Abstract
Introduction:
Persistent imbalance between work demands and resources seems to be a crucial contributor to the development of burnout among medical professionals. Yet, it seems that Middle East is lacking studies analyzing psychological well-being's of medical residents. Hence, we aimed to conduct a nationwide study to understand and address burnout and depression in medical residents in the UAE.
Methods:
A multicenter, cross-sectional study was designed to evaluate professional burnout and depression among medical residents to address the gap.
Results:
Our results indicate that 75.5% (216/286) of UAE medical residents had moderate-to-high emotional exhaustion (EE), 84% (249/298) had high depersonalization (DP), and 74% (216/291) had a low sense of personal accomplishment. In aggregate, 70% (212/302) of medical residents were considered to be experiencing at least one symptom of burnout based on a high EE score or a high DP score. Depression ranging from 6% to 22%, depending on the specialty was also noted. Noticeably, 83% (40/48) of medical residents who had high scores for depression also reported burnout.
Conclusions:
This study shows that burnout and depression are high among medical residents in UAE. There is a crucial need to address burnout through effective interventions at both the individual and institutional levels. Professional counseling services for residents will certainly be a step forward to manage resident burnout provided the social stigma associated with counseling can be eliminated with awareness. The work hour regulations suggested by the Accreditation Council for Graduate Medical Education partly provides a solution to improve patient safety and care quality. There is an urge to reconfigure the approach to medical training for the well-being of the next generation of physicians in the Arab world.
Keywords: Burnout, depression, mental health, residency training, United Arab Emirates
Introduction
Burnout is defined as “a state of mental and/or physical exhaustion that is related to one's occupation or caregiving.”[1] Persistent imbalance between work demands and resources seems to be a crucial contributor to development of burnout among medical professionals.[2,3,4,5] Extended years of training compared to any other careers, long and irregular work hours,[6] high levels of responsibility and relatively lack of professional experience[7,8] contribute to factors leading to burnout and depression in medical residents.[9,10,11,12,13,14] Burnout rates may vary – from 27% to 75%, depending on the specialty, country, and the method of analysis.[10,11]
Burnout among physicians is reported to be associated with reduced learning capacity,[15] stress-related health problems,[16] emotional exhaustion (EE), and low sense of professional efficacy.[17] Adverse personal consequences including substance abuse, depression, family conflicts, and suicidal ideation[3,18,19] has also followed professional burnout.[20,21,22]
Apart from the negative effects on an individual's health,[18,23,24,25,26] burnout may negatively impact the health-care system as a whole by lowering the quality of patient care,[23,24] decreasing physician productivity,[23] and burdening health-care system with enormous costs due to early retirement and reduction in clinical hours.[23] Burnout not only affects the health of physicians but also being associated with implications for patients by decreasing the patient satisfaction,[25] promoting unprofessional conduct,[17] and ultimately reducing patient care quality.[26,27]
The United Arab Emirates is a relatively young country established almost 45 years ago in the Arabian Peninsula and is a member country of the Gulf Cooperation Council. The discovery of oil and natural gas catapulted the economic growth, which led to the higher per capita and the quality infrastructure in health, education, and transportation. The government initiatives in the past 5 years has helped to transform medical education in the country.[28,29] The country has two main medical residency training programs, one in Abu Dhabi and the other in Dubai; both being accredited by Arab Board of Health Specializations.[30,31,32] Several factors related to career choices among medical students,[28,29,33] accreditation perception among residents and resident’ satisfaction of the residency program in Dubai and Abu Dhabi were recently addressed.[30,34] In spite, a concerted nationwide study to understand and address burnout and depression in the medical residency program has not been conducted not only in the UAE but also the region in general. To address this gap, a nationwide, multicenter, cross-sectional study was designed to evaluate professional burnout and depression among medical residents in the UAE.
Methods
A correlational, cross-sectional study using the Maslach Burnout Inventory (MBI)[17,35] and the Patient Health Questionnaire-9 (PHQ-9)[36] survey instruments were conducted at several health-care centers in the emirates of Dubai and Abu Dhabi between May and December 2016. The medical residency program in UAE is active in health authorities of Abu Dhabi and Dubai, plus Ministry of Health (MOH). Yet, the program in MOH recently established, hence it is not included in this study. Doctors complete an intern year before applying for residency in UAE. Surveys used in this study consisted of three major components: Sociodemographic characteristics, the MBI, and the PHQ-9. Considering that our residents are obliged to get minimum score of 550 in TOEFL or 6 in IELTS as an entry requirement for UAE residency programs, all surveys used in this study were in English,
Participants and procedure
Medical residents were approached in academic days, morning reports, and outpatient's clinics. The purpose of the study was explained to the residents and asked to voluntarily participate in the study. Participants were from different specialties such as internal medicine, pediatrics, obstetrics and gynecology, neurology, ophthalmology, emergency medicine, psychiatry, surgery, radiology, neurosurgery, otolaryngology, orthopedics, family medicine, and trauma. Aggregate reporting of data assured to enhance confidentiality and accurate reporting by the respondents.
Surveys
Sociodemographic characteristics questionnaire
Demographic data, including gender, age, nationality, marital status, place of birth and upbringing, location of medical school, and postgraduate year were recorded. Previous work has shown a link between burnout and factors such as the presence or absence of support networks, longer working hours, opportunities for relaxation, and a perceived lack of control of one's time.[37,38] Therefore, based on previously published work, a mini questionnaire was developed utilizing a 4-point Likert scale (agree, disagree, strongly agree, and strongly disagree).
Maslach Burnout Inventory
The MBI – Human Services Version is considered a reliable and valid tool used to evaluate burnout state related to occupational stress. The MBI consists of 22 items with three subscales; EE (9 items), depersonalization (DP, 5 items), and personal accomplishment (PA, 8 items).[17] Responses are provided using a 7-point Likert-type scale with response options ranging from 1 (never) to 7 (daily).
EE reflects “feelings of being emotionally overextended,” DP relates to an “impersonal response toward recipients of one's service,” and PA stands for “feelings of competence and successful achievement in one's work with people,” which turns into the opposite in a burnout situation.[17,37] Higher levels of burnout state are associated with higher EE and DP scores and lower PA scores.[39] A score of ≥27 on the EE subscale score and/or ≥10 on the DP was considered as moderate to high-level burnout.[17]
Patient Health Questionnaire-9
The PHQ-9 is widely used as a screening tool for depression.[36] Participants read nine statements and indicate how often they experienced these symptoms over the past 2 weeks (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day). Scores were summed with a maximum possible score of 27 and scores ≥15 was considered as moderately severe to severe depression.
Data analysis and statistics
Descriptive statistics were computed for the sociodemographic variables, MBI scores, and PHQ 9 scores. A score for burnout and depression was calculated for each individual participant. Correlation analysis was done to examine the relationships between the psychometric study variables. The prevalence rates of burnout and depression were also assessed and expressed as percentage of the total. The prevalence rates were compared for significant differences using Pearson's Chi-square analysis. Independent t-tests and analysis of variance were performed to analyze the differences of means between the demographic variables, in the context of burnout and depression. Tukey's post hoc tests were used to further examine group differences. All analyses were performed using SPSS version 20 (IBM Corp., Released 2011, Armonk, NY, US). For all tests, alpha (α) was set at 0.05.
Results
Demographic characteristics of medical residents
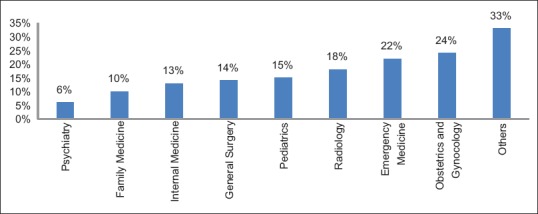
Dubai and Abu Dhabi health authorities each have 270 and 400 medical residents, respectively. We were not able to reach all the residents, as around 150 of them are out of the country for fellowship, and some were in maternity or sick leaves or suspended their residency for personal reasons. Hence, we were able to access 446 medical residents and invited them to participate, out of which 302 responded (68% response rate). The majority of respondents were females (236, 79%), non-UAE nationals (161, 53%), >25 years of age (275, 91%) and born in the UAE (186, 62%). The demographics also highlighted the fact that a sizable number of participants were from Dubai (210, 70%), single (171, 57%), without children (212, 70%), and lived with family (182, 60%) [Table 1]. Excepting for the year-five of training, the respondents were near equally distributed, although dominated by the internal medicine specialty (200, 66%). In spite of the fact that the professional job satisfaction rate was high at 62.5% (187/299), yet more than half (56%, 165/300) of the participants thought of quitting the residency program (sometimes/frequently). Results show that majority of survey participants received emotional support from their families (83%, 251/301) and were nonsmokers (62%, 187/299). The majority of the respondents (67%, 202/301) stated that they work more than 40 h/week, and 76% (216/285) mentioned that they have <5 days between their on calls.
Table 1.
Baseline characteristics of respondents (n=302)
Prevalence and predictive factors of burnout and depression
Characteristics of responding residents with respect to burnout and depression in the past 12 months, and satisfaction with work–life balance were analyzed using the MBI. Interestingly, 75.5% (216/286) of the medical residents surveyed had moderate-to-high EE, 84% (249/298) had high DP, and 74% (216/291) had a low sense of PA. In aggregate, 70% (212/302) of medical residents were considered to be experiencing at least one symptom of burnout based on a high EE score or a high DP score. On the other hand, among the 302 residents who responded to the depression assessment using PHQ-9, 16% (48/302) had moderately severe to severe depression. Alarmingly, a high percentage (83% 40/48) of the medical residents who scored high on depression also had reported burnout.
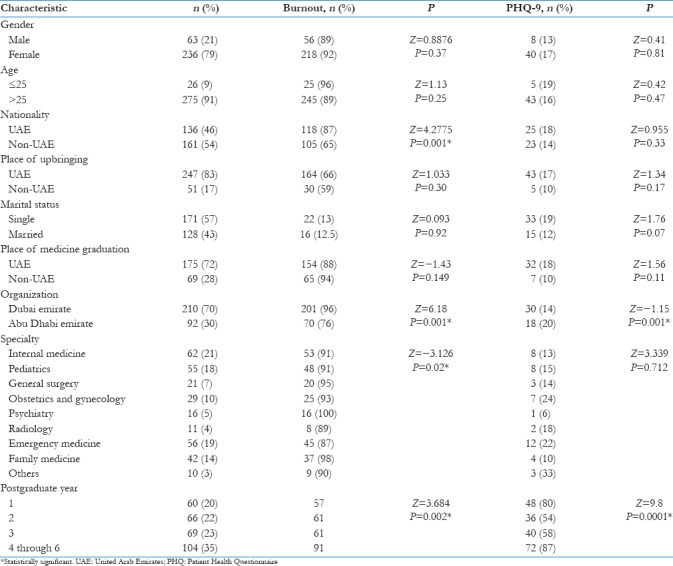
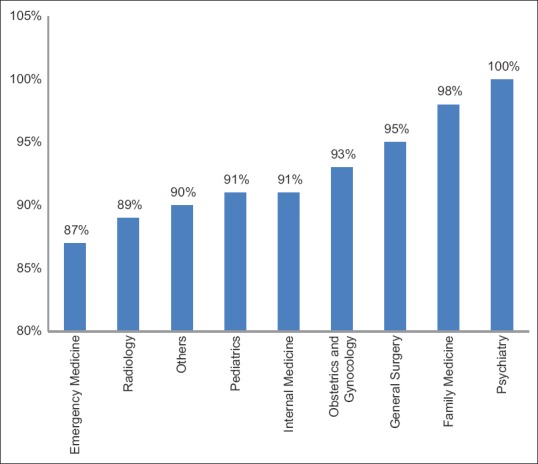
Both, the subspecialties (P = 0.02); [Figure 1] and the year of postgraduate study (P = 0.002); [Table 1] affected burnout among medical residents significantly. Burnouts among medical residents were alarmingly high close to a 100%, especially for psychiatry, family medicine, and general surgery [Figure 1]. Comparatively, emergency medicine (87%) and radiology residents (89%) had lower burnout. Early years of residency presented lesser burnout rates as compared to the latter years (years 4–6). More than one-third (35%, P < 0.002) of the residents experienced burnout in their advanced years of residency [Table 1]. Notably, burnout was significantly different between UAE national residents when compared with nonnationals (P < 0.001). Abu Dhabi residents indicated lower burnout (P = 0.001), [Table 1]. Depression varied between 6% and 33% among the subgroups of medical specialties. In contrast to psychiatry and family medicine that experienced high burnout, depression was at the lowest among these specialties [Figure 2 and Table 1]. More than 20% of the medical residents in the otolaryngology, ophthalmology, orthopedics (33% combined), obstetrics and gynecology (24%) and emergency medicine (22%), program experienced depression. Significant differences in depression was not observed among the subspecialties (P = 0.7). Marital status did not influence burnout (P = 0.92) but affected depression among the medical residents (P = 0.07), [Table 1].
Figure 1.
Varying levels of burnout among medical residents from different specialties in UAE. Others = otolaryngology, orthopedics, and ophthalmology
Figure 2.
Varying levels of depression among medical residents from different specialties in UAE. Others = otolaryngology, orthopedics, and ophthalmology
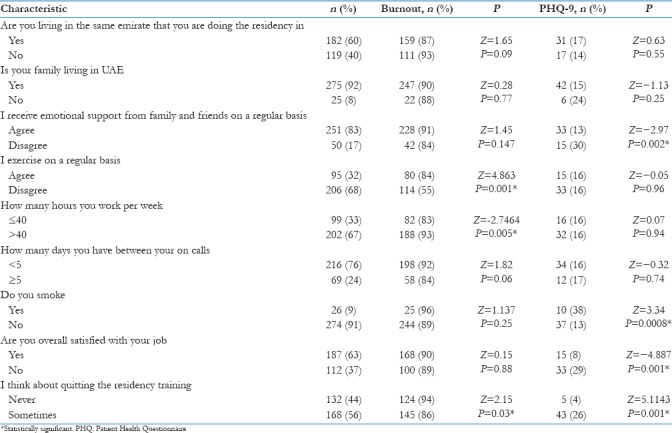
Evidently, three factors: Work hours >40/week (P = 0.005), scheduling on calls in <5 days (P = 0.06), regular exercise (P = 0.001), and thoughts of quitting the residency program (P = 0.03) were significantly related to burnout among residents. Living closer to work (same living in an emirate where being trained, P = 0.09) was associated with burnout [Table 2]. Invariably, residents who; did not smoke (P = 0.0008), found job satisfaction (P = 0.001), never had thoughts of quitting the residency program (P = 0.001), and received emotional support from their family and friends (P = 0.002) were significantly less likely to be depressed as compared to their counterparts [Table 2].
Table 2.
Characteristics associated with burnout and depression in medical residents in United Arab Emirates
Discussion
Work-life imbalance for health-care professionals leading to burnout and depression has gathered significant attention globally because of the negative impact it renders on patient care and safety. Physicians who had high burnout and depression reportedly committed more medical errors.[3] Despite extensive global data, to the best of our knowledge, there have been scanty reports addressing burnout among physicians in the Middle East. Middle East countries have their own characteristics being fast developing during past 20 years, multicultural, and having relatively cultural difference than western countries. These are burnout among otorhinolaryngology residents and pediatricians in Saudi Arabia and general practitioners in Qatar.[40,41] Systematic nation-wide studies have been lacking in the region to address the issue primarily because of traditional health-care practice prevalent until a few years ago.[42] The transformation of health care in the UAE started from the affiliation with Western managed health-care providers, introduction of medical insurance, and development of the medical residency programs.[43] Burnout characterized by high EE, high DP, and a low sense of PA were prevalent in more than 70% of the residents in our study, almost two-fold higher than observed for the otolaryngology residents in Saudi Arabia. Shanafelt et al.[5] have reported similar percentages (76%) of burnout among internal medicine residents in the USA residency program. The worrying matter here is that burned-out residents were reported to be two to three times more likely to report suboptimal patient care practices.[5] This will definitely affect patient care in the long run.
Depression ranging from 6% to 22%, depending on the specialty for medical residents was also noticeable given the fact the Arab culture lays high emphasis on family bonding and support.[44] The extended Arab family structure provides stability, coherence, physical, and psychological support.[44,45] Compared to the UAE national residents, the nonnational (expatriates) are not immune to the societal, environmental, and financial burdens, yet the latter seems to manage burnout and depression better 45 [Table 1]. It was not surprising to observe that environmental, behavioral, and psychological triggers, irrespective of the specialty contributed to burnout and depression among the medical residents. Nonsmoker residents with a positive attitude (not thinking of quitting the program), who enjoyed their residency (job satisfaction), worked only 40-h/week and were on call after 5 days coped with burnout and depression better than their respective counterparts [Tables 1 and 2]. As expected, specialties and higher years of resident training affected burnout and depression [Table 1]. The higher burnout observed among psychiatry residents in our study [Figure 1] may have been contributed by stressors including fear and exposure to patient violence and suicide.[46]
The results of our study indicate that burnout and depression among medical residents might be high. There is a crucial need to address burnout through effective interventions at both the individual and institutional levels. Professional counseling services for residents will certainly be a step forward to manage resident burnout provided the social stigma associated with counseling can be eliminated with awareness. The work hour regulations suggested by the Accreditation Council for Graduate Medical Education partly provides a solution to improve patient safety and care quality.[47] Work hour and on-call limitation may decrease burnout and improve resident quality of life; however, its implementation should ensure a balance of expected service responsibilities, with the academic and educational training mission and values.
Even though our results are in accordance with studies published elsewhere, a direct comparison with those or within the individual specialties in our study may be inappropriate and construed as a limitation of this study. Differences in the settings such as the residency programs, sample selection, study size, participation rates, in addition to local culture and tradition may confound interpretation. We have used screening tools in this study; further clinical psychiatric diagnostic interview using a structured psychiatric diagnostic instrument is needed to further confirm the findings of this study. The cross-sectional nature of this study limit conclusions that can be drawn for causality. especially when it can be assumed that cynicism and decreased humanism can also lead to EE and DP. Our study is distinguished not only as the first in the region that addresses burnout and depression among medical residents but also multicentric, nationwide in study design with a high participation rate.
Conclusions
As the country moves toward national health-care reforms, it is imperative to reconfigure the approach to medical training. In addition to professionalism and ethical values, personal well-being is critical to the successful education of the next generation of physicians. The results of our study are anticipated not only to benefit the UAE but also to find application in the Arab world, with similar residency programs, values, culture, and tradition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank all residents who responded to the survey.
References
- 1.Ishak W, Nikravesh R, Lederer S, Perry R, Ogunyemi D, Bernstein C, et al. Burnout in medical students: A systematic review. Clin Teach. 2013;10:242–5. doi: 10.1111/tct.12014. [DOI] [PubMed] [Google Scholar]
- 2.Pantenburg B, Luppa M, König HH, Riedel-Heller SG. Burnout among young physicians and its association with physicians’ wishes to leave: Results of a survey in Saxony, Germany. J Occup Med Toxicol. 2016;11:2. doi: 10.1186/s12995-016-0091-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 4.Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50:132–49. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 6.Martini S, Arfken CL, Balon R. Comparison of burnout among medical residents before and after the implementation of work hours limits. Acad Psychiatry. 2006;30:352–5. doi: 10.1176/appi.ap.30.4.352. [DOI] [PubMed] [Google Scholar]
- 7.Gray-Stanley JA, Muramatsu N. Work stress, burnout, and social and personal resources among direct care workers. Res Dev Disabil. 2011;32:1065–74. doi: 10.1016/j.ridd.2011.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ, et al. Psychosocial interventions for managing occupational stress and burnout among medical doctors: A systematic review. Syst Rev. 2017;6:144. doi: 10.1186/s13643-017-0526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prins JT, Hoekstra-Weebers JE, Gazendam-Donofrio SM, Van De Wiel HB, Sprangers F, Jaspers FC, et al. The role of social support in burnout among Dutch medical residents. Psychol Health Med. 2007;12:1–6. doi: 10.1080/13548500600782214. [DOI] [PubMed] [Google Scholar]
- 10.Prins JT, Hoekstra-Weebers JE, van de Wiel HB, Gazendam-Donofrio SM, Sprangers F, Jaspers FC, et al. Burnout among Dutch medical residents. Int J Behav Med. 2007;14:119–25. doi: 10.1007/BF03000182. [DOI] [PubMed] [Google Scholar]
- 11.Braun SE, Auerbach SM, Rybarczyk B, Lee B, Call S. Mindfulness, burnout, and effects on performance evaluations in internal medicine residents. Adv Med Educ Pract. 2017;8:591–7. doi: 10.2147/AMEP.S140554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soler JK, Yaman H, Esteva M, Dobbs F, Asenova RS, Katic M, et al. Burnout in European family doctors: The EGPRN study. Fam Pract. 2008;25:245–65. doi: 10.1093/fampra/cmn038. [DOI] [PubMed] [Google Scholar]
- 13.Cheng DR, Poon F, Nguyen TT, Woodman RJ, Parker JD. Stigma and perception of psychological distress and depression in Australian-trained medical students: Results from an inter-state medical school survey. Psychiatry Res. 2013;209:684–90. doi: 10.1016/j.psychres.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: A systematic review. Med Educ. 2014;48:963–79. doi: 10.1111/medu.12512. [DOI] [PubMed] [Google Scholar]
- 15.Kahn JS, Witteles RM, Mahaffey KW, Desai SA, Ozdalga E, Heidenreich PA, et al. A 15-year review of the Stanford internal medicine residency program: Predictors of resident satisfaction and dissatisfaction. Adv Med Educ Pract. 2017;8:559–66. doi: 10.2147/AMEP.S138467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 17.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. Mountain View, CA: CPP Inc. and Davies-Black; 1996. [Google Scholar]
- 18.Shanafelt T, Sloan J, Satele D, Balch C. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212:421–2. doi: 10.1016/j.jamcollsurg.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Scheepers RA, Boerebach BC, Arah OA, Heineman MJ, Lombarts KM. A systematic review of the impact of physicians’ occupational well-being on the quality of patient care. Int J Behav Med. 2015;22:683–98. doi: 10.1007/s12529-015-9473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y, Feng X. The relationship between job satisfaction, burnout, and turnover intention among physicians from urban state-owned medical institutions in Hubei, China: A cross-sectional study. BMC Health Serv Res. 2011;11:235. doi: 10.1186/1472-6963-11-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreno-Jiménez B, Gálvez-Herrer M, Rodríguez-Carvajal R, Sanz Vergel AI. A study of physicians’ intention to quit: The role of burnout, commitment and difficult doctor-patient interactions. Psicothema. 2012;24:263–70. [PubMed] [Google Scholar]
- 22.Estryn-Behar M, Fry C, Guetarni K, Aune I, Machet G, Doppia MA, et al. Work week duration, work-family balance and difficulties encountered by female and male physicians: Results from the French SESMAT study. Work. 2011;40(Suppl 1):S83–100. doi: 10.3233/WOR-2011-1270. [DOI] [PubMed] [Google Scholar]
- 23.Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shirom A, Nirel N, Vinokur AD. Overload, autonomy, and burnout as predictors of physicians’ quality of care. J Occup Health Psychol. 2006;11:328–42. doi: 10.1037/1076-8998.11.4.328. [DOI] [PubMed] [Google Scholar]
- 25.Dyrbye LN, Massie FS, Jr, Eacker A, Harper W, Power D, Durning SJ, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–80. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 26.Demerouti E, Bakker AB, Leiter M. Burnout and job performance: The moderating role of selection, optimization, and compensation strategies. J Occup Health Psychol. 2014;19:96–107. doi: 10.1037/a0035062. [DOI] [PubMed] [Google Scholar]
- 27.Block L, Wu AW, Feldman L, Yeh HC, Desai SV. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J. 2013;89:495–500. doi: 10.1136/postgradmedj-2012-131743. [DOI] [PubMed] [Google Scholar]
- 28.Abdulrahman M, Makki M, Shaaban S, Al Shamsi M, Venkatramana M, Sulaiman N, et al. Specialty preferences and motivating factors: A national survey on medical students from five UAE medical schools. Educ Health (Abingdon) 2016;29:231–43. doi: 10.4103/1357-6283.204225. [DOI] [PubMed] [Google Scholar]
- 29.Ibrahim H, Nair SC, Shaban S, El-Zubeir M. Reducing the physician workforce crisis: Career choice and graduate medical education reform in an emerging Arab country. Educ Health (Abingdon) 2016;29:82–8. doi: 10.4103/1357-6283.188716. [DOI] [PubMed] [Google Scholar]
- 30.Abdulrahman M, Qayed KI, AlHammadi HH, Julfar A, Griffiths JL, Carrick FR, et al. Challenges facing medical residents’ satisfaction in the middle east: A Report from United Arab Emirates. Teach Learn Med. 2015;27:387–94. doi: 10.1080/10401334.2015.1077125. [DOI] [PubMed] [Google Scholar]
- 31.Ibrahim H, Nair SC. Focus on international research strategy and teaching: TheFIRST programme. Perspect Med Educ. 2014;3:129–35. doi: 10.1007/s40037-013-0098-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmed A, Qayed KI, Abdulrahman M, Tavares W, Rosenfeld J. The multiple mini-interview for selecting medical residents:First experience in the Middle East region. Med Teach. 2014;36:703–9. doi: 10.3109/0142159X.2014.907875. [DOI] [PubMed] [Google Scholar]
- 33.Ibrahim H, Awadhi AA, Shaban S, Nair SC. Can our residents carry the weight of the obesity crisis? A mixed methods study. Obes Res Clin Pract. 2015;9:228–33. doi: 10.1016/j.orcp.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 34.Archuleta S, Ibrahim H, Stadler DJ, Shah NG, Chew NW, Cofrancesco J, Jr, et al. Perceptions of leaders and clinician educators on the impact of international accreditation. Acad Med. 2015;90:S83–90. doi: 10.1097/ACM.0000000000000906. [DOI] [PubMed] [Google Scholar]
- 35.Maslach C. Job burnout: New directions in research and intervention. Curr Dir Psychol Sci. 2003;12:189–92. [Google Scholar]
- 36.Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010;304:1181–90. doi: 10.1001/jama.2010.1300. [DOI] [PubMed] [Google Scholar]
- 37.Ripp J, Babyatsky M, Fallar R, Bazari H, Bellini L, Kapadia C, et al. The incidence and predictors of job burnout in first-year internal medicine residents: A five-institution study. Acad Med. 2011;86:1304–10. doi: 10.1097/ACM.0b013e31822c1236. [DOI] [PubMed] [Google Scholar]
- 38.Mazurkiewicz R, Korenstein D, Fallar R, Ripp J. The prevalence and correlations of medical student burnout in the pre-clinical years: A cross-sectional study. Psychol Health Med. 2012;17:188–95. doi: 10.1080/13548506.2011.597770. [DOI] [PubMed] [Google Scholar]
- 39.Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85:S33–6. doi: 10.1097/ACM.0b013e3181ed4c47. [DOI] [PubMed] [Google Scholar]
- 40.Abdulla L, Al-Qahtani D, Al-Kuwari M. Prevalence and determinants of burnout syndrome among primary healthcare physicians in Qatar. S Afr Fam Pract. 2011;53:380–3. [Google Scholar]
- 41.Aldrees T, Badri M, Islam T, Alqahtani K. Burnout among otolaryngology residents in Saudi Arabia: A Multicenter study. J Surg Educ. 2015;72:844–8. doi: 10.1016/j.jsurg.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 42.Nair SC, Ibrahim H, Celentano DD. Clinical trials in the Middle East and North Africa (MENA) region: Grandstanding or grandeur? Contemp Clin Trials. 2013;36:704–10. doi: 10.1016/j.cct.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 43.Ibrahim H, Lindeman B, Matarelli SA, Nair SC. International residency program evaluation: Assessing the reliability and initial validity of the ACGME-I resident survey in Abu Dhabi, United Arab Emirates. J Grad Med Educ. 2014;6:517–20. doi: 10.4300/JGME-D-13-00381.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dhami S, Sheikh A. The Muslim family: Predicament and promise. West J Med. 2000;173:352–6. doi: 10.1136/ewjm.173.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A Systematic review and meta-analysis. JAMA. 2016;316:2214–36. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Woodside JR, Miller MN, Floyd MR, McGowen KR, Pfortmiller DT. Observations on burnout in family medicine and psychiatry residents. Acad Psychiatry. 2008;32:13–9. doi: 10.1176/appi.ap.32.1.13. [DOI] [PubMed] [Google Scholar]
- 47.Goodman DM, Winkler MK, Fiser RT, Abd-Allah S, Mathur M, Rivero N, et al. The accreditation council for graduate medical education proposed work hour regulations. Pediatr Crit Care Med. 2011;12:120–1. doi: 10.1097/PCC.0b013e3181fe3d4b. [DOI] [PubMed] [Google Scholar]


