Abstract
Vitamin D is a fat-soluble vitamin playing a vital role in human physiology. Vitamin D deficiency is prevalent worldwide. This deficiency has many consequences which are still being explored, apart from the well-known skeletal complications. With this review, we aim to summarize the existing literature on Vitamin D status in India and understand the enormity of the problem. The prevalence of Vitamin D deficiency ranged from 40% to 99%, with most of the studies reporting a prevalence of 80%–90%. It was prevalent in all the age groups and high-risk groups alike. With the consequences of Vitamin D deficiency, namely, autoimmune diseases, cardiovascular diseases, cancer, and tuberculosis being explored, we can imagine the burden it would cause in our country. We need to create awareness among the public and healthcare providers about the importance of Vitamin D and the consequences of deficiency. Our Indian diet generally fails to satisfy the daily requirement of Vitamin D for a normal adult. This stresses on the need for fortifying various food with Vitamin D, through the national programs. This silent epidemic should be addressed appropriately with concrete public health action.
Keywords: Fortification, India, prevalence, Vitamin D deficiency
Vitamin D is a fat-soluble vitamin, known for its antirachitic activity.[1] Calciferols are a group of lipid-soluble compounds with a 4-ringed cholesterol backbone and refer to both, Vitamin D3, i.e., cholecalciferol and Vitamin D2, i.e., ergocalciferol.[2] Vitamin D, in general, refers to Vitamin D3. Vitamin D can be synthesized endogenously. About 90% of the required Vitamin D is synthesized in the skin under sun exposure.[3]
It is needed for the maintenance of normal blood levels of calcium and phosphate that are required for normal mineralization of bone, muscle contraction, nerve conduction, and general cellular function in all cells of the body. It is also found to be important for immune function, for inflammation, cell proliferation, and differentiation.[3,4]
The active form of Vitamin D stimulates the absorption of calcium in the duodenum and increases calcium influx in distal tubules of kidney through nuclear Vitamin D receptor (VDR); latter is specifically regulated by parathormone level.[5]
Sources of Vitamin D3
The major source of Vitamin D is the endogenous synthesis in skin on exposure to sunlight, namely, ultraviolet B (UV-B) radiation of wavelength 290–320 nm. Main dietary sources are fish, fortified food, and supplements. Vegetables and grains are poor sources.
Synthesis of vitamin in skin on exposure to UV-B is also affected by latitude, solar zenith angle, atmospheric pollution, ozone layer, and melanin pigmentation.[6]
Metabolism
In the skin, ultraviolet light catalyzes conversion of 7-dehydrocholesterol to Vitamin D3, which is released into the bloodstream, in bound form (along with Vitamin D-binding protein).[3,4,7]
From the blood, it reaches liver to form 25-hydroxyvitamin D(25(OH)D). This is followed by formation of 1, 25-dihydroxyvitamin D, the most active form of Vitamin D in the kidney by hydroxylation and in some other tissues in which the mechanism is unclear.
Formation of 1, 25 dihydroxyvitamin D, is the key step in regulating Vitamin D metabolism, which is increased by low serum phosphate concentrations and low serum calcium, mediated by parathyroid hormone. Cellular receptors for active form of Vitamin D are found in intestine, bone, and in many other tissues also.
25(OH)D is the most useful measure and reflects the Vitamin D status in the body because the level depends on the available and circulating Vitamin D.[8] The level of 1, 25 dihydroxyvitamin D is also a direct measure for assessing Vitamin D status; however, it is not used because of its regulation by calcium, phosphate, and parathyroid hormone concentrations. The half-life of 1, 25 dihydroxyvitamin D, calciferol, and 25(OH)D are 4 h, 24 h, and 3 weeks, respectively.
Clinical manifestation of rickets occurs only when there is severe Vitamin D deficiency. The sunlight exposure can be the most important determinant of 25(OH)D concentrations. Seasonal variation should be considered as there is difference in summer and winter season.
Vitamin D Status in Relation to 25-Hydroxyvitamin D Levels
Adequate levels of serum 25(OH) D is essential to maintain the skeletal and extraskeletal physiologic effects. The threshold levels of serum 25(OH) D required to optimize its effects may not be the same in the various target organs. According to the classification given by the US Endocrine Society, <20 ng/mL of serum 25(OH) D with consequent and consistent elevation of parathyroid hormone and a decrease in intestinal calcium absorption is considered to be Vitamin D deficiency.[9] The diagnostic cutoffs of levels of serum Vitamin D are indicated in Table 1.[9]
Table 1.
Diagnostic cut-offs of levels of serum Vitamin D
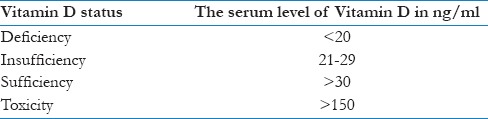
Desirable and safe range of serum 25(OH) D level would be 30–100 ng/mL as at serum 25(OH) D levels of 30 ng/mL intestinal calcium absorption reaches its peak, and PTH levels continue to fall until this level of 25(OH) D is attained.[6,10]
Magnitude of Vitamin D Deficiency in India
The prevalence of Vitamin D deficiency is reported worldwide, both in sunshine deficient and sunshine sufficient countries. Still, it is the most underdiagnosed and undertreated nutritional deficiency in the world.[11,12] However, various studies showed poor Vitamin D status irrespective of age, sex, and geography. As there is no standard guideline which is followed all over the world for classifying the Vitamin D status, these studies had different cutoff values for the deficiency. The vast majority of these studies used serum 25(OH) D level of <20 ng/ml as Vitamin D deficiency. Studies which used other cutoffs have been so indicated in footnotes.
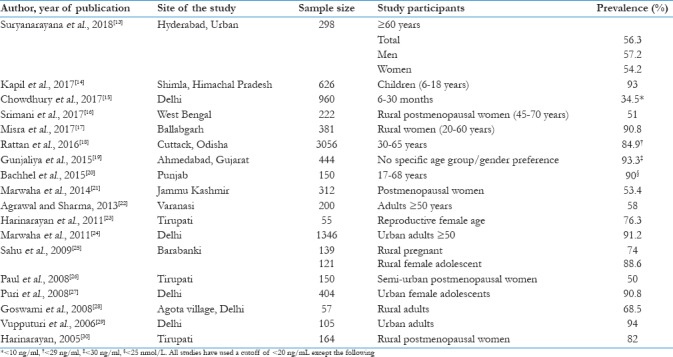
The community-based Indian studies of the past decade done on apparently healthy controls reported a prevalence ranging from 50% to 94%, except for one study which reported a prevalence of 34.5% which can be due to the low cutoff. These studies which included various age groups reflect the magnitude of the problem. High prevalence was seen throughout the country[13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] [Table 2].
Table 2.
Community-based studies on prevalence of Vitamin D deficiency in India
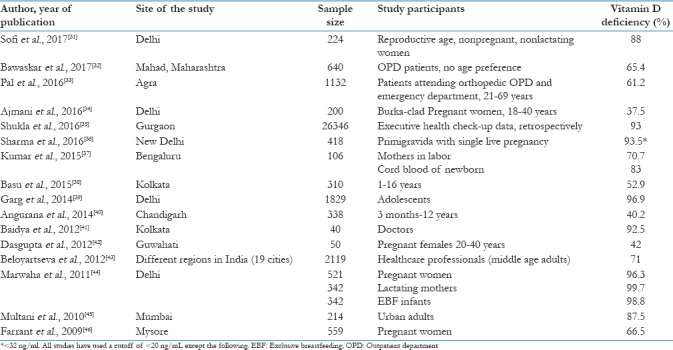
Hospital-based studies showed a prevalence of Vitamin D deficiency ranging from 37% to 99%.[31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] Studies on Vitamin D deficiency in specific disease conditions have been excluded from the study [Table 3].
Table 3.
Hospital-based studies on the prevalence of Vitamin D deficiency in India
A school-based study on premenarchal girls (n = 214) in Pune was conducted by Kadam et al. in 2011. It showed a prevalence of 34.2% of Vitamin D.[47] Another school-based study done by Kapil et al. in 2017 on 1222 school children aged 6–18 years in Kangra and Kullu districts of Himachal Pradesh, showed the prevalence of 81% and 80% respectively.[14] Both the studies reported the prevalence of Vitamin D deficiency based on the U. S. Endocrine Society cutoff.[9]
Causes of Vitamin D Deficiency
It is evident from the above tables that Vitamin D deficiency is quite rampant in India. Apart from low intake in diet, people with liver, kidney and skin disorders also have Vitamin D deficiency. There are many reasons for it being so common in our country.
Increased indoor lifestyle, thereby preventing adequate exposure to sunlight. This is mainly in the urban population due to modernization.
Pollution can hamper the synthesis of Vitamin D in the skin by UV rays[48]
Changing food habits contribute to low dietary calcium and Vitamin D intake
Phytates and phosphates which are present in fiber rich diet, can deplete Vitamin D stores and increase calcium requirement[49]
Increased skin pigmentation and application of sunscreens
Cultural practices such as the burqa and purdah system[34]
Unspaced and unplanned pregnancies in women with dietary deficit can lead to worsening of Vitamin D status in both mother and child.
Consequences of Vitamin D Deficiency
Vitamin D deficiency results in a variety of skeletal and extraskeletal manifestations. Very few Indian studies have been published on the consequences of Vitamin D deficiency. Hence, overseas studies on this issue are cited.
Skeletal manifestations
The commonly known consequences of Vitamin D deficiency are rickets in children and osteomalacia and osteoporosis in adults. In children, it causes defective mineralization of bone due to imbalance between calcium and phosphorous in the bone, resulting in rickets and external skeletal deformity. It also causes muscle weakness and bone pain. In adults, inadequate dietary intake of Vitamin D leads to poor absorption of calcium from diet and increased calcium resorption from the bone and kidney and reduces bone mineral density resulting in osteoporosis and osteomalacia, muscle weakness and increased risk of falls. It is theorized that Vitamin D may increase muscle strength, thereby preventing falls. Many studies have shown an association between low Vitamin D concentrations and an increased risk of fractures and falls in older adults.[50,51,52,53]
Depression
Vitamin D deficient patients took significantly longer duration for recovery than nondeficient persons. It signifies the importance of treating hypovitaminosis D for the effective management of depression.[54]
Parkinson's disease
Vitamin D insufficiency was seen in patients with Parkinson's disease (PD). Evidence suggests VDR as a genetic risk factor for PD, thereby underlining the potential importance of Vitamin D in PD. As Vitamin D status is a modifiable factor, Vitamin D acts as a potential preventive/therapeutic strategy for this disorder. However, there is a need for further studies on VDR as well as its interaction with Vitamin D levels in PD.[55,56,57]
Suicide
Lower 25(OH) D levels are associated with an increased risk for suicide.[58]
Infectious disease
Infectious disease such as tuberculosis, upper respiratory tract infections of viral origin, i.e., influenza is seen in individuals with Vitamin D deficiency.[59,60,61]
Autoimmune diseases
Vitamin D is a potent modulator of immune system, and it is involved in regulating cell proliferation and differentiation.[62,63,64] It was shown in a case–control study that Vitamin D deficiency was considerably higher in Type 1 diabetic (91%) children when compared to nondiabetic (85%) children. Supplementation of Vitamin D resulted in 30% reduction in the risk of developing Type 1 diabetes mellitus. Lower levels of Vitamin D were found to be associated with rheumatoid arthritis.[50]
Cancer
Vitamin D has a protective role in certain tissues by promoting apoptosis and inhibiting angiogenesis. Low level of Vitamin D in stores, such as lung, breast, colorectal, prostate, ovary, pancreas and esophagus, are associated with cancers. Vitamin D decreases cell proliferation and increases cell differentiation. It stops the growth of new blood vessels and has significant anti-inflammatory effects.[65,66,67]
Heart disease
In the Framingham Heart Study, patients with low Vitamin D concentrations (<15 ng/Ml) had a 60% higher risk of heart disease (through the renin-angiotensin hormone system) than those with higher concentrations. Severe Vitamin D deficiency is seen in patients with acute myocardial infarction and it is associated with many of its risk factors.[68,69]
Type 2 diabetes mellitus
Vitamin D deficiency has been associated with increased risk of type 2 diabetes mellitus, insulin resistance, and decreased insulin production, and hence, it has been associated with syndrome X. A trial of nondiabetic patients aged 65 years and older found that those who received 700 IU of Vitamin D (plus calcium) had a smaller rise in fasting plasma glucose over 3 years versus those who received placebo. Evidence reveals that Vitamin D reduces the risk of progression and development of type 2 diabetes mellitus.[70,71,72]
Obesity
Levels of 25(OH) D are inversely associated with body mass index, waist circumference, and body fat but are positively associated with age, lean body mass, and Vitamin D intake.[73,74,75]
The Way Forward
Although we are aware of the causes of Vitamin D deficiency, we are not able to prevent it to a large extent. India being a tropical country has adequate sunshine. Most of the Indian population live in areas with adequate sunlight throughout the year and are expected to have adequate Vitamin D. Contrary to this, the prevalence of Vitamin D deficiency is high in India.
This is due to the skin complexion, poor exposure to sunlight, sunscreen creams, Indian dietary habits and lower intake of Vitamin D fortified foods.[48] Indians are mostly vegetarians and Vitamin D rich foods are of animal origin. All the above-mentioned factors can be a cause in urban population. However, the rural population, who by the virtue of their occupation have sufficient sunlight exposure, too have low Vitamin D levels. This can be due to the high phytate and low calcium diet they consume. Phytate rich diet is known to reduce the intestinal absorption of calcium. Hence, low dietary calcium increases the catabolism of 25(OH) D and increases the inactive metabolites with the resultant reduction in 25(OH)D concentrations.[49,76]
This calls for appropriate and concrete public health action. The following measures can be taken to reduce the burden of the disease.
Food fortification with Vitamin D is the best option to address this issue. All grades of milk can be fortified. Oil and milk products such as curd, yogurt, infant formulas, and butter can be fortified with Vitamin D. Widely consumed food items such as atta, maida, and rice flour can also be fortified. Vitamin D fortified food items should be made available to the public at minimal cost and be included in the public distribution system. Effective legislation is required to ensure this. Sustained political and administrative will and support are a must for the development of a fortification program. In India, Vanaspati (dalda) is fortified with 200 IU of Vitamin D per 100 g. Milk products of certain brand are also fortified with Vitamin D
Educational programs are a must to create awareness about Vitamin D deficiency as it is the most underdiagnosed and undertreated nutritional disease. Both physicians and the public should be made aware of its implications. To develop, launch and sustain such a program, adequate investment in the form of time, money, and effort is required
Vitamin D supplements of good quality should be made available at PHC level for the population at risk, i.e., pregnant women, lactating women, children, and elderly
Revision of RDA for Vitamin D by ICMR is needed as it is less compared to other guidelines
School going children can be benefitted from the following: educating them about the need for Vitamin D sufficiency and healthy lifestyle; providing Vitamin D fortified foods at mid-day meals in schools; daily physical exercise which would ensure exposure to sunlight.
Testing facilities for Vitamin D levels should be made affordable and accessible to those at high risk of clinical Vitamin D deficiency (pregnant women, children, elderly especially women), as mass screening is not feasible
Government should support research groups to study and monitor the impact of supplementation programs and fortification strategies.
Conclusion
In India, Vitamin D deficiency is widespread. However, the clinically diagnosed cases represent only the tip of the iceberg. With the knowledge of the multiple consequences, it can lead to; we can imagine the burden, this silent epidemic would cause the development of the country. Vitamin D deficiency needs to be addressed with due attention and strong action.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sharman IM. Vitamin D: Anti-rachitic factor and kidney hormone. Nutr Food Sci. 1975;75:4–7. [Google Scholar]
- 2.Houghton LA, Vieth R. The case against ergocalciferol (Vitamin D2) as a vitamin supplement. Am J Clin Nutr. 2006;84:694–7. doi: 10.1093/ajcn/84.4.694. [DOI] [PubMed] [Google Scholar]
- 3.Holick MF. Vitamin D: A millenium perspective. J Cell Biochem. 2003;88:296–307. doi: 10.1002/jcb.10338. [DOI] [PubMed] [Google Scholar]
- 4.Kumar V, Abbas AK, Aster JC. Robbins Basic Pathology. Environmental and Nutritional Diseases. 9th ed. Philadelphia: Elsevier Saunders; 2013. pp. 438–41. [Google Scholar]
- 5.Holick MF. The Vitamin D epidemic and its health consequences. J Nutr. 2005;135:2739S–48S. doi: 10.1093/jn/135.11.2739S. [DOI] [PubMed] [Google Scholar]
- 6.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 7.Willet W. Nutritional epidemiology. In: Willet W, Lenart E, editors. Biochemical Indicators of Dietary Intake. 3rd ed. New York: Oxford University Press; 2013. pp. 178–82. [Google Scholar]
- 8.Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R, et al. Estimates of optimal Vitamin D status. Osteoporos Int. 2005;16:713–6. doi: 10.1007/s00198-005-1867-7. [DOI] [PubMed] [Google Scholar]
- 9.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of Vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 10.El-Hajj Fuleihan G, Nabulsi M, Tamim H, Maalouf J, Salamoun M, Khalife H, et al. Effect of Vitamin D replacement on musculoskeletal parameters in school children: A randomized controlled trial. J Clin Endocrinol Metab. 2006;91:405–12. doi: 10.1210/jc.2005-1436. [DOI] [PubMed] [Google Scholar]
- 11.van Schoor NM, Lips P. Worldwide Vitamin D status. Best Pract Res Clin Endocrinol Metab. 2011;25:671–80. doi: 10.1016/j.beem.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global Vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807–20. doi: 10.1007/s00198-009-0954-6. [DOI] [PubMed] [Google Scholar]
- 13.Suryanarayana P, Arlappa N, Sai Santhosh V, Balakrishna N, Lakshmi Rajkumar P, Prasad U, et al. Prevalence of Vitamin D deficiency and its associated factors among the urban elderly population in Hyderabad metropolitan city, South India. Ann Hum Biol. 2018;45:133–9. doi: 10.1080/03014460.2018.1425479. [DOI] [PubMed] [Google Scholar]
- 14.Kapil U, Pandey RM, Goswami R, Sharma B, Sharma N, Ramakrishnan L, et al. Prevalence of Vitamin D deficiency and associated risk factors among children residing at high altitude in Shimla district, Himachal Pradesh, India. Indian J Endocrinol Metab. 2017;21:178–83. doi: 10.4103/2230-8210.196031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chowdhury R, Taneja S, Bhandari N, Sinha B, Upadhyay RP, Bhan MK, et al. Vitamin-D deficiency predicts infections in young North Indian children: A secondary data analysis. PLoS One. 2017;12:e0170509. doi: 10.1371/journal.pone.0170509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Srimani S, Saha I, Chaudhuri D. Prevalence and association of metabolic syndrome and Vitamin D deficiency among postmenopausal women in a rural block of West Bengal, India. PLoS One. 2017;12:e0188331. doi: 10.1371/journal.pone.0188331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misra P, Srivastava R, Misra A, Kant S, Kardam P, Vikram NK, et al. Vitamin D status of adult females residing in Ballabgarh health and demographic surveillance system: A community-based study. Indian J Public Health. 2017;61:194–8. doi: 10.4103/ijph.IJPH_176_16. [DOI] [PubMed] [Google Scholar]
- 18.Rattan R, Sahoo D, Mahapatra S. Prevalence of Vitamin D deficiency in adults in the coastal regions of Odisha, India. IOSR J Pharm Biol Sci. 2016;11:49–52. [Google Scholar]
- 19.Gunjaliya A, Patil R, Vaza J, Patel H, Maniyar A. Prevalence of Vitamin D deficiency in higher socioeconomical class of Ahemdabad, Gujarat, India. Int J Med Sci Public Health. 2015;4:617–20. [Google Scholar]
- 20.Bachhel R, Singh NR, Sidhu JS. Prevalence of Vitamin D deficiency in North-West Punjab population: A cross-sectional study. Int J Appl Basic Med Res. 2015;5:7–11. doi: 10.4103/2229-516X.149220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tandon VR, Sharma S, Mahajan S, Raina K, Mahajan A, Khajuria V, et al. Prevalence of Vitamin D deficiency among Indian menopausal women and its correlation with diabetes: A first Indian cross sectional data. J Midlife Health. 2014;5:121–5. doi: 10.4103/0976-7800.141188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agrawal NK, Sharma B. Prevalence of osteoporosis in otherwise healthy Indian males aged 50 years and above. Arch Osteoporos. 2013;8:116. doi: 10.1007/s11657-012-0116-x. [DOI] [PubMed] [Google Scholar]
- 23.Harinarayan CV, Sachan A, Reddy PA, Satish KM, Prasad UV, Srivani P, et al. Vitamin D status and bone mineral density in women of reproductive and postmenopausal age groups: A cross-sectional study from South India. J Assoc Physicians India. 2011;59:698–704. [PubMed] [Google Scholar]
- 24.Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A, et al. Vitamin D status in healthy Indians aged 50 years and above. J Assoc Physicians India. 2011;59:706–9. [PubMed] [Google Scholar]
- 25.Sahu M, Bhatia V, Aggarwal A, Rawat V, Saxena P, Pandey A, et al. Vitamin D deficiency in rural girls and pregnant women despite abundant sunshine in Northern India. Clin Endocrinol (Oxf) 2009;70:680–4. doi: 10.1111/j.1365-2265.2008.03360.x. [DOI] [PubMed] [Google Scholar]
- 26.Paul TV, Thomas N, Seshadri MS, Oommen R, Jose A, Mahendri NV, et al. Prevalence of osteoporosis in ambulatory postmenopausal women from a semiurban region in Southern India: Relationship to calcium nutrition and Vitamin D status. Endocr Pract. 2008;14:665–71. doi: 10.4158/EP.14.6.665. [DOI] [PubMed] [Google Scholar]
- 27.Puri S, Marwaha RK, Agarwal N, Tandon N, Agarwal R, Grewal K, et al. Vitamin D status of apparently healthy schoolgirls from two different socioeconomic strata in Delhi: Relation to nutrition and lifestyle. Br J Nutr. 2008;99:876–82. doi: 10.1017/S0007114507831758. [DOI] [PubMed] [Google Scholar]
- 28.Goswami R, Kochupillai N, Gupta N, Goswami D, Singh N, Dudha A, et al. Presence of 25(OH) D deficiency in a rural North Indian village despite abundant sunshine. J Assoc Physicians India. 2008;56:755–7. [PubMed] [Google Scholar]
- 29.Vupputuri MR, Goswami R, Gupta N, Ray D, Tandon N, Kumar N, et al. Prevalence and functional significance of 25-hydroxyvitamin D deficiency and Vitamin D receptor gene polymorphisms in Asian Indians. Am J Clin Nutr. 2006;83:1411–9. doi: 10.1093/ajcn/83.6.1411. [DOI] [PubMed] [Google Scholar]
- 30.Harinarayan CV. Prevalence of Vitamin D insufficiency in postmenopausal South Indian women. Osteoporos Int. 2005;16:397–402. doi: 10.1007/s00198-004-1703-5. [DOI] [PubMed] [Google Scholar]
- 31.Sofi NY, Jain M, Kapil U, Seenu V, Ramakrishnan L, Yadav CP, et al. Status of serum Vitamin D and calcium levels in women of reproductive age in national capital territory of India. Indian J Endocrinol Metab. 2017;21:731–3. doi: 10.4103/ijem.IJEM_134_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bawaskar PH, Bawaskar HS, Bawaskar PH, Pakhare AP. Profile of Vitamin D in patients attending at general hospital Mahad India. Indian J Endocrinol Metab. 2017;21:125–30. doi: 10.4103/2230-8210.196004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pal CP, Kumar H, Kumar D, Mittal V, Deshwar G, Altaf D, et al. Prevalence of Vitamin D deficiency in orthopaedic patients – A single centre study. J Clin Orthop Trauma. 2016;7:143–6. doi: 10.1016/j.jcot.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ajmani SN, Paul M, Chauhan P, Ajmani AK, Yadav N. Prevalence of Vitamin D deficiency in burka-clad pregnant women in a 450-bedded maternity hospital of Delhi. J Obstet Gynaecol India. 2016;66:67–71. doi: 10.1007/s13224-015-0764-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shukla K, Sharma S, Gupta A, Raizada A, Vinayak K. Current scenario of prevalence of Vitamin D deficiency in ostensibly healthy Indian population: A Hospital based retrospective study. Indian J Clin Biochem. 2016;31:452–7. doi: 10.1007/s12291-016-0552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma S, Kumar A, Prasad S, Sharma S. Current scenario of Vitamin D status during pregnancy in North Indian population. J Obstet Gynaecol India. 2016;66:93–100. doi: 10.1007/s13224-014-0658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar P, Shenoi A, Kumar RK, Girish SV, Subbaiah S. Vitamin D deficiency among women in labor and cord blood of newborns. Indian Pediatr. 2015;52:530–1. [PubMed] [Google Scholar]
- 38.Basu S, Gupta R, Mitra M, Ghosh A. Prevalence of Vitamin D deficiency in a pediatric hospital of Eastern India. Indian J Clin Biochem. 2015;30:167–73. doi: 10.1007/s12291-014-0428-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garg MK, Tandon N, Marwaha RK, Menon AS, Mahalle N. The relationship between serum 25-hydroxy Vitamin D, parathormone and bone mineral density in Indian population. Clin Endocrinol (Oxf) 2014;80:41–6. doi: 10.1111/cen.12248. [DOI] [PubMed] [Google Scholar]
- 40.Angurana SK, Angurana RS, Mahajan G, Kumar N, Mahajan V. Prevalence of Vitamin D deficiency in apparently healthy children in North India. J Pediatr Endocrinol Metab. 2014;27:1151–6. doi: 10.1515/jpem-2013-0387. [DOI] [PubMed] [Google Scholar]
- 41.Baidya A, Chowdhury S, Mukhopadhyay S, Ghosh S. Profile of Vitamin D in a cohort of physicians and diabetologists in Kolkata. Indian J Endocrinol Metab. 2012;16:S416–7. doi: 10.4103/2230-8210.104113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dasgupta A, Saikia U, Sarma D. Status of 25(OH) D levels in pregnancy: A study from the North Eastern part of India. Indian J Endocrinol Metab. 2012;16:S405–7. doi: 10.4103/2230-8210.104109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beloyartseva M, Mithal A, Kaur P, Kalra S, Baruah MP, Mukhopadhyay S, et al. Widespread Vitamin D deficiency among Indian health care professionals. Arch Osteoporos. 2012;7:187–92. doi: 10.1007/s11657-012-0096-x. [DOI] [PubMed] [Google Scholar]
- 44.Marwaha RK, Tandon N, Chopra S, Agarwal N, Garg MK, Sharma B, et al. Vitamin D status in pregnant Indian women across trimesters and different seasons and its correlation with neonatal serum 25-hydroxyvitamin D levels. Br J Nutr. 2011;106:1383–9. doi: 10.1017/S000711451100170X. [DOI] [PubMed] [Google Scholar]
- 45.Multani SK, Sarathi V, Shivane V, Bandgar TR, MenonPS, Shah NS. Study of bone mineral density in resident doctors working at a teaching hospital. J Postgrad Med. 2010;56:65–70. doi: 10.4103/0022-3859.65272. [DOI] [PubMed] [Google Scholar]
- 46.Farrant HJ, Krishnaveni GV, Hill JC, Boucher BJ, Fisher DJ, Noonan K, et al. Vitamin D insufficiency is common in Indian mothers but is not associated with gestational diabetes or variation in newborn size. Eur J Clin Nutr. 2009;63:646–52. doi: 10.1038/ejcn.2008.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kadam NS, Chiplonkar SA, Khadilkar AV, Fischer PR, Hanumante NM, Khadilkar VV, et al. Modifiable factors associated with low bone mineral content in underprivileged premenarchal Indian girls. J Pediatr Endocrinol Metab. 2011;24:975–81. doi: 10.1515/jpem.2011.405. [DOI] [PubMed] [Google Scholar]
- 48.Babu US, Calvo MS. Modern India and the Vitamin D dilemma: Evidence for the need of a national food fortification program. Mol Nutr Food Res. 2010;54:1134–47. doi: 10.1002/mnfr.200900480. [DOI] [PubMed] [Google Scholar]
- 49.Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao PV, Sarma KV, et al. High prevalence of low dietary calcium, high phytate consumption, and Vitamin D deficiency in healthy South Indians. Am J Clin Nutr. 2007;85:1062–7. doi: 10.1093/ajcn/85.4.1062. [DOI] [PubMed] [Google Scholar]
- 50.Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S–6S. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 51.Holick MF. The role of Vitamin D for bone health and fracture prevention. Curr Osteoporos Rep. 2006;4:96–102. doi: 10.1007/s11914-996-0028-z. [DOI] [PubMed] [Google Scholar]
- 52.Hazell TJ, DeGuire JR, Weiler HA. Vitamin D: An overview of its role in skeletal muscle physiology in children and adolescents. Nutr Rev. 2012;70:520–33. doi: 10.1111/j.1753-4887.2012.00510.x. [DOI] [PubMed] [Google Scholar]
- 53.Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral Vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: Randomised double blind controlled trial. BMJ. 2003;326:469. doi: 10.1136/bmj.326.7387.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nebhinani N, Sharma P, Suthar N. Role of Vitamin D supplementation in patients with depressive disorders and hypovitaminosis D: A longitudinal study. J Ment Health Hum Behav. 2017;22:14–20. [Google Scholar]
- 55.Gangwar AK, Rawat A, Tiwari S, Tiwari SC, Narayan J, Tiwari S, et al. Role of Vitamin-D in the prevention and treatment of Alzheimer's disease. Indian J Physiol Pharmacol. 2015;59:94–9. [PubMed] [Google Scholar]
- 56.Singh K, Singh VB, Meena BL, Beniwal S, Gaur S, Ujwal V, et al. Association of mild cognitive impairment with serum Vitamin D level in type 2 diabetes mellitus. Indian J Health Sci Biomed Res. 2015;8:120–4. [Google Scholar]
- 57.Butler MW, Burt A, Edwards TL, Zuchner S, Scott WK, Martin ER, et al. Vitamin D receptor gene as a candidate gene for Parkinson disease. Ann Hum Genet. 2011;75:201–10. doi: 10.1111/j.1469-1809.2010.00631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Umhau JC, George DT, Heaney RP, Lewis MD, Ursano RJ, Heilig M, et al. Low Vitamin D status and suicide: A case-control study of active duty military service members. PLoS One. 2013;8:e51543. doi: 10.1371/journal.pone.0051543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H, et al. Randomized trial of Vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91:1255–60. doi: 10.3945/ajcn.2009.29094. [DOI] [PubMed] [Google Scholar]
- 60.Banda R, Mhemedi B, Allain TJ. Prevalence of Vitamin D deficiency in adult tuberculosis patients at a central hospital in Malawi. Int J Tuberc Lung Dis. 2011;15:408–10. [PubMed] [Google Scholar]
- 61.Arya SC, Agarwal N. Vitamin D deficiency in adult tuberculosis patients. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2011;15:1133–4. doi: 10.5588/ijtld.11.0113. [DOI] [PubMed] [Google Scholar]
- 62.Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: A systematic review and meta-analysis. Arch Dis Child. 2008;93:512–7. doi: 10.1136/adc.2007.128579. [DOI] [PubMed] [Google Scholar]
- 63.Borkar VV, Devidayal, Verma S, Bhalla AK. Low levels of Vitamin D in North Indian children with newly diagnosed type 1 diabetes. Pediatr Diabetes. 2010;11:345–50. doi: 10.1111/j.1399-5448.2009.00589.x. [DOI] [PubMed] [Google Scholar]
- 64.Bener A, Alsaied A, Al-Ali M, Al-Kubaisi A, Basha B, Abraham A, et al. High prevalence of Vitamin D deficiency in type 1 diabetes mellitus and healthy children. Acta Diabetol. 2009;46:183–9. doi: 10.1007/s00592-008-0071-6. [DOI] [PubMed] [Google Scholar]
- 65.Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: Results of a randomized trial. Am J Clin Nutr. 2007;85:1586–91. doi: 10.1093/ajcn/85.6.1586. [DOI] [PubMed] [Google Scholar]
- 66.Anderson LN, Cotterchio M, Vieth R, Knight JA. Vitamin D and calcium intakes and breast cancer risk in pre- and postmenopausal women. Am J Clin Nutr. 2010;91:1699–707. doi: 10.3945/ajcn.2009.28869. [DOI] [PubMed] [Google Scholar]
- 67.Ahn J, Peters U, Albanes D, Purdue MP, Abnet CC, Chatterjee N, et al. Serum Vitamin D concentration and prostate cancer risk: A nested case-control study. J Natl Cancer Inst. 2008;100:796–804. doi: 10.1093/jnci/djn152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–11. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Roy A, Lakshmy R, Tarik M, Tandon N, Reddy KS, Prabhakaran D, et al. Independent association of severe Vitamin D deficiency as a risk of acute myocardial infarction in Indians. Indian Heart J. 2015;67:27–32. doi: 10.1016/j.ihj.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mathieu C, Gysemans C, Giulietti A, Bouillon R. Vitamin D and diabetes. Diabetologia. 2005;48:1247–57. doi: 10.1007/s00125-005-1802-7. [DOI] [PubMed] [Google Scholar]
- 71.Pittas AG, Harris SS, Stark PC, Dawson-Hughes B. The effects of calcium and Vitamin D supplementation on blood glucose and markers of inflammation in nondiabetic adults. Diabetes Care. 2007;30:980–6. doi: 10.2337/dc06-1994. [DOI] [PubMed] [Google Scholar]
- 72.Parameaswari PJ, Revathy C, Shanthi B. A cross-sectional study on Vitamin D3 level in type 2 diabetes mellitus patients from Chennai, India. Int J Basic Med Sci. 2012;3:130–4. [Google Scholar]
- 73.Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, et al. Causal relationship between obesity and Vitamin D status: Bi-directional mendelian randomization analysis of multiple cohorts. PLoS Med. 2013;10:e1001383. doi: 10.1371/journal.pmed.1001383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parikh SJ, Edelman M, Uwaifo GI, Freedman RJ, Semega-Janneh M, Reynolds J, et al. The relationship between obesity and serum 1,25-dihydroxy Vitamin D concentrations in healthy adults. J Clin Endocrinol Metab. 2004;89:1196–9. doi: 10.1210/jc.2003-031398. [DOI] [PubMed] [Google Scholar]
- 75.Kaur S, Sachdev HP, Dwivedi SN, Lakshmy R, Kapil U. Prevalence of overweight and obesity amongst school children in Delhi, India. Asia Pac J Clin Nutr. 2008;17:592–6. [PubMed] [Google Scholar]
- 76.Clements MR, Johnson L, Fraser DR. A new mechanism for induced Vitamin D deficiency in calcium deprivation. Nature. 1987;325:62–5. doi: 10.1038/325062a0. [DOI] [PubMed] [Google Scholar]


