Abstract
Objective
To update the projected prevalence of arthritis and arthritis-attributable activity limitations among US adults, using a newer baseline for estimates.
Methods
Baseline prevalence data were obtained from the 2010–2012 National Health Interview Survey. Arthritis was defined as an answer of “yes” to the question “Have you ever been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus or fibromyalgia?” Arthritis-attributable activity limitation was defined as an answer of “yes” to the question “Are you limited in any way in any of your usual activities because of arthritis or joint symptoms?” The baseline prevalence of arthritis and arthritis-attributable activity limitation was stratified according to age and sex and was statistically weighted to account for the complex survey design. The projected prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation was calculated by multiplying the age- and sex-stratified population estimates projected for 2015–2040 (in 5-year intervals; provided by the US Census Bureau) by the baseline estimates. Age-and sex-specific prevalences were summed to provide the total prevalence estimates for each year.
Results
In 2010–2012, 52.5 million adults in the US (22.7% of all adults) had doctor-diagnosed arthritis, and 22.7 million (9.8%) had arthritis-attributable activity limitation. By 2040, the number of US adults with doctor-diagnosed arthritis is projected to increase 49% to 78.4 million (25.9% of all adults), and the number of adults with arthritis-attributable activity limitation will increase 52% to 34.6 million (11.4% of all adults).
Conclusion
Updated projections suggest that arthritis and arthritis-attributable activity limitation will remain large and growing problems for clinical and public health systems, which must plan and create policies and resources to address these future needs.
Arthritis and other rheumatic conditions affect 53 million US adults ages 18 and older (1), are the most common cause of disability (2), and are associated with considerable pain, activity limitation, and restriction of work and social participation (1,3–5). Projecting changes in the prevalence and impact of chronic diseases such as arthritis is crucial for planning future clinical and public health needs, informing health policy, and establishing priorities for planning and resource allocation.
The aging of the population is a factor that has driven previous projections of arthritis prevalence and the associated impact (6). A new report from the US Census Bureau confirms that aging will remain an important factor in the future: by the time of the 2030 census, all “baby boomers” will have reached age 65 years, and 1 in 5 US adults will be 65 years of age or older (7).
Previous projections of arthritis prevalence (6) based on 2003 data have tracked well against subsequent arthritis prevalence estimates (1). For example, the prevalence of arthritis was 52.5 million in 2010–2012 (1), and in 2003 the prevalence projected for 2015 was 55.7 million (6), which is consistent with the observed net increase in prevalence of ~1 million per year. In contrast, the prevalence of arthritis-attributable activity limitation for 2010–2012 (22.7 million) (1) has already surpassed the prevalence projected for 2020 (22.1 million) (6), which is higher than the previously observed net increase of ~500,000 per year. Given the apparent change in the prevalence of arthritis-attributable activity limitation, the purpose of this study was to update the age- and sex-specific projections for arthritis prevalence and arthritis-attributable activity limitation in adults ages 18 years and older through 2040, using a newer baseline for estimates.
PATIENTS AND METHODS
The National Health Interview Survey (NHIS), which is one of the major data collection programs of the National Center for Health Statistics (NCHS), is an annual population-based survey that uses a complex stratified sample design to collect data on ~30,000 households (children and adults). The Sample Adult Core contains detailed health information on 1 adult who was randomly selected from each sampled household; these adults completed a questionnaire administered in-person by a trained interviewer. The NHIS provides national estimates for the non-institutionalized civilian US population (8).
In contrast to the prior projection using a single year of data (2003) for baseline estimates (6), this analysis used a 3- year (2010–2012) rolling average for 2 reasons: 1) a rolling average will likely smooth any year-to-year random variation in baseline estimates, and 2) these years are the basis for current estimates of the prevalence of arthritis and arthritis-attributable activity limitation (1). The unweighted sample size and response rates for the Sample Adult Core were 27,157 (60.8%), 33,014 (66.3%), and 34,525 (61.2%) for 2010, 2011, and 2012, respectively. A case of doctor-diagnosed arthritis was defined as an answer of “yes” to the question “Have you ever been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus or fibromyalgia?” This definition of arthritis has been cognitively tested and validated for population surveillance purposes (9). Among adults with doctor-diagnosed arthritis, arthritis-attributable activity limitation was defined as an answer of “yes” to the question “Are you limited in any way in any of your usual activities because of arthritis or joint symptoms?”
The baseline prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation according to age and sex was estimated using sample weights provided by the NCHS to account for the complex survey design. Projected estimates of the population of persons ages 18 years and older, according to age and sex, for 2015–2040 were obtained from the US Census Bureau (10). These projected population estimates are based on the July 1, 2013 population estimates, which in turn use the 2010 census as the base.
The projected prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation, overall and stratified by age and sex, was calculated by multiplying the projected estimate of the population (in 5-year intervals) by the baseline 3-year rate provided by the NHIS. We analyzed age in predefined strata combinations to determine the narrowest age bands across all age and sex groups that consistently met NCHS standards for reliability (ages 18–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85+ years). Age- and sex-specific prevalences were summed to provide the total prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation for each year.
RESULTS
In 2010–2012, 52.5 million US adults (22.7% of all adults) had doctor-diagnosed arthritis, and 22.7 million had arthritis-attributable activity limitation (Table 1). By 2040, the prevalence of doctor-diagnosed arthritis is projected to increase 49% to 78.4 million (25.9% of the adult population) (Table 2), and the prevalence of arthritis-attributable activity limitation will increase 52% to 34.6 million (11.4% of the population [43.2% of adults with arthritis]) (Table 2). In 2040, women will continue to account for the majority of arthritis cases (58.5%; 45.8 million).
Table 1.
Baseline age- and sex-specific weighted prevalence estimates of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, from the National Health Interview Survey 2010–2012
| Sex, age in years | Doctor-diagnosed arthritis | Arthritis-attributable activity limitation | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Sample size | Weighted no. in 1,000s* | Proportion* | Sample size | Weighted no. in 1,000s* | Proportion* | |
| Men | ||||||
| 18–34 | 461 | 1,387 | 3.9 | 154 | 480 | 1.4 |
| 35–44 | 731 | 2,023 | 10.4 | 284 | 747 | 3.8 |
| 45–54 | 1,549 | 4,500 | 20.9 | 705 | 1,900 | 8.8 |
| 55–64 | 2,316 | 5,873 | 33.0 | 1,054 | 2,503 | 14.1 |
| 65–74 | 1,842 | 4,308 | 41.6 | 784 | 1,725 | 16.7 |
| 75–84 | 1,152 | 2,553 | 46.0 | 541 | 1,209 | 21.8 |
| 85+ | 379 | 782 | 48.6 | 210 | 410 | 25.5 |
| Total | 8,430 | 21,426 | 19.1 | 3,732 | 8,974 | 8.0 |
| Women | ||||||
| 18–34 | 761 | 1,847 | 5.2 | 271 | 642 | 1.8 |
| 35–44 | 1,202 | 2,826 | 14.0 | 534 | 1,165 | 5.8 |
| 45–54 | 2,463 | 6,188 | 27.6 | 1,161 | 2,713 | 12.1 |
| 55–64 | 3,577 | 8,005 | 41.8 | 1,776 | 3,732 | 19.5 |
| 65–74 | 3,167 | 6,340 | 53.1 | 1,411 | 2,579 | 21.6 |
| 75–84 | 2,215 | 4,135 | 55.2 | 1,079 | 1,910 | 25.5 |
| 85+ | 1,031 | 1,752 | 57.1 | 585 | 986 | 32.1 |
| Total | 14,416 | 31,094 | 26.0 | 6,817 | 13,727 | 11.5 |
| Total population | 22,846 | 52,520 | 22.7 | 10,549 | 22,701 | 9.8 |
Numbers and proportions (%) are weighted using the adult sample weight provided by the National Center for Health Statistics.
Table 2.
Projected US adult population and projected prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation among adults ages 18 years and older, 2015–2040*
| Year | Estimated population | Projected prevalence of doctor-diagnosed arthritis | Projected prevalence of arthritis-attributable activity limitation | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Total | Men | Women | Total | Men | Women | ||
| 2015 | 247.7 | 58.0 (23.4) | 23.8 (19.7) | 34.2 (26.9) | 25.1 (10.1) | 10.0 (8.3) | 15.1 (11.9) |
| 2020 | 260.4 | 62.7 (24.1) | 25.8 (20.3) | 36.9 (27.7) | 27.2 (10.4) | 10.9 (8.5) | 16.3 (12.2) |
| 2025 | 272.3 | 67.2 (24.7) | 27.8 (20.8) | 39.5 (28.4) | 29.2 (10.7) | 11.7 (8.8) | 17.5 (12.5) |
| 2030 | 283.1 | 71.5 (25.2) | 29.6 (21.3) | 41.9 (29.0) | 31.1 (11.0) | 12.5 (9.0) | 18.6 (12.9) |
| 2035 | 292.9 | 75.1 (25.6) | 31.1 (21.7) | 44.0 (29.4) | 32.9 (11.2) | 13.3 (9.3) | 19.6 (13.1) |
| 2040 | 302.0 | 78.4 (25.9) | 32.6 (22.0) | 45.8 (29.8) | 34.6 (11.4) | 14.0 (9.4) | 20.6 (13.4) |
Values are the number (%) in millions.
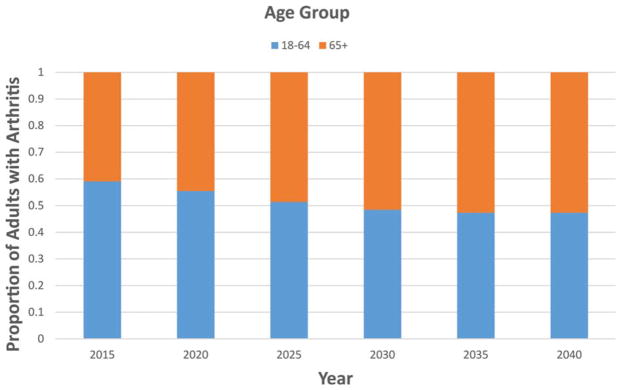
Between 2015 and 2040, the number of adults with doctor-diagnosed arthritis will increase 37% among men and 34% among women, while the number with arthritis-attributable activity limitation will increase 40% among men and 36% among women. For both men and women, the largest increase (from 73% to 78%) in the prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation will occur in the group of adults ages 65 years and older (data not shown). Adults in the traditional working-age population (ages 18–64 years) currently comprise the majority of affected adults. Adults in this age group will continue to comprise the majority of affected adults through 2025 and fully 47–48% of affected adults through 2040 (Figure 1), when 36.9 million will be affected. Given increasing trends in the upper age limit of what is classified as “working age” (11), those in an expanded working-age population may continue to comprise the majority of affected adults through 2040.
Figure 1.
Projected proportion of US adults with arthritis, according to age group and year.
DISCUSSION
These projections based on the current age- and sex-specific prevalence suggest that by 2040, 1 in 4 US adults (78.4 million) will have doctor-diagnosed arthritis, and 1 in 9 adults (34.6 million) will have arthritis-attributable activity limitation. Given that previous projections for the prevalence of arthritis-attributable activity limitation underestimated the observed prevalence for reasons that are not yet clear, the latter projection may also be low. Projected increases are similar in both sexes.
Not surprisingly, the largest population growth is among adults ages 65 years and older, because as baby boomers age, they become part of a higher-risk age group. This will likely have serious effects on Social Security Disability Income (SSDI) and Medicare programs. Between 1981 and 2000, SSDI benefits for musculoskeletal conditions increased 41%, surpassing circulatory disorders as the condition most frequently associated with the receipt of benefits (12). The SSDI trust fund is expected to be exhausted in 2016 (13). Between 1987 and 2002, arthritis accounted for 9% of the overall increase in health care spending among Medicare beneficiaries (ranked fourth of 10 chronic conditions) (14). Spending for arthritis will undoubtedly increase substantially with the increasing number of baby boomers eligible for Medicare and the increasing number of expensive (but effective) total joint replacements (15). According to Rula et al (16), using effective health promotion and chronic disease management programs aimed at reducing the risk of onset and progression of chronic disease such as arthritis could save Medicare between $650 billion and $1.43 trillion over 10 years.
Approximately half of adults with arthritis will be of traditional working age through 2040, which may affect the ability, type, and amount of work that they can do (4). Given the aging workforce, employers may need to increase efforts to modify worksites, job tasks, environments, and processes to accommodate employees who have arthritis. Vocational rehabilitation programs can result in the successful return to work of up to 69% of patients with rheumatic disease (17). Worksites might be useful places at which to offer physical activity and self-management education interventions that have been proven to improve pain, function, and quality of life in adults with arthritis (18).
What can be done to mitigate these projected effects? For individuals with arthritis, physical activity has been shown to decrease pain and improve function, which is particularly relevant for the millions of people with arthritis-attributable activity limitation (19). Walking 5,000–7,499 steps per day has a protective effect (relative risk 0.50, 95% confidence interval 0.33–0.76) against incident functional limitation (measured as slow gait speed) among adults with knee osteoarthritis (20). Walking programs such as the Arthritis Foundation’s Walk With Ease program have been proven to improve function, gait speed, strength, balance, and self-efficacy and to reduce pain, fatigue, and stiffness; these programs are easy and inexpensive strategies for increasing physical activity, which in turn may reduce functional limitation (21).
Can the health care system accommodate these projected increases? By 2025, the expected demand for rheumatologists is expected to exceed supply by 2,576 adult and 33 pediatric rheumatologists (22). The shortage of rheumatologists in non-urban areas is especially critical; for some areas, the closest rheumatologist is located >200 miles away (23). Shortages in the workforce of orthopedic surgeons, particularly among those performing total joint replacements, are also expected. Using sophisticated regression modeling accounting for growth in the population (not specifically growth in arthritis prevalence), rate of change in the number of arthroplasties from 1993 to 2010, age, race, sex, and Census region, Kurtz et al projected that the demand for total knee replacements will be 1.4 million per year by 2020 (15). Assuming that clinicians retire at age 65 years, the workforce of orthopedic surgeons in 2016 will be able to perform only 422,225 primary total knee replacements annually (24). Because the number of retiring surgeons will likely exceed the number of orthopedic residency slots in upcoming years, demand will outpace supply unless strategies for increasing the number of graduates of orthopedic training programs are immediately implemented (24). Strategies to address these shortages include using more physician assistants and nurse practitioners (25,26), implementing nurse-led clinics (27,28), and intensifying efforts to recruit trainees to the rheumatology and orthopedic specialties (29). As an adjunct to clinical care, health care providers can also refer patients to effective self-management education and physical activity programs offered in their local communities.
This study has several limitations. First, we could not take into account the effects of the current obesity epidemic, because census population projections do not include projections for body mass index (10). Obesity is a strong risk factor for knee osteoarthritis (30), which is one of the most common types of arthritis, and possibly other types of arthritis. If obesity could be taken into account, these estimates would likely be much higher, although we cannot speculate on the magnitude with any confidence at this time. Second, our analysis assumes that the 2010–2012 age- and sex-specific prevalence proportions will persist unchanged in the future, which may not be true, especially if the effects of the obesity epidemic affect later proportions. Last, public-access census projections were not available for race and ethnicity according to our age and sex stratifications; therefore, we were unable to assess the effects of the changing race and ethnicity demographics occurring through 2040 (10).
The strengths of this study include use of the large population-based NHIS to calculate the baseline prevalence and use of a 3-year rolling average to smooth any year-to-year variations in prevalence. Our case-finding question includes arthritis and other rheumatic conditions that would typically be seen by rheumatologists (e.g., fibromyalgia) and has been shown to be valid for public health surveillance purposes (9). These projections are also useful in planning for future clinical and public health needs, assessing health care utilization, anticipating workforce demands, and informing health policy.
These projected increases in the prevalence of arthritis and arthritis-attributable activity limitation have serious implications for a condition that is already the most common cause of disability (2). This large and increasing burden of arthritis over the next 25 years, along with the important role that arthritis already plays in the millions of adults with multiple chronic conditions (31), suggest that arthritis will remain an important factor for personal health and quality of life as well as public health.
Footnotes
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Helmick had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Hootman, Helmick, Barbour, Theis.
Acquisition of data. Hootman, Helmick, Theis.
Analysis and interpretation of data. Hootman, Helmick, Barbour, Theis, Boring.
The findings and conclusions contained herein are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the Agency for Toxic Substances and Disease Registry.
References
- 1.Barbour KE, Helmick CG, Theis KA, Murphy LB, Hootman JM, Brady TJ, et al. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation-United States, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;62:869–73. [PMC free article] [PubMed] [Google Scholar]
- 2.Brault MW, Hootman J, Helmick CG, Theis KA, Armour BS. Prevalence and most common causes of disability among adults, United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–6. [PubMed] [Google Scholar]
- 3.Theis KA, Murphy L, Hootman JM, Wilkie R. Social participation restriction among US adults with arthritis: a population-based study using the International Classification of Functioning, Disability and Health. Arthritis Care Res (Hoboken) 2013;65:1059–69. doi: 10.1002/acr.21977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Theis KA, Murphy L, Hootman JM, Helmick CG, Sacks JJ. Arthritis restricts volunteer participation: prevalence and correlates of volunteer status among adults with arthritis. Arthritis Care Res (Hoboken) 2010;62:907–16. doi: 10.1002/acr.20141. [DOI] [PubMed] [Google Scholar]
- 5.Theis KA, Murphy L, Hootman JM, Helmick CG, Yelin E. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey data. Arthritis Rheum. 2007;57:355–63. doi: 10.1002/art.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54:226–9. doi: 10.1002/art.21562. [DOI] [PubMed] [Google Scholar]
- 7.Colby SL, Ortman JM. Population estimates and projections: current population reports. Washington (DC): US Census Bureau; Mar, 2015. Projections of the size and composition of the U.S. population: 2014 to 2060. URL: http://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. [Google Scholar]
- 8.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the National Health Interview Survey, 2006–2015. Vital Health Stat 2. 2014;165:1–53. [PubMed] [Google Scholar]
- 9.Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32:340–7. [PubMed] [Google Scholar]
- 10.US Census Bureau. National population projections: summary tables. 2014 URL: http://www.census.gov/population/projections/data/national/2014/summarytables.html.
- 11.Riffkin R. Average U.S. retirement age rises to 62. Gallup; Apr 28, 2014. URL: http://www.gallup.com/poll/168707/average-retirementage-rises.aspx. [Google Scholar]
- 12.National Research Council. The dynamics of disability: measuring and monitoring disability for Social Security programs. URL: http://www.ncbi.nlm.nih.gov/books/NBK220744/pdf/TOC.pdf. [PubMed]
- 13.Social Security and Medicare Boards of Trustees. Status of the Social Security and Medicare programs: a summary of the 2014 annual reports. URL: https://www.socialsecurity.gov/OACT/TRSUM/tr14summary.pdf.
- 14.Thorpe KE, Howard DH. The rise in spending among Medicare beneficiaries: the role of chronic disease prevalence and changes in treatment intensity. Health Aff (Millwood) 2006;25:w378–88. doi: 10.1377/hlthaff.25.w378. [DOI] [PubMed] [Google Scholar]
- 15.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–30. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 16.Rula EY, Pope JE, Hoffman JC. Potential Medicare savings through prevention and risk reduction. Popul Health Manag. 2011;14:S35–44. doi: 10.1089/pop.2010.0063. [DOI] [PubMed] [Google Scholar]
- 17.De Buck PD, Schoones JW, Allaire SH, Vliet Vliieland TP. Vocational rehabilitation in patients with chronic rheumatic diseases: a systematic literature review. Semin Arthritis Rheum. 2002;32:196–203. doi: 10.1053/sarh.2002.34609. [DOI] [PubMed] [Google Scholar]
- 18.Brady TJ, Jernick SL, Hootman JM, Sniezek JE. Public health interventions for arthritis: expanding the toolbox of evidence-based interventions. J Womens Health (Larchmt) 2009;18:1905–17. doi: 10.1089/jwh.2009.1571. [DOI] [PubMed] [Google Scholar]
- 19.Kelley GA, Kelley KS, Hootman JM, Jones DL. Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res (Hoboken) 2011;63:79–93. doi: 10.1002/acr.20347. [DOI] [PubMed] [Google Scholar]
- 20.White DK, Tudor-Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res (Hoboken) 2014;66:1328–36. doi: 10.1002/acr.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callahan LF, Shreffler JH, Altpeter M, Schoster B, Hootman J, Houenou LO, et al. Evaluation of group and self-directed formats of the Arthritis Foundation’s Walk With Ease program. Arthritis Care Res (Hoboken) 2011;63:1098–107. doi: 10.1002/acr.20490. [DOI] [PubMed] [Google Scholar]
- 22.Deal CL, Hooker R, Harrington T, Birnbaum N, Hogan P, Bouchery E, et al. The United States rheumatology workforce: supply and demand, 2005–2025. Arthritis Rheum. 2007;56:722–9. doi: 10.1002/art.22437. [DOI] [PubMed] [Google Scholar]
- 23.American College of Rheumatology Committee on Rheumatology Training and Workforce Issues. Regional distribution of adult rheumatologists. Arthritis Rheum. 2013;65:3017–25. doi: 10.1002/art.38167. [DOI] [PubMed] [Google Scholar]
- 24.Fehring TK, Odum SM, Troyer JL, Iorio R, Kurtz SM, Lau EC. Joint replacement access in 2016: a supply side crisis. J Arthroplasty. 2010;25:1175–81. doi: 10.1016/j.arth.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 25.Solomon DH, Bitton A, Fraenkel L, Brown E, Tsao P, Katz JN. Roles of nurse practitioners and physician assistants in rheumatology practices in the US. Arthritis Care Res (Hoboken) 2014;66:1108–13. doi: 10.1002/acr.22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hooker RS. The extension of rheumatology services with physician assistants and nurse practitioners. Best Pract Res Clin Rheumatol. 2008;22:523–33. doi: 10.1016/j.berh.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Larsson I, Fridlund B, Arvidsson B, Teleman A, Bergman S. Randomized controlled trial of nurse-led rheumatology clinic for monitoring biological therapy. J Adv Nurs. 2014;70:164–75. doi: 10.1111/jan.12183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dougados M, Soubrier M, Perrodeau E, Gossec L, Fayet F, Gilson M, et al. Impact of nurse-led programme on comorbidity management and impact of patient self-assessment of disease activity on the management of rheumatoid arthritis: results of a prospective, multicenter, randomized, controlled trial (COMEDRA) Ann Rheum Dis. 2015;74:1725–33. doi: 10.1136/annrheumdis-2013-204733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katz SJ, Yacyshyn EA. Attracting internal medicine trainees to rheumatology: where and when programs should focus efforts. J Rheumatol. 2009;36:2802–5. doi: 10.3899/jrheum.081200. [DOI] [PubMed] [Google Scholar]
- 30.Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:507–15. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 31.Qin J, Theis KA, Barbour KE, Helmick CG, Baker NA, Brady TJ. Impact of arthritis and multiple chronic conditions on selected life domains: United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:578–82. [PMC free article] [PubMed] [Google Scholar]