Abstract
With the development of modern international medicine, the subject of disorders of consciousness (DOCs) has begun to be raised in mainland China. Much progress has been made to date in several specialties related to the management of chronic DOC patients in China. In this article, we briefly review the present status of DOC studies in China, specifically concerning diagnosis, prognosis, therapy, and rehabilitation. The development of DOC-related scientific organizations and activities in China are introduced. Some weaknesses that need improvement are also noted. The current program provides a good foundation for future development.
Keywords: China, Disorders of consciousness, Diagnosis, Therapy
Introduction
Five decades or so ago, several states of disorders of consciousness (DOCs), such as the vegetative state/unresponsive wakefulness syndrome (VS/UWS), minimally-conscious state (MCS), and locked-in syndrome (LIS), were specifically described and gradually named [1–3]. Since then, a long and intense debate has been provoked among clinical scientists, health professionals, and even moral philosophers and lawyers, because there is an apparent dissociation between awareness and wakefulness – two cardinal elements of consciousness. For example, patients in a VS appear to be awake with eye-opening but lack any sign of a working mind dealing with either themselves or the environment, while patients in MCS exhibit signs of awareness with some fluctuating but reproducible behavior while remaining unable to functionally communicate or use objects.
Patients with DOCs face major challenges in diagnosis, prognosis, treatment, and rehabilitation. In the clinic, since it is not always easy to detect meaningful mental activity related to consciousness, the diagnosis of DOCs is currently based on the observed behavior. However, misdiagnosis often occurs because the behavior is frequently temporary and voluntary behaviors are limited in severely brain-damaged patients. For example, one important retrospective clinical study has demonstrated that 40% of patients with a diagnosis of VS may be misdiagnosed, retaining some level of consciousness [4]. In the last few years, as a result of rapid technical developments, several state-of-the-art neuroimaging methods have greatly improved the investigation of consciousness-related neural activity. Researchers have generally agreed that consciousness depends on the integrity of sufficient thalamocortical and intercortical connections [5]. Therefore, evaluating the remaining extent of the structural and functional integrity of the brain by neuroimaging techniques, as well as by some neuromodulation techniques, can provide additional information on the diagnosis, prognosis, and therapeutic interventions in patients with DOCs [5–7].
Since the early stage in the 1990s, the term persistent VS (PVS), as well as other terms related to DOCs such as MCS and LIS, have been gradually introduced into China, and increasing numbers of Chinese investigators have realized the importance of this subject. Now, a Chinese version of the diagnostic criteria for PVS has been proposed, and DOC-related neuroimaging research has been carried out by increasing numbers of Chinese researchers. Complex treatments with traditional Chinese Medicine (TCM) and Western medicine have also been gradually developed. To further accelerate the understanding of DOCs in China, some Chinese scientific organizations and activities have emerged in the last few years. Therefore, the field of DOCs in China has begun to develop a sound momentum.
In this article, we review the present status of DOC studies in China against the background of developments in modern international medicine, specifically concerning diagnosis, prognosis, therapy, and rehabilitation.
Diagnosis and Prognosis
Diagnosis
The diagnosis of DOCs is largely based on behavioral responses to commands. Numerous clinical scales have been developed in Europe and the USA to help assess the levels of wakefulness and awareness before a diagnosis can be confirmed, including the Coma Recovery Scale-Revised (CRS-R) [8], Glasgow Coma Scale [9], Sensory Modality Assessment and Rehabilitation Technique [10], Wessex Head Injury Matrix [11], Reuth DOC Response Assessment [12], Sensory Tool to Assess Responsiveness [13], and Motor Behavior Tool [14]. Among these, the CRS-R is the most widely used standardized tool that includes the diagnostic criteria for coma, VS/UWS, and MCS and is based on the presence or absence of behavioral responses to specific sensory stimuli. It includes six subscales that address auditory, visual, motor, oromotor, communication, and arousal functions, which are summed to yield a total score ranging from 0 to 23. Nevertheless, the diagnosis of VS/UWS and MCS is particularly challenging because the behavioral responses may be very low, inconsistent, and unreliable; for instance in cases where the sensory or cognitive systems are impaired by brain injury [5]. Evidence has shown that the CRS-R should be administered to patients several times over a short period, such as five times a week, in order to avoid misdiagnosis due to fluctuations of arousal [15].
Going back to the history of China, although there was no concept of DOCs in ancient China, TCM has recorded several relevant expositions for diagnosis, such as shenhun (神昏“mental confusion”), hunkui (昏愦“dote”), and hunmi (昏迷“coma”). The Neijing (内经), the earliest Chinese medical classic written during the time of the warring states 2,200 years ago, describes relevant symptoms (Fig. 1). Later, more enriched descriptions can be found in WenbingTiaobian (温病条辨) and LeizhengZhicai (类证治裁). In modern times, according to TCM theory, Xi et al. [16] also classified DOCs into two categories: Shi and Xu syndrome (excess and deficient syndrome), and five subtypes (phlegm and static blood blocking orifices, phlegm heat obstructing lung, wind phlegm blocking orifices, deficiency of Qi and blood, and kidney blight orifices). After the initial diagnostic criteria for PVS were reported by the US Multi-Society Task Force in 1994 [17], the first definition of the diagnostic criteria and scale for PVS in China was developed in 1996 [18]. This scale included six subscales: command following, language, limb movement, eye movement, swallowing, and emotional response [19], and was revised in 2001 and 2011, under the name Chinese Nanjing PVS scale (CNPVSS), with the integrated electroencephalography (EEG) and somatosensory evoked potentials [20]. However, the CNPVSS is not yet widely used. Actually, in Chinese clinical situations, a diagnosis of DOC still mainly relies on scales developed in other countries. For example, Di et al. have completed a Chinese translation of the CRS-R [21]. Other hospitals, like the PLA Army General Hospital, uses the CRS-R translated by themselves. Nowadays, CRS-R is widely recognized as the standard criteria in China.
Fig. 1.
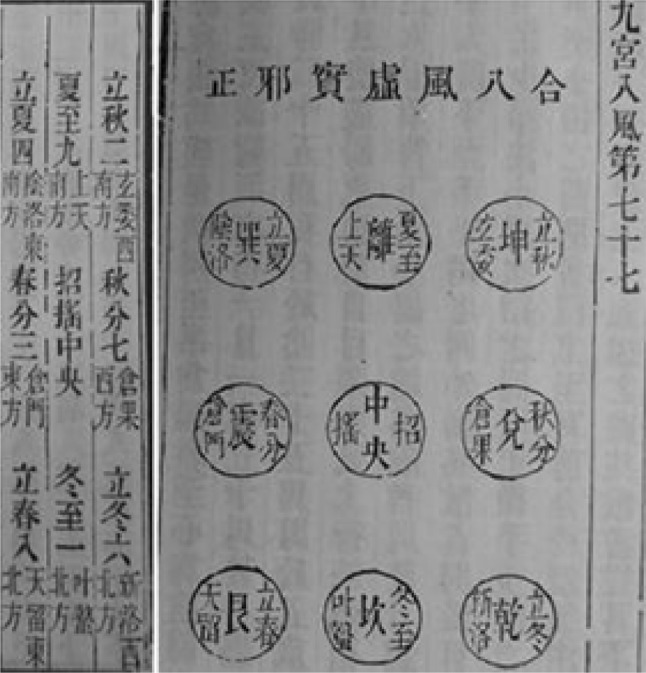
Neijing, Song Dynasty version.
Although bedside behavioral assessments remain the gold standard for the diagnosis of DOCs, neuroimaging and other techniques have the potential to characterize levels of consciousness [22, 23] and automatically differentiate VS/UWS from MCS [24], and these could benefit clinical diagnosis (see reviews [6, 7, 25] for details). Particularly, the Perturbational Complexity Index has been proposed to quantify the complexity of brain responses to transcranial magnetic stimulation (TMS) pulses using EEG, and has proved to be a reliable tool to discriminate various levels of consciousness at an individual level, including VS/UWS, MCS, and LIS [26, 27].
Chinese clinical and research centers have made great efforts to use neuroimaging techniques to assist accurate diagnosis of DOCs. The advances in diagnostic techniques using functional magnetic resonance imaging (fMRI), diffusion MRI (dMRI), and EEG are reviewed below.
fMRI
Qin and colleagues recruited 56 UWS/VS and 29 MCS patients from Huashan Hospital, Fudan University, Shanghai and evaluated the strength of functional connectivity in their salience network (i.e., connectivity between the supragenual anterior cingulate cortex and left anterior insula). They found that the functional connectivity in the salience network was lower in the UWS/VS than in the MCS patients, showing that connectivity in the salience network correlates with behavioral signs of consciousness [28]. Another study, recruited 14 coma, 18 VS/UWS, 27 MCS and 40 controls from Huashan Hospital, and found decreased strength of functional connectivity with loss of consciousness, mainly distributed in the posterior cingulate cortex/precuneus, medial prefrontal cortex, and lateral parietal cortex. However, they did not find any significant difference between VS/UWS and MCS patients [29]. In addition, a study that combined VS/UWS and MCS patients found disrupted functional connectivity between the default mode network and the thalamus [30].
dMRI
dMRI offers a unique opportunity to detect subtle structural damage in white matter, one of characteristics of DOCs. A recent study recruited 30 DOC patients (8 comatose, 8 VS/UWS, and 14 MCS) from Huashan Hospital and compared the dMRI parameters of 48 key white matter regions of interest across groups using analysis of covariance. The authors found the fractional anisotropy of the right corticospinal tract was significantly lower in VS/UWS patients than in MCS patients, and this tract was also significantly correlated with CRS-R scores [31]. Cui and colleagues recruited 21 VS/UWS and 29 MCS from the PLA Army General Hospital in Beijing, and found that the thalamus was represented mainly in the dorsal and posterior portions of the posteromedial cortex, and the white matter tracts connecting these subdivisions to the thalamus had less integrity in VS/UWS patients than in MCS patients and healthy controls [32]. In addition, a study that combined VS/UWS and MCS patients found white matter alterations in connections between the basal ganglia, thalamus, and frontal cortex [33].
EEG
The EEG records electrical activity of the brain by measuring voltage fluctuations resulting from ionic currents within the neuronal populations. Researchers from Xuanwu Hospital quantified the degree of suppression in DOC patients using nonlinear EEG analysis. Specifically, they calculated several nonlinear EEG indices (Lempel-Ziv complexity, approximate entropy, and cross-approximate entropy) and found that the VS/UWS patients had the lowest indices followed by the MCS patients, while the controls had the highest [34]. This research suggested that EEG can be an indicator of the level of consciousness of patients with DOCs. In addition, a brain-computer interface (BCI) combining P300 and steady-state evoked potential responses has been proposed by researchers from South China University of Technology to assess awareness. They found command-following in all four healthy controls, two of 7 DOC patients, and one LIS patient, suggesting that the hybrid BCI system can be used as a supportive bedside tool to detect awareness in patients with DOCs [35].
Prognosis
The prognosis is a fundamental concern for DOC patients, as medical treatment, rehabilitation therapy, and even ethical decisions depend on this information [36]. A DOC patient’s prognosis can be considered according to three dimensions: survival/mortality, recovery of consciousness, and functional recovery [37, 38]. Several pioneering studies have suggested that the etiology, incidence age, and duration of DOCs are important indicators for the prognosis [17]. Specifically, patients with non-traumatic brain injury are expected to have a higher mortality rate and worse functional recovery than those with traumatic brain injury, and young patients are considered more likely to have a favorable outcome than older ones. In addition, several factors are associated with the outcome of DOC patients, including medical complications and nutrition.
Physicians and scientists have been seeking more accurate and objective prognostic markers for DOC patients [39, 40]. Some pilot models have been explored based on features of neurological examination [41–43], abnormalities detected with EEG and evoked potentials [44–46], anatomical and functional changes identified using computed tomography, positron emission tomography (PET), and magnetic resonance imaging (MRI) [47–51], and physiological and biochemical disturbances at both the brain and body levels [52, 53].
In China, researchers have investigated the predictive value of brain imaging for the prognosis of DOC patients, including structural MRI [54] and resting-state fMRI [29, 55]. The study [54] suggested that lesions in the thalamus, tegmentum, and tectum are factors of the greatest adverse prognostic significance in DOC patients after severe traumatic brain injury. Multivariate support vector machine discrimination analysis revealed that the functional connectivity strength patterns from the resting-state fMRI predict whether patients with VS/UWS and coma regain consciousness with an accuracy of 81.25% [29]. Another resting-state fMRI study showed that the functional connectivity between posterior cingulate cortex and left lateral parietal cortex in the default mode network predicts recovery of consciousness [55]. Since DOCs have many different causes, are associated with several neuropathological processes, and differ in severity, any method used alone carries a risk of false prediction [56, 57], so hybrid prognostic models have been proposed [58, 59]. For example, motor response, type of brain injury, EEG reactivity, sleep spindles, and N20 were integrated to predict the recovery of awareness [58]. Recently, a combination of resting-state fMRI and clinical predicators has been reported to discriminate between patients who would later recover consciousness and those who would not with an accuracy of ~90% on multiple independent datasets [59].
Therapy and Rehabilitation
The primary goal of DOC treatment programs is to promote arousal while preventing secondary medical complications. Many different pharmacological and non-pharmacological interventions have been used to date; however, most of the available evidence for their effectiveness is limited by small sample sizes, uncontrolled study designs, or other methodological weaknesses. Consequently, there are no established standards of care to help guide clinical management [60].
Treatment of DOCs has a long history in China. TCM has many kinds of approaches, which are totally different from those of Western medicine, such as many Chinese medicinal herbs and acupuncture physiotherapy. The most famous prescription is AngongNiuhuangWan (安功牛黄丸) invented in the Qin Dynasty recorded in WenbingTiaobian. It is manufactured by Tongrentang (同仁堂), a time-honored pharmaceutical factory in Beijing. AngongNiuhuangWan has saved millions of people with acute and chronic cerebral diseases, including DOCs [61]. Clinically, TCM methods, as well as hyperbaric oxygen, have been carried out as traditional schemes [62], but their efficacy is not good. In recent years, Chinese investigators have done a lot of useful work in tracking the latest international research trends and the application of new technologies. Neuromodulation therapies using electrophysiological techniques have contributed to the latest promising and growing field of therapeutic trials for DOC patients.
Neuromodulation
Deep Brain Stimulation
Deep brain stimulation (DBS) is an invasive technique that requires the surgical implantation of a stimulator. Thalamic and brainstem control of forebrain arousal is not a novel concept. This neurophysiological concept has led to the consideration of thalamic electrical stimulation to promote consciousness in DOC patients [63].
The operation of DBS for DOCs in China started in 2011, carried out by the team of Director He Jianghong. In 2013, they reported 53 patients diagnosed with PVS from July 2011 to December 2012 [64]. After selection, 42 patients were enrolled (27 males and 15 females, mean age 42.9 ± 5.47 years). Patients in the surgical group received DBS (n = 5) or spinal cord stimulation (SCS) (n = 17), while patients in the control group (n = 20) underwent routine rehabilitation. Behavioral assessments were repeatedly performed using CRS-R. Seven patients in the surgical group emerged from PVS to achieve consistent behavioral evidence of consciousness, giving a recovery rate of 35%, while only one from the control group did so, giving a recovery rate of 5.9%. Improvement in behavioral assessments (CRS-R scores) in the surgical group was significantly better than that in the control group. However, no significant difference in CRS-R scores was noted between patients receiving DBS and SCS. So far, 22 DBS operations have been performed by their team.
Spinal Cord Stimulation
Yamamoto et al. have reported SCS for DOCs from 1997 to 2017 [65]. Cervical SCS at 5 Hz caused increased cerebral blood flow (CBF) and induced muscle twitches of the upper extremities, and MCS patients showed remarkable recovery of consciousness and motor function in the upper extremities compared with the lower extremities. This SCS method could be a new neuromodulation and neurorehabilitation technique, and MCS patients may be good candidates for SCS therapy.
According to the literature, the earliest SCS for DOCs in China was carried out by Pei Baifeng in 1991 using dorsal column stimulation to treat one patient with VS [66]. In June 2011, Dong et al. from Tianjin Armed Police Hospital reported one case of VS with high cervical SCS [67], a 46 year-old male who had been unconscious for 2 months after a car accident. The recovery time, EEG, evoked potential, cerebral blood perfusion after cervical SCS were investigated. The patient emerged from coma 2 months after SCS. The EEG gradually returned to normal (rhythm and evoked potential latency improved, and cerebral blood perfusion increased significantly). In 2014, Zhang et al. from Tianjin Huanhu Hospital also reported on a prolonged coma patient with SCS treatment. That was a case of a 30-year-old male who was unconscious for 3 months after a head injury. But there was no systematic behavioral score and objective evaluation index in this report [68]. At present, the largest number of SCS reports in China are from He and colleagues. Since 2011, this team has performed SCS operations for 113 cases. They have also evaluated the different effects of distinct SCS parameters on cerebral activity using neuroimaging and neurophysiological techniques, and optimized the SCS protocol. Bai et al. [69] and Si et al. [70] have evaluated the frequency-specific effects of SCS using EEG and functional near-infrared spectroscopy (fNIRS), respectively. They found that, SCS at 70 Hz and 100 Hz significantly increased hemodynamic responses in the prefrontal cortex [70], and altered the relative power and synchronization in the delta and gamma bands [69]. SCS at 70 Hz also induced significant improvement in the functional connectivity between prefrontal and occipital areas [70] and significantly decreased the bicoherence within the delta band [69]. In addition, Zhang et al. evaluated the influence of the inter-stimulus interval (ISI) of SCS using fNIRS recording. They found that, even with a short stimulus duration (30 s), SCS induced significant cerebral blood volume changes in the prefrontal cortex, and the improvement was more marked with a shorter ISI [71]. This work, for the first time, implied that the ISI is an important factor for SCS.
Median Nerve Stimulation
Median nerve stimulation (MNS) began in China in 1997, by the Second People’s Hospital of Suzhou [72]. They reported 7 cases of PVS treated with low-frequency, pulsed electrotherapy to stimulate the palms of both hands. Before and after treatment, the EEG and brainstem auditory evoked potential were measured. There were 3 cases with unconsciousness recovered while 4 remained unchanged. At present, MNS is also applied in acute-subacute DOCs by Gao and colleagues at Shanghai Huashan Hospital [73]. During 2005–2011, they enrolled a total of 456 patients, of whom 437 completed the treatment. They were randomly divided into control (216 patients receiving routine management) and treatment (221 patients receiving routine management plus right MNS) groups. The treatment lasted for > 2 weeks [73]. CBF imaging and brainstem evoked potentials demonstrated significant improvement in the treatment group. A total of 386 patients were followed up for 6 months postoperatively. The patients in the treatment group showed a higher ratio of regained consciousness and a lower ratio of VS compared with the control group, but the ratio of MCS showed no statistical difference from the other two groups. They have now launched a multicenter randomized-controlled study of right MNS in Asia, covering more than 200 centers, which are being widely carried out in grass-roots hospitals throughout the country.
Transcranial Magnetic Stimulation
TMS provides neuromodulation by the application of rapidly-changing magnetic fields to the scalp via a copper coil connected to a magnetic stimulator. TMS is less invasive and more suitable for routine treatment than DBS, and may prove to be useful for identifying DOC patients who might benefit from a permanently implanted DBS device [74]. A case report has implied that TMS can mediate neurobehavioral gains in coma recovery [75]. Significant improvements have been found in both EEG power spectra and CRS-R scores by repetitive TMS (rTMS) but not peripheral nerve stimulation. Specifically, the patients demonstrated improved arousal, command following, and functional object use.
TMS was first applied in China in 1990. It has been widely used for the treatment of DOCs in the last 10 years. First was the team of Zhou et al. from Xuanwu Hospital. Recently, in a sham-controlled study [76] at the First Affiliated Hospital of Zhejiang University, 20-Hz and sham rTMS were applied over the left primary motor cortex of 5 patients in VS and 5 patients in MCS. The clinical behavior and CBF velocity in the bilateral middle cerebral artery (MCA) were evaluated before and after rTMS. Compared with the VS group, the MCS group exhibited significant increases in peak systolic velocity and mean flow velocity in the left MCA which were temporally related to the rTMS. In cooperation with Li et al. from Beijing Normal University, non-invasive neuromodulation therapies (mainly rTMS and transcranial direct current stimulation [tDCS]) have been carried out by He and colleagues at a relatively large scale of patient group in the Coma Center of the PLA Army General Hospital. They found that treatment with 10-Hz multisession rTMS applied to the left dorsolateral prefrontal cortex was promising for the rehabilitation of DOC patients in their latest study [77].
Vagus Nerve Stimulation
Vagus nerve stimulation is another technique that can modulate functional brain activity. In the past year, it has been piloted in some domestic centers, such as Beijing Rehabilitation Hospital and the PLA Army General Hospital. At present, there are several surgical patients, but no specific report in the literature as there has not yet been enough time. In addition, at the PLA Army General Hospital and in collaboration with the China Academy of Chinese Medical Sciences, a patient with hypoxic-ischemic encephalopathy after cardiac arrest was treated with 4 weeks of transcutaneous auricular vagus nerve stimulation [78]. The CRS-R score was raised from 6 to 13, the clinical manifestations were clearly improved, and repeatable compliance movements appeared. The hemodynamic activity recorded by fMRI was significantly improved.
Transcranial Direct Current Stimulation
TDCS is a form of neurostimulation that delivers a low constant current to an area of the brain using scalp electrodes. Anodal tDCS elicits prolonged increases in cortical excitability and facilitates underlying regional activity, while cathodal tDCS has the opposite effect. Emerging data are available on the use of tDCS for transient improvement in consciousness in patients in MCS but not VS [79]. When used in conjunction with rehabilitation, tDCS may enhance cortical plasticity and recovery in patients with DOCs. Therefore, the ease of use, minimal risk of harm, and portability make tDCS as an additional intervention for the DOC population [80].
Bai et al. reported that, after tDCS modulation, the frontoparietal coherence significantly increased in the theta band and decreased in the gamma band in MCS patients, but no significant changes were found in VS patients [81]. The coherence of responses was significantly correlated with the baseline CRS-R scores. No distinct changes occurred in sham sessions for either the MCS or VS patients [81].
Pharmaceuticals
There are two categories of pharmacological treatment: nervous system depressants (zolpidem, lamotrigine, and baclofen) and stimulants (amantadine, amphetamine, apomorphine, bromocriptine, levodopa, methylphenidate, and pramipexole). The best results are seen with zolpidem, an imidazopyridine or non-benzodiazepine hypnotic that works by selectively stimulating GABAA receptors (BZ-1 or omega 1 subtype). Only amantadine hydrochloride has been convincingly shown to accelerate the pace of recovery in patients with post-traumatic DOCs [82].
But at present, there are few systematic studies of emerging pharmaceuticals in China. AngongNiuhuangWan, invented in the Qin Dynasty as noted earlier, is a famous prescription for the treatment of DOCs. Other pharmaceutical research has mainly focused on Xingnaojing, monosialic ganglioside, and Nalmet. Regular randomized controlled studies are lacking.
A study at Shenzhen People’s Hospital [83] has investigated the effect of zolpidem in promoting the awakening of patients from PVS and has attracted much attention in China. This report showed that, after treatment with zolpidem, the cerebral state index and electromyogram index were significantly increased, and cerebral perfusion in the injured brain regions was significantly improved in all the patients as compared with that before treatment. Awakening was achieved in 3 patients, who were capable of simple communication ~30 min after zolpidem administration, and of simple calculations and lower limb flexion and extension 2 days later.
Hyperbaric Oxygen Treatment
Hyperbaric oxygen treatment (HBOT) has been proposed for patients with DOCs on the hypothesis that improve the perfusion of damaged brain structures and help to protect the penumbra from secondary ischemic damage [84]. The results of a prospective randomized clinical trial and an observational study [85, 86] have provided some evidence that HBOT increases cerebral metabolism and cerebral blood flow while decreasing intracranial pressure and cerebrospinal fluid lactate levels.
HBOT in China began in the 1880s, and Wang et al. [87] reported 168 PVS cases treated with hyperbaric oxygen in 1998, along with a relatively early review of the literature on its efficacy. The Hyperbaric Oxygen Medical Association of the Chinese Medical Association formally approved the establishment of the Brain Resuscitation Research Center on October 16th, 1992. HBOT has been carried out all over the country, and the numbers of patients have increased considerably. However, there are still controversies about the window period and treatment times of HBOT for DOCs, and related studies are rarely found in other countries. To solve this issue, in 2015, a meta-analysis comprehensively evaluated the Chinese literature to systematically review the curative effects and time window of HBOT for PVS [88]. In this study, all articles about hyperbaric oxygen for PVS from January 1990 to December 2013 were retrieved from the China National Knowledge Internet. The search terms yielded 165 articles and 19 were included in the final analysis of treatment efficacy; the treatment group included 939 patients and the control group included 659 patients. Data from articles were pooled and analyzed, and the results showed that the effective rate in the treatment group was 67.51% and in the control group 34.45% [88].
Traditional Chinese Medicine
TCM has a long history of DOC treatment, but there is no scientific literature. In 1994, Zhang et al. [89] reported 19 PVS cases treated with meridian leveling therapy. In February 1996, Wang [90] used TCM as the main method to treat 10 PVS patients. In 2000, Wang et al. [91] used acupuncture as the main method to treat PVS patients after brain injury, and evaluated the effect of strong acupuncture stimulation at 12 Jing-well points. Furthermore, another theoretical and clinical study called “three-dimensional five senses awaking treatment of persistent vegetative state (PVS)” [92] has been shown to have a certain effect on DOC patients.
Comprehensive Rehabilitation
Neurorehabilitation uses standardized assessments to measure the DOC level and focuses on recovery of consciousness, functional communication, and positioning and mobility. Physical and occupational therapy focusing on range of motion, positioning, and splinting are reasonable and low-risk strategies for maximizing the functional outcomes in DOC patients. There is also some evidence from case studies that specialized wheelchairs, positioning devices (e.g., head and foot rests), tilt tables, and weight-bearing activities can aid in the correction of contractures, tonal issues, and promoting increased arousal [4]. While numerous studies have investigated the effectiveness of sensory stimulation and regulation, most were conducted over 20 years ago and none were methodologically sound enough to draw firm conclusions about the effectiveness or ineffectiveness of these treatments [93].
Comprehensive rehabilitation refers to multi-sensory stimulation, body position, limb function training, and musical, light, and electrical as well as somatosensory stimulation. In June 1996, Yang [94] and other TCM doctors combined musical, light, and electrical stimulation to assess and summarize the clinical treatment of 104 PVS cases. Di et al. of Hangzhou Normal University used peripheral sensory stimulation to awaken DOC patients. Di cooperated with Caroline Schnakers in University of Liège, Belgium wrote a review about sensory stimulation program in the book of “Coma and Disorders of Consciousness” [95]. It introduces the theoretical principles underlying sensory stimulation programs for brain-injured patients, and discusses the limitations of this treatment and consider future directions for clinical research.
Conclusions and Perspectives
During the last twenty years of development and effort, the field of DOC studies has progressed greatly in China. On the one hand, following the footsteps of Western medical development, increasing numbers of clinical staff have been trained to conduct thorough behavioral assessments of patients according to the standard diagnostic criteria of DOCs. Comprehensive therapeutic approaches have also been widely applied. From diagnosis to prognosis and to therapeutic approaches, the management of chronic DOC patients in China has become increasingly evidence-based and standardized. On the other hand, Chinese investigators have carried out a lot of useful work in DOC-related neuroimaging research. Some of their studies investigating the predictive value of brain imaging for the prognosis of the DOC patients have been approved by international peers. Furthermore, in 2018, The Chinese Society of Consciousness and Disorders of Consciousness was founded as a branch of the Chinese Neuroscience Society; it aims to promote a multidisciplinary approach to DOC studies in China. At the same time, the Disorders of Consciousness Group was also founded by the Neural Repair Academic Committee of the Chinese Medical Doctor Association. This organization of clinicians aims to accelerate the development of treatment and rehabilitation for DOCs in China. Furthermore, a non-governmental organization, the Consortium of DOCs for Chinese doctors has also been established among > 40 Chinese hospitals. All of the above organizations and consortia will push interdisciplinary studies of DOCs in China.
Although progress is evident, it should be stressed that the status quo of DOC studies in China is still in the fledgling stage. The number of experts on DOCs is still inadequate. There are no unified diagnostic criteria among all centers and diagnostic levels differ significantly. There are no accurate epidemiological data on DOCs in China, either. More than two-thirds of the Chinese population, especially in rural and minority areas, still do not have access to effective management services if they became DOC patients.
In future, it will be necessary to train many more young doctors in the management of DOCs by sending them to other countries to gain advanced skills and to rural areas in China for further practical experience. It is also important to unify the diagnostic criteria in Mainland China; this will improve nation-wide epidemiological investigations and scientific research on DOCs. Given the high misdiagnosis rate of VS/UWS and MCS, accurate identification of MCS is very challenging if it depends solely on behavioral responses to stimuli. The integration of neuroimaging techniques such as fMRI, dMRI, EEG, or PET may provide subjective markers that reflect the residual consciousness. The diagnostic criteria thus may be enriched and improved with these markers to facilitate accurate diagnosis. Prognosis also needs improvement. First, though many prognosis models have been proposed, a much larger cohort is needed for further validation. The number of patients, in particular those patients who later recover consciousness, is relatively low. Second, DOCs have many different causes, are associated with several neuropathological processes, and differ in severity, such that any method used alone carries the risk of false prediction, so hybrid prognostic models should be more promising. Third, the development of good prognostic models requires convergence of diverse disciplines, especially biology, medicine, and informatics. The development of new imaging and data analysis technologies has revolutionized our ability to measure and understand DOCs.
The management of DOCs remains challenging for all countries in the world because of the superficial understanding of the neural mechanisms of consciousness to date. We hope that, on the basis of the huge number of DOC patients in China, the growth of DOC studies in China will improve the international development about DOC studies.
Acknowledgements
I gratefully thank Yujin Zhang for her help in manuscript preparation and Jianghong He, Qiuyou Xie, Yi Yang, Ming Song, and Yue Cui for providing materials for the manuscript.
Compliance with Ethical Standards
Conflict of interest
The author declares no competing financial interests.
References
- 1.Jennett B, Plum F. Persistent vegetative state after brain damage. A syndrome in search of a name. Lancet. 1972;1:734–737. doi: 10.1016/S0140-6736(72)90242-5. [DOI] [PubMed] [Google Scholar]
- 2.Giacino JT, Zasler ND, Katz DI, Kelly JP, Rosenberg JH, Filley CM. Development of practice guidelines for assessment and management of the vegetative and minimally conscious states. J Head Trauma Rehabil. 1997;12:79–89. doi: 10.1097/00001199-199708000-00008. [DOI] [Google Scholar]
- 3.Giacino JT, Ashwal S, Childs N, Cranford R, Jennett B, Katz DI, et al. The minimally conscious state: definition and diagnostic criteria. Neurology. 2002;58:349–353. doi: 10.1212/WNL.58.3.349. [DOI] [PubMed] [Google Scholar]
- 4.Andrews K, Murphy L, Munday R, Littlewood C. Misdiagnosis of the vegetative state: retrospective study in a rehabilitation unit. BMJ. 1996;313:13–16. doi: 10.1136/bmj.313.7048.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014;10:99–114. doi: 10.1038/nrneurol.2013.279. [DOI] [PubMed] [Google Scholar]
- 6.Di Perri C, Annen J, Antonopoulos G, Amico E, Cavaliere C, Laureys S. Measuring consciousness through imaging. In: Monti MM, Sannita WG (Eds.). Brain Function and Responsiveness in Disorders of Consciousness. Springer; 2016: 51–65.
- 7.Vanhaudenhuyse A, Boly M, Bruno MA, Gosseries O, Demertzi A, Kirsch M, et al. Functional imaging and impaired consciousness. In: Schnakers C, Laureys S, et al., editors. Coma and Disorders of Consciousness. London: Springer; 2012. pp. 25–34. [Google Scholar]
- 8.Kalmar K, Giacino JT. The JFK coma recovery scale—revised. Neuropsychol rehabil. 2005;15:454–460. doi: 10.1080/09602010443000425. [DOI] [PubMed] [Google Scholar]
- 9.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;304:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 10.Gill-Thwaites H. The Sensory Modality Assessment Rehabilitation Technique-a tool for assessment and treatment of patients with severe brain injury in a vegetative state. Brain Inj. 1997;11:723–734. doi: 10.1080/026990597123098. [DOI] [PubMed] [Google Scholar]
- 11.Shiel A, Horn S, Wilson B, Watson M, Campbell M, McLellan D. The Wessex Head Injury Matrix (WHIM) main scale: a preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin Rehabil. 2000;14:408–416. doi: 10.1191/0269215500cr326oa. [DOI] [PubMed] [Google Scholar]
- 12.Gilutz Y, Lazary A, Karpin H, Vatine JJ, Misha T, Fortinsky H, et al. Detailed behavioral assessment promotes accurate diagnosis in patients with disorders of consciousness. Front Hum Neurosci. 2015;9:87. doi: 10.3389/fnhum.2015.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stokes V, Gunn S, Schouwenaars K, Badwan D. Neurobehavioural assessment and diagnosis in disorders of consciousness: a preliminary study of the Sensory Tool to Assess Responsiveness (STAR). Neuropsychol Rehabil 2016: 1–18. [DOI] [PubMed]
- 14.Pignat JM, Mauron E, Jöhr J, de Keranflec’h CG, Van De Ville D, Preti MG, et al. Outcome prediction of consciousness disorders in the acute stage based on a complementary motor behavioural tool. PLoS One. 2016;11:e0156882. doi: 10.1371/journal.pone.0156882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wannez S, Heine L, Thonnard M, Gosseries O, Laureys S, Collaborators CSG. The repetition of behavioral assessments in diagnosis of disorders of consciousness. Ann Neurol. 2017;81:883–889. doi: 10.1002/ana.24962. [DOI] [PubMed] [Google Scholar]
- 16.Xi Z, Feng G, Liu T, Gan Y, Wang P, Ma H. Traditional Chinese medicine study of persistent vegetative state. Clin Res. 2006;27:21–23. [Google Scholar]
- 17.The Multi-Society Task Force on PVS Medical aspects of the persistent vegetative state. N Engl J Med. 1994;330:1499–1508. doi: 10.1056/NEJM199405263302107. [DOI] [PubMed] [Google Scholar]
- 18.The expert panel for disorders of consciousness The nomenclature, definition and diagnostic criteria of persistent vegetative state. J Modern Clinic Biomedical Engineering. 1996;2:232. [Google Scholar]
- 19.Zhang G, Wang C, Ding X. Chinese diagnostic criteria and assessment scale for persistent vegetative state. Chin J Crit Care Med. 1999;19:632–633. [Google Scholar]
- 20.Diagnostic criteria and clinical curative effect scale for persistent vegetative state (Chinese Nanjing Criteria 2011 revised version, in Chinese). Chin J Naut Med Hyperbar Med 2011, 18: 319.
- 21.Di H, He M, Zhang Y, Cheng L, Wang F, Nie Y, et al. Chinese translation of the Coma Recovery Scale—Revised. Brain Inj. 2017;31:363–365. doi: 10.1080/02699052.2016.1255780. [DOI] [PubMed] [Google Scholar]
- 22.Fernandez-Espejo D, Soddu A, Cruse D, Palacios EM, Junque C, Vanhaudenhuyse A, et al. A role for the default mode network in the bases of disorders of consciousness. Ann Neurol. 2012;72:335–343. doi: 10.1002/ana.23635. [DOI] [PubMed] [Google Scholar]
- 23.Vanhaudenhuyse A, Noirhomme Q, Tshibanda LJ, Bruno MA, Boveroux P, Schnakers C, et al. Default network connectivity reflects the level of consciousness in non-communicative brain-damaged patients. Brain. 2010;133:161–171. doi: 10.1093/brain/awp313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stender J, Gosseries O, Bruno MA, Charland-Verville V, Vanhaudenhuyse A, Demertzi A, et al. Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet. 2014;384:514–522. doi: 10.1016/S0140-6736(14)60042-8. [DOI] [PubMed] [Google Scholar]
- 25.Song M, Zhang Y, Cui Y, Yang Y, Jiang T. Brain network studies in chronic disorders of consciousness: advances and perspectives. Neurosci Bull. 2018;34:592–604. doi: 10.1007/s12264-018-0243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casali AG, Gosseries O, Rosanova M, Boly M, Sarasso S, Casali KR, et al. A theoretically based index of consciousness independent of sensory processing and behavior. Sci Transl Med 2013, 5: 198ra105. [DOI] [PubMed]
- 27.Casarotto S, Comanducci A, Rosanova M, Sarasso S, Fecchio M, Napolitani M, et al. Stratification of unresponsive patients by an independently validated index of brain complexity. Ann Neurol. 2016;80:718–729. doi: 10.1002/ana.24779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qin P, Wu X, Huang Z, Duncan NW, Tang W, Wolff A, et al. How are different neural networks related to consciousness? Ann Neurol. 2015;78:594–605. doi: 10.1002/ana.24479. [DOI] [PubMed] [Google Scholar]
- 29.Wu X, Zou Q, Hu J, Tang W, Mao Y, Gao L, et al. Intrinsic functional connectivity patterns predict consciousness level and recovery outcome in acquired brain injury. J Neurosci. 2015;35:12932–12946. doi: 10.1523/JNEUROSCI.0415-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He J, Cui Y, Song M, Yang Y, Dang Y, Jiang T, et al. Decreased functional connectivity between the mediodorsal thalamus and default mode network in patients with disorders of consciousness. Acta Neurol Scand. 2015;131:145–151. doi: 10.1111/ane.12299. [DOI] [PubMed] [Google Scholar]
- 31.Wu X, Zhang J, Cui Z, Tang W, Shao C, Hu J, et al. White matter deficits underlie the loss of consciousness level and predict recovery outcome in disorders of consciousness. Neurosci Bull. 2018;34:668–678. doi: 10.1007/s12264-018-0253-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cui Y, Song M, Lipnicki DM, Yang Y, Ye C, Fan L, et al. Subdivisions of the posteromedial cortex in disorders of consciousness. arXiv preprint arXiv:1805.09999 2018. [DOI] [PMC free article] [PubMed]
- 33.Weng L, Xie Q, Zhao L, Zhang R, Ma Q, Wang J, et al. Abnormal structural connectivity between the basal ganglia, thalamus, and frontal cortex in patients with disorders of consciousness. Cortex. 2017;90:71–87. doi: 10.1016/j.cortex.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 34.Yao S, Song J, Gao L, Yan Y, Huang C, Ding H, et al. Thalamocortical sensorimotor circuit damage associated with disorders of consciousness for diffuse axonal injury patients. J Neurol Sci. 2015;356:168–174. doi: 10.1016/j.jns.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 35.Pan J, Xie Q, He Y, Wang F, Di H, Laureys S, et al. Detecting awareness in patients with disorders of consciousness using a hybrid brain–computer interface. J Neural Eng. 2014;11:056007. doi: 10.1088/1741-2560/11/5/056007. [DOI] [PubMed] [Google Scholar]
- 36.Bernat JL. Chronic disorders of consciousness. Lancet. 2006;367:1181–1192. doi: 10.1016/S0140-6736(06)68508-5. [DOI] [PubMed] [Google Scholar]
- 37.Bruno MA, Ledoux D, Vanhaudenhuyse A, Gosseries O, Thibaut A, Laureys S. Prognosis of patients with altered state of consciousness. In: Schnakers C, Laureys S, editors. Coma and Disorders of Consciousness. London: Springer; 2012. pp. 11–23. [Google Scholar]
- 38.Luaute J, Maucort-Boulch D, Tell L, Quelard F, Sarraf T, Iwaz J, et al. Long-term outcomes of chronic minimally conscious and vegetative states. Neurology. 2010;75:246–252. doi: 10.1212/WNL.0b013e3181e8e8df. [DOI] [PubMed] [Google Scholar]
- 39.Demertzi A, Sitt J, Sarasso S, Pinxten W. Measuring states of pathological (un)consciousness: research dimensions, clinical applications, and ethics. Neurosci Conscious 2017, 3. [DOI] [PMC free article] [PubMed]
- 40.Noirhomme Q, Brecheisen R, Lesenfants D, Antonopoulos G, Laureys S. “Look at my classifier’s result”: Disentangling unresponsive from (minimally) conscious patients. Neuroimage. 2017;145:288–303. doi: 10.1016/j.neuroimage.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 41.Zandbergen EGJ, de Haan RJ, Stoutenbeek CP, Koelman J, Hijdra A. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet. 1998;352:1808–1812. doi: 10.1016/S0140-6736(98)04076-8. [DOI] [PubMed] [Google Scholar]
- 42.Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004;291:870–879. doi: 10.1001/jama.291.7.870. [DOI] [PubMed] [Google Scholar]
- 43.Dolce G, Quintieri M, Serra S, Lagani V, Pignolo L. Clinical signs and early prognosis in vegetative state: A decisional tree, data-mining study. Brain Inj. 2008;22:617–623. doi: 10.1080/02699050802132503. [DOI] [PubMed] [Google Scholar]
- 44.Hofmeijer J, van Putten MJAM. EEG in postanoxic coma: Prognostic and diagnostic value. Clin Neurophysiol. 2016;127:2047–2055. doi: 10.1016/j.clinph.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 45.Steppacher I, Eickhoff S, Jordanov T, Kaps M, Witzke W, Kissler J. N400 predicts recovery from disorders of consciousness. Ann Neurol. 2013;73:594–602. doi: 10.1002/ana.23835. [DOI] [PubMed] [Google Scholar]
- 46.Chennu S, Annen J, Wannez S, Thibaut A, Chatelle C, Cassoi H, et al. Brain networks predict metabolism, diagnosis and prognosis at the bedside in disorders of consciousness. Brain. 2017;140:2120–2132. doi: 10.1093/brain/awx163. [DOI] [PubMed] [Google Scholar]
- 47.Maas AIR, Steyerberg EW, Butcher I, Dammers R, Lu J, Marmarou A, et al. Prognostic value of computerized tomography scan characteristics in traumatic brain injury: Results from the IMPACT study. J Neurotrauma. 2007;24:303–314. doi: 10.1089/neu.2006.0033. [DOI] [PubMed] [Google Scholar]
- 48.Sidaros A, Engberg A, Sidaros K, Liptrot MG, Herning M, Petersen P, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain. 2008;131:559–572. doi: 10.1093/brain/awm294. [DOI] [PubMed] [Google Scholar]
- 49.Luyt CE, Galanaud D, Perlbarg V, Vanhaudenhuyse A, Stevens RD, Gupta R, et al. Diffusion tensor imaging to predict long-term outcome after cardiac arrest a bicentric pilot study. Anesthesiology. 2012;117:1311–1321. doi: 10.1097/ALN.0b013e318275148c. [DOI] [PubMed] [Google Scholar]
- 50.Galanaud D, Perlbarg V, Gupta R, Stevens RD, Sanchez P, Tollard E, et al. Assessment of white matter injury and outcome in severe brain trauma a prospective multicenter cohort. Anesthesiology. 2012;117:1300–1310. doi: 10.1097/ALN.0b013e3182755558. [DOI] [PubMed] [Google Scholar]
- 51.Stender J, Gosseries O, Bruno MA, Charland-Verville V, Vanhaudenhuyse A, Demertzi A, et al. Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet. 2014;384:514–522. doi: 10.1016/S0140-6736(14)60042-8. [DOI] [PubMed] [Google Scholar]
- 52.Kaneko T, Kasaoka S, Miyauchi T, Fujita M, Oda Y, Tsuruta R, et al. Serum glial fibrillary acidic protein as a predictive biomarker of neurological outcome after cardiac arrest. Resuscitation. 2009;80:790–794. doi: 10.1016/j.resuscitation.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 53.Rundgren M, Karlsson T, Nielsen N, Cronberg T, Johnsson P, Friberg H. Neuron specific enolase and S-100B as predictors of outcome after cardiac arrest and induced hypothermia. Resuscitation. 2009;80:784–789. doi: 10.1016/j.resuscitation.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 54.Xu W, Kaur H, Wang X, Li H. The role of magnetic resonance imaging in the prediction of minimally conscious state after traumatic brain injury. World Neurosurg. 2016;94:167–173. doi: 10.1016/j.wneu.2016.06.123. [DOI] [PubMed] [Google Scholar]
- 55.Qin P, Wu X, Huang Z, Duncan NW, Tang W, Wolff A, et al. How are different neural networks related to consciousness? Ann Neurol. 2015;78:594–605. doi: 10.1002/ana.24479. [DOI] [PubMed] [Google Scholar]
- 56.Bernat JL. Prognostic limitations of syndromic diagnosis in disorders of consciousness. AJOB Neurosci. 2016;7:46–48. doi: 10.1080/21507740.2016.1146367. [DOI] [Google Scholar]
- 57.Rossetti AO, Rabinstein AA, Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 2016;15:597–609. doi: 10.1016/S1474-4422(16)00015-6. [DOI] [PubMed] [Google Scholar]
- 58.Kang XG, Li L, Wei D, Xu XX, Zhao R, Jing YY, et al. Development of a simple score to predict outcome for unresponsive wakefulness syndrome. Crit Care 2014, 18. [DOI] [PMC free article] [PubMed]
- 59.Song M, Yang Y, He J, Yang Z, Yu S, Xie Q, et al. Prognostication of chronic disorders of consciousness using brain functional networks and clinical characteristics. Neurons Cogn 2018. https://scirate.com/arxiv/1801.03268. [DOI] [PMC free article] [PubMed]
- 60.Whyte J, Katz D, Long D, DiPasquale MC, Polansky M, Kalmar K, et al. Predictors of outcome in prolonged posttraumatic disorders of consciousness and assessment of medication effects: A multicenter study. Arch Phys Med Rehabil. 2005;86:453–462. doi: 10.1016/j.apmr.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 61.Wang Y. Effect of AngongNiuhuang Wan on the recovery of disorders of consciousness after brain injury. J Integr Tradit West Med. 1989;9:726–727. [Google Scholar]
- 62.Guo Y, Xu R, Xiao H, Xu Q, Chen Y. Observation on the curative effect of integrated traditional Chinese and Western medicine combined with comprehensive rehabilitation therapy in the treatment of persistent vegetative state. Modern Rehabil. 2001;5:101. [Google Scholar]
- 63.Giacino J, Fins JJ, Machado A, Schiff ND. Central thalamic deep brain stimulation to promote recovery from chronic posttraumatic minimally conscious state: challenges and opportunities. Neuromodulation. 2012;15:339–349. doi: 10.1111/j.1525-1403.2012.00458.x. [DOI] [PubMed] [Google Scholar]
- 64.He JH, Yang Y, Jiao H, Dang YY, Dai YW, Zhang Q, et al. Neruomodulation treatment for patients under persistent vegetative state. Chin J Neuromed. 2013;12:1197–1200. [Google Scholar]
- 65.Yamamoto T, Watanabe M, Obuchi T, Kobayashi K, Oshima H, Fukaya C, et al. Spinal cord stimulation for vegetative state and minimally conscious state: changes in consciousness level and motor function. Acta Neurochir Suppl. 2017;124:37–42. doi: 10.1007/978-3-319-39546-3_6. [DOI] [PubMed] [Google Scholar]
- 66.Pei B. Spinal dorsal column stimulation (DCS) for vegetative statement. J Qiqihar Med Sch 1991: 16–17 [Article in Chinese].
- 67.Dong Y, Li J, Zhang S. Awoking effects of high cervical spinal cord stimulation on a comatose patient due to traumatic brain injury and literature review. Chin J Neurosurg 2011, 27: 568–570 [Article in Chinese].
- 68.Zhang X, Chen H, Liang E. A case of coma after traumatic brain injury was treated by high cervical spinal cord stimulation. Natl Med J China 2014, 94: 1512–1513 [Article in Chinese].
- 69.Bai Y, Xia X, Li X, Wang Y, Yang Y, Liu Y, et al. Spinal cord stimulation modulates frontal delta and gamma in patients of minimally consciousness state. Neuroscience. 2017;346:247–254. doi: 10.1016/j.neuroscience.2017.01.036. [DOI] [PubMed] [Google Scholar]
- 70.Si J, Dang Y, Zhang Y, Li Y, Zhang W, Yang Y, et al. Spinal cord stimulation frequency influences the hemodynamic response in patients with disorders of consciousness. Neurosci Bull. 2018;34:659–667. doi: 10.1007/s12264-018-0252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang Y, Yang Y, Si J, Xia X, He J, Jiang T. Influence of inter-stimulus interval of spinal cord stimulation in patients with disorders of consciousness: A preliminary functional near-infrared spectroscopy study. Neuroimage Clin. 2018;17:1–9. doi: 10.1016/j.nicl.2017.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Han Z, Zhou D, He H. Medianus nervi stimulation for persistent vegetative state after head injury: A report of 7 cases. Chin J Phys Ther 1999: 272 [Article in Chinese].
- 73.Gao GY, Bao YH, Liang YM, Pan YH, Ding SH, Jiang JY. Clinical efficacy of early right median nerve electrical stimulation for coma patients following craniocerebral trauma. Chin J Trauma 2012: 200–204.
- 74.Piccione F, Cavinato M, Manganotti P, Formaggio E, Storti SF, Battistin L, et al. Behavioral and neurophysiological effects of repetitive transcranial magnetic stimulation on the minimally conscious state: a case study. Neurorehabil Neural Repair. 2011;25:98–102. doi: 10.1177/1545968310369802. [DOI] [PubMed] [Google Scholar]
- 75.Louise-Bender Pape T, Rosenow J, Lewis G, Ahmed G, Walker M, Guernon A, et al. Repetitive transcranial magnetic stimulation-associated neurobehavioral gains during coma recovery. Brain Stimul. 2009;2:22–35. doi: 10.1016/j.brs.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 76.Liu P, Gao J, Pan S, Meng F, Pan G, Li J, et al. Effects of high-frequency repetitive transcranial magnetic stimulation on cerebral hemodynamics in patients with disorders of consciousness: a sham-controlled study. Eur Neurol. 2016;76:1–7. doi: 10.1159/000447325. [DOI] [PubMed] [Google Scholar]
- 77.Xia X, Bai Y, Zhou Y, Yang Y, Xu R, Gao X, et al. Effects of 10 Hz repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex in disorders of consciousness. Front Neurol. 2017;8:182. doi: 10.3389/fneur.2017.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yu YT, Yang Y, Wang LB, Fang JL, Chen YY, He JH, et al. Transcutaneous auricular vagus nerve stimulation in disorders of consciousness monitored by fMRI: The first case report. Brain Stimul. 2017;10:328–330. doi: 10.1016/j.brs.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 79.Thibaut A, Bruno MA, Ledoux D, Demertzi A, Laureys S. tDCS in patients with disorders of consciousness: sham-controlled randomized double-blind study. Neurology. 2014;82:1112–1118. doi: 10.1212/WNL.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 80.Cavanna AE, Shah S, Eddy CM, Williams A, Rickards H. Consciousness: a neurological perspective. Behav Neurol. 2011;24:107–116. doi: 10.1155/2011/645159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bai Y, Xia X, Wang Y, Guo Y, Yang Y, He J, et al. Fronto-parietal coherence response to tDCS modulation in patients with disorders of consciousness. Int J Neurosci. 2018;128:587–594. doi: 10.1080/00207454.2017.1403440. [DOI] [PubMed] [Google Scholar]
- 82.Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med. 2012;366:819–826. doi: 10.1056/NEJMoa1102609. [DOI] [PubMed] [Google Scholar]
- 83.Cai KH, Liu LJ, Dai LM, Wan Y, Du B, Zhao YY. Efficacy of zolpidem in promoting awakening from persistent vegetative state in patients with brain injury. Chin J Neuromed 2008, 7: 1174–1176 [Article in Chinese].
- 84.Huang L, Obenaus A. Hyperbaric oxygen therapy for traumatic brain injury. Med Gas Res. 2011;1:21. doi: 10.1186/2045-9912-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rockswold GL, Ford SE, Anderson DC, Bergman TA, Sherman RE. Results of a prospective randomized trial for treatment of severely brain-injured patients with hyperbaric oxygen. J Neurosurg. 1992;76:929–934. doi: 10.3171/jns.1992.76.6.0929. [DOI] [PubMed] [Google Scholar]
- 86.Rockswold SB, Rockswold GL, Zaun DA, Zhang X, Cerra CE, Bergman TA, et al. A prospective, randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism, intracranial pressure, and oxygen toxicity in severe traumatic brain injury. J Neurosurg. 2010;112:1080–1094. doi: 10.3171/2009.7.JNS09363. [DOI] [PubMed] [Google Scholar]
- 87.Wang C, Zhang G, Cao L. Hyperbaric oxygen as the main therapy for persistent vegetative state. Chin J Navig Med 1998, 5: 199–202 [Article in Chinese].
- 88.Yang Y, He JH, Jiao H, Xia XY, Dang YY, Dai YW, et al. The clinical efficacy of hyperbaric oxygen therapy and Meta analysis of time windows. Chin J Neurol 2015, 14: 501–505 [Article in Chinese].
- 89.Zhang X, Zhang P, Xu C, Wu D, Guo X. Clinical analysis of 19 cases of vegetative treatment with meridian guiding therapy. Nei Mongol Journal of Traditional Chinese Medicine 1994, 13: 42 [Article in Chinese].
- 90.Wang T. Buyang five decoction is the main treatment for 10 cases of vegetative diseases. The practical Chinese medicine journal 1996, 12: 3–5 [Article in Chinese].
- 91.Wang S, Hong J, Deng A, Kang W, He X. Clinical observation on 36 cases of persistent vegetative state after brain injury treated by acupuncture. Chin Acupunct 2000, 5: 267–268 [Article in Chinese].
- 92.Zhang L, Song HJ. Clinical study on the influence of three dimensional five senses awakening method on the PVS scale score of PVS patients and its awakening effect. Chin Med Clin Res 2012, 4: 10–11 [Article in Chinese].
- 93.Lombardi F, Taricco M, De Tanti A, Telaro E, Liberati A. Sensory stimulation of brain-injured individuals in coma or vegetative state: results of a Cochrane systematic review. Clin Rehabil. 2002;16:464–472. doi: 10.1191/0269215502cr519oa. [DOI] [PubMed] [Google Scholar]
- 94.Yang S. Clinical rehabilitation of patients with persistent vegetative state. Chinese Journal of rehabilitation medicine 1997, 12: 22–24 [Article in Chinese].
- 95.Di H, Schnakers C. Sensory stimulation program. In: Schnakers C, Laureys S, editors. Coma and Disorders of Consciousness. London: Springer-Verlag; 2012. pp. 97–103. [Google Scholar]


