Abstract
Background Inpatient portals are an emerging technology that can facilitate collaborative interactions between patients and care teams, but little is known about how organizations attempt to implement and facilitate inpatient portal use for their providers.
Methods We held in-person, semistructured interviews with care team members and information technology (IT) staff and conducted rigorous thematic analysis of transcripts.
Results Interviews with 220 care team members and 4 IT staff identified 3 new areas of training needed to optimize inpatient portal implementation and use that extend beyond training to use other technologies: (1) teaching staff to train patients about tool use; (2) training about how to promote tool use to patients; and (3) training about optimal use of secure messaging.
Discussion Our findings show that inpatient portals are implemented within a collaborative multistakeholder context. Training efforts must consider the importance of this collaborative context to help providers learn to both incorporate the technology into their workflow and assist patients with portal use.
Keywords: patient portals, hospitalization, medical informatics, implementation, training
Background and Significance
Inpatient portals are a new health information technology (HIT) that provides hospitalized patients and their families/caregivers access to information from their electronic health record (EHR) that is tailored to the hospital setting. While study of inpatient portals is increasing, with scholars currently proposing both future research questions 1 and evaluation frameworks, 2 3 previously published studies have only described inpatient portal use on a small scale 4 5 6 or for specific settings or populations such as intensive care, cancer, or elderly patients. 5 7 8 These small-scale studies focus primarily on tool usability, 6 7 8 9 use rates for specific features, 4 10 11 12 13 and patient satisfaction, 4 6 7 8 13 and thus far have not focused on how organizations attempt to implement and facilitate inpatient portal use for their providers. 14
The inpatient portal differs from other HIT implementations, such as EHRs and infusion pumps, because of its potential for collaborative use. Staff must teach patients how to use portal features and actively encourage use. Further, patient-facing elements of the portal may generate new questions for the care team including questions about using the tool itself as well as questions that arise when patients can view their results and medication schedules. These elements thus represent a new type of patient/care team interaction that is introduced when the tool is implemented.
Objectives
This case report focuses on the large-scale implementation of an inpatient portal across a five-hospital academic medical center (AMC). Results of a survey of AMC providers conducted immediately postimplementation showed that despite deploying a robust training approach similar to that used in previous HIT implementations, a majority of care team members reported a need for more training and many expressed frustration about their ability to use the tool to its full capacity. 15 We hypothesized that the new collaborative elements of this inpatient portal might have contributed to respondents' frustration and designed a qualitative study to explore our hypothesis and improve understanding of this new HIT. Our research questions were: What are the perceptions of providers and staff related to the collaborative capabilities of this tool? And what are the training implications for HIT with collaborative elements?
Case Description
Our case site is a five-hospital AMC in a large Midwestern city that cares for over 1.5 million people each year and employs roughly 10,000 individuals. This AMC currently offers hospitalized patients an Android tablet with access to Epic's MyChart Bedside (MCB)—an inpatient portal tethered to a patient's EHR. The MCB application includes the patient's daily schedule, laboratory/test results, current medications, secure messaging with the care team, a place to take notes, access to educational materials, and the ability to order meals. Implementation of MCB began in August of 2016 using a phased rollout across the hospitals.
The staff education plan for MCB implementation included the selection and training of a staff champion, termed a “superuser.” Superusers were typically unit care associates or nurses who were released from work duties to complete additional off-unit training around MCB use. Superusers were then expected to serve as resources on the unit during the MCB rollout and beyond. Information technology (IT) staff also conducted on-unit trainings sessions to inform staff about the new MCB tool and its features including how to provision the tablet with MCB installed to patients and how to use the provider-facing elements of the tool. All staff also had access to MCB education and tip sheets via the employee Intranet. The rolling implementation across the AMC also included the deployment of IT staff to each unit during the initial period of MCB use so that they could serve as additional resources.
The process of provisioning a tablet to patients was standardized across the AMC to include the following steps: (1) care team member evauates patient eligibility and appropriateness for tablet use (i.e., over 18 years of age, speaks English, not a prisoner, capable of using the technology); (2) care team member offers the tablet to the patient; and (3) care team member electronically assigns a specific tablet to a patient and guides the patient though the steps of creating a secure personal identification number and starting the MCB tutorial (a 10-minute embedded tutorial). Prior to MCB implementation, the IT team developed a script for care team members to use when offering tablets to patients. This script addressed features of MCB as well as what to expect from the health system regarding MCB use. The provisioning process was not standardized across the hospital leading to significant variation across units with respect to which care team member became responsible for provisioning the tablet (i.e., nurse, patient care assistant [PCA], unit clerk, or a combination).
Methods
We conducted in-person interviews with 220 care team members across the AMC. Interviewees included nursing staff ( N = 137), nurse managers ( N = 20), PCAs ( N = 51), and unit clerical assistants (UCAs) ( N = 12). Interviews were conducted across 22 units, and included care team members who cared for a wide variety patients with different levels of acuity. Due to the initial rolling implementation of MCB across all hospital units during 2016 and 2017, interviewees were at various stages of implementation in their units, but all were within 9 months of the unit going live. A semistructured interview guide was used to assess perceptions of changes in workflow, organizational culture, and patient interaction attributable to the introduction of the inpatient portal technology. Interviews were conducted in person by study investigators throughout the five hospitals. Each interview lasted approximately 10 minutes and was digitally audio-recorded in a deidentified format.
In-person interviews were also conducted with four AMC HIT staff involved in the technology implementation. Three interviewees were members of the study site's clinical applications team that supported the MCB application and included the team manager and two senior systems consultants. The director responsible for EHR training and optimization was also interviewed. These interviews were similarly semistructured using an interview guide that focused on the staff training process, barriers and facilitators during the technology roll-out process, comparisons to other technology rollouts, and lessons learned. Please see the Supplementary Material (available in the online version) for a copy of the study Interview Guide.
As one piece of a larger study, this article reports specifically on the collaborative nature of this technology and implications for training. Rigorous qualitative methods—including double coding each transcript with the coding team reaching consensus on disagreement—were used to define broad categories of findings common across all provider and HIT team member interviews, such as “interpersonal technology,” “training,” and “impact on provider.” The goal of this process was to build a grounded theory around inpatient portal implementation and training, as outlined by Glaser and Strauss. 16 Then, following the methods of thematic analysis from Constas, 17 these codes were examined further and categorized into commonly occurring subthemes related to training that we present in detail below. The Atlas.ti (version 6.0) qualitative data analysis software was used to support this coding process. 18
Results
We found three new areas of training perceived necessary for inpatient portal implementation and use that were noted to differ from implementations of other HIT: (1) need for an expanded training to include teaching staff to train patients on the use of the tool; (2) need for training on how to promote tool use with patients; and (3) need for training to optimize the use of secure messaging. In Table 1 , we summarize findings about similarities and differences in training needs associated with the inpatient portal compared with other HIT implementations, using the organizing framework of best practices in EHR implementation training presented by McAlearney et al. 19 Below, we discuss these three new areas for training in greater detail, providing additional supportive quotes in Table 2 .
Table 1. Similarities and differences between training needs associated with the inpatient portal compared with other health information technologies.
| Best practices in EHR implementation training 14 | Similarities to prior HIT implementations | Identified training needs different from prior HIT implementations |
|---|---|---|
| Assess users' skills and training needs | Elements of training include tool features, trouble-shooting | Expand focus of training to include how staff should train patients to use the tool |
| Match training to users' needs | Staff needs the opportunity to practice with the tool itself | Specific training needed on the collaborative potential of the tool |
| Use multiple training approaches | Computer-based learning modules, one-on-one, on-unit trainers | Allow providers to engage with the tool from the patient perspective |
| Provide training support throughout implementation | On-unit champions with time dedicated to the project | Provide focused support to staff on how to encourage/market patient use of the tool |
| Retrain and optimize | Additional training, re-training about the provider-facing elements of the tool to optimize use | Ensure retraining includes the patient-facing and collaborative elements of the tool |
Abbreviations: EHR, electronic health record; HIT, health information technologies.
Table 2. Training needed to optimize collaborative use of an inpatient portal.
| Training needs | Representative verbatim quotes |
|---|---|
| Focus on teaching staff how to train patients | |
| “ When this started, I was never trained on the tablets. So me being the person to go into and talk to the patient on how to use them, I didn't feel was something I should do. Because I didn't know how to use them myself, so I didn't even know how to navigate them through it.” | |
| “I feel like staff need better education as well to be able to feel comfortable teaching how to, you know, go to the education portion and look at the lab results and just stuff like that.” | |
| Training to promote patient buy-in | |
| “ I think our patients down here, they tend to be long-term patients, the ones that actually stay here and would utilize them [the tablets]. And I just feel we haven't been the greatest at getting the information out regarding MyChart Bedside.” | |
| “We [nurses provisioning the tablets] just say ‘It's very user friendly’, a lot of people of all age ranges and all conditions here, some like it some don't but it's not that hard to use.” | |
| Training to optimize use of secure messaging | |
| Lack of care team buy-in regarding the need for secure messaging | “Usually if they have questions about the results, they just call out and ask. They never refer to MyChart Bedside with it.” |
| “To be honest, we have a small unit. If we are full, what is it, 16 patients? It's only this hallway, so I feel like just hitting the call light is better than the message feature.” | |
| “Yeah, I think for me that's kind of confusing too, because they can use their call light, they can use that so you have to check different avenues for where my patients might be asking for things.” | |
| “We're in our patients' rooms so much that it's…hardly gets used here. Because our patients aren't allowed to get up out of the bed by themselves…. We're always in there.” | |
| Infrequent use of secure messaging | “Since we've rolled it out in October we've probably had six messages sent to providers. And those are never seen or looked at until I've had to track people down…because it's seen so rarely.” |
| “My guess is the messaging is probably our…I haven't even pushed that. I'm pushing to just get tablets to be provisioned and get them to function. So I think that's a down the line goal like I kind of brought that up. We have that monthly MyChart Bedside, we have a panel that we go to, and I brought that up. But it doesn't seem like a lot of people are quite there yet as far as that communication.” | |
| “You know like when I go on, I'll see a couple. But usually it's silly stuff, like, ‘Hi, stop by and see me later.’ Or, you know… it's like really insignificant and stuff.” | |
| “Nurses don't realize it's there, and sometimes patients don't…I mean patients may send it but don't… You know. I think they just use their call light for pain. We try to implement like if they're going to ask a question about something that's not pressing, so if it's a pain need, nurses aren't going to look in their chart. Most of the time they're going to wait for their call light to go in and address that.” | |
| Lack of knowledge about work flow related to secure messages | “I have seen a few on there but I told them, I said ‘If you need something, call me.’ Because sometimes I miss it. I don't see them because I'm not used to looking for them. And I know the doctors are not answering them because I looked at one the other day that was three days old that was sent to a doctor and there was no response whatsoever to it.” |
| “And then, I can't really remember too much. You read the note and then you have different ways you can reply I guess.” | |
| “I've only seen it one time. I just, that's it…it was, I think it was like two days old. So I think the question's kind of moot.” | |
Focus on Teaching Staff How to Train Patients
One new area of training mentioned by providers and IT staff was the need to train staff to both use the technology themselves and to show patients how to use it. While the IT team provided training for care team members, training patients to use the inpatient portal fell on the nursing staff. As one IT staff member noted: “ So the concept of getting our staff comfortable with it first and to have a level of understanding to be able to then kind of teach patients was challenging at first .” This is a new element of HIT implementation, as highlighted by one IT staff member: “ [in other implementations] they don't have to worry about ‘Oh, now my patient is going to do this too.’ So it is scary for them .”
Staff concerns about training patients to use the portal in the inpatient setting paralleled IT team perceptions. One provider noted, “ It's new to me too so… I think it's a learning process for both of us .” As another provider explained, “ The first couple of months I had no idea how to use it, so to try to teach my patients how to use it was difficult. So then I just didn't do it. Here in the last month and a half, two months, I've tried to learn a little bit more about it. That has helped me teach my patients about it .”
Training to Promote Patient Buy-In
Another new training need commonly mentioned by both providers and IT staff involved teaching providers how to promote the portal itself. As one IT staff member explained, “ it has kind of a marketing slant to it…. It is something that we are trying to get our patients to do and you need to help .” Embracing this need, one provider explained how she helps to encourage use: “ I've used MyChart myself for my stuff out in the real world. So I try to sell it in that way .” In contrast, another interviewee noted she does not spend much time promoting use: “ I haven't told them [patients] a lot about it. … I don't really go into great detail honestly about a lot of the stuff on there. I just give very brief instructions on what is available on there and usually I say, ‘Go through it, you know, tool around through there. If you have any questions, concerns, let me know .’”
Training to Optimize Use of Secure Messaging
Finally, because MCB encourages collaborative work between the patient and care team through secure messaging, a third need for training involved building a use case by explaining the benefits of this collaborative communication feature and building its use into provider workflows. The MCB application sends an electronic message from a patient to all members of the care team. According to the AMC policy, the unit clerk should review messages every 4 hours and nurses are expected to add the message notification field into their electronic patient chart homepage. Our interviews found that the workflow after receiving the initial message varied by unit. In some units, the unit clerk was responsible for triaging secure messages; in others, this responsibility was assigned to a staff nurse. Thus, while the work process for dealing with secure messages consistently starts with an electronic message that is sent to all members of the care team, there is no standardized workflow for who should respond to that patient's message nor about how that response should occur (i.e., response via secure message vs. in-person communication with the patient).
When asked about the secure messaging feature, the great majority of providers interviewed had limited experience and did not appreciate its potential. As one provider summarized, “ So you mean the communication part? The messaging… that's probably our weakest area. Like people just don't know how to use it .”
Three interrelated subthemes emerged about secure messaging indicating specific needs for new training about this collaborative feature: lack of nursing staff buy-in about secure messaging; a low rate of secure message use among patients; and confusion about the care team process for handling secure messages.
First, some providers felt that the secure message feature was unnecessary because existing levels of in person contact between the patient and care team were frequent and sufficient. Many interviewees specifically noted that patients could utilize their call light or call the nurse if they had an immediate need. As one nurse noted, “ we are all available on the unit, so if you need something, call me. If you have a question, don't send it through that thing [secure message] because you're probably not going to get an answer .”
Another subtheme involved the low rate of secure message use among patients, highlighting the need for training to encourage patient use of secure messaging. At these interviews that occurred 5 to 10 months postimplementation most providers reported they had received very few messages and had difficulty recalling how to view them. One provider explained, “ we don't get a lot of messages. I think because we're going to see our patients so much and we're in and out .”
Finally, related to the low volume of messages was a third subtheme indicating little knowledge about workflow related to secure messages. This frequently discussed topic was summarized by a floor nurse: “ And honestly, if they sent a message, I wouldn't [laughing] I don't know, I think the UCA [Unit Clerk Associate] is supposed to… I don't even know about the messages .”
Discussion
Using a qualitative approach, we found evidence that successful implementation of an inpatient portal requires training of frontline staff and nurse managers in a manner that is different from other HIT implementations. As we present in Table 1 , these training components are not included in the current best practices for training in EHRs. 19 Optimal use of an inpatient portal requires both patients and care team members to understand the value of the tool and to collaborate in using it. Therefore, training must include new capabilities such as how to train patients about tool use and teaching both staff and patients about the opportunities for bidirectional communication through secure messaging.
We propose that understanding of the opportunity for collaboration provided by inpatient portals can be improved by considering the lens of a sociotechnical model of HIT use and evaluation, such as that presented by the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 framework. 20 In prior work, we have suggested that SEIPS 2.0, in highlighting the importance of collaborative patient/provider work, can be used as a logic model that places patients at the center of a multistakeholder context within which inpatient portals are being implemented 3 (see Fig. 1 for our modified SEIPS 2.0 framework). Sittig and Singh propose a slightly different sociotechnical model for patient portal implementation that places more focus on the HIT elements of the tool including the hardware, software, clinical content, and user interface. 21 While this model fills an important role when considering usability studies, we feel that the SEIPS 2.0 model places a greater emphasis on the collaborative work between care team members and patients in this context and positions this collaboration as a factor necessary for successful implementation and use of the tool.
Fig. 1.
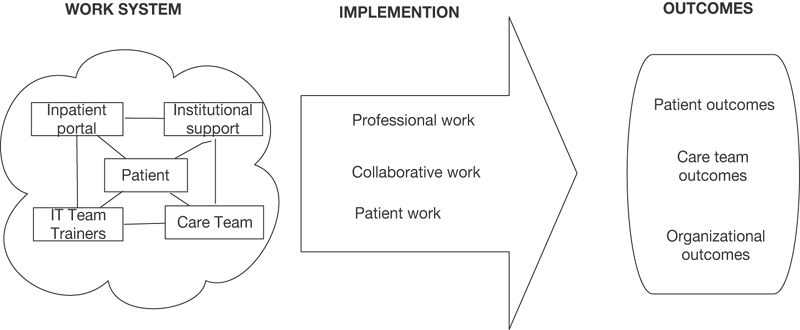
Adapted Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 model for collaborative inpatient portal work. 2
Limitations and Future Directions
Our study has several limitations that may limit the generalizability of these findings including that it was conducted as a single site case study in an AMC. Nonteaching for-profit health systems may have different staffing models and thus experience issues not identified in this study. Yet, while research on inpatient portal technology is increasing, there is little published research on a full-scale implementation across a multihospital medical center. Future research should continue to study implementation from the provider perspective, addressing the themes explored here as well as examining how they may change 1-year postimplementation and beyond. Another limitation of this study is our reliance on provider interviews. Future research would benefit from adding the perspective of patients, especially given the collaborative nature of this tool.
Conclusion
Our study highlights the concerns of providers related to the need to learn how to use the technology themselves while also helping patients with use, and concerns about incorporating a new information component to their workflow when inpatient secure messaging is introduced. Expanded training should allow providers to engage with the tool from the perspective of patients in addition to teaching both care team members and patients about the provider-facing components to fully support optimal collaborative use. It would be particularly effective if these training elements were not simply computer-based learning modules, but were designed as hands-on nursing competencies involving demonstration of tablet and MCB feature use. Further, as many of the providers we interviewed did not fully understand the potential benefits of the secure messaging feature and therefore did not encourage patients to use it, enhanced training would ideally extend beyond the “how” of provider-facing elements of the tool to address the “why” of using collaborative features such as secure messaging. These elements of enhanced training would be best delivered in staff meetings or as short messages in morning unit huddles, with the presentation of a use case for secure messaging as well as permitting sufficient time for questions and discussion.
Clinical Relevance Statement
This study has important implications for administration and management at health systems considering implementation of an inpatient portal, something that is rapidly increasing in popularity and reach. Health systems traditionally focus on training staff on the technical aspects of new technologies, but our results indicate that for new collaborative technologies to be successfully incorporated into care team workflow training initiatives must also consider how the technology may change patient/staff interactions and develop approaches to address these issues.
Multiple Choice Question
When implementing an inpatient portal that includes secure messaging between care team members and patients, which of the following should be included in frontline staff training?
Allow care team members to engage with the tool from the perspective of the patient.
Inform care team members that this is now the most effective way to communicate with patients and that the health system will be using it exclusively.
Provide staff with a training manual to read during breaks.
Frontline staff will not be using the tool as patients will be using it so they do not need training about the secure message function.
Correct Answer: The correct answer is option a. Using a qualitative approach, we found evidence that successful implementation of an inpatient portal requires training of frontline staff and nurse managers in a manner that is different from other HIT implementations. 19 Specifically, we found that expanded training should be provided that allows providers to engage with the tool from the perspective of patients, in addition to teaching care team members about the provider-facing components of the tool to fully support optimal collaborative use. These training components are not included in the current best practices for EHR training and should be a new consideration for learning to use and incorporate type of collaborative tool into clinical care.
Acknowledgments
The authors wish to thank Lindsey Sova and Alice Gaughan, both affiliated with the authors' organization, for their assistance with this project, as well as other research team members who helped with data collection. We also thank all of the care team members and staff associated with our study organization for their participation in this study.
Funding Statement
Funding This research was supported by grants from the Agency for Healthcare Research and Quality [Grant# P30HS024379, Grant# R01HS024091, and Grant #R21HS024767]. The conduct of this research was reviewed and approved by the Institutional Review Board of the authors.
Conflict of Interest None.
Protection of Human and Animal Subjects
This study protocol was approved by the Biomedical Institutional Review Board affiliated with the authors' institution.
Supplementary Material
References
- 1.Collins S, Dykes P, Bates D W et al. An informatics research agenda to support patient and family empowerment and engagement in care and recovery during and after hospitalization. J Am Med Informat Assoc. 2018;25(02):206–209. doi: 10.1093/jamia/ocx054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins S A, Rozenblum R, Leung W Yet al. Acute care patient portals: a qualitative study of stakeholder perspectives on current practices J Am Med Inform Assoc 201724(e1):e9–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker D M, Hefner J L, Sieck C J, Huerta T R, McAlearney A S. Atlanta, GA: Conference Presentation; 2017. Framework for Evaluating Inpatient Portals: A Multi-Stakeholder Perspective. Academy of Management. [Google Scholar]
- 4.Kelly M M, Hoonakker P L, Dean S M. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2017;24(01):153–161. doi: 10.1093/jamia/ocw070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masterson Creber R, Prey J, Ryan B et al. Engaging hospitalized patients in clinical care: study protocol for a pragmatic randomized controlled trial. Contemp Clin Trials. 2016;47:165–171. doi: 10.1016/j.cct.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greysen S R, Magan Mendoza Y, Rosenthal J et al. Using tablet computers to increase patient engagement with electronic personal health records: protocol for a prospective, randomized interventional study. JMIR Res Protoc. 2016;5(03):e176. doi: 10.2196/resprot.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dykes P C, Stade D, Chang F et al. Participatory design and development of a patient-centered toolkit to engage hospitalized patients and care partners in their plan of care. AMIA Annu Symp Proc. 2014;2014:486–495. [PMC free article] [PubMed] [Google Scholar]
- 8.Britto M T, Jimison H B, Munafo J K, Wissman J, Rogers M L, Hersh W. Usability testing finds problems for novice users of pediatric portals. J Am Med Inform Assoc. 2009;16(05):660–669. doi: 10.1197/jamia.M3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yen P-Y, McAlearney A S, Sieck C J, Hefner J L, Huerta T R. Health information technology (HIT) adaptation: refocusing on the journey to successful HIT implementation. JMIR Med Inform. 2017;5(03):e28. doi: 10.2196/medinform.7476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dalal A K, Dykes P C, Collins S et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc. 2016;23(01):80–87. doi: 10.1093/jamia/ocv093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis S E, Osborn C Y, Kripalani S, Goggins K M, Jackson G P. Health literacy, education levels, and patient portal usage during hospitalizations. AMIA Annu Symp Proc. 2015;2015:1871–1880. [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson J R, Davis S E, Cronin R M, Jackson G P. Use of a patient portal during hospital admissions to surgical services. AMIA Annu Symp Proc. 2017;2016:1967–1976. [PMC free article] [PubMed] [Google Scholar]
- 13.Winstanley E L, Burtchin M, Zhang Y et al. Inpatient experiences with MyChart Bedside. Telemed J E Health. 2017;23(08):691–693. doi: 10.1089/tmj.2016.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly M M, Coller R J, Hoonakker P L. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(06):405–412. doi: 10.12788/jhm.2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hefner J L, Sieck C J, Walker D M, Huerta T R, McAlearney A S. System-wide inpatient portal implementation: survey of health care team perceptions. JMIR Med Inform. 2017;5(03):e31. doi: 10.2196/medinform.7707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glaser B G, Strauss A L. Piscataway, NJ: Transaction Publishers; 2009. The Discovery of Grounded Theory: Strategies for Qualitative Research. [Google Scholar]
- 17.Constas M A. Qualitative analysis as a public event: the documentation of category development procedures. Am Educ Res J. 1992;29(02):253–266. [Google Scholar]
- 18.Scientific Software Development. Atlas.ti. Berlin: Scientific Software Development; 2013
- 19.McAlearney A S, Robbins J, Kowalczyk N, Chisolm D J, Song P H. The role of cognitive and learning theories in supporting successful EHR system implementation training: a qualitative study. Med Care Res Rev. 2012;69(03):294–315. doi: 10.1177/1077558711436348. [DOI] [PubMed] [Google Scholar]
- 20.Asan O, Holden R J, Flynn K E, Yang Y, Azam L, Scanlon M C. Provider use of a novel EHR display in the pediatric intensive care unit. Large customizable interactive monitor (LCIM) Appl Clin Inform. 2016;7(03):682–692. doi: 10.4338/ACI-2016-02-RA-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sittig D F, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19 03:i68–i74. doi: 10.1136/qshc.2010.042085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


