Abstract
Swyer-James-MacLeod syndrome is a rare pulmonary disorder that exhibits unilateral hyperlucency of a part of or the entire lung and because it is usually asimptomatic the diagnostic of this illness is discovered accidentally after a chest X-ray. Although the cause of this disorder is not completely understood, most authors believe that this is due to late sequela of infectious bronchiolitis that occurs during childhood. The symptoms presented by the individuals are often scarce at the moment of diagnostic, but a history of recurrent episodes of pulmonary infection accompanied by dyspnea, hemoptysis and/or chronic productive cough should raise the suspicion for such a diagnosis. Swyer-James-MacLeod syndrome can be interpreted as asthma or pulmonary embolism and this can result in inappropriate therapy.
This case report describes a 38-year-old patient with chronic respiratory symptoms diagnosed on the findings of the chest X-ray and high resolution CT.
Keywords:Swyer James MacLeod syndrome, hyperluncent lung, high resolution CT
INTRODUCTION
Swyer James MacLeod is a rare pulmonary disorder that exhibits unilateral hyperlucency of a part or of one entire lung. It was first described in 1953 by Swyer and James and subsequently in 1954 by MacLeod (1, 2).
Swyer-James-MacLeod syndrome (SJMS) is frequently diagnosed in childhood but rarely, patients are diagnosed as adults if post infective bronchiectasis is not very severe (5).
CASE DESCRIPTION
A 38-year-old non-smoker patient was admitted to the pulmonology clinic accusing chronic dry cough that, on occasion, accompanied by expectoration of sputum and stage III dyspnea on the mMRC scale. Following a thorough anamnesis, it was revealed that the symptoms were present for some years and the cough that he described seemed to be related to temperature variation, especially in the morning.
The personal history of the patient has a long record of respiratory infections. Probably the first respiratory event occurred when he was no older than 1, at which time he had a severe respiratory condition that required him to be treated in the hospital for a long period of time, probably without sever clinical events in adulthood that required hospitalization.
Family history included the mother with asthma and his grandmother on his mother’ side was diagnosed with chronic bronchitis.
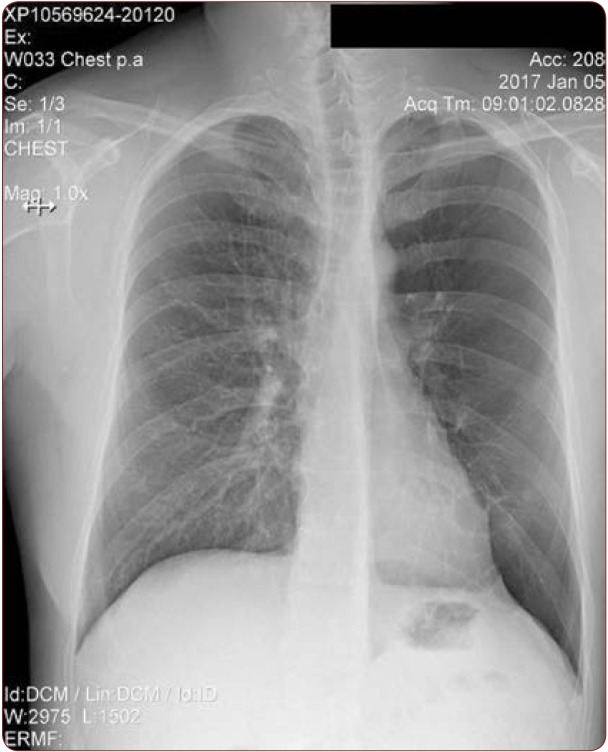
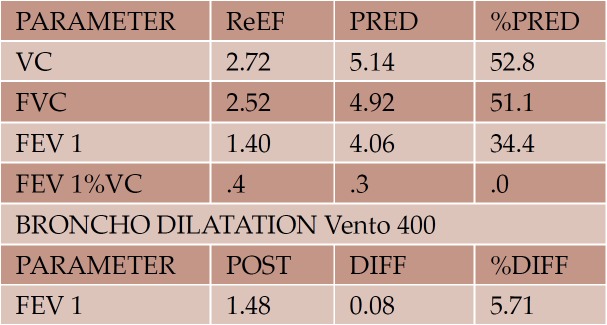
The clinical exam showed that the patient was in a general good condition with no fever, no hemoptysia or weight loss. The pulmonary auscultation revealed diminished breath sounds on the left side, and after a prolonged expiration, intermittent sibilant rales could be heard in the same area and a peripheral oxygen saturation of 98%. The chest X-ray displayed a hyperlucent left hemithorax with a reduced interstitial design and low vascularization of the hilum (Figure 1).The spirometry exam showed a severe mixed ventilatory dysfunction without any reversibility postbronchodilator administration (Figure 2).
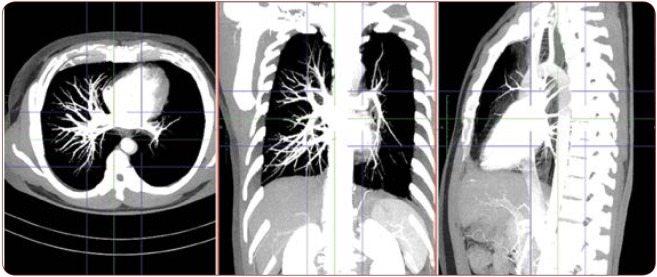
The computed tomography (CT) examination indicated:
– generalized hyperlucency of the left lung;
– attenuated (decreased) vascular markings on the left pulmonary area (Figure 3);
– small left hilum compared to the one on the other side;
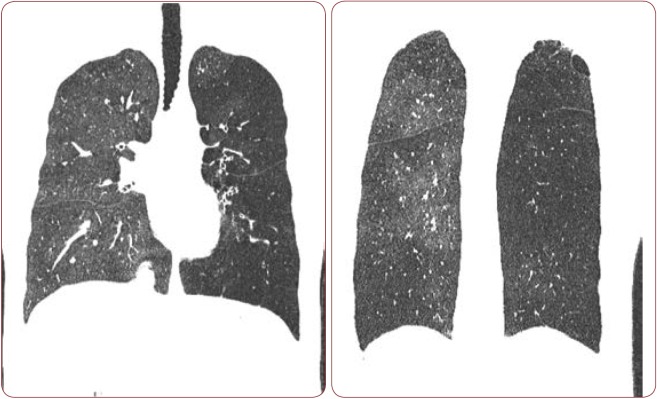
– inhale/exhale scanning did not reveal significant differences of the lung attenuation (the lung maintained a hyperlucency) – air trapping images (Figure 4);
– a few sub-pleural emphysema bullae in the superior left lobe, the largest one of almost 4 cm in size;
– focal “tree in bud” nodules in the apical region of the superior left lobe;
– diffuse bronchiectasis in the superior and inferior left lobes;
– bronchiectasis diffusely present on the pulmonary right area;
– focal “tree in bud” nodules in the posterobasale region of the inferior right lobe (Figure 5);
– mediastinum on the midline.
He was discharged on the same day with a prescription for bronchodilator therapy, both inhaler and orally (Theophylline 200 mg daily and budesonide/formoterol 320/9, 1 puff twice a day). Also, influenza and pneumococcal vaccinations were recommended.
DISCUSSION
The cause of SJMS is not completely understood (3). Most authors say that the disease develops after viral bronchiolitis and/or viral pneumonia in early childhood. The infectious agents, such as Mycoplasma pneumonia, Bordetella pertusis, adenovirus, paramyxovirus and measles, results in an inflammatory response, which causes obliteration of peripheral airways in the infected lung. This inflamation causes obliteration of the vascularity of the lung and impeded lung development. On long term, destruction of the alveoli and emphysema may occur (1, 2, 4). This pattern matches the personal history of our patient, who suffered recurrent episodes of pulmonary infections during his childhood.
Individuals with SJMS may be asymptomatic at diagnostic, but usually present dyspnea, hemoptysis, chronic productive cough and declare a history of recurrent episodes of pulmonary infection with onset early in life. For the case presented in this paper, the diagnosis was reached during a new follow-up for the patient’s chronic respiratory symptoms.
The diagnostic criteria for SJMS require one of the following three: unilateral loss of lung volume with hyperlucency as demonstrated by chest X-ray, unilateral reduction in vascularity on CT scan of the chest, or unilateral loss of perfusion on technetium TC99m lung scan (2).
For our 38-year-old patient, the chest X-ray offered the first criteria highly suggestive for this disease. However, in order to confirm the diagnostic, a high resolution CT (HRCT) during inspiration and expiration was performed, which indeed showcased a decreased caliber of the left pulmonary artery and attenuated vascular markings. Further more, air trapping images were found during the inhale/exhale scanning of the lungs. These features represent another important characteristic associated with SJMS. Having confirmed two out of three criteria, the ventilation- perfusion lung scanning was not performed. Another reason for this decision was the fact that false-positives results could appear in the case of any disorder involving distal airway (6).
The treatment for this affliction is conservative in most cases, comprising treatment of recurrent lung infections and prevention using influenza and pneumococcal vaccinations (7, 8). However, there are a few reports in literature describing surgical treatment, when patients underwent pneumectomy, lobectomy or segmentectomy (7). As for morbidity and mortality associated with this syndrome, no studies have been done yet (6).
CONCLUSIONS
The importance of the presented case is that this patient represents one of the rare occurances of Swayer-James-MacLeod syndrome in an adult. Considering this, and the fact that the condition may be asymptomatic, it is well worth to consider this diagnostic for patients who present an unilateral hyperlucency of the lung on a chest X-ray.
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
Chest X-ray showing a hyperlucent left hemithorax with the reduction of interstitial design and low vascularization of the hilum
FIGURE 2.
Spirometry test portraying severe mixed ventilatory dysfunction
FIGURE 3.
CT exam showing hyperlucency of the entire left lung, decreased vascular markings on the left pulmonary area. Small left hilum compared to the one on the other side
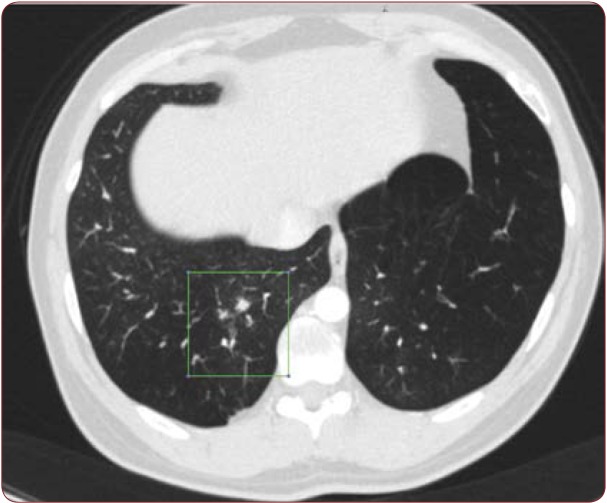
FIGURE 4.
CT exam revealing focal “tree in bud” nodules in the apical region of the superior left lobe and diffuse bronchiectasis in the superior and inferior left lobes
FIGURE 5.
CT exam portraying focal “tree in bud” nodules in the posterobasale region of the inferior right lobe
Contributor Information
Diana Veronica TURCU, “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
Stefana Cristina DUPA, “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
Adina TURCANU, “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
Traian Mihaescu, "Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania; Pulmonology Clinical Hospital, Iasi, Romania.
REFERENCES
- da Silva LPS, Lopes R, Neto MH. Swyer-James-Macleod syndrome in a surgically treated child: a case report and brief literature review. Journal of Pediatric Surgery. 2012;4:e17–e22. doi: 10.1016/j.jpedsurg.2011.12.011. [DOI] [PubMed] [Google Scholar]
- Chaucer B, Chevenon M, Toro C, et al. Swyer-James-Macleod syndrome: a rare finding and important differential in the ED setting. The American Journal of Emergency Medicine. 2016;7:1329.e3–1329.e4. doi: 10.1016/j.ajem.2015.12.045. [DOI] [PubMed] [Google Scholar]
- Chong B, Xiao-Lian S, Hui S, et al. Swyer-James Syndrome with Peculiar Course and Ipsilateral Pulmonary Vein Defect. Internal Medicine. 2011;17:1829–1833. doi: 10.2169/internalmedicine.50.4151. [DOI] [PubMed] [Google Scholar]
- Tortajada M, Gracia M, Garcia E, Hernández R. Consideraciones diagnosticas sobre el llamado sindrome del pulmon hiperclaro unilateral (sindrome de Swyer-James o de Mc-Leod). Allergologia et Immunopathologia. 2004;5:265–270. doi: 10.1016/s0301-0546(04)79253-8. [DOI] [PubMed] [Google Scholar]
- Chauhan S, Yegneswaran B. A rare childhood condition newly diagnosed in a 82-year-old patient. CHEST 2016 Annual Meeting Abstracts. 2016;4:643A. [Google Scholar]
- Capela C, Gouveia P, Sousa M, Regadas MJ. Adult diagnosis of Swyer-James-MacLeod syndrome: a case report. J Med Case Reports. 2011;5:2. doi: 10.1186/1752-1947-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fregonese L, Girosi D, Battistini E, et al. Clinical, physiologic, and roentgenographic changes after pneumonectomy in a boy with Macleod/Swyer-James syndrome and bronchiectasis. Pediatr Pulmonol. 2002;5:412–416. doi: 10.1002/ppul.10178. [DOI] [PubMed] [Google Scholar]
- Gómez Belda AB, Martínez-Moragón E, Fabrellas FE. Swyer-James syndrome: diagnostic contributions of helical computerized tomography. Arch Bronconeumol. 2000;7:421–422. [PubMed] [Google Scholar]