 A large number of nongenotoxic chemicals have been shown to increase the incidence of liver tumours in rats and/or mice by a mode of action (MOA) involving activation of the constitutive androstane receptor (CAR).
A large number of nongenotoxic chemicals have been shown to increase the incidence of liver tumours in rats and/or mice by a mode of action (MOA) involving activation of the constitutive androstane receptor (CAR).
Abstract
A large number of nongenotoxic chemicals have been shown to increase the incidence of liver tumours in rats and/or mice by a mode of action (MOA) involving activation of the constitutive androstane receptor (CAR). Studies with the model CAR activator phenobarbital (PB) and its sodium salt (sodium phenobarbital; NaPB) have demonstrated that the key and associative events for rat and mouse liver tumour formation include CAR activation, increased hepatocyte replicative DNA synthesis (RDS), induction of cytochrome P450 CYP2B subfamily enzymes, liver hypertrophy, increased altered hepatic foci and hepatocellular adenomas/carcinomas. The key species difference between the rat and mouse compared to humans, is that human hepatocytes are refractory to the mitogenic effects of PB/NaPB and other CAR activators. While PB/NaPB and other CAR activators stimulate RDS in rat and mouse hepatocytes in both in vitro and in vivo studies, such compounds do not stimulate RDS in cultured human hepatocytes and in in vivo studies performed in chimeric mice with humanised livers. In terms of species differences in RDS, unlike the rat and mouse, humans are similar to other species such as the Syrian hamster and guinea pig in being nonresponsive to the mitogenic effects of CAR activators. Overall, the MOA for rat and mouse liver tumour formation by PB/NaPB and other CAR activators is considered qualitatively not plausible for humans. This conclusion is supported by data from a number of epidemiological studies, which demonstrate that chronic treatment with PB does not increase the incidence of liver cancer in humans.
Introduction
Many genotoxic and nongenotoxic chemicals have been shown to produce tumours in chronic studies performed in the rat and mouse.1–3 As shown in Table 1, analysis of tumour data demonstrates that the liver is the most common site of tumour formation in both these two rodent species, compared to other target organs including the lung, kidney, thyroid gland and mammary gland. In recent years, frameworks for analysing the modes of action (MOAs) by which chemicals produce tumours in laboratory animals, such as the rat and mouse, and the relevance of such tumours for human risk assessment have been developed.4–8 Such mode of action (MOA) frameworks are invaluable tools to permit human risk assessment of animal (e.g. rodent) carcinogens. By use of the modified Bradford Hill considerations, the key and associative events for the MOA for tumour formation in animals can be identified, which can subsequently be compared both qualitatively and then quantitatively with effects in humans.
Table 1. Frequency of selected target organ carcinogenicity in rats and mice a .
| Target organ | Percentage of carcinogenic chemicals |
|
| Rats (n = 526 chemicals) | Mice (n = 412 chemicals) | |
| Liver | 39 | 56 |
| Lung | 10 | 28 |
| Kidney | 16 | 6 |
| Thyroid gland | 6 | 4 |
| Mammary gland | 19 | 6 |
aData from Gold et al. (2001).2
In terms of liver tumour formation, a number of MOAs have now been identified.4,5,9–15 Some examples are shown in Table 2. Clearly, liver tumours are known to be produced in both rodents and humans by genotoxic agents, such as aflatoxin B1.16 However, apart from DNA reactive compounds, liver tumours can also be produced by nongenotoxic MOAs, which involve the stimulation of replicative DNA synthesis (RDS). Some of the nongenotoxic liver tumour MOAs listed in Table 2 (e.g. estrogen, cytotoxicity, infection and metal overload) can be relevant for humans.9 For example, xenobiotic-induced hepatic cytotoxicity could be relevant for humans, depending on the level of human exposure to the xenobiotic and other factors, as compounds which produce a sustained regenerative hyperplasia can result in liver tumour formation in rodents.
Table 2. Some modes of action for liver tumour formation a .
| Genotoxic |
| -DNA reactivity |
| Nongenotoxic – receptor mediated |
| -Aryl hydrocarbon receptor activation (CYP1A induction) |
| -Constitutive androstane receptor activation (CYP2B induction) |
| -Peroxisome proliferator-activated receptor alpha activation (CYP4A induction) |
| -Estrogen |
| -Statins |
| Nongenotoxic – non receptor activated |
| -Cytotoxicity |
| -Infection |
| -Metal overload (e.g. iron, copper) |
| -Increased apoptosis |
aModified from Cohen (2010).9
Some MOAs for rodent liver tumour formation by nongenotoxic agents are associated with induction of hepatic microsomal cytochrome P450 (CYP) enzymes.5,9,12–15 Receptors involved in the induction of hepatic CYP1A, CYP2B, CYP3A and CYP4A subfamily enzymes comprise, respectively, the aryl hydrocarbon receptor (AhR), the constitutive androstane receptor (CAR), the pregnane X receptor (PXR) and the peroxisome proliferator-activated receptor alpha (PPARα). It should be noted that, apart from AhR, CAR, PXR and PPARα, other hepatic receptors, such as the glucocorticoid receptor, vitamin D receptor, farnesoid X receptor, liver X receptor and hepatocyte nuclear factor-4 are also involved in the regulation of hepatic CYP enzymes.17 Rodent liver tumour MOAs have been established for activators of the AhR, CAR and PPARα receptors.5,9,12–15 Due to lack of suitable data, no MOA for rodent liver tumour formation by PXR activators has yet been established, although such a MOA would likely be similar to that established for CAR and PPARα activators, where receptor activation leads to a pleotrophic response including the stimulation of RDS.14 This review will focus on rodent liver tumours produced by CAR activators and the relevance of such tumours for humans.
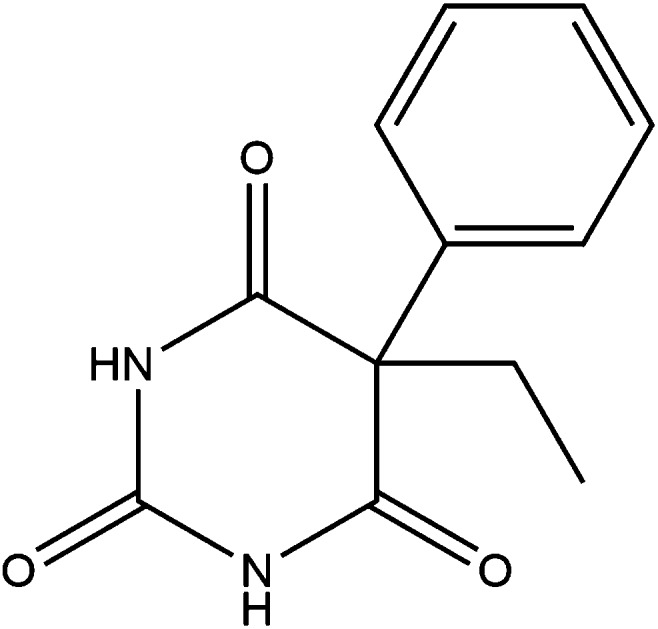
Phenobarbital
Phenobarbital (phenobarbitone; PB) and its sodium salt, namely sodium phenobarbital (sodium phenobarbitone; NaPB), are prototypical inducers of hepatic CYP2B subfamily enzymes in rodent liver. As described below, because of the large amount of available data from both animal and human studies, PB and NaPB are considered to be model compounds for the MOA for rodent liver tumour formation by CAR activators. Data for other rodent liver CAR activators will also be included in this review.
Treatment with PB/NaPB induces CYP2B1 and CYP2B2 enzymes in rat liver and Cyp2b9 and Cyp2b10 enzymes in mouse liver.18 Other known rodent hepatic CYP2B enzyme inducers include 1,4-bis[2-(3,5-dichloropyridyloxy)]benzene (TCPOBOP), 1,1,1-trichloro-2,2-bis(4-chlorophenyl)ethane (DDT), cyproconazole, chlordane, dieldrin, metofluthrin, momfluorothrin, oxazepam and the natural pyrethrins.12,14,17–22 In addition to effects on hepatic CYP2B subfamily enzymes, these compounds also induce other phase I xenobiotic metabolising enzymes (e.g. CYP2C and CYP3A subfamily enzymes) and various phase II xenobiotic metabolising enzymes including microsomal epoxide hydrolase and UDPglucuronosyltransferase enzymes and cytosolic sulphotransferase and GSH S-transferase enzymes.12,19 In human liver, PB/NaPB have been shown to induce a number of CYP enzymes including CYP2B6, CYP2C9, CYP2C19 and CYP3A4.23
Hepatic CAR
For induction of CYP2B subfamily enzymes, after chemical activation CAR undergoes nuclear translocation and heterodimerises with the retinoid X receptor (RXR), which is followed by binding to response elements in DNA.17,19,23 A number of splice variants of CAR have been identified in both rodent and human liver.19,24,25 Unlike some other receptors, CAR can be activated either by direct ligand binding to the receptor or by indirect activation.17,19,23,26 While PB is not a direct activator of CAR, compounds such as TCPOBOP and 6-(4-chlorophenyl)imidazo[2,1-b][1,3]thiazole-5-carbaldehyde O-(3,4-dichlorobenzyl)oxime (CITCO) are direct activators of the receptor.17,19,24 The localisation and function of hepatic CAR is regulated by phosphorylation of threonine 38 in human liver and of threonine 42 in mouse liver.26–28 While epidermal growth factor (EGF) activates the epidermal growth factor receptor (EGFR) preventing the dephosphorylation of CAR, PB inhibits EGFR signalling resulting in CAR activation.26–28 Ligands such as TCPOBOP and CITCO can bind directly to phosphorylated CAR leading to CAR activation.26 In this review, compounds will be referred to as CAR activators, without any consideration of whether they can bind directly to the receptor or activate the receptor by an indirect mechanism.
While PB is an indirect hepatic CAR activator in many species, TCPOBOP and CITCO have been reported to be potent direct activators of mouse and human CAR, respectively.17,19,29,30 However, it should be noted that these two potent mouse and human CAR activators are not species specific. For example, the mouse CAR activator TCPOBOP at high doses has been shown to induce CYP2B enzymes in rat liver and to promote liver tumours after initiation with the known genotoxin diethylnitrosamine (DEN), whereas the human CAR activator CITCO has been shown to activate CAR-responsive genes in mouse liver.31–33
Several studies have demonstrated that there can be considerable crosstalk between hepatic receptors with respect to induction of CYP enzymes.17,19 There is a high degree of similarity between CAR and PXR, with some compounds being activators of both receptors.34–36 Apart from regulation of hepatic xenobiotic metabolising enzymes, CAR is also involved in the regulation of genes involved in cell proliferation, apoptosis and intermediary metabolism.17,19
Rodent liver tumours induced by PB/NaPB and other CAR activators
Many studies have investigated liver tumour formation by PB/NaPB in various rat and mouse strains.14,37,38 As discussed by Elcombe et al. (2014),14 some of these studies have utilised just one dose level (e.g. 500 ppm in the diet or drinking water) and were conducted some time ago, before the adoption of modern pathological diagnostic criteria. Hence, in early publications lesions were sometimes classified as neoplastic or hyperplastic nodules and sometimes as eosinophilic or basophilic nodules etc. Current morphological criteria would classify PB/NaPB-induced tumours as either hepatocellular adenoma or as hepatocellular carcinoma. Male mice are considered to be more susceptible than female mice to both spontaneous and chemically-induced liver tumour formation.39 High susceptibility strains include C3H, CBA and B6C3F1 mice, with CD-1 mice having intermediate susceptibility and BALB/c, C57BL/6 and C57BL/10 mice having only low susceptibility. Genetic differences between high and low spontaneous incidence mouse strains have been described and transcriptomic differences between the short-term effects of PB and TCPOBOP in male and female CD-1 mice have been reported.39–41
Examination of the available literature clearly demonstrates that chronic treatment with PB/NaPB results in liver tumour formation in the mouse.37,38,42–44 While there are marked mouse strain differences in susceptibility to spontaneous liver tumour formation, PB/NaPB has been shown to produce liver tumours in both high (e.g. C3H/He) and low (e.g. C57BL/6) spontaneous incidence mouse strains.37,38,43,45,46 For example, in a study with the low spontaneous incidence C57BL/10J mouse strain, employing current morphological criteria, the treatment of male mice with 1000 ppm NaPB in the diet for 99 weeks resulted in statistically significant increases in both hepatocellular adenoma and hepatocellular carcinoma.44 This study also demonstrated a clear threshold for liver tumour formation with no liver tumours being observed in male mice at a dietary level 200 ppm and a clear sex difference with no statistically significant increase in liver tumours being observed in female mice given both 200 and 1000 ppm NaPB.
Although a number of studies have demonstrated that PB/NaPB can produce hepatocellular adenomas and carcinomas in the mouse, in some studies conducted in the rat PB/NaPB has been reported only to increase the incidence of altered hepatic foci.37,38,47,48 However, in one study the treatment of Wistar rats with 500 ppm NaPB in the drinking water was reported to produce hepatocellular adenomas.49
Overall, when administered at a high enough dosage for a sufficient period, PB/NaPB would be expected to produce liver tumours in many mouse strains, whereas rat strains are more resistant to liver tumour formation by this CAR activator. Generally, other nongenotoxic rodent CAR activators also produce liver tumours more readily in mice than in rats. However, there are exceptions and hence the observed increased sensitivity of the mouse to liver tumour formation by some rodent CAR activators should not be interpreted as a general rule by which to assess such compounds. For example, the synthetic pyrethroids metofluthrin and momfluorothrin, the fungicide fluopyram and the natural pyrethrins, which are all nongenotoxic CAR activators, have been shown to produce liver tumours in the rat but not in the mouse.20–22,50 Differences between the rat and mouse in susceptibility for liver tumour formation by CAR activators may possibly reflect species differences in receptor activation or may be due to other factors including pharmacokinetic and/or metabolism differences.
The hepatic effects of PB/NaPB on liver foci and tumour formation have been shown to be more pronounced in old rather than in young F344 rats and C3H/He mice.51,52 The increased susceptibility with age suggests that liver tumour formation by PB/NaPB and other CAR activators may involve the promotion of spontaneously initiated preneoplastic lesions that are more commonly observed in the livers of aging rodents.53
While PB/NaPB and other CAR activators can produce liver tumours in the rat and/or mouse, such compounds can also be effective promoters of genotoxic carcinogen-induced liver lesions. A number of initiation/promotion studies have been conducted where PB/NaPB have been administered to adult rats and mice after treatment with a genotoxic agent such as DEN, with subsequent treatment with PB/NaPB increasing the incidence of liver tumour formation.37,38 Similarly, other CAR activators have also been shown to promote liver tumour formation in rats and mice following treatment with a genotoxic agent. For example, TCPOBOP was shown to promote liver tumours in male F344 rats treated with a single dose of DEN, whereas DDT was shown to promote liver tumours in male Sprague-Dawley rats after treatment with 2-acetylaminoflurone and dieldrin was shown to promote liver tumours in B6C3F1 mice treated with a single dose of DEN.32,54,55
While PB/NaPB have been shown to promote genotoxic carcinogen-induced liver lesions in many studies conducted in adult rodents, studies conducted in young animals have yielded equivocal results.37,38,56 As discussed below, whether PB/NaPB either promote or inhibit liver tumour formation in young rodents is dependent on a number of factors including the experimental design (e.g. the time and order between genotoxin and PB/NaPB treatment), the age, sex and strain of the animals used and the genotoxin employed. The treatment of male 15 day old B6C3F1 mice with a single dose of DEN followed by subsequent PB treatment resulted in an inhibition of liver tumour formation compared to mice given DEN alone.57–61 However, unlike male 15 day old B6C3F1 mice, PB promoted liver tumour formation in female 15 day old B6C3F1 mice given a single dose of DEN.60 Apart from sex differences, mouse strain differences in effects of PB promotion of genotoxic carcinogen-induced liver lesions have also been observed. For example, unlike male B6C3F1 mice, PB promoted liver tumour formation in male 15 day old BALB/c mice given a single dose of DEN.58,62 In another study, male 15 day old B6C3F1, C3H/He and C57BL/6 mice were given single genotoxin doses of either DEN or dimethylnitrosamine (DMN) followed by subsequent PB treatment.61 As in previous studies, PB treatment inhibited liver tumour formation in B6C3F1 mice initiated with DEN, whereas liver tumour formation was increased in B6C3F1 mice initiated with DMN and in C3H/He mice initiated with either DEN or DMN. Treatment with PB did not affect liver tumour formation in C57BL/6 mice given either DEN or DMN.
Overall, while a number of studies have demonstrated that PB/NaPB are effective promoters of genotoxic carcinogen-induced liver lesions in adult rodents, studies conducted in young mice have produced equivocal results. While PB/NaPB have been shown to inhibit liver tumour formation in some instances, this is clearly not a consistent finding and as described above is dependent on many factors including the experimental design, the age, sex and strain of the animals used and the genotoxin employed.
MOA for PB-induced rodent liver tumour formation
A number of studies have described similar MOAs for rodent liver tumour formation by PB and related compounds.5,9,12,14 One comprehensive evaluation of the available literature was performed by Elcombe et al. (2014), employing PB as a model CAR activator, where key events, associative events and modulating factors for the MOA for PB-induced rodent liver tumour formation were identified.7,14 A key event was considered as an empirically observable precursor step to tumour formation that was a necessary element of the MOA, whereas an associative event was considered to be a biological process that was not a causal precursor step to the MOA, but was a reliable indicator or marker for key events. Hence, an associative event can be employed as a surrogate marker for a key event. Modulating factors were considered to be not necessary to influence the adverse outcome, but could modulate dose–response relationships or probability of inducing one or more key events or tumour formation. Based on an evaluation of the available literature, the key events, associative events and modulating factors for the MOA for PB-induced rodent liver tumour formation identified by Elcombe et al. (2014)14 are shown in Table 3 and comments on some of these key and associative events and modulating factors are given below.
Table 3. MOA for PB-induced rodent liver tumour formation: key and associative events and modulating factors a .
| Parameter | Endpoint |
| Key event | CAR activation |
| Altered gene expression specific to CAR activation | |
| Increased cell proliferation | |
| Clonal expansion leading to altered foci | |
| Liver adenomas/carcinomas | |
| Associative event | Altered epigenetic changes specific to CAR activation |
| CYP2B enzyme induction | |
| Liver hypertrophy | |
| Inhibition of apoptosis | |
| Associative event or a modulating factor | Inhibition of gap junctional intercellular communication |
aFrom Elcombe et al. (2014).14
CAR activation (key event)
The initial key event is clearly activation of the nuclear receptor CAR. In establishing the MOA for rodent liver tumour formation by PB/NaPB and other CAR activators, studies in transgenic mice lacking CAR (i.e. CAR knockout (KO) mice) have been particularly valuable. Such studies have demonstrated that PB/NaPB does not increase liver weight, produce liver hypertrophy (by morphological examination) and does not induce Cyp2b enzymes or hepatocyte RDS in CAR KO mice.63–66 Moreover, PB does not promote liver tumours in CAR KO mice after initiation with the genotoxic agent DEN, or after treatment with the potent mouse CAR activator TCPOBOP, either with or without prior DEN administration.64,65 The CAR KO mice employed in these liver tumour promotion studies were generated from both high (C3H/He) and low (C57BL/6) spontaneous liver tumour incidence mouse strains.64,65
As described above, several studies have demonstrated that there can be considerable crosstalk between hepatic CAR and PXR receptors, with some compounds being activators of both these nuclear receptors.17,19,34–36 This has led to the development of CAR/PXR KO mice, where short term treatment with PB/NaPB has been shown not to increase liver weight, produce liver hypertrophy and not to induce Cyp2b and Cyp3a enzymes or hepatocyte RDS.25,66 Recently, transgenic rat models lacking CAR, PXR and both CAR and PXR (CAR KO/PXR KO rats) have been developed and have become commercially available.67 In one study, treatment with TCPOBOP increased hepatic CYP2B2 mRNA levels in wild type (i.e. normal) rats, but not in CAR KO/PXR KO rats; whereas in another study treatment with NaPB increased liver weight, produced liver hypertrophy and induced CYP2B and CYP3A enzymes and hepatocyte RDS in wild type but not in CAR KO/PXR KO rats.67,68
RDS (key event)
Evaluation of the literature demonstrates that the stimulation of hepatocyte RDS is the pivotal key event in the MOA for rodent liver tumour formation induced by PB/NaPB and other CAR activators. Indeed, as described below, species differences in this key event demonstrate that the MOA for rodent liver tumour formation by PB/NaPB and other CAR activators is not applicable to humans.
A number of experimental techniques can be utilised to examine the effect of a chemical on RDS in rodent liver.14,69 Hepatocyte RDS in rodent liver can be assessed by administering a DNA precursor (e.g. [3H]thymidine or 5-bromo-2′-deoxyuridine (BrdU)) followed by analysis of liver sections to determine the hepatocyte labelling index (i.e. the percentage of hepatocyte nuclei undergoing replicative DNA synthesis). While the DNA precursor can be given as a single dose, this is not as sensitive in detecting low levels of cell proliferation as administering the DNA precursor continuously via a subcutaneously implanted osmotic pump for a suitable period (e.g. 7 days). Other methods of assessing effects on hepatocyte RDS include measurement of hepatic mRNA levels and immunocytochemistry of liver section for markers such as proliferating cell nuclear antigen (PCNA) or Ki-67.
Cell proliferation in rodent liver, when assessed as the hepatocyte labelling index, appears on an initial examination to be transient and not sustained. Several studies with PB/NaPB and other CAR activators have demonstrated significant increases in RDS in rat and mouse hepatocytes, determined as the hepatocyte labelling index, at early time points (e.g. 3 or 7 days of treatment), but generally not a longer time points (e.g. 28 or 90 days of treatment).21,22,37,38,44,70–72 Indeed, the effect of PB/NaPB and other CAR activators on RDS in rodent hepatocytes has been frequently described in the literature as only “transient”.37,38,73–75 It is certainly not correct to assess the effect of CAR activators on cell proliferation in rodent liver solely in terms of an effect on the hepatocyte labelling index. While the labelling index is just a measure of the percentage of hepatocyte nuclei undergoing RDS, this takes no account of the increase in liver weight and hence the total number of hepatocytes in rodents treated with PB/NaPB and other CAR activators.9,10,12,14 In one study employing a stereological technique, the treatment of male F344 rats with PB for 2 and 12 weeks resulted in a significant increase in liver weight at both time points and as shown in Table 4, a significant increase in the total number of hepatocytes per rat after 12 weeks.76 Such data can be put into perspective with that from other studies. For example, treatment with 500 ppm PB in the diet significantly increased RDS (assessed as the hepatocyte labelling index) in the livers of male B6C3F1 mice after 7, 14, 21 and 28 days of treatment, with the maximal increase being observed after 7 days of treatment and the hepatocyte labelling index having returned to control levels after 90 days of treatment.70 However, in this study PB produced a sustained increase in relative liver weight at all time points, thus indicating an overall increase in the number of hepatocytes per animal in PB treated mice compared to control mice even after 90 days of PB administration and hence a continued stimulation of the overall magnitude of cell proliferation in treated compared to control mice. Indeed, several studies have demonstrated that the prolonged administration (e.g. up to 2 years) of PB/NaPB results in a sustained increase in relative liver weight and hence in the number of hepatocytes in treated animals compared to controls.44,46,48
Table 4. Effect of PB on the number of hepatocytes in the livers of male F344 rats a .
| Treatment (drinking water) b | Time (weeks) | Total number of hepatocytes/rat × 108 |
| Control | 2 | 20.5 ± 0.5 (100) c |
| PB 1000 ppm | 2 | 20.9 ± 2.0 (102) |
| Control | 12 | 24.3 ± 1.7 (100) |
| PB 1000 ppm | 12 | 30.8 ± 1.5* (127) |
aData from Carthew et al. (1998).76
bPB was administered in the drinking water to male F344 rats for periods of 2 and 12 weeks.
cResults are mean ± SEM for groups of 4 animals. Values significantly different from respective controls are: *p < 0.05. Figures in parentheses are percentage of control values.
Clonal expansion leading to altered liver foci (key event)
Altered liver foci are considered to be the precursor lesions for subsequent tumour formation.77,78 However, unlike some other key and associative events, where effects can be assessed in short term studies, the detection of altered foci requires prolonged administration of PB/NaPB.14
Liver adenomas/carcinomas (key event)
Based on current morphological criteria the chronic treatment of mice with NaPB/PB can result in the formation of both hepatocellular adenoma and carcinoma.14,37,38,44 While the formation of liver adenomas in rats by treatment with NaPB has only been reported in one study, as described above, some other rodent liver CAR activators have been shown to produce liver tumours in the rat and not in the mouse.20–22,38,49,50
CYP2B induction (associative event)
PB/NaPB and other CAR activators induce hepatic CYP enzymes in rodent liver.17–19 As such induction proceeds through CAR activation, the measurement of CYP enzymes thus provides a reliable marker (i.e. an associative event) to assess the effects and dose–response relationships of a test compound in rodent liver. CYP enzyme induction can be assessed by determination of CYP mRNA levels (e.g. CYP2B1 for the rat and Cyp2b10 for the mouse) and by the determination of microsomal enzyme activities. The activity of 7-pentoxyresorufin O-depentylase (PROD) is a good marker for CYP2B induction in rat and mouse liver, with other useful enzyme activities also including testosterone 16β-hydroxylase and 7-benzyloxyresorufin O-debenzylase (BROD). CAR activators also induce CYP3A and other CYP enzymes. CYP3A induction can also be assessed by determination of CYP mRNA levels (e.g. CYP3A1 for the rat and Cyp3a11 for the mouse) and by enzyme activities such as 7-benzyloxyquinoline O-debenzylase (BQ) or testosterone 6β-hydroxylase.
Studies in male F344 rats with PB and a series of other barbiturates have shown some correlations between the magnitude of induction of hepatic CYP2B enzyme activities and liver tumour promotion following DEN initiation.79,80 However, the magnitude of effect of a test chemical on any of the key and associative events for a CAR activator MOA cannot be reliably employed to predict subsequent liver tumour formation.
The effect of NaPB on hepatic Cyp2b10 mRNA levels and RDS has been studied in male and female C57Bl/6 (WT) mice and in Cyp2a(4/5) null mice where all Cyp2b genes are deleted.81 While NaPB did not induce hepatic Cyp2b10 mRNA levels in male and female Cyp2a(4/5) null mice, unlike WT mice, hepatocyte RDS was induced in both WT and null mice, there being little difference in the magnitude of induction of RDS between WT and Cyp2a(4/5) null mice. This study demonstrates that the key event of increased hepatocyte RDS and the associative event of induction of Cyp2b10 mRNA levels constitute independent endpoints in the hepatic effects of CAR activators.
Liver hypertrophy (associative event)
PB/NaPB and other CAR activators produce hypertrophy in rodent liver, which can be assessed either as increased liver weight or by morphological examination of liver sections.14 Liver hypertrophy is normally observed in the centrilobular region of the liver lobule, although treatment with some CAR activators can result in either hypertrophy in other regions of the liver lobule or in a diffuse hypertrophy.12,14,21,22,72 As with CYP2B enzyme induction, liver enlargement (which is due to both hyperplasia and hypertrophy) proceeds through CAR activation, hence the measurement of liver enlargement provides a reliable marker (i.e. an associative event) to assess the effects and dose–response relationships of a test compound in rodent liver.
Other associative events and modulating factors
The inhibition of apoptosis is considered to be an associative event in the MOA for rodent liver tumour formation by PB/NaPB and other CAR activators.14 However, this can be a difficult endpoint to quantify in short term studies, owing to low control levels of apoptosis in mouse liver. The inhibition of apoptosis may be of importance when altered liver foci are present, as this could enhance lesion growth by an accumulation of hepatocytes and hence liver tumour formation. For example, in studies with male F344 rats and B6C3F1 mice following DEN initiation, subsequent treatment with PB was shown to significantly increase RDS in focal hepatocytes and to significantly decrease rates of apoptosis.82 Because of the technical difficulties in quantifying low levels of apoptosis, data for this associative event should not be considered essential in establishing a CAR activator MOA for rodent liver tumour formation.
The inhibition of gap junctional intercellular communication (GJIC) was considered to represent an associative event or a modulating factor.14 A number of nongenotoxic hepatocarcinogens, including PB/NaPB, have been shown to inhibit GJIC in rodent liver, which may contribute to the process of tumour formation.83,84 In contrast to inhibition of GJIC, oxidative stress was not considered to constitute a key or associative event or a modulating factor. While the treatment of rats with PB/NaPB leads to induction of some CYP enzymes (e.g. CYP2B1, CYP3A2) which can produce hydroxyl radicals, evaluation of the literature does not reveal any distinct role for oxidative stress in the MOA for rodent liver tumour formation by PB/NaPB.14,85
Evaluation of key and associative events using the modified Bradford Hill considerations
The identified key and associative events in the MOA for rodent liver tumour formation by PB/NaPB have been evaluated using the modified Bradford Hill considerations, including dose and temporal concordance, biological plausibility, coherence, strength, consistency and specificity.6,8,14 Clearly effects on key events and also on associative events used as markers for key events should be observed at carcinogenic dose levels, with effects on some key and associative events also possibly being observed at lower noncarcinogenic dose levels. In terms of concordance of dose–response relationships, some data for NaPB and the natural pyrethrins are given in Tables 5 and 6, respectively. NaPB at a dietary level of 1000 ppm was shown to produce liver adenomas and carcinomas after 99 weeks in male C57BL/10J mice, whereas liver tumour incidence was not increased in male mice given 200 ppm NaPB.44 The natural pyrethrins are a mixture of the six active insecticide components of pyrethrum which is derived from the flowers of Chrysanthemum cinerariaefolium. The treatment of female Sprague-Dawley rats with 3000 ppm, but not 100 ppm, natural pyrethrins for 2 years was shown to increase the incidence of liver adenomas and the combined incidence of liver adenomas and carcinomas.22 As shown in Table 5 for NaPB and in Table 6 for the natural pyrethrins, the effects on key and associative events were always observed at the carcinogenic dose levels. For NaPB, a significant increase in the associative event of liver hypertrophy was also observed (after 8, 15 and 29 days and 99 weeks of treatment) at the noncarcinogenic 200 ppm dose level (Table 5). With the natural pyrethrins, the stimulation of RDS was only observed after 7 and 14 days of treatment (based on determination of just the hepatocyte labelling index, see above), whereas effects on liver hypertrophy and CYP2B induction were sustained, being observed after 7, 14 and also 42 days of treatment (Table 6).
Table 5. Dose-dependent effects of NaPB on some key (KE) and associative (AE) events for liver tumour formation in male C57BL/10J mice a .
| Key (KE) or associative (AE) event | NaPB dietary level |
|
| 200 ppm | 1000 ppm | |
| CAR activation (KE) b | No data | No data |
| Increased RDS (KE) c | No | Yes |
| Liver hypertrophy (AE) d | Yes | Yes |
| Clonal expansion leading to altered foci (KE) e | No | Yes |
| Liver adenomas/carcinomas (KE) e | No | Yes |
aData from Jones et al. (2009).44
bWhile activation of CAR was not directly demonstrated, this can be inferred from the increase in liver weight at both NaPB dietary levels and from literature data.
cHepatocyte RDS was evaluated by giving BrdU (single i.p. dose plus in drinking water for 1 day), with significant increases being observed in mice given 1000 ppm NaPB for 3, 8 and 15 days.
dIncreased liver weight was observed in both short-term studies (up to 29 days) and after 99 weeks of treatment.
eLiver foci and tumours were observed after 99 weeks of treatment.
Table 6. Dose-dependent effects of natural pyrethrins on some key (KE) and associative (AE) events for liver tumour formation in female Sprague-Dawley rats a .
| Key (KE) or associative (AE) event | Treatment time | Fold induction or response
b
|
|
| 100 ppm | 3000 ppm | ||
| CAR activation (KE) c | All | No | Yes |
| Increased RDS (KE) d | 7 days | 0.97 | 2.85* |
| 14 days | 0.89 | 2.79* | |
| 42 days | 1.31 | 0.87 | |
| CYP2B enzyme induction (AE) e | 7 days | 1.1 | 5.4* |
| 14 days | 0.9 | 7.5* | |
| 42 days | 1.0 | 9.5* | |
| Liver hypertrophy (AE) f | 7 days | 0.98 | 1.25* |
| 14 days | 1.01 | 1.27* | |
| 42 days | 0.94* | 1.22* | |
| Clonal expansion leading to altered foci (KE) | 2 years | No | Yes |
| Liver adenomas/carcinomas (KE) | 2 years | No | Yes |
aData from Osimitz and Lake (2009).22
bData for effect of 100 and 3000 ppm natural pyrethrins are shown as either fold control animal levels after 7, 14 and 42 days of treatment (values significantly different from control are: *p < 0.05) or as response observed after 2 years of treatment.
cWhile activation of CAR in rats given 3000 ppm natural pyrethrins was not directly demonstrated, this can be inferred from the effects observed in this study on RDS, CYP2B enzyme induction and liver hypertrophy.
dHepatocyte RDS was evaluated using 7 day osmotic pumps (i.e. study days 0–7, 7–14 and 35–42) containing BrdU.
eCYP2B enzyme induction was determined by measurement of hepatic microsomal PROD activity. Treatment with 3000 ppm natural pyrethrins for 7, 14 and 42 days also induced testosterone 16β-hydroxylase (CYP2B) and testosterone 6β-hydroxylase (CYP3A) activities.
fLiver hypertrophy was determined as increase in relative liver weight. Morphological examination of liver sections from rats given 3000 ppm natural pyrethrins revealed hepatocyte hypertrophy at all time points.
In terms of temporal association, if a key event (or events) are an essential element for carcinogenesis, effects on these key event(s) must precede the appearance of liver tumours. The effects of PB/NaPB in rodent liver on the key events of CAR activation, increased hepatocyte RDS and the associative events of liver hypertrophy and induction of CYP2B enzymes are all observed following short term treatment with PB/NaPB. In contrast, the formation of altered liver foci and ultimately hepatocellular adenomas and carcinomas requires prolonged treatment.
A comparison of the MOA for rodent liver tumour formation by PB/NaPB with other modified Bradford Hill considerations including biological plausibility and consideration of alternative MOAs has been performed by Elcombe et al. (2014).14
By use of the established MOA framework and the modified Bradford Hill considerations a number of nongenotoxic compounds have been shown to produce liver tumours in rats and/or mice by a CAR activation MOA similar to that established for PB/NaPB. Some examples are shown in Table 7.20–22,50,86–95 For these compounds effects at carcinogenic dose levels were observed for the key event of increased hepatocyte RDS and the associative events of liver hypertrophy and CYP2B enzyme induction. In some studies the short term effects of the test chemicals were shown to be reversible on cessation of treatment and for some compounds increased numbers of altered hepatic foci were reported in chronic studies. For some compounds the CAR dependence of the hepatic effects observed were demonstrated either in vivo by the used of knockout (KO) animals or in vitro in cultured hepatocytes by use of the RNA interference (siRNA) technique. Two compounds, namely nitrapyrin and pronamide, were shown to be inhibitors of CYP2B enzymes, thus indicating that CYP enzyme induction is best assessed by determination of both CYP enzyme activity and mRNA levels (see below). One compound shown in Table 7, namely pronamide, is unusual as it has been shown to produce liver tumours by both hepatic CAR and PPARα activation.92 However, the activation of both CAR and PPARα produces similar effects on RDS in rodent hepatocytes and many studies have demonstrated that human hepatocytes are refractory to the effects of both rodent CAR (see below) and PPARα activators.9,11,12,14,15,96,97 For metofluthrin, momfluorothrin and nitrapyrin RDS studies were also performed in cultured hepatocytes and for metofluthrin and momfluorothrin in vivo investigations were also performed with chimeric mice with humanised livers (see below). Finally, a CAR activation MOA has also been described for the triazole fungicide propiconazole which has been shown to produce liver tumours in CD-1 mice.98 MOA studies with this compound demonstrated effects on liver hypertrophy and hepatocyte RDS, with propiconazole producing a similar toxicogenomic profile in mouse liver to that observed with NaPB.
Table 7. Some literature examples of nongenotoxic compounds for which a CAR activation MOA has been established for rat and/or mouse liver tumour formation.
| Compound (species) and references a | Parameters examined
b
|
||||
| Liver weight/hypertrophy | RDS | CYP enzymes |
Other endpoints examined c , d | ||
| CYP2B | Other CYPs e | ||||
| Cyproconazole (mouse)86 | Yes | Yes | Yes | Yes | CAR KO mouse study. |
| Fluopyram (rat)50 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. |
| Metofluthrin (rat)20,87–89 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. Gene array study. Humanised mouse study. Rat hepatocyte siRNA study. Rat and human hepatocyte RDS studies. |
| Momfluorothrin (rat)21,90 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. Gene array study. CAR KO rat study. Humanised mouse study. Rat hepatocyte siRNA study. Rat and human hepatocyte studies. |
| Nitrapyrin (mouse)91 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. CAR KO mouse study. Mouse and human hepatocyte RDS studies. |
| Pronamide f (mouse)92 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. PPARα induction markers. |
| Pyrethrins (rat)22,93 | Yes | Yes | Yes | Yes | Recovery study. Altered foci. Rat and human hepatocyte RDS studies. |
| Sulfoxaflor (rat and mouse)94,95 | Yes | Yes | Yes | Yes | Recovery study. Altered foci (mouse). CAR KO/PXR KO and hCAR/hPXR mouse studies. |
aThe species in which liver tumours were observed (rat and/or mouse) is shown in parentheses.
bParameters examined included effects on liver weight/hypertrophy (associative event), hepatocyte RDS (key event) and CYP2B enzyme induction (associative event).
cIn some instances studies were performed with knock out (KO) rats and/or mice lacking either the CAR receptor (CAR KO) or both the CAR and PXR receptors (CAR KO/PXR KO). For metofluthrin and momfluorothrin studies were performed with chimeric mice with humanised livers, whereas for sulfoxafluor investigations were also performed with mice where the mouse hepatic CAR and PXR receptors had been replaced with their human counterparts (hCAR/hPXR mice).
dIn some instances studies were also performed in cultured hepatocytes. For metofluthrin and momfluorothrin the RNA interference (siRNA) technique was used to demonstrate the role of CAR in the induction of CYP2B enzymes. RDS studies in cultured rodent and human hepatocytes were also conducted with some compounds.
eIn addition to effects on CYP2B enzymes, the effect of the test chemical on other CYP subfamily enzymes (e.g. CYP1A, CYP3A and CYP4A) enzymes was also determined.
fUnlike the other compounds shown in this table, pronamide was shown to produced rodent liver tumours by a MOA involving activation of both CAR and PPARα.92
Data required to demonstrate a CAR activation MOA for rodent liver tumour formation
Much of the data required to demonstrate a CAR activator MOA for rodent liver tumour formation can be obtained from short term studies.9–12,14 Data on liver tumour formation will have been obtained from rodent bioassays and data on formation of altered liver foci may be observed from examination of liver section from interim and/or terminal necropsies from bioassay studies. However, as described above, altered liver foci can be considered the precursor lesions for subsequent tumour formation and may not be detected in interim necropsies in a bioassay and also may be difficult to quantify in liver sections from terminal necropsies where numbers of liver adenomas and/or carcinomas are present.
In terms of the key and associative events described above for the MOA for PB-induced rodent liver tumour formation, data are required on CAR activation, RDS in hepatocytes, liver hypertrophy and induction of CYP2B enzymes. Activation of CAR can be either inferred by effects of the test compound on induction of CYP2B enzymes or can be determined experimentally. For example, the CAR-dependence of CYP2B mRNA induction in cultured hepatocytes can be examined with the RNA interference (siRNA) technique and in vitro assays are available for compounds which are direct activators of CAR.20,21,24 A definitive test for the involvement of CAR in the MOA for a compound is the use of CAR knockout animals, of which both rat and mouse CAR KO and CAR KO/PXR KO models are now available.25,63–68
Liver tissue from animals treated with the test compound for a suitable period (e.g. 7, 14, 28 or 90 days) can be used to examine effects on liver hypertrophy (both as effect on liver weight and by morphological examination of liver sections) and on CYP enzymes as markers of activation of CAR and other hepatic receptors. Generally, it is useful to screen compounds for effects on CYP1A, CYP2B, CYP3A and CYP4A subfamily enzymes by determining both CYP enzyme activity and mRNA levels. Good enzymatic markers for CYP1A, CYP2B, CYP3A and CYP4A enzyme induction in the rat and mouse comprise 7-ethoxyresorufin O-deethylase, PROD, BQ or testosterone 6β-hydroxylase and lauric acid 12-hydroxylase, respectively. In terms of CYP4A induction, which is due to PPARα activation, markers of hepatic peroxisome proliferation (e.g. cyanide-insensitive palmitoyl-CoA oxidation as a marker for the peroxisomal fatty acid β-oxidation cycle) may also be useful. Suitable mRNA markers include CYP1A2, CYP2B1, CYP3A1 and CYP4A1 for the rat and Cyp1a2, Cyp2b10, Cyp3a11 and Cyp4a10 for the mouse. CYP induction is best assessed both by enzyme activity and mRNA measurement as a few compounds have been shown to be suicide inhibitors of CYP2B enzymes and hence inductive effects would not have been observed by measurement of enzyme activities alone.91,92 A pivotal key event for the MOA for a CAR activator is to demonstrate that the test compound is a mitogenic agent in rodent liver by determining effects on hepatocyte RDS as described above. Some examples of the endpoints determined to identify a compound as a CAR activator in rodent liver are shown in Table 7. As shown in Table 7 for a number of compounds, recovery studies have also been conducted to demonstrate that the effects of the test compound are reversible on cessation of treatment. Information on the hepatic effects of a test compound can also be obtained from gene array studies, with gene signatures for CAR and also for AhR and PPARα activators having been developed.33,99,100
A major point in developing a CAR activator MOA for rodent liver tumour formation is to be able to exclude alternative MOAs by acquiring appropriate experimental data. Rodent liver CAR activators are not genotoxic agents and produce liver enlargement by a mitogenic stimulation of hepatocyte RDS and not as the result of toxicity leading to a regenerative hyperplasia. As described above, the determination of the effect of the test compound on the induction profile of CYP1A, CYP2B, CYP3A and CYP4A enzymes and mRNA levels, together with additional markers as appropriate (e.g. markers for hepatic peroxisome proliferation) should demonstrate that the test compound is primarily a CAR activator in rodent liver. Data are also required to exclude other possible MOAs for liver tumour formation including hormonal perturbation, immunosuppression and porphyria.9–11,14
Human relevance of CAR activator-induced rodent liver tumours
Concordance analysis
In order to evaluate the human relevance of an animal MOA for liver tumour formation, it is useful to compare the effects of a chemical between rodents and humans on the key and associative events of the rodent MOA.6 Based on the key and associative events described by Elcombe et al. (2014),14 as shown in Table 8, it is clear that some effects of PB/NaPB and indeed other CAR activators can also be observed in human liver. For example, PB/NaPB can clearly activate human CAR and induce hepatic CYP enzymes, including CYP2B6, CYP2C9, CYP2C19 and CYP3A4.18,19,23 Treatment with PB/NaPB and other anticonvulsant drugs has been shown to increase liver size with morphological examination revealing swelling of hepatocytes without any evidence of toxicity and ultrastructural examination revealing a proliferation of the smooth endoplasmic reticulum.101–103 However, the effects of PB/NaPB and other CAR activators that are not observed in human liver comprise the lack of effect on stimulation of hepatocyte RDS, together with no evidence for altered hepatic foci and liver tumour formation.
Table 8. Comparison of some key and associative events for PB/NaPB-induced liver tumour formation between rats and mice and humans.
| Key (KE) or associative (AE) event a | Evidence in rats and mice | Evidence in humans |
| CAR activation (KE) | Yes | Yes |
| Altered gene expression (KE) | Yes | Yes |
| Increased RDS (KE) b | Yes | No |
| CYP2B enzyme induction (AE) | Yes | Yes |
| Liver hypertrophy (AE) | Yes | Yes |
| Inhibition of apoptosis (AE) | Yes | No |
| Clonal expansion leading to altered foci (KE) | Yes | Unlikely |
| Liver adenomas/carcinomas (KE) c | Yes | No |
aKey and associative events taken from Elcombe et al. (2014).14
bEffect on RDS in rats and mice demonstrated in both in vivo studies and in in vitro studies with cultured hepatocytes. Lack of effect in humans demonstrated in in vitro studies in cultured hepatocytes and in in vivo studies in chimeric mice with humanised livers.
cWhile PB/NaPB produced liver tumours in rodent liver, a number of epidemiological studies have demonstrated that PB/NaPB does not increase the incidence of liver tumour formation in humans.
Species differences in RDS in rat, mouse and human hepatocytes
Based on an evaluation of the literature, it is clear that the pivotal key species difference between the effects of PB/NaPB and other CAR activators in rat and mouse liver (as against human liver) is the lack of effect on hepatocyte RDS, which accounts for the subsequent absence of altered hepatic foci and liver tumour formation in human liver. This key species difference has been investigated by both in vitro and in vivo studies performed in a number of laboratories. However, as described below, the results of these studies need to be carefully evaluated with respect to their relevance for liver tumour formation in humans.
PB/NaPB and other rodent CAR activators have been shown in studies conducted in a number of laboratories to stimulate RDS in rat and mouse hepatocytes both after in vivo treatment and in in vitro studies performed in cultured hepatocytes. As described above, data from in vivo studies conducted in rats and mice should not be interpreted as producing only a transient effect on hepatocyte RDS. In terms of providing data on species differences in hepatocyte RDS, studies have been performed in vitro with cultured rodent and human hepatocytes and in vivo both with transgenic mice (where one or more hepatic mouse receptors have been replaced with their human counterparts) and in chimeric mice with humanised livers. Available data from studies with these in vitro and in vivo models are described below.
Cultured hepatocytes
Cultured hepatocytes comprise a very useful in vitro technique for predicting the possible in vivo effects of chemicals and establishing species differences in response. For example, cultured human hepatocytes can be reliably employed to screen therapeutic agents and other chemicals as potential inducers of hepatic CYP enzymes.23,96 In keeping with in vivo findings, a number of studies have demonstrated that PB/NaPB and other CAR activators can stimulate RDS in cultured rat and mouse hepatocytes.22,88–91,104–106 In contrast, while increased RDS can be demonstrated in cultured rat and mouse hepatocytes, human hepatocytes are refractory to stimulation of RDS by PB/NaPB and other CAR activators. Such studies have been performed in a number of laboratories, with the functional viability of the human hepatocyte preparations being demonstrated by significant increases in RDS following treatment with epidermal growth factor (EGF) and/or hepatocyte growth factor (HGF). In some studies the induction of CYP enzymes and/or mRNA levels in cultured human hepatocytes by PB/NaPB and other CAR activators was also demonstrated, as additional markers of the functional viability of the human hepatocyte preparations employed. Some rat, mouse and human hepatocyte data for effect of treatment with NaPB from three different laboratories are shown in Table 9. In all these studies treatment with NaPB produced significant increases in RDS in cultured mouse and/or rat hepatocytes, but did not stimulate RDS in cultured human hepatocyte preparations from 29 subjects. The majority of the human donors were Caucasian subjects, the donors comprising 13 male subjects (age range 26–73 years) and 16 female subjects (age range 0.83–80 years). However, the functional viability of the human hepatocyte preparations used in these studies was demonstrated by significant increases in RDS being observed after treatment with either EGF or HGF. Moreover, in one study, the effect of NaPB on Ki-67 mRNA levels in cultured human hepatocytes was also determined as an additional marker of cell proliferation. While NaPB treatment had no effect in Ki-67 mRNA levels in cultured human hepatocytes from two male and two female Caucasian subjects, the treatment of human hepatocytes with HGF produced significant increases in Ki-67 mRNA levels.89 In four of the studies shown in Table 9, the functional viability of the hepatocyte preparations used was also confirmed by measurement of the effect of NaPB on CYP mRNA and/or enzyme activities. Treatment with NaPB resulted in increases in CYP2B6 mRNA levels in human hepatocytes in three studies and CYP enzyme activities in two studies.
Table 9. Effect of NaPB on RDS and CYP enzymes in cultured rat, mouse and human hepatocytes.
| Hepatocyte RDS
a
|
CYP induction b | Reference | |||
| Rat and mouse c | Human |
||||
| Response d | Positive control e | Subjects sex and age (years) | |||
| Wistar rat↑ | None | EGF | 6 (males 35,41 and 49 and females 45, 55 and 77) f | Not studied | Parzefall et al. (1991)104 |
| Wistar rat↑ | None | EGF and HGF | 2 (females 41 and 63) g | Rat CYP2B1 and human CYP2B6 mRNA levels increased. PROD enzyme activity increased in both species | Hirose et al. (2009)88 |
| Wistar rat↑ | None | HGF | 4 (males 26 and 66 and females 38 and 52) g | Human CYP2B6 mRNA levels increased | Yamada et al. (2015)89 |
| Wistar rat↑ | None | HGF | 10 (males 26, 28, 57, 58 and 66 and females 0.83, 3, 38, 52, and 80) h | Rat CYP2B1/2 and human CYP2B6 mRNA levels increased | Okuda et al. (2017)90 |
| CD-1 mouse↑, C57BL/6J mouse↑ and Sprague-Dawley rat↑ | None | EGF | 7 (males 51, 68 and 73 and females 37,52,57 and 68) g | PROD, BROD and BQ enzyme activities increased in all three species | Haines et al. (2018)106 |
aRDS in cultured rodent and human hepatocytes was studied by treatment with a DNA precursor ([3H]thymidine or BrdU) followed by either determination of the hepatocyte labelling index or by incorporation of BrdU into DNA.
bInduction of CYP enzymes was determined by measurement of either CYP mRNA levels and/or CYP enzyme activities. All these increases were statistically significant except for the effect of NaPB on rat CYP2B1 and human CYP2B6 mRNA levels in the study of Hirose et al. (2009)88 where only two replicates were evaluated.
cSignificant increases (indicated by ↑) in RDS were observed in all studies with rat and mouse hepatocytes.
dHepatocyte RDS was not increased cultured human hepatocytes.
eSignificant increases in RDS in rat, mouse and human hepatocytes were observed in all studies following treatment with either EGF or HGF, with the exception of the study of Hirose et al. (2009)88 where the effects of EGF and HGF were only examined in human hepatocytes.
fEthnicity of human hepatocyte donors was not specified.
gHuman hepatocyte donors were all Caucasian subjects.
hAll 10 hepatocyte preparations were used for RDS studies, whereas CYP induction studies were conducted with 7 hepatocyte preparations. All human hepatocyte donors were Caucasian subjects, with the exception of one 0.83 years (10 months) old female Hispanic donor.
Apart from the data shown in Table 9 for NaPB, a number of other CAR activators including α-hexachlorocyclohexane, metofluthrin, momfluorothrin, nitrapyrin and the natural pyrethrins have been shown to stimulate RDS in cultured rodent hepatocytes, but not in human hepatocytes.22,88–91,104 In another study, Wistar rat, CD-1 mouse and human (from 3 donors) hepatocytes were cultured in an optimised defined medium with RDS being determined using the nucleoside analogue 5-ethynyl-2′-deoxyuridine.107 While treatment with either CITCO or TCPOBOP stimulated RDS in both rat and mouse hepatocytes, these two CAR activators had no effect on RDS in cultured human hepatocytes. Under these experimental conditions treatment with CITCO was shown to induce CYP2B6 mRNA levels in cultured human hepatocytes, the effect of TCPOBOP not being studied.
In addition to the studies described above, many unpublished studies (including submissions made to regulatory authorities by various agrochemical companies) have also demonstrated that human hepatocytes are refractory to the mitogenic effects of PB/NaPB and other rodent CAR activators. However, as a positive control in these investigations, treatment with either EGF or HGF was shown to stimulate RDS in cultured human hepatocytes. As an additional measure of the viability of the human hepatocyte preparations used in these various studies, PB/NaPB and other CAR activators have been shown to induce CYP2B and other CYP enzymes in rat and mouse hepatocytes and also in human hepatocytes. Moreover, these studies have been performed in a number of laboratories employing different experimental conditions.
Transgenic mice
Studies aimed at investigating in vivo species differences in RDS produced by PB/NaPB and other CAR activators have been conducted in transgenic mice containing human hepatic PXR and/or CAR receptors and also in chimeric mice with humanised livers (see below). The application of genetically humanised mice and chimeric mice with humanised livers for studies of xenobiotic metabolism and toxicity have been reviewed.66,108–111 The treatment of hCAR mice (i.e. where mouse CAR has been replaced by human CAR) with 500 ppm PB in the diet for one week was reported to result in increased Cyp2b10 mRNA levels and hepatocyte RDS.65 Studies have also been performed with transgenic mice, where both mouse CAR and mouse PXR have been replaced with their human counterparts (hCAR/hPXR mice).25,66,108 In this mouse model, the expression of human CAR and PXR in the liver was at physiological levels and splice variants of both human receptors were expressed.25,66 The treatment of hCAR/hPXR mice with either NaPB (80 mg kg–1 day–1 by i.p. injection) or chlordane (100 mg kg–1 day–1 by gavage) for 4 days resulted in liver hypertrophy and an induction of Cyp2b and Cyp3a enzyme activities and Cyp2b10 and Cyp3a11 protein levels, but unlike wild type (C57BL/6J) mice, neither NaPB nor chlordane stimulated RDS in the hCAR/hPXR mice.25 In another study, hCAR/hPXR mice were given 0.05% PB in the drinking water for periods of 1–91 days.112 PB treatment resulted in a sustained induction of hepatic Cyp2b10 mRNA levels in hCAR/hPXR mice and a transient induction of DNA replication and mitotic genes, with peak expression occurring between 1 and 7 days of treatment. Braeuning et al. (2014)74 conducted an initiation/promotion study in wild type and hCAR/hPXR mice. Wild type and hCAR/hPXR mice were give a single 90 mg kg–1 i.p. injection of the known genotoxin DEN followed one week later by administration of either 0 (control) or 0.05% (500 ppm) PB in the diet for 40 weeks. While PB promoted DEN-initiated liver tumours in both wild type and hCAR/hPXR mice, tumour incidence, assessed as either multiplicity or tumour volume fraction, was less marked in the hCAR/hPXR mice. These findings could be interpreted that the human CAR and PXR receptors could support PB-induced tumour promotion in mouse liver, although it needs to be recognised that the two human receptors are operating in a mouse hepatocyte environment.74
In summary, in one study with hCAR mice PB was shown to increase hepatocyte RDS, whereas in two studies with hCAR/hPXR mice PB/NaPB produced equivocal results. However, as described below, the apparent lack of induction of hepatocyte RDS by NaPB in hCAR/hPXR mice in the study of Ross et al. (2010)25 is attributable to the dose and treatment time employed. In another study, the hepatic effects of NaPB at dietary levels of 186, 496, 654 and 984 ppm for 7 days were compared in male C57BL/6J (wild type) and hCAR/hPXR mice.106 Treatment with NaPB produced liver hypertrophy and induction of hepatic microsomal Cyp2b and Cyp3a enzyme activities in both wild type and hCAR/hPXR mice. While treatment with 184–984 ppm NaPB in the diet produced significant dose-dependent increases in hepatocyte RDS in wild type mice, significant increases in hepatocyte RDS were only observed in hCAR/hPXR mice at NaPB dietary levels of 496–984 ppm. In addition, the magnitude of stimulation of RDS was less marked in hCAR/hPXR than in wild type mice at all dietary NaPB levels examined.
Overall, treatment with PB/NaPB can induce RDS in hepatocytes from hCAR and hCAR/hPXR transgenic mice. However, recent studies with hCAR/hPXR mice clearly demonstrate that hepatocytes from this transgenic mouse model are less responsive to PB/NaPB induction of RDS than those from wild type mice.
Chimeric mice with humanised livers
In addition to the transgenic mouse models containing human genes described above, chimeric mouse models where human hepatocytes are transplanted into immunocompromised mice have been developed. One such model is the urokinase-type plasminogen activator/severe combined immunodeficient (uPA/SCID) mouse model which has been employed for various xenobiotic metabolism and toxicity studies.108–111 It is possible to achieve a high replacement index of mouse with human hepatocytes in this model, with the human hepatocytes being responsive to mitogens such as EGF.90,108,109,113
The in vivo effects of NaPB administered at dietary levels of 500–2500 ppm for 7 days were studied in male chimeric mice with humanised livers (utilising human hepatocytes from a female Hispanic donor aged 2 years) and also in male Wistar rats and male CD-1 mice.113 Due to toxicity in the chimeric mice the maximum tolerated dose of NaPB was 1500 ppm in the diet. However, plasma levels of PB in chimeric mice with humanised livers given 1000 and 1500 ppm NaPB were some 3–5 fold higher than those observed in human subjects given therapeutic doses of PB.113,114 Treatment with NaPB significantly increased hepatic CYP2B1/2 and CYP3A1 mRNA levels in Wistar rats, Cyp2b10 and Cyp3a11 mRNA levels in CD-1 mice and CYP2B6 and CYP3A4 mRNA levels in chimeric mice with humanised livers. While treatment with NaPB resulted in significant increases in hepatocyte RDS in Wistar rats and CD-1 mice, RDS was not increased in the human hepatocytes of the chimeric mice. In addition, NaPB increased hepatic mRNA levels of some cell cycling genes (e.g. Ki-67, PCNA and Gadd 45β) in the livers of Wistar rats and CD-1 mice, but had no effect in the human hepatocytes of the chimeric mice. However, as positive controls, NaPB did increase RDS in hepatocytes of SCID mice and treatment with human EGF did increase RDS and Ki-67 mRNA levels in human hepatocytes of the chimeric mice.
Recently, some additional studies were performed with this humanised mouse model employing the known CAR activators metofluthrin and momfluorothrin.90 Three separate studies were performed utilising hepatocytes from a male Caucasian donor aged 2 years, a male African American donor aged 5 years and a female Hispanic donor aged 2 years. The animals were treated with 1800 ppm metofluthrin and either 1100 or 3000 ppm momfluorothrin in the diet for 7 days, these dose levels resulting in compound intakes either similar to or higher than those which produced liver tumours in the rat bioassays of these two synthetic pyrethroids. Treatment with both metofluthrin and momfluorothrin stimulated Cyp2b10 mRNA levels in mouse hepatocytes and in some instances also increased CYP2B6 mRNA levels in the human hepatocytes of the chimeric mice. While treatment with metofluthrin and momfluorothrin resulted in significant decreases in RDS in human hepatocytes, treatment with human EGF resulted in significant increases in RDS in the human hepatocytes of the chimeric mice.
In another recent study, analysis of DNA methylation, hydroxymethylation and gene expression was undertaken in liver samples from male C3H/He mice given a single dose of DEN followed by treatment with NaPB at dietary levels of 0 (control) and 500 ppm for 27 weeks, together with liver samples from male CD-1 mice given 0 and 2500 ppm NaPB and from male chimeric mice with humanised livers given 0 and 1000 ppm NaPB for 7days.113,115 After DEN initiation, the treatment of C3H/He mice with 500 ppm NaPB for 27 weeks resulted in the formation of hepatocellular adenomas. In this study, while some cell proliferation/growth related genes were increased in CD-1 mice and in NaPB-promoted mouse liver adenomas, these genes were not increased in NaPB-treated humanised mice, thus suggesting a clear species difference between the effects of NaPB in mouse and human hepatocytes.115
Overall, the studies with chimeric mice with humanised livers demonstrate that while human hepatocytes were refractory to the mitogenic effects of NaPB, metofluthrin and momfluorothrin, the functional viability of the human hepatocytes to a mitogen were demonstrated by significant increases in human hepatocyte RDS following treatment with human EGF. In addition, in a study of candidate genes responsible for early key events in NaPB-promoted mouse liver tumour formation, the gene changes produced by NaPB in human hepatocytes of chimeric mice were found not to overlap with those observed in normal mice.
Other species differences between experimental animals and humans
Many studies have compared the effects of PB/NaPB and other CAR activators observed in rat and mouse liver with those observed in human liver. However, data has also been obtained in studies with other species which support the conclusion that effects of CAR activators in rat and mouse liver are not relevant for humans. Like the rat and mouse, liver microsomes from the Syrian hamster and guinea pig contain CYP2B subfamily enzymes which are inducible by treatment with PB.12,14,116,117 Although PB/NaPB has been shown to stimulate RDS in cultured rat and mouse hepatocytes, no such effects of PB were observed in either Syrian hamster or guinea pig hepatocytes.105 In addition, while PB inhibited apoptosis in cultured rat hepatocytes, no suppression of either spontaneous or transforming growth factor β1-induced apoptosis was observed in either Syrian hamster or guinea pig hepatocytes.105
While PB is an inducer of hepatic CYP2B subfamily enzymes in the Syrian hamster, the treatment of Syrian hamsters with 500 ppm in the drinking water for 69 weeks did not result in the formation of either hepatocellular adenomas or carcinomas.118 Moreover, unlike studies conducted in adult rats and mice, PB is not a promoter of genotoxin-induced liver lesions in the Syrian hamster. For example, treatment with PB did not promote liver lesions induced in the Syrian hamster following treatment with either DEN, DMN or methylazoxymethanol acetate.118,119 In another study, Syrian hamsters were given a single dose of DMN followed by treatment with either PB, DDT or the cytotoxic agent carbon tetrachloride.120 Although the two mitogenic CYP2B inducers PB and DDT had no effect on subsequent liver foci or tumour formation, treatment with carbon tetrachloride enhanced the formation of altered foci and liver tumours, presumably due to stimulation of a regenerative hyperplasia following treatment with this cytotoxic agent.
Human epidemiology studies
PB has been used as a sedative, hypnotic and antiepileptic drug in humans for many years and hence data are available from a number of epidemiological studies.37,38,121 In subjects receiving therapeutic doses of PB (3–6 mg kg–1), blood levels of PB are similar to those which produce liver tumours in mice.114 Based on an evaluation of human epidemiological studies published up to 1995, IARC concluded that there was inadequate evidence in humans for the carcinogenicity of PB.38 However, in a much more recent evaluation of the available literature, La Vecchia and Negri (2014)121 concluded that “epidemiological data on phenobarbital and liver cancer are limited, but indicate an absence of any specific association and, in any case, allow the exclusion of an appreciable excess risk”. The key point here is that while a large number of human subjects have been studied, the power of the studies is limited by the low observed incidence of human liver tumours. However, the human epidemiological studies performed would have had sufficient power to detect an increase in liver tumours in human subjects given PB.
In terms of other rodent CAR activators, oxazepam is known to have similar effects on CYP enzymes and hepatocyte RDS in mouse liver to those produced by PB/NaPB and on prolonged administration produces hepatocellular adenomas and carcinomas in B6C3F1 mice.122 However, in one human epidemiological study, no association was observed between oxazepam treatment and liver tumour formation in humans.123
Discussion
PB and its sodium salt NaPB are model CAR activators and have been investigated in many studies conducted in experimental animals and humans. PB/NaPB and a large number of other CAR activators are not genotoxic agents. Treatment with PB/NaPB and other CAR activators results in the induction of hepatic xenobiotic metabolising enzymes (particularly CYP2B subfamily enzymes) in both rodents and other species including humans.
Several investigators have described MOAs for rat and mouse liver tumour formation by PB/NaPB and other CAR activators.5,9–12,14,20–22,86,87,90–95,98 Overall, these various MOAs are not at variance with that proposed by Elcombe et al. (2014)14 for PB/NaPB. While a number of evaluations have concluded that the MOA for rat and mouse liver tumour formation by PB/NaPB and other CAR activators is either qualitatively or quantitatively not plausible for humans, others have suggested that this is not the case, with the human relevance of the MOA for rat and mouse liver tumour formation by PB/NaPB and other CAR activators being considered as highly controversial.73–75,124–126
As described in this review, based on a critical evaluation of the published literature, there is a clear fundamental species difference between the mitogenic response observed in rats and mice to PB/NaPB and other CAR activators and the effects of these compounds in human hepatocytes and in hepatocytes from other species. In establishing this species difference, data has been obtained from in vitro studies with cultured rat, mouse and human hepatocytes and from in vivo studies with chimeric mice with humanised livers. However, as discussed below, the data obtained from these in vitro and in vivo models appear to be at variance with some in vivo data obtained with transgenic mice (where one or more hepatic mouse receptors have been replaced with their human counterparts).
In terms of studies with cultured hepatocytes an argument might be made that such cultures do not reflect the in vivo situation due to lack of other cell types, culture conditions etc. However, the use of cultured human hepatocytes is well established and certainly is a model used by the pharmaceutical industry to effectively screen compounds for their ability to induce CYP enzymes in human liver.23,96 As described in this review, studies with PB/NaPB and other CAR activators in human hepatocytes have been performed in several laboratories employing different experimental conditions, with all studies demonstrating that while PB/NaPB and other CAR activators do not induce RDS in human hepatocytes, RDS can be produced by treatment with mitogenic agents such as EGF and HGF. Moreover, as shown in Table 9 and in other studies, these investigations have been conducted with a large number of male and female human hepatocyte preparations from a wide donor age range.22,88–91,104,106,107
That cultured human hepatocytes are refractory to stimulation of RDS by PB/NaPB and other CAR activators is clearly supported by in vivo studies in chimeric mice with humanised livers, but not by some studies with transgenic mice where one or more hepatic mouse receptors have been replaced with their human counterparts. As described above, the CAR activators NaPB, metofluthrin and momfluorothrin did not stimulate RDS in human hepatocytes of chimeric mice with humanised livers, whereas RDS was increased after treatment with human EGF. Moreover, in the NaPB study a maximum tolerated dose was clearly achieved with PB plasma levels being some 3–5 fold higher than those observed in human subjects given therapeutic doses of PB.113,114 In contrast, studies in transgenic mice with human PXR and/or CAR receptor(s) have yielded contradictory results. While PB increased RDS in one study with hCAR mice, in investigations with hCAR/hPXR mice NaPB, chlordane, cyproconazole, prochloraz and sulfoxaflor have been reported not to induce RDS (determined as an increase in the hepatocyte labelling index); whereas in other studies treatment with NaPB has been reported to increase RDS in hepatocytes from hCAR/hPXR mice.25,65,75,94,95,106 In these studies, the effects of cyproconazole and prochloraz are somewhat difficult to interpret as the effect on the hepatocyte labelling index was only investigated employing Ki-67 immunocytochemistry after 28 days of treatment, whereas an earlier time point would have been more desirable to assess the acute effect of treatment with the test chemicals on the hepatocyte labelling index.75 As demonstrated by a recent NaPB dose–response study, RDS can be stimulated by treatment with NaPB for 7 days in hCAR/hPXR mice, although the effect on RDS is less marked that that observed in wild type mice.106 Indeed while the treatment of WT mice with 186–984 ppm NaPB for 7 days produced statistically significant dose-dependent increases in hepatocyte RDS, no increase in RDS was observed in hCAR/hPXR mice given 186 ppm NaPB, with much smaller increases in RDS compared to WT mice being observed in hCAR/hPXR mice given 496–984 ppm NaPB.106
Overall, with both cultured human hepatocytes and in human hepatocytes of chimeric mice with humanised livers, the human CAR and other receptors are acting in a human hepatocyte environment. This is not case with either hCAR or hCAR/hPXR mice, where the human receptors function in the context of mouse target gene regulatory elements and chromatin structure and hence gene regulation protein interactions may differ from human hepatocytes mouse gene regulatory elements.74,112 As cited by Cohen (2017),10 the mathematician George Box stated that “models are all wrong, some are useful”. Here we have three experimental models, one in vitro model with cultured human hepatocytes, together with two in vivo models, namely transgenic mice (where one or more hepatic mouse receptors have been replaced with their human counterparts) and chimeric mice with humanised livers. Based on the available data, it can be concluded that either the hCAR or the hCAR/hPXR mouse do not comprise suitable animal models for studies on the hepatic effects of nongenotoxic rodent CAR activators. That human hepatocytes are refractory to the mitogenic effects of NaPB and other rodent CAR activators, has been clearly demonstrated by studies performed in a number of laboratories with cultured human hepatocytes and in in vivo studies performed in chimeric mice with humanised livers. However, when present in a mouse hepatocyte environment human PXR and/or CAR receptors appear to be able to exhibit a mitogenic response to rodent CAR activators.
In one study liver tumours were observed after DEN initiation followed by PB promotion in both wild type and hCAR/hPXR mice, with tumour incidence, assessed as either multiplicity or tumour volume fraction, being less marked in hCAR/hPXR mice compared to wild type mice.74
The results of this study are not surprising as the human CAR and PXR receptors are operating in a mouse hepatocyte environment. Indeed, the magnitude of liver tumour formation being more marked in wild type than in hCAR/hPXR mice correlates with the dose–response effects of NaPB, where the stimulation of hepatocyte RDS was clearly more marked in wild type than in hCAR/hPXR mice.106 In the hCAR/hPXR mouse initiation/promotion model the human CAR and PXR receptors are operating in a mouse hepatocyte regulatory environment, which includes gene interactions leading to increased hepatocyte RDS and hence promotion of DEN-initiated liver lesions. Thus in the hCAR/hPXR mouse DEN initiation/CAR activator model described by Braeuning et al. (2014),74 one would expect other CAR activators (e.g. CITCO) at sufficient dosage to also promote liver tumours with the same morphological characteristics as those observed in the study with PB.
In addition to the clear difference between rat and mouse hepatocytes, compared to human hepatocytes, in the mitogenic response to PB/NaPB and other CAR activators, other species such as the Syrian hamster and guinea pig are also refractory to the mitogenic effects of rat and mouse CAR activators. Moreover, studies in the Syrian hamster have also demonstrated that PB does not produce liver tumours and also does not promote liver tumours after initiation with known genotoxic agents. In assessing species differences to the mitogenic effects of CAR activators, the rat and mouse should be considered as outliers, with humans like other species in being nonresponsive to the mitogenic effects of rat and mouse liver CAR activators. There is thus a clear species difference in gene regulation, with activation of human CAR only leading to some effects (e.g. CYP enzyme induction), but not to a mitogenic effect resulting in hepatocyte proliferation.
The observed species differences in the hepatic effects of CAR activators are analogous to those produced by PPARα activators. While treatment with PPARα activators can result in a hypolipidaemic effect in both rodents and humans, these compounds only stimulate RDS in rat and mouse hepatocytes and not in hepatocytes from other species including humans, Syrian hamsters, guinea pigs and primates.9,11,12,15,96,97
One other aspect of the importance of the stimulation of RDS being the pivotal key event in the MOA for rat and mouse liver tumour formation by PB/NaPB and other CAR activators is that the stimulation of cell proliferation in hepatocytes is not transient as has been reported in the literature.37,38,73–75,126 PB/NaPB and other CAR activators stimulate cell proliferation assessed as the hepatocyte labelling index at early time points (e.g. 3 or 7 days of treatment), but generally not at longer time points (e.g. 28 or 90 days of treatment).21,22,37,38,44,70–72 However, as described in this review, PB/NaPB and other CAR activators produce a sustained increase in liver weight in treated animals, with treated animals having greater numbers of hepatocytes per animal than control animals. Thus even if the labelling index returns to control levels, there will still be an increase in overall cell proliferation per animal following treatment with PB/NaPB and other CAR activators.9,10,12,14
PB was classified by IARC in 2001 into Group 2B as being possibly carcinogenic to humans, based on there being inadequate evidence in humans for the carcinogenicity of PB, but sufficient evidence in experimental animals for the carcinogenicity of PB.38 The current IARC classification of PB may thus be interpreted that PB might be carcinogenic for humans.73,124 However, this IARC assessment was the result of a meeting conducted in October 2000 which occurred before the development of currently accepted MOA frameworks and the publication of much PB/NaPB MOA data including the development of chimeric mouse models with humanised livers.4–8,14,90,113 In addition, the epidemiological studies examined by IARC comprised only those published up to 1995, with a much more recent evaluation of available human PB epidemiology studies concluding that “epidemiological data on phenobarbital and liver cancer are limited, but indicate an absence of any specific association and, in any case, allow the exclusion of an appreciable excess risk”.121 Based on current knowledge, the existing IARC evaluation of PB would appear to be outdated.
While an evaluation of the available human epidemiological studies indicates that PB/NaPB and other CAR activators do not increase the incidence of liver cancer in humans, it has been suggested that PB/NaPB might act as a tumour selector, by promoting the formation of one type of tumour while inhibiting the formation of another type.73,124,126 In terms of inhibition of liver tumour formation, the results of PB/NaPB promotion studies conducted in young mice after initiation with a genotoxin are equivocal. Although treatment with PB/NaPB may result in an inhibition of liver tumour formation after genotoxin treatment in young mice, this effect is only observed in some studies and is clearly dependent on many factors, including the experimental design, the age, sex and strain of the animals used and the genotoxin employed.37,38,56–62 Based on these observations, it is difficult to utilise such contradictory young rodent data to make any reliable predictions of what may or may not occur in humans.
Comparisons have also been made between the role of β-catenin in the formation of both mouse and human liver tumours. The Wnt/β-catenin signalling pathway regulates key aspects of mammalian cell biology, the dysregulation of which can lead to tumour formation in the liver and other organs.127,128 The treatment of mice with DEN followed by subsequent PB promotion has been shown to result in a high incidence of liver tumours containing β-catenin mutations.129 The adenomatous polyposis coli (Apc) protein is a negative regulator of β-catenin.130 When Apc-deficient mice were given a single dose of tamoxifen, subsequent PB treatment significantly promoted the outgrowth of Apc-deficient hepatocellular adenomas, whereas PB simultaneously inhibited the formation of Apc-deficient hepatocellular carcinomas.130 In another study, the combined activation of β-catenin and CAR resulted in mouse liver tumours that showed an extensive gene expression signature with those of β-catenin positive human hepatocellular carcinomas.128 These two studies suggest that under certain conditions PB can influence the formation of adenomas as against carcinomas in mouse liver and also that combining the activation of β-catenin and CAR can result in mouse liver tumours with a similar gene expression signature to those observed in β-catenin-positive human hepatocellular carcinomas.128,130 There is certainly more scope for investigations to compare the gene expression profiles of rat and mouse liver tumours with human liver tumours. While the mouse liver tumours produced in the study of Dong et al. (2015)128 had a similar gene expression signature to those observed in β-catenin-positive human hepatocellular carcinomas, differences in gene expression profiles have been observed between the effects of NaPB in chimeric mice with humanised livers, compared to NaPB treated CD-1 mice and to NaPB-promoted mouse liver adenomas.115 In this study, while some cell proliferation/growth related genes were increased in CD-1 mice and in NaPB-promoted mouse liver adenomas, these genes were not increased in NaPB-treated humanised mice.115 Moreover, while the expression of many genes related to the Wnt/β-catenin signalling network were altered in NaPB treated CD-1 mice and in NaPB-promoted mouse liver adenomas, fewer genes were altered in the human hepatocytes of the chimeric mice.115 Overall, while the Wnt/β-catenin signalling pathway is implicated in the formation of some mouse and human liver tumours, a key species difference exists between the mitogenic function of CAR in stimulating cell proliferation in rodent hepatocytes as against human hepatocytes. As such, data derived from Apc-deficient mouse studies and from investigations where both β-catenin and CAR are activated in mouse liver may not be relevant for assessing the risk to humans of PB/NaPB-induced liver tumour formation.
Overall, the available epidemiological data demonstrates that PB/NaPB does not increase the incidence of liver tumours in humans.121 For PB/NaPB, the treatment of human subjects with therapeutic doses has been shown to result in similar blood levels to those which produce liver tumours in mice.114 However, for other CAR activators, including metofluthrin, momfluorothrin and the natural pyrethrins, likely human exposure to such compounds are orders of magnitude below the dose levels which are required in order to produce liver tumours in rodents.22,87,90 Thus for many CAR activators, the MOA established for liver tumour formation by Elcombe et al. (2014)14 is both qualitatively (i.e. on the basis of the species difference in cell proliferation) and also quantitatively (i.e. on the basis of likely human exposure) not plausible for humans.
In summary, a robust MOA for rodent liver tumour formation by PB/NaPB and other CAR activators has been established.14 Although CAR activators can produce liver tumours in the rat and/or mouse, the MOA for rodent liver tumour formation is qualitatively not plausible for humans. The key species difference is that while such compounds induce RDS in rat and mouse hepatocytes, other species including humans are refractory to the mitogenic effects of rodent CAR activators and thus would not be expected to be carcinogenic in humans. This conclusion is supported by available epidemiological data in humans chronically exposed to PB.
Conflicts of interest
The author has no conflicts of interest to declare. The production of this paper has not been funded by any academic, commercial or other organisation.
Acknowledgments
I should like to thank my colleagues Professor Samuel Cohen (University of Nebraska Medical Center, Omaha, Nebraska, USA) and Dr Tomoya Yamada (Sumitomo Chemical Company Limited, Osaka, Japan) for many valuable and stimulating discussions on the human relevance of a CAR activation MOA for rodent liver tumour formation. This review is dedicated to the memory of Dr Clifford R. Elcombe. The author is proud to have known Cliff for very many years and to have been able to collaborate with Cliff in various studies on the hepatic effects of both CAR and PPARα activators. Cliff was an excellent scientist and had a great sense of humour. He will be remembered for his many contributions to toxicology, in particular for his studies on the hepatic effects of nongenotoxic compounds, including the use of hepatocyte culture techniques.
Biography

Brian G. Lake
Professor Brian G. Lake holds BSc, PhD and DSc degrees from the University of Surrey (Guildford, UK) and is a Fellow of the British Toxicology Society. He is a Visiting Professor in the Faculty of Health and Medical Sciences at the University of Surrey and is a member of the UK Committee on Toxicity (COT). A major focus of his research has been investigations into the mode of action of chemicals which are activators of either the constitutive androstane receptor (CAR) or the peroxisome proliferator-activated receptor alpha (PPARα) in rodent liver and the relevance of rodent liver tumours produced by such compounds to humans.
References
- Huff J., Cirvello J., Haseman J., Bucher J. Environ. Health Perspect. 1991;93:247–270. doi: 10.1289/ehp.9193247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold L. S., Manley N. B., Slone T. H., Ward J. M. Toxicol. Pathol. 2001;29:639–652. doi: 10.1080/019262301753385979. [DOI] [PubMed] [Google Scholar]
- Gold L. S., Manley N. B., Slone T. H., Rohrbach L., Garfinkel G. B. Toxicol. Sci. 2005;85:747–808. doi: 10.1093/toxsci/kfi161. [DOI] [PubMed] [Google Scholar]
- Meek B. E., Bucher J. R., Cohen S. M., Dellarco V., Hill R. N., Lehman-McKeeman L. D., Longfellow D. G., Pastoor T., Seed J., Patton D. E. Crit. Rev. Toxicol. 2003;33:591–653. doi: 10.1080/713608373. [DOI] [PubMed] [Google Scholar]
- Holsapple M. P., Pitot H. C., Cohen S. M., Boobis A. R., Klaunig J. E., Pastoor T., Dellarco V. L., Dragan Y. P. Toxicol. Sci. 2006;89:51–56. doi: 10.1093/toxsci/kfj001. [DOI] [PubMed] [Google Scholar]
- Boobis A. R., Cohen S. M., Dellarco V., McGregor D., Meek M. E., Vickers C., Willcocks D., Farland W. Crit. Rev. Toxicol. 2006;36:781–792. doi: 10.1080/10408440600977677. [DOI] [PubMed] [Google Scholar]
- Andersen M. E., Preston R. J., Maier A., Willis A. M., Paterson J. Crit. Rev. Toxicol. 2014;44:50–63. doi: 10.3109/10408444.2013.835785. [DOI] [PubMed] [Google Scholar]
- Meek M. E., Boobis A., Cote I., Dellarco V., Fotakis G., Munn S., Seed J., Vickers C. J. Appl. Toxicol. 2014;34:1–8. doi: 10.1002/jat.2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. M. Toxicol. Pathol. 2010;38:487–501. doi: 10.1177/0192623310363813. [DOI] [PubMed] [Google Scholar]
- Cohen S. M. Curr. Opin. Toxicol. 2017;3:6–11. [Google Scholar]
- Cohen S. M., Arnold L. L. Toxicol. Sci. 2011;120(S1):S76–S92. doi: 10.1093/toxsci/kfq365. [DOI] [PubMed] [Google Scholar]
- Lake B. G. Xenobiotica. 2009;39:582–596. doi: 10.1080/00498250903098184. [DOI] [PubMed] [Google Scholar]
- Budinsky R. A., Schrenk D., Simon T., Van den Berg M., Reichard J. F., Silkworth J. B., Aylward L. L., Brix A., Gasiewicz T., Kaminski N., Perdew G., Starr T. B., Walker N. J., Rowlands J. C. Crit. Rev. Toxicol. 2014;44:83–119. doi: 10.3109/10408444.2013.835787. [DOI] [PubMed] [Google Scholar]
- Elcombe C. R., Peffer R. C., Wolf D. C, Bailey J., Bars R., Bell D., Cattley R. C., Ferguson S. S., Geter D., Goetz A., Goodman J. I., Hester S., Jacobs A., Omiecinski C. J., Schoeny R., Xie W., Lake B. G. Crit. Rev. Toxicol. 2014;44:64–82. doi: 10.3109/10408444.2013.835786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corton J. C., Cunningham M. L., Hummer B. T., Lau C., Meek B., Peters J. M., Popp J. A., Rhomberg L., Seed J., Klaunig J. E. Crit. Rev. Toxicol. 2014;44:1–49. doi: 10.3109/10408444.2013.835784. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC), IARC monographs on the evaluation of carcinogenic risk to humans. Some naturally occurring substances: food items and constituents, heterocyclic aromatic amines and mycotoxins, 1993, vol. 56, pp. 245–395. [Google Scholar]
- Yoshinari Y., Tien E., Negishi M. and Honkakoski P., Receptor-mediated regulation of cytochromes P450, in Cytochromes P450: role in the metabolism and toxicity of drugs and other xenobiotics, ed. C. Ioannides, RSC Publishing, Cambridge, UK, 2008, pp. 417–448. [Google Scholar]
- Martignoni M., Groothuis G. M. M., de Kanter R. Expert Opin. Drug Metab. Toxicol. 2006;2:875–894. doi: 10.1517/17425255.2.6.875. [DOI] [PubMed] [Google Scholar]
- Omiecinski C. J., Vanden Heuvel J. P., Perdew G. H., Peters J. M. Toxicol. Sci. 2011;120(S1):S49–S75. doi: 10.1093/toxsci/kfq338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deguchi Y., Yamada T., Hirose Y., Nagahori H., Kushida M., Sumida K., Sukata T., Tomigahara Y., Nishioaka N., Uwagara S., Kawamura S., Okuno Y. Toxicol. Sci. 2009;108:69–80. doi: 10.1093/toxsci/kfp006. [DOI] [PubMed] [Google Scholar]
- Okuda Y., Kushida M., Sumida K., Nagahori H., Nakamura Y., Higuchi H., Kawamura S., Lake B. G., Cohen S. M., Yamada T. Toxicol. Sci. 2017;158:412–430. doi: 10.1093/toxsci/kfx102. [DOI] [PubMed] [Google Scholar]
- Osimitz T. G., Lake B. G. Crit. Rev. Toxicol. 2009;39:501–511. doi: 10.1080/10408440902914014. [DOI] [PubMed] [Google Scholar]
- Pelkonen O., Turpeinen M., Hakkola J., Honkakoski P., Hukkanen J., Raunio H. Arch. Toxicol. 2008;82:667–715. doi: 10.1007/s00204-008-0332-8. [DOI] [PubMed] [Google Scholar]
- Omiecinski C. J., Coslo D. M., Chen T., Laurenzana E. M., Peffer R. C. Toxicol. Sci. 2011;123:550–562. doi: 10.1093/toxsci/kfr191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J., Plummer S. M., Rode A., Scheer N., Bower C. C., Vogel O., Henderson C. J., Wolf C. R., Elcombe C. R. Toxicol. Sci. 2010;116:452–466. doi: 10.1093/toxsci/kfq118. [DOI] [PubMed] [Google Scholar]
- Negishi M. Drug Metab. Dispos. 2017;45:532–539. doi: 10.1124/dmd.116.074872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutoh S., Osabe M., Inoue K., Moore R., Pedersen L., Perera L., Rebolloso Y., Sueyoshi T., Negishi M. J. Biol. Chem. 2009;284:34785–34792. doi: 10.1074/jbc.M109.048108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutoh S., Sobhany M., Moore R., Perera L., Pedersen L., Sueyoshi T., Negishi M. Sci. Signaling. 2013;6:ra31. doi: 10.1126/scisignal.2003705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzameli I., Pissios P., Schuetz E. G., Moore D. D. Mol. Cell. Biol. 2000;20:2951–2958. doi: 10.1128/mcb.20.9.2951-2958.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maglich J. M., Parks D. J., Moore L. B., Collins J. L., Goodwin B., Billin A. N., Stoltz C. A., Kliewer S. A., Lambert M. H., Willson T. M., Moore J. T. J. Biol. Chem. 2003;278:17277–17283. doi: 10.1074/jbc.M300138200. [DOI] [PubMed] [Google Scholar]
- Nims R. W., Sinclair P. R., Sinclair J. F., Dragnev K. H., Jones C. R., Mellini D. W., Thomas P. E., Lubet R. A. Xenobiotica. 1993;23:1411–1426. doi: 10.3109/00498259309059450. [DOI] [PubMed] [Google Scholar]
- Diwan B. A., Henneman J. R., Rice J. M., Nims R. W. Carcinogenesis. 1996;17:37–43. doi: 10.1093/carcin/17.1.37. [DOI] [PubMed] [Google Scholar]
- Oshida K., Vasani N., Jones C., Moore T., Hester S., Nesnow S., Auerbach S., Geter D. R., Aleksunes L. M., Thomas R. S., Applegate D., Klaassen C. D., Corton J. C. Nucl. Recept. Signaling. 2015;13:e002. doi: 10.1621/nrs.13002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore L. B., Parks D. J., Jones S. A., Bledsoe R. K., Consler T. G., Stimmel J. B., Goodwin B., Liddle C., Blanchard S. G., Willson T. M., Collins J. L., Kliewer S. A. J. Biol. Chem. 2000;275:15122–15127. doi: 10.1074/jbc.M001215200. [DOI] [PubMed] [Google Scholar]
- Maglich J. M., Stoltz C. M., Goodwin B., Hawkins-Brown D., Moore J. T., Kliewer S. A. Mol. Pharmacol. 2002;62:638–646. doi: 10.1124/mol.62.3.638. [DOI] [PubMed] [Google Scholar]
- Moore J. T., Moore L. B., Maglich J. M., Kliewer S. A. Biochim. Biophys. Acta. 2003;1619:235–238. doi: 10.1016/s0304-4165(02)00481-6. [DOI] [PubMed] [Google Scholar]
- Whysner J., Ross P. M., Williams G. M. Pharmacol. Ther. 1996;71:153–191. doi: 10.1016/0163-7258(96)00067-8. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC), IARC monographs on the evaluation of carcinogenic risk to humans. Some thyrotropic agents, 2001, vol. 79, pp. 161–288. [PMC free article] [PubMed] [Google Scholar]
- Maronpot R. R. J. Toxicol. Pathol. 2009;22:11–33. doi: 10.1293/tox.22.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geter D. R., Bhat V. S., Gollapudi B. B., Sura R., Hester S. D. Toxicol. Sci. 2014;138:425–445. doi: 10.1093/toxsci/kfu014. [DOI] [PubMed] [Google Scholar]
- Lodato N. J., Melia T., Rampersaud A., Waxman D. J. Toxicol. Sci. 2017;159:25–41. doi: 10.1093/toxsci/kfx114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe E., Walker A. I. T. Food Chem. Toxicol. 1972;11:433–442. doi: 10.1016/0015-6264(73)90008-4. [DOI] [PubMed] [Google Scholar]
- Becker F. F. Cancer Res. 1982;42:3918–3923. [PubMed] [Google Scholar]
- Jones H. B., Orton T. C., Lake B. G. Food Chem. Toxicol. 2009;47:1333–1340. doi: 10.1016/j.fct.2009.03.014. [DOI] [PubMed] [Google Scholar]
- Evans J. G., Collins M. A., Savage S. A., Lake B. G., Butler W. H. Carcinogenesis. 1986;7:627–631. doi: 10.1093/carcin/7.4.627. [DOI] [PubMed] [Google Scholar]
- Evans J. G., Collins M. A., Lake B. G., Butler W. H. Toxicol. Pathol. 1992;20:585–594. doi: 10.1177/019262339202000405. [DOI] [PubMed] [Google Scholar]
- Butler W. H. Br. J. Cancer. 1978;37:418–423. doi: 10.1038/bjc.1978.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara A., Miyata E., Tamano S., Sano M., Masuda C., Funae Y., Ito N., Fukushima S., Shirai T. Food Chem. Toxicol. 1999;37:869–879. doi: 10.1016/s0278-6915(99)00072-1. [DOI] [PubMed] [Google Scholar]
- Rossi L., Ravera M., Repetti G., Santi L. Int. J. Cancer. 1977;19:179–185. doi: 10.1002/ijc.2910190207. [DOI] [PubMed] [Google Scholar]
- Tinwell H., Rouquié D., Schorsch F., Geter D., Wason S., Bars R. Regul. Toxicol. Pharmacol. 2014;70:648–658. doi: 10.1016/j.yrtph.2014.09.011. [DOI] [PubMed] [Google Scholar]
- Ward J. M. J. Natl. Cancer Inst. 1983;71:815–823. [PubMed] [Google Scholar]
- Ward J. M., Lynch P., Riggs C. Cancer Lett. 1988;39:9–18. doi: 10.1016/0304-3835(88)90035-3. [DOI] [PubMed] [Google Scholar]
- Schulte-Hermann R., Timmermann-Trosiener I., Schuppler J. Cancer Res. 1983;43:839–844. [PubMed] [Google Scholar]
- Peraino C., Fry R. J. M., Staffeldt E., Christopher J. P. Cancer Res. 1975;35:2884–2890. [PubMed] [Google Scholar]
- Kolaja K. L., Stevenson D. E., Walborg Jr. E. F., Klaunig J. E. Carcinogenesis. 1996;17:1243–1250. doi: 10.1093/carcin/17.6.1243. [DOI] [PubMed] [Google Scholar]
- Lee G.-H. Toxicol. Pathol. 2000;28:215–225. doi: 10.1177/019262330002800201. [DOI] [PubMed] [Google Scholar]
- Diwan B. A., Rice J. M., Ward J. M., Ohshima M., Lynch P. H. Cancer Lett. 1984;23:223–234. doi: 10.1016/0304-3835(84)90157-5. [DOI] [PubMed] [Google Scholar]
- Pereira M. A., Klaunig J. E., Herren-Freund S. L., Ruch R. J. J. Natl. Cancer Inst. 1986;77:449–452. [PubMed] [Google Scholar]
- Klaunig J. E., Weghorst C. M., Pereira M. A. Toxicol. Appl. Pharmacol. 1987;90:79–85. doi: 10.1016/0041-008x(87)90308-5. [DOI] [PubMed] [Google Scholar]
- Weghorst C. M., Klaunig J. E. Carcinogenesis. 1989;10:609–612. doi: 10.1093/carcin/10.3.609. [DOI] [PubMed] [Google Scholar]
- Weghorst C. M., Pereira M. A., Klaunig J. E. Carcinogenesis. 1989;10:1409–1412. doi: 10.1093/carcin/10.8.1409. [DOI] [PubMed] [Google Scholar]
- Klaunig J. E., Pereira M. A., Ruch R. J., Weghorst C. M. Toxicol. Pathol. 1988;16:381–385. doi: 10.1177/019262338801600310. [DOI] [PubMed] [Google Scholar]
- Wei P., Zhang J., Egan-Hafley M., Liang S., Moore D. D. Nature. 2000;407:920–923. doi: 10.1038/35038112. [DOI] [PubMed] [Google Scholar]
- Yamamoto Y., Moore R., Goldsworthy T. L., Negishi M., Maronpot R. R. Cancer Res. 2004;64:7197–7200. doi: 10.1158/0008-5472.CAN-04-1459. [DOI] [PubMed] [Google Scholar]
- Huang W., Zhang J., Washington M., Liu J., Parant J. M., Lozano G., Moore D. D. Mol. Endocrinol. 2005;19:1646–1653. doi: 10.1210/me.2004-0520. [DOI] [PubMed] [Google Scholar]
- Scheer N., Ross J., Rode A., Zevnik B., Niehaves S., Faust N., Wolf C. R. J. Clin. Invest. 2008;118:3228–3239. doi: 10.1172/JCI35483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes K. P., Kouranova E., Tinker D., Janowski K., Cortner D., McCoy A., Cui X. Drug Metab. Dispos. 2017;45:1068–1076. doi: 10.1124/dmd.117.075788. [DOI] [PubMed] [Google Scholar]
- Haines C., Chatham L. R., Vardy A., Elcombe C. R., Foster J. R., Lake B. G. Xenobiotica. 2018 doi: 10.1080/00498254.2018.1437300. [DOI] [Google Scholar]
- Wood C. E., Hukkanen R. R., Sura R., Jacobson-Kram D., Nolte T., Odin M., Cohen S. M. Toxicol. Pathol. 2015;43:760–775. doi: 10.1177/0192623315576005. [DOI] [PubMed] [Google Scholar]
- Kolaja K. L., Stevenson D. E., Johnson J. T., Walborg Jr. E. F., Klaunig J. E. Fundam. Appl. Toxicol. 1996;29:219–228. doi: 10.1006/faat.1996.0025. [DOI] [PubMed] [Google Scholar]
- Orton T. C., Doughty S. E., Kalinowski A. E., Lord P. G., Wadsworth P. F. Carcinogenesis. 1996;17:973–981. doi: 10.1093/carcin/17.5.973. [DOI] [PubMed] [Google Scholar]
- Phillips J. C., Price R. J., Cunninghame M. E., Osimitz T. G., Cockburn A., Gabriel K. L., Preiss F. J., Butler W. H., Lake B. G. Fundam. Appl. Toxicol. 1997;38:64–74. doi: 10.1006/faat.1997.2326. [DOI] [PubMed] [Google Scholar]
- Braeuning A. Arch. Toxicol. 2014;88:1771–1772. doi: 10.1007/s00204-014-1331-6. [DOI] [PubMed] [Google Scholar]
- Braeuning A., Gavrilov A., Brown S., Wolf C. R., Henderson C. J., Schwarz M. Toxicol. Sci. 2014;140:259–270. doi: 10.1093/toxsci/kfu099. [DOI] [PubMed] [Google Scholar]
- Marx-Stoelting P., Ganzenberg K., Knebel C., Schmidt F., Rieke S., Hammer H., Schmidt F., Pötz O., Schwarz M., Braeuning A. Arch. Toxicol. 2017;91:2895–2907. doi: 10.1007/s00204-016-1925-2. [DOI] [PubMed] [Google Scholar]
- Carthew P., Edwards R. E., Nolan B. M. Toxicol. Sci. 1998;44:46–51. doi: 10.1006/toxs.1998.2473. [DOI] [PubMed] [Google Scholar]
- Williams G. M., Carcinogenic responses to toxic liver injury in rodents, in Comprehensive Toxicology. Volume 9. Hepatic and Gastrointestinal Toxicology, ed. R. S. McCuskey and D. L. Earnest, Pergamon, Oxford, UK, 1997, pp. 165–179. [Google Scholar]
- Thoolen B., ten Kate F. J. W., van Diest P. J., Malarkey D. E., Elmore S. A., Maronpot R. R. J. Toxicol. Pathol. 2012;25:189–199. doi: 10.1293/tox.25.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nims R. W., Devor D. E., Henneman J. R., Lubet R. A. Carcinogenesis. 1987;8:67–71. doi: 10.1093/carcin/8.1.67. [DOI] [PubMed] [Google Scholar]
- Rice J. R., Diwan B. A., Hu H., Ward J. M., Nims R. W., Lubet R. A. Carcinogenesis. 1994;15:395–402. doi: 10.1093/carcin/15.2.395. [DOI] [PubMed] [Google Scholar]
- Li L., Bao X., Zhang Q.-Y., Negishi M., Ding X. Drug Metab. Dispos. 2017;45:977–981. doi: 10.1124/dmd.117.076406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolaja K. L., Stevenson D. E., Walborg Jr. E. F., Klaunig J. E. Carcinogenesis. 1996;17:947–954. doi: 10.1093/carcin/17.5.947. [DOI] [PubMed] [Google Scholar]
- Klaunig J. E., Ruch R. J., Weghorst C. M. Toxicol. Appl. Pharmacol. 1990;102:553–563. doi: 10.1016/0041-008x(90)90050-5. [DOI] [PubMed] [Google Scholar]
- Chipman J. K., Mally A., Edwards G. O. Toxicol. Sci. 2003;71:146–153. doi: 10.1093/toxsci/71.2.146. [DOI] [PubMed] [Google Scholar]
- Imaoka S., Osada M., Minamiyama Y., Yukimura T., Toyokuni S., Takemura S., Hiroi T., Funae Y. Cancer Lett. 2004;203:117–125. doi: 10.1016/j.canlet.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Peffer R. C., Moggs J. G., Pastoor T., Currie R. A., Wright J., Milburn G., Waechter F., Rusyn I. Toxicol. Sci. 2007;99:315–325. doi: 10.1093/toxsci/kfm154. [DOI] [PubMed] [Google Scholar]
- Yamada T., Uwagawa S., Okuno Y., Cohen S. M., Kaneko H. Toxicol. Sci. 2009;108:59–68. doi: 10.1093/toxsci/kfp007. [DOI] [PubMed] [Google Scholar]
- Hirose Y., Nagahori H., Yamada T., Deguchi Y., Tomigahara Y., Nishioka K., Uwagawa S., Kawamura S., Isobe N., Lake B. G., Okuno Y. Toxicology. 2009;258:64–69. doi: 10.1016/j.tox.2009.01.007. [DOI] [PubMed] [Google Scholar]
- Yamada T., Kikumoto H., Lake B. G., Kawamura S. Toxicol. Res. 2015;4:901–913. [Google Scholar]
- Okuda Y., Kushida M., Kikumoto H., Nakamura Y., Higuchi H., Kawamura S., Cohen S. M., Lake B. G., Yamada T. J. Toxicol. Sci. 2017;42:773–788. doi: 10.2131/jts.42.773. [DOI] [PubMed] [Google Scholar]
- LaRocca J. L., Rasoulpour R. J., Gollapudi B. B., Eisenbrandt D. L., Murphy L.A., LeBaron M. J. Toxicol. Rep. 2017;4:586–597. doi: 10.1016/j.toxrep.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBaron M. J., Rasoulpour R. J., Gollapudi B. B., Sura R., Kan H. L., Schisler M. R., Pottenger L. H., Papineni S., Eisenbrandt D. L. Toxicol. Sci. 2014;142:74–92. doi: 10.1093/toxsci/kfu155. [DOI] [PubMed] [Google Scholar]
- Price R. J., Walters D. G., Finch J. M., Gabriel K. L., Capen C. C., Osimitz T. G., Lake B. G. Toxicol. Appl. Pharmacol. 2007;218:186–195. doi: 10.1016/j.taap.2006.11.004. [DOI] [PubMed] [Google Scholar]
- LeBaron M. J., Geter D. R., Rasoulpour R. J., Gollapudi B. B., Thomas J., Murray J., Kan H. L., Wood A. J., Elcombe C., Vardy A., McEwan J., Terry C., Billington R. Toxicol. Appl. Pharmacol. 2013;270:164–173. doi: 10.1016/j.taap.2013.04.009. [DOI] [PubMed] [Google Scholar]
- LeBaron M. J., Gollapudi B. B., Terry C., Billington R., Rasoulpour R. J. Crit. Rev. Toxicol. 2014;44(S2):15–24. doi: 10.3109/10408444.2014.910751. [DOI] [PubMed] [Google Scholar]
- Lake B. G. and Price R. J., Induction of hepatic cytochrome P450 enzymes: importance in drug development and toxicity, in New horizons in predictive drug metabolism and pharmacokinetics, ed. A. G. E. Wilson, RSC Publishing, Cambridge, UK, 2016, pp. 309–332. [Google Scholar]
- Corton J. C., Peters J. M., Klaunig J. E. Arch. Toxicol. 2018;92:83–119. doi: 10.1007/s00204-017-2094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie R. A., Peffer R. C., Goetz A. K., Omiecinski C. J., Goodman J. I. Toxicology. 2014;321:80–88. doi: 10.1016/j.tox.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshida K., Vasani N., Thomas R. S., Applegate D., Gonzalez F. J., Aleksunes L. M., Klaasssen C. D., Corton J. C. Toxicology. 2015;336:99–112. doi: 10.1016/j.tox.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshida K., Vasani N., Thomas R. S., Applegate D., Rosen M., Abbott B., Lau C., Guo G., Aleksunes L. M., Klaassen C., Corton J. C. PLoS One. 2015;10:e0112655. doi: 10.1371/journal.pone.0112655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirttiaho H. I., Sotaniemi E. A., Ahokas J. T., Pitkänen U. Br. J. Clin. Pharmacol. 1978;6:273–278. doi: 10.1111/j.1365-2125.1978.tb04597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirttiaho H. I., Sotaniemi E. A., Pelkonen R. O., Pitkänen U. Eur. J. Clin. Pharmacol. 1982;22:441–445. doi: 10.1007/BF00542550. [DOI] [PubMed] [Google Scholar]
- Aiges H. W., Daum F., Olson M., Kahn E., Teichberg S. J. Pedriatr. 1980;97:22–26. doi: 10.1016/s0022-3476(80)80123-5. [DOI] [PubMed] [Google Scholar]
- Parzefall W., Erber E., Sedivy R., Schulte-Hermann R. Cancer Res. 1991;51:1143–1147. [PubMed] [Google Scholar]
- James N. H., Roberts R. A. Carcinogenesis. 1996;17:1623–1632. doi: 10.1093/carcin/17.8.1623. [DOI] [PubMed] [Google Scholar]
- Haines C., Elcombe B. M., Chatham L. R., Vardy A., Higgins L., Elcombe C. R., Lake B. G. Toxicology. 2018;396–397:23–32. doi: 10.1016/j.tox.2018.02.001. [DOI] [PubMed] [Google Scholar]
- Soldatow V., Peffer R. C., Trask O. J., Cowie D. E., Andersen M. E., LeCluyse E., Deisenroth C. Toxicol. In Vitro. 2016;36:224–237. doi: 10.1016/j.tiv.2016.08.006. [DOI] [PubMed] [Google Scholar]
- Scheer N., Wilson I. D. Drug Discovery Today. 2016;21:250–263. doi: 10.1016/j.drudis.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Foster J. R., Lund G., Sapelnikova S., Tyrrell D. L., Kneteman N. M. Xenobiotica. 2014;44:109–122. doi: 10.3109/00498254.2013.867553. [DOI] [PubMed] [Google Scholar]
- Kitamura S., Sugihara K. Xenobiotica. 2014;44:123–134. doi: 10.3109/00498254.2013.868062. [DOI] [PubMed] [Google Scholar]
- Miyamoto M., Iwasaki S., Chisaki I., Nakagawa S., Amano N., Hirabayashi H. Xenobiotica. 2017;47:1052–1063. doi: 10.1080/00498254.2016.1265160. [DOI] [PubMed] [Google Scholar]
- Luisier R., Lempiäinen H., Scherbichler N., Braeuning A., Geissler M., Dubost V., Müller A., Scheer N., Chibout S.-D., Hara H., Picard F., Theil D., Couttet P., Vitobello A., Grenet O., Grasl-Kraupp B., Ellinger-Ziegelbauer H., Thomson J. P., Meehan R. R., Elcombe C. R., Henderson C. J., Wolf C. R., Schwarz M., Moulin P., Terranova R., Moggs J. G. Toxicol. Sci. 2014;139:501–511. doi: 10.1093/toxsci/kfu038. [DOI] [PubMed] [Google Scholar]
- Yamada T., Okuda Y., Kushida M., Sumida K., Takeuchi H., Nagahori H., Fukuda T., Lake B. G., Cohen S. M., Kawamura S. Toxicol. Sci. 2014;142:137–157. doi: 10.1093/toxsci/kfu173. [DOI] [PubMed] [Google Scholar]
- Monro A. Regul. Toxicol. Pharmacol. 1993;18:115–135. doi: 10.1006/rtph.1993.1048. [DOI] [PubMed] [Google Scholar]
- Ohara A., Takahashi Y., Kondo M., Okuda Y., Takeda S., Kushida M., Kobayashi K., Sumida K., Yamada T. Toxicol. Res. 2017;6:795–813. doi: 10.1039/c7tx00163k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J. H., Rush G. F., Hook J. B. Toxicology. 1986;38:209–218. doi: 10.1016/0300-483x(86)90122-8. [DOI] [PubMed] [Google Scholar]
- Oguri K., Kaneko H., Tanimoto Y., Yamada H., Yoshimura H. Arch. Biochem. Biophys. 1991;287:105–111. doi: 10.1016/0003-9861(91)90394-x. [DOI] [PubMed] [Google Scholar]
- Diwan B. A., Ward J. M., Anderson L. M., Hagiwara A., Rice J. M. Toxicol. Appl. Pharmacol. 1986;86:298–307. doi: 10.1016/0041-008x(86)90060-8. [DOI] [PubMed] [Google Scholar]
- Stenbäck F., Mori H., Furuya K., Williams G. M. J. Natl. Cancer Inst. 1986;76:327–333. [PubMed] [Google Scholar]
- Tanaka T., Mori H., Williams G. M. Carcinogenesis. 1987;8:1171–1178. doi: 10.1093/carcin/8.9.1171. [DOI] [PubMed] [Google Scholar]
- La Vecchia C., Negri E. Eur. J. Cancer Prev. 2014;23:1–7. doi: 10.1097/CEJ.0b013e32836014c8. [DOI] [PubMed] [Google Scholar]
- Griffin R. J., Dudley C. N., Cunningham M. L. Fundam. Appl. Toxicol. 1996;29:147–154. doi: 10.1006/faat.1996.0016. [DOI] [PubMed] [Google Scholar]
- Friedman G. D., Jiang S.-F., Udaltsova N., Quesenberry Jr. C. P., Chan J., Habel L. A. Int. J. Cancer. 2009;125:2172–2178. doi: 10.1002/ijc.24545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braeuning A., Schwarz M. Arch. Toxicol. 2016;90:1525–1526. doi: 10.1007/s00204-016-1712-0. [DOI] [PubMed] [Google Scholar]
- Groll N., Petrikat T., Vetter S., Wenz C., Dengjel J., Gretzmeier C., Weiss F., Poetz O., Joos T. O., Schwarz M., Braeuning A. Toxicology. 2016;370:94–105. doi: 10.1016/j.tox.2016.09.018. [DOI] [PubMed] [Google Scholar]
- Braeuning A., Hendersen C. J., Wolf C. R., Schwarz M. Toxicol. Sci. 2015;147:299–300. [PubMed] [Google Scholar]
- Thompson M. D., Monga S. P. S. Hepatology. 2007;45:1298–1305. doi: 10.1002/hep.21651. [DOI] [PubMed] [Google Scholar]
- Dong B., Lee J.-S., Park Y.-Y., Yang F., Xu G., Huang W., Finegold M. J., Moore D. D. Nat. Commun. 2015;6:5944. doi: 10.1038/ncomms6944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydinlik H., Nguyen T. D., Moennikes O., Buchmann A., Schwarz M. Oncogene. 2001;20:7812–7816. doi: 10.1038/sj.onc.1204982. [DOI] [PubMed] [Google Scholar]
- Braeuning A., Gavrilov A., Geissler M., Wenz C., Colnot S., Templin M. F., Metzger U., Römer M., Zell A., Schwarz M. Arch. Toxicol. 2016;90:1481–1494. doi: 10.1007/s00204-016-1667-1. [DOI] [PubMed] [Google Scholar]


