DOI] [PubMed] [Google Scholar]
- 8. Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 2015;16:137–49. 10.1111/obr.12245 [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization. Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed 3/7 2018).
- 10. World Health Organization. What are the causes?: Reasons for children and adolescents to become obese. http://www.who.int/dietphysicalactivity/childhood_why/en/ (accessed 8/31 2017).
- 11. Bucher Della Torre S, Keller A, Laure Depeyre J, et al. . Sugar-Sweetened Beverages and Obesity Risk in Children and Adolescents: A Systematic Analysis on How Methodological Quality May Influence Conclusions. J Acad Nutr Diet 2016;116:638–59. 10.1016/j.jand.2015.05.020 [DOI] [PubMed] [Google Scholar]
- 12. Schwingshackl L, Hobl LP, Hoffmann G. Effects of low glycaemic index/low glycaemic load vs. high glycaemic index/ high glycaemic load diets on overweight/obesity and associated risk factors in children and adolescents: a systematic review and meta-analysis. Nutr J 2015;14:87 10.1186/s12937-015-0077-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ferranti R, Marventano S, Castellano S, et al. . Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci 2016;9:117–22. 10.1016/j.slsci.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gong QH, Li H, Zhang XH, et al. . Associations between sleep duration and physical activity and dietary behaviors in Chinese adolescents: results from the Youth Behavioral Risk Factor Surveys of 2015. Sleep Med 2017;37:168–73. 10.1016/j.sleep.2017.06.024 [DOI] [PubMed] [Google Scholar]
- 15. Kruger AK, Reither EN, Peppard PE, et al. . Do sleep-deprived adolescents make less-healthy food choices? Br J Nutr 2014;111:1898–904. 10.1017/S0007114514000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gonnissen HK, Hursel R, Rutters F, et al. . Effects of sleep fragmentation on appetite and related hormone concentrations over 24 h in healthy men. Br J Nutr 2013;109:748–56. 10.1017/S0007114512001894 [DOI] [PubMed] [Google Scholar]
- 17. Taheri S, Lin L, Austin D, et al. . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004;1:e62 10.1371/journal.pmed.0010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Korea National Health and Nutrition Examination Survey. Korea Health Statistics 2016: Korea National Health and Nutrition Examination Survey (KNHANES Ⅶ-1), 2018. [Google Scholar]
- 19. Lee J. Sleep duration’s association with diet, physical activity, mental status, and weight among Korean high school students. Asia Pac J Clin Nutr 2017;26:906–13. [DOI] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention. About BMI for Children and Teens. http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (accessed 11/14 2014).
- 21. Baron KG, Reid KJ, Kern AS, et al. . Role of sleep timing in caloric intake and BMI. Obesity 2011;19:1374–81. 10.1038/oby.2011.100 [DOI] [PubMed] [Google Scholar]
- 22. Rudnicka AR, Nightingale CM, Donin AS, et al. . Sleep Duration and Risk of Type 2 Diabetes. Pediatrics 2017. 140:e20170338 10.1542/peds.2017-0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Doo M, Kim Y. The Consumption of Dietary Antioxidant Vitamins Modifies the Risk of Obesity among Korean Men with Short Sleep Duration. Nutrients 2017;9 10.3390/nu9070780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav 2010;100:47–54. 10.1016/j.physbeh.2010.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Prentice AM, Jebb SA. Fast foods, energy density and obesity: a possible mechanistic link. Obes Rev 2003;4:187–94. 10.1046/j.1467-789X.2003.00117.x [DOI] [PubMed] [Google Scholar]
- 26. Edelstein SL, Knowler WC, Bain RP, et al. . Predictors of progression from impaired glucose tolerance to NIDDM: an analysis of six prospective studies. Diabetes 1997;46:701–10. 10.2337/diab.46.4.701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pereira MA, Kartashov AI, Ebbeling CB, et al. . Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 2005;365:36–42. 10.1016/S0140-6736(04)17663-0 [DOI] [PubMed] [Google Scholar]
- 28. Grandner MA, Jackson N, Gerstner JR, et al. . Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res 2014;23:22–34. 10.1111/jsr.12084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Majid MS, Ahmad HS, Bizhan H, et al. . The effect of vitamin D supplement on the score and quality of sleep in 20-50 year-old people with sleep disorders compared with control group. Nutr Neurosci 2017:1–9 (published Online First: 2017/05/06). 10.1080/1028415X.2017.1317395 [DOI] [PubMed] [Google Scholar]
- 30. Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res 2012;32:309–19. 10.1016/j.nutres.2012.03.009 [DOI] [PubMed] [Google Scholar]
- 31. Department of Agrofood Resources, NAAS, RDA, et al. Standard Food Composition Table. 8th revision, 2013. [Google Scholar]
- 32. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis 2006;49:59–75. 10.1016/j.pcad.2006.07.001 [DOI] [PubMed] [Google Scholar]
- 33. Fereidoun H, Pouria H. Effect of excessive salt consumption on night’s sleep. Pak J physiol 2014;10(3-4):6–9. [Google Scholar]
- 34. Javaheri S, Storfer-Isser A, Rosen CL, et al. . Sleep quality and elevated blood pressure in adolescents. Circulation 2008;118:1034–40. 10.1161/CIRCULATIONAHA.108.766410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bae J, Joung H, Kim JY, et al. . Validity of self-reported height, weight, and body mass index of the Korea Youth Risk Behavior Web-based Survey questionnaire. J Prev Med Public Health 2010;43:396–402. 10.3961/jpmph.2010.43.5.396 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022848supp001.pdf (191.1KB, pdf)
bmjopen-2018-022848supp002.pdf (234.6KB, pdf)