Abstract
Background:
Pediatric surgery is one of the most difficult surgical fellowships to obtain. It requires stellar academic credentials and, often, dedicated time pursuing research. It is unknown, however, if pediatric surgeons maintain high academic output as faculty members. We hypothesized that the majority of pediatric surgeons do not pursue robust research activities as faculty, and therefore, over time, their academic productivity decreases.
Methods:
Numbers of publications, citations, H-index, and NIH funding rates were determined for 4354 surgical faculty at the top-55 NIH based departments of surgery using websites, Scopus, NIH RePORTER, and Grantome. Continuous variables were compared with ANOVA and post-hoc Bonferroni; categorical variables by χ2 test. p < 0.05 was significant.
Results:
In this dataset, 321 pediatric surgery (PS) faculty represented 7.4% of the cohort. Among PS faculty, 31% were assistant professors, 24% associate professors, 31% full professors and 13% had no academic rank. PS faculty had significantly more publications, a higher H index, and more high level NIH funding early in their careers at the assistant professor level compared to general surgeons. PS faculty at the associate professor level had equivalent high level NIH funding, but lower recentness and academic power compared to general surgeons. Professors of PS rebounded slightly, with only observed deficiencies in number of citations compared to general surgeons.
Conclusions:
PS faculty in assistant professor ranks has higher scholarly productivity compared to equivalently ranked general surgeons. Despite some mild academic setbacks in midcareer, pediatric surgeons are able to maintain similar academic productivity to their general surgery colleagues by the time they are full professors.
Level of evidence:
2.
Keywords: Pediatric surgery Workforce, Academic metrics, Publications, Pediatric surgery, Citations, H-index
For decades the successful academic surgeon was touted as a “triple threat”. He or she maintained a busy clinical practice, was actively involved in medical education, and touted a robust research laboratory with abundant extramural funding. As medical diagnostics and patient care have become more complex though, a new paradigm of medicine has emerged, and the “triple threat” is becoming exceedingly rare. This new model recognizes that “no physician can be a competent triple threat; that few clinicians will also be investigators; that no single clinician can know everything even in his or her own specialty; and that effective care requires collaborative, multidisciplinary teams” [1,2].
In the field of pediatric surgery, the academic mission of performing research is becoming threatened. As more and more people are being financially encouraged to increase operative revenue, the efforts placed on research are becoming much less. Additionally, studies note that research endeavors decline over time as educational and administrative responsibilities increase [3]. In an area when the pediatric surgical workforce is being critically examined, we must not only consider the number of pediatric surgeons who is partaking in clinical care of patients, but also those who are being encouraged to explore scientific research. Many of the predictive models for workforce assume that each surgeon is 100% committed to patient care, when in fact, most have other academic interests, including research [4].
Additionally, a strong research background has traditionally been required for general surgery graduates to enter a pediatric surgery fellowship. Now, though program directors are questioning the utility of research altogether, and many are more inclined to allow residents to explore other growth options such as global health and service [2]. In this regard, potential work force changes that may impact the number of practicing pediatric surgeons as well as the lack of desire to pursue scientific avenues may severely endanger pediatric surgery academia. In order to guide leaders in the field, it is essential to know to what degree pediatric surgeons maintain high academic output as faculty members. We therefore hypothesized that the majority of pediatric surgeons do not pursue robust research activities as faculty, and therefore, over time, their academic productivity declines.
1. Methods
In order to define the academic drivers of success in the top U.S. departments of surgery, the top 50-ranked-university based departments of surgery were identified based on current NIH funding available from the Blue Ridge Institute for Medical Research as previously described [5–11]. Additionally, a Medline search and review of current meetings were performed to identify additional institutions that had a significant academic impact but were not present on the NIH funding rank list. This search yielded 5 additional hospital-based departments of surgery all of which were associated with, but separate from, a medical school. These 55 departments of surgery were compiled into a master database. Online websites for each of the 55 identified departments of surgery were then used to generate a list of surgical faculty members at these institutions. Demographic variables including academic rank, specialty, and division were collected from the departmental websites as available.
Three additional data sources were used to collect additional data for the surgical faculty: 1) Elsevier’s SCOPUS bibliographical database (http://proxyauth.uits.iu.edu/auth/ulib.pl?url=http://www.scopus.com); 2) the NIH Research Portfolio Online Reporting Tools (RePORT) (http://report.nih.gov/); and 3) Grantome (http://grantome.com/) databases for the type and number of NIH grants awarded to each of these faculties.
1.1. Scopus
For each faculty member identified the SCOPUS database was used to determine their individual scholarly metrics including the total publications, total career citations, 3-year citations and H-index. SCOPUS was accessed online at http://scopus.com.proxy.medlib.iupui.edu. Data collection occurred from 9/01/2014 through 1/31/2015.
1.2. NIH funding
For all faculty identified in the database, data regarding research funding from the National Institutes of Health (NIH) was also collected. This data was searched from the NIH online data repository of funding, NIH RePORT and checked with the Grantome online database. These databases were used to collect data regarding the type of NIH funding, the total funding amount in dollars, the type of NIH grant (R01, U01, F32, etc), the funding agency (NCI, NAI, NIGMS, etc), and the numbers of each of the NIH grants. These data were then used to create a binned variable to categorize NIH funding. The bins that were created included the following categories: (1) no current or former NIH funding, (2) NIH R01/U01/P01 funding, and (3) NIH smaller grants (F32, R03, T32, R23…) funding.
1.3. Ethics statement
Only publically available datasets were queried for examination. This study was exempt from review by the institutional review board (IRB) of Indiana University School of Medicine. (http://www.hhs.gov/ohrp/policy/checklists/decisioncharts.html).
1.4. Database and statistical analysis
Data from each of the sources was collated into the master database. The variables in the database were categorized as either continuous or categorical. Continuous variables included total numbers of publications, total career citations, 3-year citations, H-indices, and academic power. Categorical variables included academic rank, credentials, presence of current or past NIH funding, and type of NIH funding.
Mean and standard deviations were calculated for total publications, total- and three-year citations, and H-indices. For these variables, group comparisons were performed across the different categorical variables. Continuous variables were compared by ANOVA with post-hoc Bonferroni for multiple group comparisons. Differences between categorical variables were tested using χ2 test, as appropriate. Statistical tests with p < 0.05 were deemed significant. All statistical tests were performed using SPSS for Windows, Version 15.0. Chicago, IL, SPSS Inc. All statistical analyses were performed with consultation and input from a biostatistician (TB).
2. Results
The complete dataset consisted of 4354 members of departments of surgery from 55 different institutions. Six hundred fifty-two did not have an assigned rank within the department or were noted as “instructors”. This left 3702 members for analysis. Pediatric surgery faculty represented 7.4% of the cohort, while general surgeons (acute care, general and minimally invasive surgery, surgical oncology, and trauma/critical care) represented 36.3% of the cohort. Members of other subspecialties represented 41.3% of the cohort (Table 1). Among pediatric surgery faculty, 31% were assistant professors, 24% associate professors, 31% full professors, and 13% had no academic rank.
Table 1.
Academic ranking of faculty members in database.
| Total number |
Percent of total |
Assistant professor |
Associate professor |
Full professor |
|
|---|---|---|---|---|---|
| Pediatric surgery | 321 | 7.4 | 101 | 78 | 101 |
| General surgery | 1582 | 36.3 | 543 | 392 | 435 |
| Other surgical specialties | 1799 | 41.3 | 503 | 369 | 589 |
| Total | 3702 | 85 | 1147 | 839 | 1125 |
| Missing rank | 652 | 15 | |||
| Total | 4354 | 100 |
2.1. Publications
At the level of assistant professor, pediatric surgeons and surgeons of other specialties both had significantly more publications than general surgeons (pediatric, 33 ± 53 publications; general, 20 ± 27 publications; other specialties, 29 ± 51 publications; p = 0.027 and p = 0.008, respectively). There were no significant differences between pediatric surgeons and other specialties at the assistant professor level. At the associate professor level, surgeons of other specialties continued to maintain more publications than general surgeons, while pediatric surgeons had similar numbers of publications compared to general surgeons, thereby suggesting that the productivity of those in other specialties was maintained. There were no significant differences between pediatric surgeons, general surgeons, or surgeons of other specialties at the full professor level (Fig. 1).
Fig. 1.
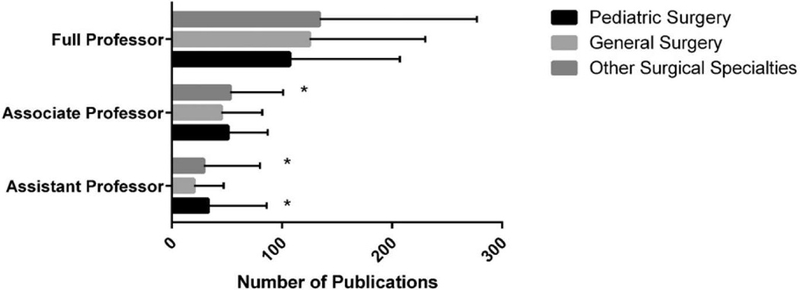
Number or publications among surgical faculty members divided by rank. * = p < 0.05 versus general surgery faculty.
2.2. Citations
There were no statistically significant differences in numbers of citations between pediatric surgeons, general surgeons, and other specialty surgeons at the assistant professor level. Associate professors of other specialties maintained more citations than general surgeons of the same rank. There were no differences between pediatric surgeons and general surgeons in regards to citations at the associate professor level. Pediatric surgeons at the full professor level had significantly fewer citations than their general surgery counterparts (pediatric, 2485 ± 2975 citations; general, 3739 ± 4442 citations; p = 0.036). There was no difference between pediatric surgery professors and other specialty professors in terms of total numbers of citations (Fig. 2).
Fig. 2.
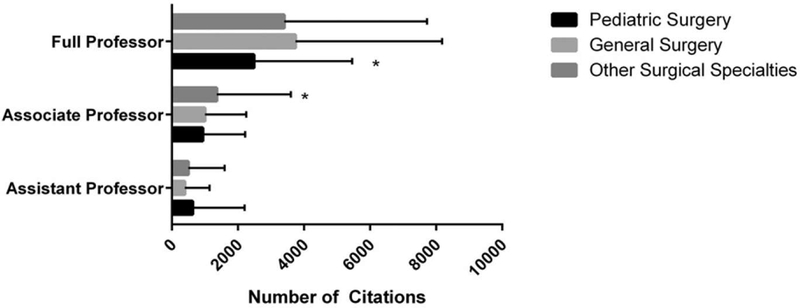
Number of citations among surgical faculty members divided by rank. * = p < 0.05 versus general surgery faculty.
Recentness of citations, defined as citations within a 3-year period divided by total citations, was significantly lower for pediatric surgery and other subspecialty associate professors as compared to general surgery associate professors (pediatric, 0.28 ± 0.17; general, 0.38 ± 0.21; other specialties, 0.30 ± 0.20; p = 0.001 and p = < 0.001, respectively). No significant differences were identified in recentness of citations between members of the assistant professor or full professor levels (Fig. 3).
Fig. 3.
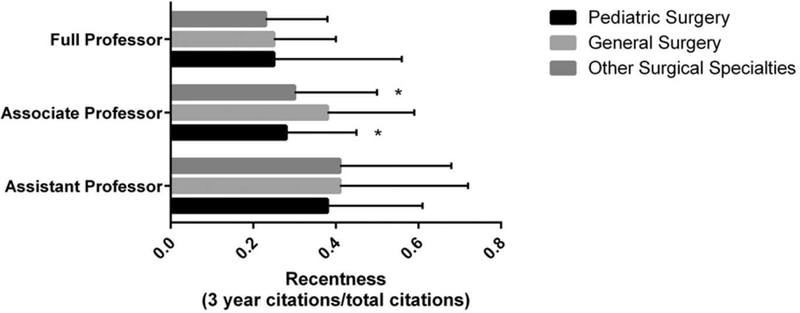
Recentness of citations (3-year citations/total citations) among surgical faculty members divided by rank. * = p < 0.05 versus general surgery faculty.
2.3. Other metrics
The H-index is a metric that attempts to measure productivity and citation impact of a scientist’s publications. It is based on the set of the scientist’s most cited papers and the number of citations that they have received in other publications [12]. It was designed so that scientists could move away from the journal’s impact factor as a way to judge their productivity. It essentially normalizes less cited articles in higher impact journals with more heavily cited articles in lower impact journals [13]. The H-index was found to be significantly higher with pediatric surgery and other specialty assistant professors as compared to general surgery assistant professors (pediatric, 10 ± 8; general, 8 ± 7; other specialty, 9 ± 8; p = 0.008 and p = 0.032 respectively). No significant differences were observed between pediatric surgery assistant professors and assistant professors of other subspecialties. Additionally, there were no significant differences in H-index levels for associate or full professor groups (Fig. 4).
Fig. 4.

H-index of surgical faculty members divided by rank. * = p < 0.05 versus general surgery faculty.
Academic power is a relatively new metric of academic productivity. It has previously been defined as [publications/total-citations] × [3-year citations/total-citations] [11]. It takes into account the academic impact and the relative recentness of publications. In essence, it is a metric of academic velocity. Academic power was found to be significantly lower in pediatric surgery associate professors compared to their general surgery counterparts (pediatric, 5.03 ± 6.77; general, 7.19 ± 5.35; p = 0.010) (Fig. 5). No significant differences were seen in academic power between assistant or full professor groups.
Fig. 5.

Academic power of surgical faculty members divided by rank. * = p < 0.05 versus general surgery faculty.
2.4. NIH funding
Although total funding was equivalent between pediatric and general surgeons across all ranks, more pediatric surgeons at the assistant professor level were found to have high level NIH funding (R01, U01, P01) as compared to their general surgery counterparts (p < 0.05, Table 2). There were no significant differences between pediatric and general surgeons in this type of funding at the associate professor or full professor levels.
Table 2.
High-level NIH funding (R01, P01, U01) among pediatric surgeons, general surgeons, and surgeons of other specialties by academic rank.
| Academic rank | Pediatric surgery | General surgery | Other surgical specialties | Pediatric vs. general surgery p value | Pediatric vs. other surgical specialties p value |
|---|---|---|---|---|---|
| Assistant | 7 (6.9) | 13 (2.4) | 15 (3.0) | 0.016 | 0.053 |
| Associate | 8 (10.3) | 29 (7.4) | 37 (10.0) | 0.392 | 0.951 |
| Professor n (%) | 21 (20.8) | 89 (20.5) | 160 (27.2) | 0.941 | 0.176 |
3. Discussion
The number of practicing pediatric surgeons in the U.S. and their ability to provide care to patients now and in the future has been a controversial topic of recent discussion. Many see a changing paradigm in the number and types of cases that are seen at academic institutions [14]. Some feel that there will be too many pediatric surgeons in the future, and that the index case loads of these individuals will be diluted. This dilution has the potential to affect outcomes and verification indices [15,16].
Unfortunately, many of the predictive models and discussions on pediatric surgical workforce fail to account for the full academic mission of pediatric surgery, namely the addition of research, education, and administrative duties. Most pediatric surgeons in academic institutions have, on average, up to 10% of their job description dedicated to these endeavors [4], and therefore predictive modeling needs to account for these additional activities.
Herein, we were able to measure the academic productivity of pediatric surgeons, general surgeons, and surgeons of other subspecialties over the course of their collective careers. We found that within assistant professor roles, pediatric surgeons and surgeons of other subspecialties had higher numbers of publications and a higher H-index than their general surgery colleagues. However, all had equivalent total citations, power, and more importantly, recentness (3-year citations/total citations) at this initial faculty level. This would suggest that much of the academic productivity in pediatric surgeons at the assistant professor level stemmed from academic work that was performed in the past, such as during residency research fellowships. In light of higher past academic productivity, assistant professors in pediatric surgery also had more high level NIH funding (NIH R01, U01, P01) as compared to similar ranked general surgeons. This may suggest that pediatric surgeons had robust research training during residency that was able to launch them fairly quickly into early, high level NIH funding.
At the associate professor level, number of publications and citations in other specialties were significantly higher than general surgeons, but the H-index and power were equivalent between these two groups. However, pediatric surgeons maintained equivalent publications, citations, H-index levels, and high level NIH funding compared to general surgeons, but lower levels of recentness and power. The combination of these metrics suggests a lower academic velocity within pediatric surgeons at the midcareer level.
By the time pediatric surgeons reach the full professor level, academic metrics appear to equilibrate with notable deficiencies only seen in number of citations in pediatric surgeons compared to general surgeons. All other measures of academic metrics were similar among professors. With regards to funding, pediatric surgeon professors had equivalent high level NIH funding compared to general surgery professors.
Sections of pediatric surgery are often small in comparison to the much larger general surgery groups. In this dataset of the top 55 funded institutions, pediatric surgeons made up 7.4% of the cohort while general surgeons made up 36.3%. Therefore, one could argue that pediatric surgeons do a similar amount of academic work with only a quarter of the personnel. In addition, because of their small group sizes, pediatric surgeons likely have more individual responsibilities within their division compared to members of the general surgery divisions (ie teaching, program director, operating room representative, etc). These other duties could reduce their productivity more than general surgeons. Work duties may be spread out in larger general surgery groups, thereby giving them more time for research practices.
During a pediatric surgeon’s career there are inarguably a number of forces that could reduce productivity. These include restricted manpower and more call, increased demands for pediatric surgeons to care for the surgical needs of all children, increased administrative burdens, decreased funding mechanisms and lower national research budgets, and decreased compensation plans for those who pursue research. In addition, many of the well published and highly productive surgeons go on to lead sections or even departments of surgery, and therefore, likely give up a portion of their research endeavors to perform these new tasks. Despite these new duties, it appears that pediatric surgery professors still maintain equivalent academic profiles compared to their general surgery colleagues.
As we continue to consider the issues surrounding pediatric surgery work force we must appropriately allocate resources to preserve the academic mission of our field. These resources include not only monetary resources, but also the surgeon scientists to actually perform the research. We must consider if perhaps more pediatric surgeons, rather than fewer, are actually required to insure the sustainability of our academic mission. Intentionally decreasing the number of pediatric surgeons would increase call coverage and other clinical responsibilities that may impede research. However, more pediatric surgeons would allow for increased protected time for surgeon scientists to pursue their valuable research, while simultaneously allowing more urgent patient care issues to be covered by those who are more clinically focused. If we value the contribution of research to our profession, we must aggressively recruit new scientists into our field and protect the time and financial interests of those who are currently pursuing academic research activities.
4. Limitations
This study has several limitations. First, as the members of the surgical faculty were compiled based on department websites, it is possible that these sites were not up to date in terms of members of the department or their rank. Additionally, 652 faculty members (approximately 15% of the study population) had no rank assignment or were missing ranks on these sites. These individuals were not included in calculations which could alter the results.
An alternative hypothesis could exist in that general surgeons who remain in an academic environment are simply more productive because of selection bias. That is, perhaps there are more options for a general surgeon to enter community or employed nonacademic practice given the size of that workforce compared to pediatric surgeons. If so, the general surgeons remaining in academic life would demonstrate a selection bias compared to pediatric surgeons. Another limitation is that the number of publications and citations were cumulative over the faculty’s career. Therefore, publications obtained in undergraduate training and medical schools were counted in addition to those achieved during their time as faculty. This may have skewed the data, but given that the method of data collection was performed the same for all faculty members, it is expected that this would “wash out” in any analysis.
Lastly, the authors realize that the NIH is not the only funding source for investigators, and that researchers could have had significant high level funding from other sources including the Department of Defense or other institutions. The NIH funding mechanisms were chosen because the data is publically available and the websites are easy to search for investigators. This is the only large, publically available dataset that would include all potential investigators.
5. Conclusion
Junior pediatric surgery faculty has more publications, a higher Hindex, and higher numbers of high level NIH grants compared to their colleagues in general surgery. Despite some mild academic setbacks in midcareer, pediatric surgeons are able to maintain similar academic productivity to their general surgery colleagues by the time they are full professors. A number of forces clearly have the potential to reduce the productivity of our academic leaders over time. Therefore, preservation of the pediatric surgeon scientist should be considered when discussions of pediatric surgery workforce are held.
Footnotes
TAM drafted manuscript and performed critical revisions of manuscript; NPV/BAK performed data collection and critical revisions to manuscript; TMB performed statistical analysis and added critical revisions of manuscript; TAZ/LGK performed study conception and design and provided critical revisions to the manuscript.
References
- [1].Emanuel EJ, Fuchs VR. Shortening medical training by 30%. JAMA 2012;307:1143–4. [DOI] [PubMed] [Google Scholar]
- [2].Markel TA, Rescorla FJ. A survey of the pediatric surgery program directors: optimizing resident research to make pediatric surgery training more efficient. J Pediatr Surg 2015;50:1053–7. [DOI] [PubMed] [Google Scholar]
- [3].Chokshi NK, Simeone DM, Chari RS, et al. A survey of academic surgeons: work, stress, and research. Surgery 2009;146:462–8. [DOI] [PubMed] [Google Scholar]
- [4].Bouchard S, Laberge JM. Pediatric surgeons’ activities and future plans. J Pediatr Surg 1997;32:801–5. [DOI] [PubMed] [Google Scholar]
- [5].Roskosk R Jr Blue Ridge Institute for Medical Research (internet); 2014.
- [6].Valsangkar NP, Zimmers TA, Kim BJ, et al. Determining the drivers of academic success in surgery: an analysis of 3,850 faculty. PLoS One 2015;10:e0131678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zarzaur BL, Valsangkar N, Feliciano DF, et al. The transforming power of early career acute care surgery research scholarships on academic productivity. J Trauma Acute Care Surg 2016;81:137–43. [DOI] [PubMed] [Google Scholar]
- [8].Valsangkar NP, Blanton C, Mayo J, et al. Is there an impending loss of academically productive trauma surgical faculty? An analysis of 4,015 faculty. J Trauma Acute Care Surg 2016. [DOI] [PubMed]
- [9].Valsangkar NP, Kays JK, Feliciano DV, et al. The impact of members of the Society of University Surgeons on the scholarship of American surgery. Surgery 2016;160: 47–53. [DOI] [PubMed] [Google Scholar]
- [10].Bell TM, Valsangkar N, Joshi M, et al. The role of PhD faculty in advancing research in departments of surgery. Ann Surg 2016. [DOI] [PMC free article] [PubMed]
- [11].Valsangkar N, Fecher AM, Rozycki GS, et al. Understanding the barriers to hiring and promoting women in surgical subspecialties. J Am Coll Surg 2016. [DOI] [PubMed]
- [12].Hirsch JE An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A 2005;102:16569–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Not-so-deep impactNature 2005;435:1003–4. [Google Scholar]
- [14].Bruns NE, Shah MA, Dorsey AN, et al. Pediatric surgery – a changing field: national trends in pediatric surgical practice. J Pediatr Surg 2016;51:1034–8. [DOI] [PubMed] [Google Scholar]
- [15].Bucher BT, Guth RM, Saito JM, et al. Impact of hospital volume on in-hospital mortality of infants undergoing repair of congenital diaphragmatic hernia. Ann Surg 2010; 252:635–42. [DOI] [PubMed] [Google Scholar]
- [16].Reames BN, Ghaferi AA, Birkmeyer JD, et al. Hospital volume and operative mortality in the modern era. Ann Surg 2014;260:244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]


