Abstract
Background
The number of falls in hospital ranges from 3.8 to 8.6 falls per 1000 bed days. 1 Around 30% of falls as inpatients are injurious, and 4%–6% can result in serious and life-threatening injury. 2 3 This results in significant health burdens and economic burdens due to increased hospital stays following a fall. Junior doctors are usually the first point of contact for managing patients who fall in hospital. It is therefore important they understand the preventative measures and postfalls management.
Aim
To assess the retention of knowledge regarding falls management in foundation year 1 (FY1) doctors before and after a short educational intervention.
Methods
A 3-stage quality improvement project was conducted at a West Midlands teaching hospital to highlight issues regarding falls management. A questionnaire assessing areas of knowledge regarding assessment and management of falls was delivered to 31 F1s. This was followed by a short presentation regarding falls management. The change in knowledge was assessed at 6 and 16 weeks postintervention. The questionnaire results were analysed using unpaired t-tests on STATA (V.14.2).
Results
The mean score for knowledge regarding falls management in the preintervention, early postintervention and late postintervention were 73.7%, 85.2% and 76.4%, respectively. Although there was an improvement in the knowledge at 6 weeks’ postintervention, this returned to almost baseline at 16 weeks. The improvement in knowledge did not translate to clinical practice of falls management during this period.
Conclusion
Although educational interventions improve knowledge, the intervention failed to sustain over period of time or translate in clinical practice. Further work is needed to identify alternative methods to improve sustainability of the knowledge of falls and bring in the change in clinical practice.
Keywords: quality improvement, medical education, team training
Problem
Falls are the most frequent adverse event reported in hospital, with more than 600 falls per day in England and Wales.4 Thirty per cent of these falls are injurious, with 4%–6% leading to serious and life-threatening injuries.2 3 The aetiology of inpatient falls are multifactorial5 often including age-related changes, acute and long-term medical conditions, medication and the hospital environment. The frequency of falls increases with age and frailty, with global estimates that 28%–35% of people aged over 65 years old fall each year increasing to 32%–42% for those over 70 years old.6 With an ageing population, the burden of falls in older people must be monitored as 20%–30% result in moderate to severe injuries such as lacerations, brain injuries and one study identified falls responsible for 87% of all fractures admitted to an Emergency Department in over-65s.5 7 8
The consequences of falls are significant for hospital trusts. A recent UK economic evaluation identified that inpatient falls alone cost the National Health Service (NHS) approximately £680 million pounds per year.9 Another study identified that falls were associated with an increased length of stay by 8 days contributing largely to this cost.10 Considering the health and economic burdens relating to falls, there is a significant need to reduce the number of injurious falls.
Background
The WHO defines a fall as ‘an event which results in a person coming to rest inadvertently on the ground or floor or other lower level’.11 In clinical practice, falls are often incorrectly subdivided by mechanical (environment-related) and non-mechanical (other causes) in nature.12
Targeted intervention programmes that are focused on reducing falls risk factors and are managed through documentation on care plans have been shown to reduce the numbers of falls.13 Some programmes also targeted staff education to further decrease the rate of inpatient falls.14 The majority of interventions have concentrated on patient education and physical reduction of risk factors. However, a less well-researched area is staff education around falls. A recent quality improvement project (QIP) which involved delivering 45 min training sessions to nursing staff and registrars by inpatient falls experts (geriatricians, senior nurses and ward managers) led to a significant reduction in the incidence of falls in the inpatient population.15 To our knowledge, no similar intervention had been trialled in doctors in training to assess the impact on knowledge of falls and risk factors.
This project was set in a large tertiary teaching hospital in the West Midlands which treats over 1 million patients per year.16 All patients admitted to the hospital undergo a falls assessment which is repeated following a change of ward or change in clinical condition identified through the electronic patient monitoring system. A specialist multidisciplinary falls team reviews patients who have fallen more than once to try to prevent recurrence. They also provide training and education to staff and junior doctors at the Trust. As a Trust policy, the Trust assesses performance by measuring the percentage of falls leading to harm which recently reduced from 18.1% in 2015/16% to 17.4% in 2016/2017.16 The trust goal is to set a target reduction to 16.5% by the end of 2017/2018 when a new policy named ‘reducing harm from falls’ is introduced.
Due to these initiatives and drive by the Trust, the authors felt this was an appropriate time to assess the current understanding of falls management among junior doctors. The role of the junior doctor in this setting is to work as part of the multidisciplinary team aiming to reduce the harm following a fall and look at methods to prevent the recurrence of falls. In this Trust, junior doctors assess patients postfall to identify any harm that had come to the patient, identify factors that lead to fall and implement measures to prevent recurrence.
Postgraduate medical educational interventions are common methods to introduce new topics or readdress difficult topics for practicing doctors. Review evidence has previously suggested that standalone sessions do show improvements in knowledge of junior doctors17 but not necessarily skills, attitudes or behaviours. Educational literature suggests a multitude of methods which can be used in a postgraduate medical setting for standalone interventions. These range from passive methods such as lectures or audio-visual tutorials to interactive methods such as problem-based learning or simulation sessions. These methods have been shown to improve knowledge retention in a variety postgraduate medical settings.18–20 As well improving knowledge retention, interactive methods such as problem-based learning have also demonstrated social benefits for the cohort undertaking this type of learning.21 However, often in postgraduate settings it can be challenging to arrange frequent interactive sessions due to the logistical challenges in their preparation and delivery. Therefore, often large group methods such as lectures are employed to assist the transference of knowledge in a medical setting.22 However, recent work has doubted the efficacy of traditional lectures as a method of teaching that provides benefit to students.23 In order to improve retention and knowledge, lectures can become more active forms of learning which stimulate individuals. One of the common ways to do this is to drastically reduce the lecture length to allow opportunity for reflection or activity following.24 Previous work we have conducted has demonstrated that a short lecture in the postgraduate setting provided a beneficial change in knowledge for junior doctors25 26 demonstrating their use when applied correctly.
Measurement
We used a questionnaire-based assessment to measure the change in the knowledge following short educational intervention regarding falls management in a longitudinal format. This is a validated and practically easy way of measuring knowledge.27 The questionnaire was adapted from the Singapore Ministry of Health Nursing Clinical Practice Guidelines on Prevention of Falls in Hospitals and Long-Term Care Institutions,28 with further modification to local guidelines and practice following consultation with the Trust’s falls team and multidisciplinary team described below (see online supplementary file for the questionnaire). The questionnaire was piloted on a sample of 10 final year medical students. The pilot audience were administered the questionnaire using the same method the foundation year 1 (FY1) doctor audience would be in the main study. The aim of this pilot was to identify any ambiguous or misleading questions and eliminate any unnecessary questions as well as ensure the questionnaire was of reasonable length. The questionnaire was then modified based on the input before being administered to the target audience in the study.
bmjoq-2017-000222supp001.pdf (76.8KB, pdf)
The questionnaire was delivered preintervention, 6 weeks postintervention and 16 weeks postintervention to measure the change and retention of knowledge following intervention. We also measured the clinical practice of postfalls management preintervention and postintervention by making note of adherence to current clinical guidelines through retrospective analysis of case notes.
There were no other interventions planned regarding falls management for the target group during this period and hence assumed any change was a result of our intervention.
Design
This prospective study was done at a large teaching hospital in the West Midlands from December 2016 to April 2017. All FY1s working at the trust and regularly attending weekly teaching during this time period were included in the study. A multidisciplinary team consisting of a consultant geriatrician, specialist registrar in general internal medicine, FY1, three falls specialist nurses and two medical students with special interest in falls was set up for this QIP.
The intervention consisted of a short informative presentation using PowerPoint lasting 5 min delivered to FY1s during their weekly teaching sessions. This presentation highlighted the prevalence, assessment and management of falls as per local Trust guidelines. FY1s have a protected weekly teaching session with fewer on-call commitments compared with the rest of the junior doctors. Also, from our observation, we noted that FY1s were the most common first point of contact to assess patients after a fall in this Trust. Hence, we assumed that targeting this group would maximise the likelihood of improvement in clinical practice.
Strategy
On obtaining necessary permission from the postgraduate education department, we delivered the questionnaire to the FY1s as part of their weekly teaching session. They were given 10 min to complete the questionnaire. This was followed by a short Q&A session to answer any queries regarding falls management. The questionnaire was repeated to the junior doctors at 6 and 16 weeks postintervention.
The change in clinical practice for postfalls assessment was measured 2 weeks preintervention and 2 weeks postintervention. Data were collected using MS Excel and was based on the Trust’s postfalls assessment proforma from current clinical guidelines.
Results
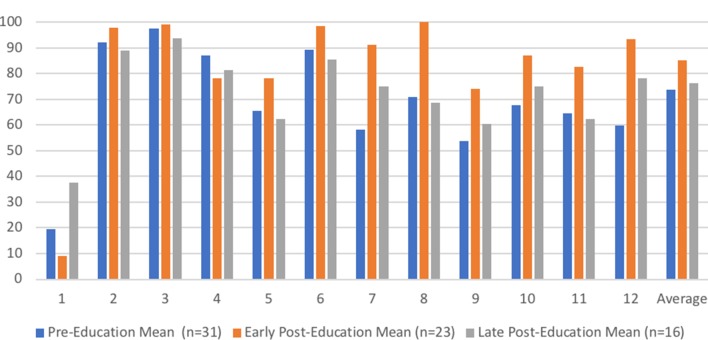
Figure 1 illustrates the percentage of correct answers to the 12 questions asked in the preintervention, early postintervention and late postintervention phases. Table 1 demonstrates the percentages of correct answers in the three phases with also tests of significance comparing the preintervention and early scores as well as the preintervention and late scores, calculated as unpaired t-tests on STATA (V.14.2). Statistical significance was set at a value of p<0.05. The intention of this type of statistical analysis was to identify if there were immediate benefits following the teaching and significant sustained benefits from this type of intervention. We saw a significantly increased overall knowledge from 73.7% to 85.2% (p=0.0016) at 6 weeks postintervention. However, this returned to near baseline in the late postintervention phase. The data from the assessment of clinical practice (2 weeks preintervention and 2 weeks postintervention) did not demonstrate any significant difference (p=0.3471) in clinical practice (63.0% (95% CI 48.3 to 77.7) vs 53.6% (95% CI 34.2 to 70.9)) after calculation through an unpaired t-test.
Figure 1.
Percentage of correct responses to the questionnaire.
Table 1.
Percentage of correct responses to the questionnaire with comparison between preintervention vs early intervention and preintervention vs late intervention
| Question number | Pre-education Mean (95% CI) (n=31) | Early posteducation Mean (95% CI) (n=23) | Pre- vs early (p value) |
Late posteducation Mean (95% CI) (n=16) | Pre- vs Late (p value) |
| 1 | 19.4 (4.6 to 34.1) | 39.1 (17.6 to 60.7) | 0.1257 | 37.5 (10.9 to 64.1) | 0.2196 |
| 2 | 92.0 (84.7 to 99.2) | 97.8 (94.7 to 100.9) | 0.1344 | 89.1 (75.3 to 102.8) | 0.6994 |
| 3 | 97.6 (94.0 to 101.2) | 99.0 (96.7 to 101.2) | 0.5257 | 93.8 (83.4 to 104.1) | 0.4664 |
| 4 | 87.1 (66.5 to 107.7) | 78.3 (60.0 to 96.5) | 0.5122 | 81.3 (59.8 to 102.7) | 0.6840 |
| 5 | 65.6 (59.7 to 71.5) | 78.3 (71.3 to 85.3) | 0.0063 | 62.5 (53.6 to 71.4) | 0.5505 |
| 6 | 89.2 (80.7 to 97.8) | 98.6 (95.5 to 101.6) | 0.0431 | 85.4 (72.5 to 98.3) | 0.6074 |
| 7 | 58.1 (39.7 to 76.5) | 91.3 (78.8 to 103.8) | 0.0034 | 75.0 (51.2 to 98.8) | 0.2460 |
| 8 | 71.1 (54.0 to 87.9) | 100.0 (100.0 to 100.0) | 0.0015 | 68.8 (43.2 to 94.3) | 0.8799 |
| 9 | 53.8 (42.1 to 65.4) | 74.0 (67.9 to 80.0) | 0.0030 | 60.4 (50.8 to 70.1) | 0.3647 |
| 10 | 67.7 (50.3 to 85.2) | 87.0 (72.1 to 101.8) | 0.0907 | 75.0 (51.2 to 98.8) | 0.6092 |
| 11 | 64.5 (46.7 to 82.4) | 82.6 (65.8 to 99.4) | 0.1343 | 62.5 (35.9 to 89.1) | 0.8957 |
| 12 | 59.7 (44.0 to 75.3) | 93.5 (86.8 to 100.2) | 0.0002 | 78.1 (61.4 to 94.9) | 0.1004 |
| Mean | 73.7 (67.1 to 80.4) | 85.2 (83.6 to 86.8) | 0.0016 | 76.4 (66.4 to 86.4) | 0.6412 |
Lessons and limitations
The key lesson from this project is the limited translation of knowledge improvement to improving clinical practice, as measured by completion of inpatient postfall proforma. This may be due to several factors—involving only a small subset of junior doctors or lack of simulation to address other practical limitations. Also, we noted only a small percentage of falls was assessed by FY1 and usually in conjunction with another doctor. Therefore, assessing the exclusive impact of the short presentation on change in practice was difficult. A limitation of this study design related to the sample size, which was largely dictated by the attendance rates to the weekly F1 teaching which in turn represented varied questionnaire responses rates per phase of the study. The FY1 were asked to complete the postintervention questionnaire only if they answered affirmatively to have attended the initial presentation. However, we acknowledge we cannot confirm the same as we did not formally register the participants. Also, it was not possible to maintain the same cohort of individuals to answer each of the three questionnaires as some FY1 may not have attended the teaching session when postintervention change in knowledge was measured or did not confirm they attended the presentation. Although a limitation, this is representative of the expected reality of the delivery of this type of intervention as not all individuals will necessarily be able to attend the sessions.
Lecture-based education has its own limitations. Learning pyramid theory suggests that average retention following a lecture can be as low as 5%.29 30 Therefore, a different method of educational intervention may be more appropriate in future. The thought that if educational sessions were better attended and targeted then this would have improved translation into clinical practice, is supported by two other quality improvement projects where educational interventions regarding falls reporting15 and assessment.31 In both of these studies, educational interventions took place on the ward weekly, led by clinicians15 or were included in the compulsory FY1 induction training31 for which 100% registered education is required. Due to limitations in time frame and resources, unfortunately neither of these approaches could be used during this project. In future interventions, these are various strategies that could be explored. One potential solution to this, which we have now introduced, is recording a version of the falls training education session which can be viewed on-line by all doctors in training in the Trust. The impact of this will be evaluated in due course.
Conclusion
We designed the study to replicate the junior doctors’ induction mandated by most Trusts and found that although such interventions result in an initial improvement in knowledge, this is neither sustainable nor does it translate to clinical practice. We plan to learn from the lessons from this study and design a more practice-based intervention to improve postfalls management in the future.
Acknowledgments
Thanks must go to the staff and patients at the Queen Elizabeth Hospital Birmingham who supported the work. Thanks must, in particular, go to the Postgraduate education team who supported the teaching and delivery of the intervention.
Footnotes
Contributors: All authors were involved in the design of the study. PK, JSC, RH, LB, JW, WM and AD were responsible in the collection of the data. PK and JSC were responsible for the data analysis. PK, JSC, RH, LB and JT were mainly responsible for the drafts of the write-up which were agreed on by all authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: This work was intended to improve patient safety and care without carrying out interventions on human subjects. As such, under Trust policy at the Queen Elizabeth Hospital, Birmingham it was exempt from ethical approval being an improvement study rather than a study on human subjects. However, the study was registered on the internal audit mechanism. All patient data was anonymised during analysis.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The raw anonymised data from the study is held by the authors who can be contacted if it is wished to be reproduced elsewhere.
References
- 1. Ringe JD. The effect of Vitamin D on falls and fractures. Scand J Clin Lab Invest Suppl 2012;243:73–8. 10.3109/00365513.2012.681965 [DOI] [PubMed] [Google Scholar]
- 2. Ash KL, MacLeod P, Clark L. A case control study of falls in the hospital setting. J Gerontol Nurs 1998;24:7–9. 10.3928/0098-9134-19981201-05 [DOI] [PubMed] [Google Scholar]
- 3. Morse JM, Prowse MD, Morrow N, et al. . A retrospective analysis of patient falls. Can J Public Health 1985;76:116–8. [PubMed] [Google Scholar]
- 4. Pearce L. Preventing falls in hospital. Nurs Stand 2017;31:15. [DOI] [PubMed] [Google Scholar]
- 5. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013;75:51–61. 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 6. Yoshida S. A global report on falls prevention epidemiology of falls. Geneva: WHO Rep, 2007:1–40. [Google Scholar]
- 7. Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001;50:116–9. 10.1097/00005373-200101000-00021 [DOI] [PubMed] [Google Scholar]
- 8. Fife D, Barancik JI. Northeastern Ohio Trauma Study III: incidence of fractures. Ann Emerg Med 1985;14:244–8. 10.1016/S0196-0644(85)80448-0 [DOI] [PubMed] [Google Scholar]
- 9. Service NI. The incidence and cost of Inpatient falls in hospitals. 2017. https://improvement.nhs.uk/uploads/documents/Falls_report_July2017.v2.pdf
- 10. Morello RT, Barker AL, Watts JJ, et al. . The extra resource burden of in-hospital falls: a cost of falls study. Med J Aust 2015;203:367 10.5694/mja15.00296 [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. Collaborating Centre for Research and Training in Mental Health. WHO | Falls. WHO 2016. http://www.who.int/mediacentre/factsheets/fs344/en/ [Google Scholar]
- 12. Sri-on J, Tirrell GP, Lipsitz LA, et al. . Is there such a thing as a mechanical fall? Am J Emerg Med 2016;34:582–5. 10.1016/j.ajem.2015.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Healey F, Monro A, Cockram A, et al. . Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing 2004;33:390–5. 10.1093/ageing/afh130 [DOI] [PubMed] [Google Scholar]
- 14. Hill AM, McPhail SM, Waldron N, et al. . Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet 2015;385:2592–9. 10.1016/S0140-6736(14)61945-0 [DOI] [PubMed] [Google Scholar]
- 15. Singh I, Okeke J. Reducing inpatient falls in a 100% single room elderly care environment: evaluation of the impact of a systematic nurse training programme on falls risk assessment (FRA). BMJ Qual Improv Rep 2016;5:u210921.w4741 10.1136/bmjquality.u210921.w4741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Annual Report and Accounts. 2016. https://www.uhb.nhs.uk/Downloads/pdf/AnnualReport16-17.pdf (accessed 8 Jul2017).
- 17. Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ 2004;329:1017 10.1136/bmj.329.7473.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smits PB, de Buisonjé CD, Verbeek JH, et al. . Problem-based learning versus lecture-based learning in postgraduate medical education. Scand J Work Environ Health 2003;29:280–7. 10.5271/sjweh.732 [DOI] [PubMed] [Google Scholar]
- 19. Boling B, Hardin-Pierce M. The effect of high-fidelity simulation on knowledge and confidence in critical care training: An integrative review. Nurse Educ Pract 2016;16:287–93. 10.1016/j.nepr.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 20. Lavelle M, Attoe C, Tritschler C, et al. . Managing medical emergencies in mental health settings using an interprofessional in-situ simulation training programme: A mixed methods evaluation study. Nurse Educ Today 2017;59:103–9. 10.1016/j.nedt.2017.09.009 [DOI] [PubMed] [Google Scholar]
- 21. Koh GC, Khoo HE, Wong ML, et al. . The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ 2008;178:34–41. 10.1503/cmaj.070565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cantillon P. Teaching large groups. BMJ 2003;326:437 10.1136/bmj.326.7386.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Freeman S, Eddy SL, McDonough M, et al. . Active learning increases student performance in science, engineering, and mathematics. Proc Natl Acad Sci U S A 2014;111:8410–5. 10.1073/pnas.1319030111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miller CJ, McNear J, Metz MJ. A comparison of traditional and engaging lecture methods in a large, professional-level course. Adv Physiol Educ 2013;37:347–55. 10.1152/advan.00050.2013 [DOI] [PubMed] [Google Scholar]
- 25. Kempegowda P, Livesey AC, McFarlane-Majeed L, et al. . Are they high on steroids? Tailored interventions help improve screening for steroid-induced hyperglycaemia in hospitalised patients. BMJ Open Qual 2018;7:e000238 10.1136/bmjoq-2017-000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kempegowda P, Saeed M, Foot S. (Short‐burst Teaching Aimed at Medical Professionals) [Impact of ‘short‐burst’ teaching on the knowledge regarding the Ipswich Touch Test] — MujahidSaeed.com. In: Diabetes UK. 2016. https://mujahidsaeed.com/wp-content/uploads/foot-stamp-study-ipswich-touch-test-mujahid-saeed-poster.pdf (accessed 29 Apr2018).
- 27. Portela MC, Pronovost PJ, Woodcock T, et al. . How to study improvement interventions: a brief overview of possible study types. BMJ Qual Saf 2015;24:325–36. 10.1136/bmjqs-2014-003620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Singapore Ministry of Health. MOH nursing clinical practice guidelineS 1/2005 Prevention of Falls in Hospitals and Long Term Care Institutions. 2005. https://www.moh.gov.sg/content/dam/moh_web/HPP/Nurses/cpg_nursing/2005/prevention_of_falls_in_hosp_ltc_institutiions.pdf (accessed 19 Aug2017).
- 29. Lalley JP, Miller RH. The learning pyramid: does it point teachers in the right direction? http://www.impudent.org.uk/wordpress/wp-content/uploads/2015/03/Lalley-Miller-TheLearningPyramid-Education-200709-.pdf (accessed 27 Apr 2018).
- 30. Sousa DA. How the brain learns : a classroom teacher’s guide. 2001. https://eric.ed.gov/?id=ED447094 (accessed 27 Apr 2018).
- 31. Nelson E, Reynolds P. Inpatient Falls: Improving assessment, documentation, and management. BMJ Qual Improv Rep 2015;4:u208575.w3781 10.1136/bmjquality.u208575.w3781 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2017-000222supp001.pdf (76.8KB, pdf)