Abstract
Objective
To evaluate the effectiveness of an educational video explaining aneuploidy testing.
Methods
This was a randomized controlled trial of women with singleton pregnancies having aneuploidy testing at <14 weeks of gestation from 9/2016–3/2017 at our prenatal ultrasound center. We developed an educational video on aneuploidy testing. Participants, stratified by age < or ≥35 years at estimated delivery date, were randomized to either view or not view the video before their ultrasound. Participants ≥35 years also met with a genetic counselor at the ultrasound appointment. All participants completed a survey assessing knowledge of genetic testing (score of 0 to 15) at baseline and after the appointment. The primary outcome was change in knowledge score after the intervention. A sample size of 23 per group (n=92) was planned for a total of 46 women <35 years of age and 46 women aged ≥35 years. Data are presented as median (interquartile range).
Results
Of 104 eligible women who were approached, 92 were randomized.. Forty women aged <35 years and 41 women aged ≥35 years completed the study. Baseline characteristics were similar across groups. In women <35, the video group had a significant improvement in knowledge score [+2.0 (1.0–5.0)] compared to the control group [0 (−1.0–1.0); P=.01] and reported better understanding of the information compared to the control group (P<.001), with no change in patient satisfaction (P=.25). In women ≥35, change in knowledge score was similar for the video and control groups (P=.98) with no difference in self-reported understanding (P=.49) or patient satisfaction (P=.30).
Conclusion
A patient-centered educational video explaining aneuploidy testing options improved knowledge and self-reported understanding of the information in women <35 years, with no change in patient satisfaction. No difference was seen for women ≥35, likely due to genetic counseling provided to these women.
Introduction
Over the last decade, options for prenatal genetic testing have advanced and expanded. Offering screening or diagnostic testing for aneuploidy is recommended for all pregnant women1 and is typically performed at the first obstetric visit. However, counseling regarding the available testing options is complex and requires detailed patient education; time available to perform this education may not be sufficient since many other topics also are addressed at the initial prenatal encounter. Studies have shown that patient knowledge regarding aneuploidy testing, including non-invasive prenatal testing (NIPT), is limited2–7. In a recent study, only 27% of women understood that a normal NIPT result did not assure a healthy baby7. In a survey of 258 obstetricians, 82.6% reported that lack of time was a barrier in counseling patients about NIPT8.
The objectives of our study were to develop and test the effectiveness of a pre-visit educational video designed to help patients understand available options for prenatal screening and diagnostic testing. We designed the video to provide patients an additional means of receiving and processing information about this complex topic. The video was targeted to a fifth grade educational level. We hypothesized that the video would improve knowledge of aneuploidy testing options, measured by a change in knowledge between baseline and post-appointment tests in women who watched the video compared to those who did not.
Materials and Methods
This was a randomized controlled trial at a single university hospital. The protocol was approved by the institutional review board at Beth Israel Deaconess Medical Center. The educational video (Video 1, available online at http://links.lww.com/xxx), developed and narrated by a maternal-fetal medicine physician (KEO) and a genetic counselor (KFM), was 15 minutes in length and provided information on the basics of genetics; common chromosomal abnormalities; and options for prenatal non-invasive and invasive aneuploidy testing. Aneuploidy testing options reviewed in the video were first-trimester combined screening (nuchal translucency and maternal serum analyte screening), cell-free DNA screening (NIPT), and diagnostic testing with chorionic villus sampling and amniocentesis. The video also described the detection rates, risks, and benefits for each of these options.
Video 1.
Testing for chromosomal abnormalities. This video provides information on the basics of genetics, common chromosomal abnormalities, and options for prenatal noninvasive and invasive aneuploidy testing. Video created by Karen O'Brien, MD, Karen Marchand, MS, and Tom Laws. Used with permission.
Women with a singleton pregnancy presenting to our ultrasound unit for nuchal translucency assessment prior to 14 weeks of gestation, who spoke English and were 18 years of age or older were eligible for enrollment. There were no additional exclusion criteria. All women received some counseling on aneuploidy testing options by their prenatal care provider at the initial prenatal visit, expressed interest in testing, and were subsequently referred for a nuchal translucency ultrasound. Eligible women were approached after checking in for their appointments. All participants provided written informed consent prior to randomization. Computer-generated block randomization, stratified by maternal age at delivery (<35 versus ≥35 years), was used to randomize women to either the video (intervention) or no video (control) group. Randomization allocation was placed in sealed sequentially numbered envelopes labeled by stratification group. One co-investigator (AMM) generated the randomization sequence and performed the randomization allocation. Co-investigators who enrolled participants (BMM, KEO) were blinded to the randomization sequence. The envelopes were opened by the participant after the consent was signed. After randomization, all women completed an initial survey and baseline test to assess knowledge of aneuploidy testing options (Figure 1). Following completion of the survey and test, the intervention group watched the video with headphones in the waiting room prior to their scheduled ultrasound appointment. All women aged ≥35 at delivery had an appointment with a genetic counselor prior to the ultrasound; those randomized to the video group attended this appointment after watching the video. Although the study was designed to blind the genetic counselor to randomization allocation, some of the women aged ≥35 years randomized to the video group inadvertently unblinded themselves to the genetic counselor. If this occurred, the genetic counselor did not change the counseling. All ultrasounds were performed by a sonographer and interpreted by a maternal-fetal medicine physician; the physician, who was blinded to randomization allocation, counseled the patient on the results. Among women choosing first-trimester combined screening, some had serum drawn and analyzed prior to the appointment and received an instant result after their ultrasound; others received a nuchal translucency result only and had serum analytes drawn after the visit. After their ultrasound, all participants completed the same 15-question knowledge test. The time between the baseline and post-appointment tests was approximately 45 minutes in women aged <35 at delivery and 90 minutes in women aged ≥35 at delivery..
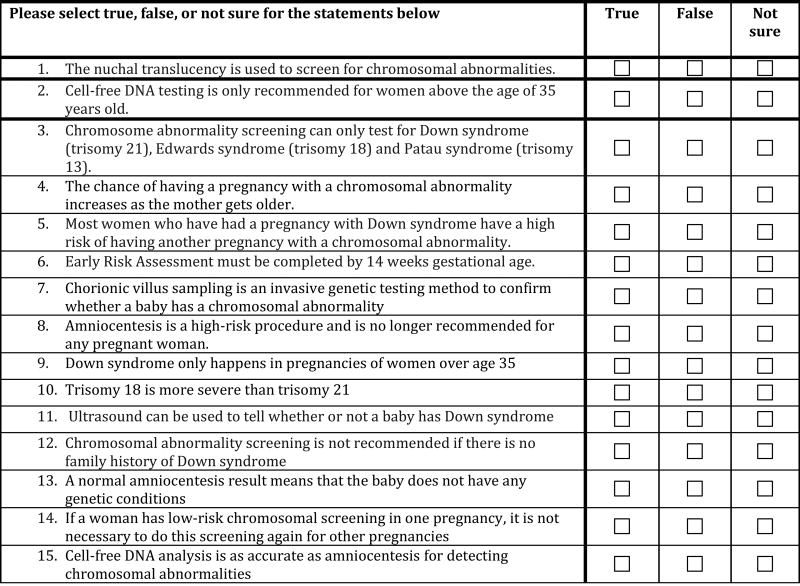
Figure 1.
Knowledge test.
The survey included questions about demographic characteristics and past and current pregnancies. This information was confirmed using the hospital’s electronic medical record. Gestational age was confirmed at the time of ultrasound. Surveys were completed on paper, and data was transferred to a secure electronic database. Two co-investigators (BMM and OHC) reviewed each survey to ensure accuracy of data transfer.
The knowledge test was created by a maternal-fetal medicine physician (KEO) and a genetic counselor (KFM). Each of the 15 questions on the test was answered as either true or false and was worth one point. Missing responses on the knowledge survey were scored as incorrect answers. On the post-appointment test, all participants also were asked to rate how well they understood the information (“How well do you feel you understand the information?; 1=not at all to 5=very well) and their satisfaction (“How satisfied were you with the visit?”; 1=not at all satisfied to 5=very satisfied). Participants randomized to the video group also rated how well the video aided their understanding of testing options and those randomized to the no video group indicated how well a video would have helped their understanding (1=not at all to 5=very much).
The primary outcome was change in knowledge score between the baseline and post-appointment tests. The secondary outcomes were participant self-reported understanding of aneuploidy testing options and patient satisfaction. We compared categorical data with a Chi-square or Fisher’s exact test based on data distribution. Wilcoxon-rank sum tests for two independent samples were used to compare continuous variables between the intervention groups and Wilcoxon signed-rank tests for paired samples were used to compare pre- and post-intervention continuous variables in the same participants. Data was analyzed with SAS 9.4 (SAS Institute Inc., Cary, NC). All tests were two sided and p-values <.05 were considered statistically significant.
A prior study at our institution found a mean knowledge score of 70% (±17) after consent among participants planning to undergo sacrocolpopexy9. Thus, we assumed that the intervention group in this study would have a mean post-appointment knowledge score of 10.5 (±3). We also assumed that a 20% absolute increase in the mean knowledge score would be clinically meaningful; this translated to a mean baseline knowledge score of 7.5 (±3) for both groups. Thus, we assumed that the mean knowledge score would increase by 3 points in the intervention group and 0 points in the control group. Assuming a two-sided alpha of .05, we needed 17 participants per group in order to have 80% power to detect the specified difference. Accounting for a possible non-normal distribution and the potential for 10% loss to follow up, we aimed to enroll 23 participants per group, for a total of 46 participants <35 years of age and 46 participants ≥35 years.
Results
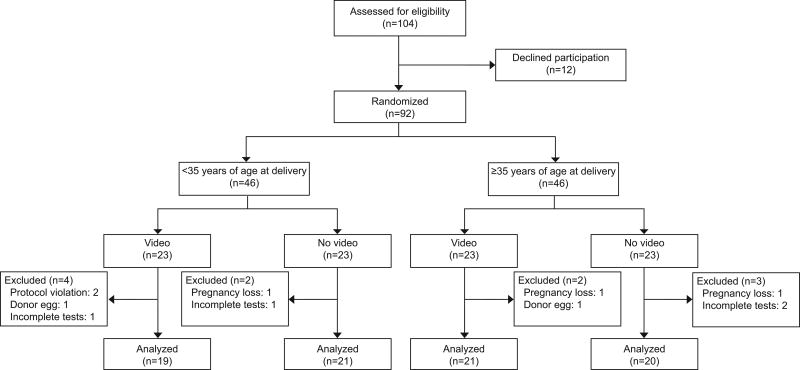
A total of 104 potentially-eligible women were approached from September 2016 through March 2017; 92 women (88%) consented and were randomized, including 46 women aged <35 years at delivery and 46 women aged ≥35 at delivery. We excluded 11 participants after randomization; 2 inadvertently watched the video before completing the baseline test, 2 were determined to have pregnancies conceived from donor oocyte after randomization; 3 had pregnancy losses identified on ultrasound; and 4 did not complete both the baseline and post-appointment tests. Participants who conceived using a donor oocyte were excluded because the genetic counselors tailor counseling based on the age of the donor oocyte, and the use of infertility treatment was not known at the time of randomization. Thus, 81 women were analyzed, including 40 women aged <35 years at delivery and 41 women aged ≥35 at delivery (Figure 2). There were no cases of thickened nuchal translucency, which was defined as ≥3 mm.
Figure 2.
Participant flowchart
Among participants in the <35 groups, baseline characteristics were similar in the video and no video groups (Table 1). The majority of women were nulliparous, college-educated, and had not had genetic counseling in the current pregnancy or in a prior pregnancy.
Table 1.
Participant characteristics stratified by randomization group
| Characteristic | <35 years at delivery | ≥35 years at delivery | ||
|---|---|---|---|---|
|
| ||||
| Video (n=19) |
No video (n=21) |
Video (n=21) |
No video (n=20) |
|
|
| ||||
| Age (years) | 30.0 (28.0–32.0) | 31.0 (26.0–32.0) | 35.0 (35.0–37.0) | 36.5 (35.0–38.5) |
|
| ||||
| Race* | ||||
| White | 7 (36.8) | 14 (66.7) | 12 (57.1) | 10 (50.0) |
| Black | 8 (42.1) | 4 (19.0) | 6 (28.6) | 2 (10.0) |
| Other | 8 (42.1) | 5 (23.8) | 3 (14.3) | 8 (40.0) |
|
| ||||
| College degree or higher | 13 (68.4) | 15 (71.4) | 13 (61.9) | 16 (80.0) |
|
| ||||
| Primigravida | 9 (47.4) | 9 (42.9) | 7 (33.3) | 5 (25.0) |
|
| ||||
| Genetic counseling in index pregnancy prior to study enrollment | 3 (15.8) | 4 (19.0) | 3 (14.3) | 2 (10.0) |
|
| ||||
| Genetic counseling in prior pregnancy† | 0 (0.0) | 4 (33.3) | 4 (28.6) | 4 (26.7) |
Data presented as median (interquartile range) or n (%).
Women could choose more than one race; thus, percentages may add to more than 100%
For participants with gravidity >1
The median baseline knowledge score was 6.0 (4.0–8.0) in the video group and 6.0 (5.0–8.0) in the no video group. The video group had a significant improvement in the primary outcome, knowledge score, [+2.0 (1.0–5.0)] compared to the control group [0 (−1.0–1.0); P=.01] (Table 2).
Table 2.
Primary outcome: Change in knowledge scores between baseline and post-appointment knowledge tests
| Video | P* | No video | P* | P† | |
|---|---|---|---|---|---|
| Age <35 years at delivery | |||||
| n=19 | n=21 | ||||
| Baseline | 6.0 (4.0–8.0) | 6.0 (5.0–8.0) | |||
| Post-appointment | 9.0 (7.0–11.0) | 7.0 (5.0–10.0) | |||
| Difference | 2.0 (1.0–5.0) | <.001 | 0.0 (−1.0–1.0) | .35 | .01 |
| Age ≥35 years at delivery | |||||
| n=21 | n=20 | ||||
| Baseline | 7.0 (5.0–8.0) | 8.0 (6.5–10.0) | |||
| Post-appointment | 9.0 (8.0–11.0) | 11.5 (8.5–12.5) | |||
| Difference | 3.0 (0.0–4.0) | .005 | 2.5 (0.0–4.5) | .005 | 0.98 |
Data presented as median (interquartile range)
Compares baseline and post-appointment scores within each group
Compares the difference between the baseline and post-appointment scores across the groups
We then assessed several secondary outcomes. When asked how well they felt they understood the information, the video group reported a better understanding of the information, with a median score of 4.0 (IQR 3.0–5.0) compared to the control group [median score 3.0 (IQR 2.0–3.0), P<.001]. Patient satisfaction scores were similar between the intervention [median score 5.0 (IQR 4.0–5.0)] and control groups [median score 4.0 (IQR 4.0–5.0), P=.25] (Table 3). Women randomized to the video felt that watching the video helped their understanding with a median score of 4.0 (IQR 4.0–5.0). The control group felt that watching a video would have improved their understanding, with a median score of 4.5 (IQR 2.5–5.0).
Table 3.
Secondary outcomes: Self-reported understanding of aneuploidy and aneuploidy testing options, and self-reported patient satisfaction
| Video | No video | P | |
|---|---|---|---|
| Age <35 years at delivery | |||
| n=19 | n=21 | ||
| Self-reported understanding | 4.0 (3.0–5.0) | 3.0 (2.0–3.0) | <.001 |
| Satisfaction | 5.0 (4.0–5.0) | 4.0 (4.0–5.0) | .25 |
| Age ≥35 years at delivery | |||
| n=21 | n=20 | ||
| Self-reported understanding | 4.0 (3.0–5.0) | 4.0 (3.5–4.0) | .49 |
| Satisfaction | 5.0 (4.0–5.0) | 5.0 (4.0–5.0) | .30 |
The majority of women aged <35 years at delivery (78.9% in the video group and 76.2% in the no video group) knew that Down syndrome does not occur only in women ≥35. In contrast, at baseline, few women <35 years (10.5% in the video group and 4.8% in the control group) understood that trisomy 18 is more severe than trisomy 21. The video appeared to improve knowledge of this question, with 68.4% in the video group correctly responding on the post-appointment test compared with 19.0% in the control group. In addition, at baseline, few women (21.1% in the video group and 14.3% in the control group) knew that ultrasound cannot be used to diagnose Down syndrome. Though both groups demonstrated better knowledge regarding this question on the post-appointment survey, the proportions remained relatively low (36.8% and 38.1% in the video and control groups, respectively).
In women ≥35 years at delivery, baseline characteristics were similar between the video and no video groups. In contrast to women <35 years at delivery, the majority of these women were multiparous. However, similar to the women <35 years at delivery, most women were college-educated and had not had genetic counseling in the current pregnancy or in a prior pregnancy.
The median baseline score was 7.0 (5.0–8.0) in the video group and 8.0 (6.5–10.0) in the no video group. Both groups had higher scores on the post-appointment knowledge test, though there was no difference in the median change in score, our primary outcome, between the video group [+3.0 (0.0–4.0)] and control group [+2.5 (0.0–4.5); P=.98] (Table 2).
We also assessed several secondary outcomes. The video group had no change in self-reported understanding of the information [median score 4.0 (IQR 3.0–5.0)] compared to the control group [median score 4.0 (3.5–4.0), P=.49]. Similar to the <35 age group, patient satisfaction scores were similar between the video and control groups in women ≥35 at delivery [median score 5.0 (IQR 4.0–5.0) for both groups, P=.30] (Table 3). Women randomized to the video felt that watching the video helped their understanding; with a median score of 4.0 (IQR 4.0–5.0). The control group felt that watching a video would have improved their understanding, with a median score of 4.0 (IQR 3.0–4.0).
Most women aged ≥35 at delivery (81.0% and 95.0% in the video and control groups, respectively) understood that the chance of a chromosomal abnormality increases with maternal age. Like the women <35, few women aged ≥35 at delivery (14.3% in the video group and 15.0% in the control group) knew that trisomy 18 is more severe than trisomy 21. Both groups demonstrated improvement on the post-appointment survey, with 66.7% in the video group and 75.0% in the control group correctly responding. At baseline, 28.6% of the video group and 50.0% of the control group understood that ultrasound cannot be used to diagnose Down syndrome. These proportions were similar on the post-appointment test, with no improvement in the video group (28.6%) and minimal improvement in the control group (60.0%).
Discussion
We report that in women <age 35 at delivery, a pre-appointment educational audiovisual presentation improved understanding of aneuploidy and available aneuploidy testing options at our tertiary care center. This was measured both objectively, by change in knowledge score on a test taken before and after the appointment, and also subjectively, by participant self-report. In contrast, women aged ≥35 at delivery had no change in knowledge score or self-reported understanding. This likely occurred because genetic counseling was provided to all women in the ≥35 age group. Women who watched the video found it helpful, and those who did not watch the video felt that a video would have helped them understand aneuploidy testing options.
Educational videos have been shown to improve patient knowledge and understanding. Among ICU patients and surrogate decision makers, a video demonstrating cardiopulmonary resuscitation (CPR) and preferences for resuscitation improved knowledge of inpatient CPR terminology and options among those randomized to video plus usual care compared to usual care alone10. In another study, women with a new diagnosis of advanced stage ovarian cancer who were randomized to an educational video discussing cancer information and experiences had improved knowledge compared to a placebo video; however, these women also had an increase in negative learning attitudes and intrusive thoughts consistent with increased distress11.
Educational materials to supplement in-person counseling for aneuploidy testing have been examined in prior studies. Interactive prenatal genetic testing decision aids, designed to assist women with decision making on aneuploidy testing, have been shown to improve patient knowledge12,13 and satisfaction12. Yee et. al. showed that pregnant women randomized to an interactive computer program had improved test scores compared to those receiving standard counseling14. However, this program did not include NIPT as it was designed prior to its availability.
In the United States there is a shortage of clinical genetic counselors, which is anticipated to continue to grow with increased demand for genetic testing15. The results of our study support the potential use of audio-visual counseling aids to educate average-risk women regarding their aneuploidy testing options. Further studies are needed to determine if video-based genetic counseling alone is as effective as in-person genetic counseling.
Our study has several limitations. First, we excluded women in both age groups with early pregnancy loss diagnosed on ultrasound; this was done so that women could leave immediately after the appointment. Second, the knowledge test we developed and tested was not a validated assessment tool; however, it specifically addressed the topics reviewed in the video. Third, baseline knowledge scores were different than what we assumed for the power calculation. We only included women who had already decided to have nuchal translucency ultrasound; therefore, women who declined screening and diagnostic testing may have had different baseline knowledge of these testing options. Additionally, most participants were Caucasian and had at least a college education and all of them spoke English, which may limit generalizability to other populations. Lastly, the study was not designed to assess a difference in participant decisions regarding specific aneuploidy testing options; rather, our goal was to develop and test a video that patients would be able to watch prior to coming to the hospital, which would educate them on their options prior to their visit and save time in provider counseling.
Despite these limitations, our study has several strengths. The randomized design allowed us to minimize confounding, and we stratified by age 35 years in order to account for women who received genetic counseling. Our study adds to the literature by specifically addressing whether an educational video improves knowledge of aneuploidy testing options in obstetric patients. In addition, we had a very high rate of study participation, with 88% of women approached agreeing to participate.
We found that a patient-centered educational video, which we developed to explain the concept of aneuploidy and aneuploidy testing options, improved knowledge and subjective understanding of the information in women aged <35 at delivery, with no change in patient satisfaction. We did not observe a difference in women aged ≥35 at delivery, likely due to genetic counseling provided to these women.
Supplementary Material
Acknowledgments
A Shore Fellowship Grant was obtained through Harvard Medical School to fund this project. This work was conducted with support from Harvard Catalyst: The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102 and financial contributions from Harvard University and its affiliated academic health care centers).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
Presented at the 38th Annual Meeting of the Society for Maternal-Fetal Medicine, January 29–February 3, 2018, Dallas, Texas.
References
- 1.Screening for fetal aneuploidy. Practice Bulletin No. 163. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2016;127:e123–37. doi: 10.1097/AOG.0000000000001406. [DOI] [PubMed] [Google Scholar]
- 2.Rowe HJ, Fisher JR, Quinlivan JA. Are pregnant Australian women well informed about prenatal genetic screening? A systematic investigation using the Multidimensional Measure of Informed Choice. Aust N Z J Obstet Gynaecol. 2006;46(5):433–9. doi: 10.1111/j.1479-828X.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 3.Bryant AS, Norton ME, Nakagawa A, Bishop JT, Pena S, Gregorich SE, et al. Variation in Women’s Understanding of Prenatal Testing. Obstet Gynecol. 2015;125(6):1306–12. doi: 10.1097/AOG.0000000000000843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karagkiouzis T, Sifakis S, Makrithanasis P, Dessypris N, Petridou ET, Kitsiou-Tzeli S, et al. Awareness of prenatal screening for fetal aneuploidy among pregnant women in Greece. In Vivo. 2015;29(1):155–60. [PubMed] [Google Scholar]
- 5.Sheinis M, Bensimon K, Selk A. Patients’ Knowledge of Prenatal Screening for Trisomy 21. J Genet Couns. 2018;27(1):95–103. doi: 10.1007/s10897-017-0126-3. [DOI] [PubMed] [Google Scholar]
- 6.Farrell R, Hawkins A, Barragan D, Hudgins L, Taylor J. Knowledge, understanding and uptake of noninvasive prenatal testing among Latina women. Prenat Diagn. 2015;35(8):748–53. doi: 10.1002/pd.4599. [DOI] [PubMed] [Google Scholar]
- 7.Piechan JL, Hines KA, Koller DL, Stone K, Quaid K, Torres-Martinez W, et al. NIPT and Informed Consent: an Assessment of Patient Understanding of a Negative NIPT Result. J Genet Couns. 2016;25(5):1127–37. doi: 10.1007/s10897-016-9945-x. [DOI] [PubMed] [Google Scholar]
- 8.Farrell RM, Agatisa PK, Mercer MB, Mitchum AG, Coleridge MB. The use of noninvasive prenatal testing in obstetric care: eduational resources, practice patterns, and barriers reported by a national sample of clinicians. Prenat Diagn. 2016;36(6):499–506. doi: 10.1002/pd.4812. [DOI] [PubMed] [Google Scholar]
- 9.Adams SR, Hacker MR, Merport Modest A, Rosenblatt PL, Elkadry EA. Informed Consent for Sacrocolpopexy: Is counseling effective in achieving patient comprehension? Female Pelvic Med Reconstr Surg. 2012;18(6):352–6. doi: 10.1097/SPV.0b013e31827816c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson ME, Krupa A, Hinds RF, Litell JM, Swetz KM, Akhoundi A, et al. A video to improve patient and surrogate understanding of cardiopulmonary resuscitation choices in the ICU: a randomized controlled trial. Crit Care Med. 2015;43(3):621–9. doi: 10.1097/CCM.0000000000000749. [DOI] [PubMed] [Google Scholar]
- 11.Geller MA, Downs LS, Judson PL, Ghebre R, Argenta PA, Carson LF, et al. Learning about ovarian cancer at the time of diagnosis: video versus usual care. Gynecol Oncol. 2010;119(2):370–5. doi: 10.1016/j.ygyno.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 12.Kuppermann M, Norton ME, Gates E, Gregorich SE, Learman LA, Nakagawa S, et al. Computerized prenatal genetic testing decision-assisting tool: a randomized controlled trial. Obstet Gynecol. 2009;113(1):53–63. doi: 10.1097/AOG.0b013e31818e7ec4. [DOI] [PubMed] [Google Scholar]
- 13.Kuppermann M, Pena S, Bishop JT, Nakagawa S, Gregorich SE, Sit A, et al. Effect of enhanced information, values clarification, and removal of financial barriers on use of prenatal genetic testing: a randomized clinical trial. JAMA. 2014;312(12):1210–7. doi: 10.1001/jama.2014.11479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yee LM, Wolf M, Mullen R, Bergeron AR, Cooper Bailey S, Levine R, et al. A randomized trial of a prenatal genetic testing interactive computerized information aid. Prenat Diagn. 2014;34(6):552–7. doi: 10.1002/pd.4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulz CJ. Genetic counselor workforce trends in the United States: 2002 to 2016. Ann Arbor (MI): ProQuest LLC; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.