Abstract
Fetal intra-abdominal umbilical vein varix (FIUVV) is a rare pathology and suggests an enlargement of the umbilical vein. Prenatal diagnosis is done through meticulous ultrasound imaging. Management variables are the diameter of varix, presence or absence of turbulent flow, and fetal anomalies. Color and power Doppler ultrasound helps in diagnosis and follow-up and has a critical role in decision-making for intervention. Clinical guidelines for management are not clear. The adverse fetal outcome is usually associated with multiple malformations, turbulent flow, and thrombotic varix. This case study presents the prenatal diagnosis, obstetric management, and neonatal development of a fetus, diagnosed with FIUVV along with a brief review of the literature.
Keywords: Epispadias, fetal umbilical vein, prenatal diagnosis, turbulent flow, umbilical vein varix
Introduction
Fetal intra-abdominal umbilical vein varix (FIUVV) is uncommon (0.4–1.1/1000 fetuses),[1] characterized by focal dilation of the umbilical vein from its entry in the abdominal wall to the portal system. The diameter of umbilical vein increases linearly with gestational age,[2] and the diagnosis is made when the diameter of umbilical vein exceeds two standard deviations for the gestation age. Other diagnostic criteria are the diameter of umbilical vein diameter >9 mm at term gestation, >1.5 times its intrahepatic portion, or >50% of its nondilated portion.[3,4] The natural history, etiology, and obstetric management guidelines are not clear. Diameters of varix, a presence of turbulent flow and thrombosis, associated fetal anomalies, and growth parameters influence the outcome of the fetus. We present a case of FIUVV diagnosed at 22-week obstetric management. We found epispadias as an associated novel finding.
Case Report
A 29-year, gravida 3, para 1, abortion 1, known hypothyroid lady on replacement therapy diagnosed with fetal umbilical vein dilation of 8 mm at 22 weeks of gestation. She had nonconsanguineous marriage and had a healthy first child of 3 years. Her first trimester (at 13 weeks) aneuploidy assessment screen was found to be low risk. Her medical and antenatal history was uneventful, and blood investigations were normal. Anatomical survey of the fetus revealed no morphological anomaly at 19 weeks, but umbilical vein dilatation was noted. Scan at 22 weeks showed 8 mm dilated umbilical vein. She was followed up once in three weeks thereafter, and at 30 weeks dilation of umbilical vein measured was 15.5 mm. The ultrasound at 33 weeks suggested increased amniotic fluid index (24.5 cm) and fetal growth between 25th and 50th percentiles without additional structural anomaly. Umbilical vein varix increased to 17 mm at 33 weeks. Color and power Doppler showed continuous venous flow without turbulence or apparent thrombosis. She was counseled about the fetal venous flow abnormality and subsequent chances of fetal mortality and morbidity and advised for weekly follow-up. At 35 weeks, the size of varix measured 19 mm [Figures 1 and 2a] with venous turbulence. Her umbilical vein and middle cerebral artery Doppler were normal. Fetal echocardiography was normal. She was euglycemic throughout the pregnancy. At 36 weeks, an emergency cesarean section was performed for turbulent flow in varix, and a male baby of 2.56 kg was delivered with Apgar score of 8 at 1 min and 9 at 5 min. Neonatal physical examination revealed distal epispadias, for which follow-up was suggested. An abdominal ultrasound indicated thrombosis in varix and confirmed the diagnosis of FIUVV on day 2. Neonatal echocardiograph was normal. Karyotype was not performed. At present, the infant is 6 months and has appropriate growth and milestones for his age.
Figure 1.
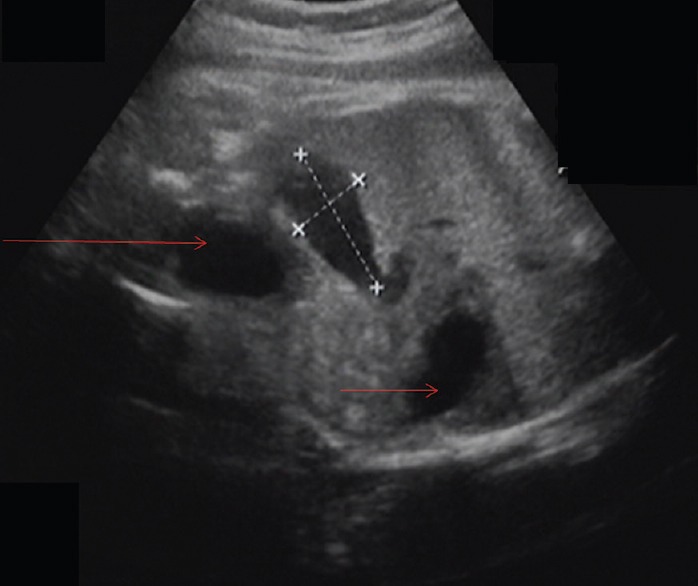
Grayscale ultrasound showing intra-abdominal, intrahepatic umbilical vein varix of 19 mm adjacent to bladder (large arrow) at 35 weeks’ gestation, small arrow – stomach
Figure 2.
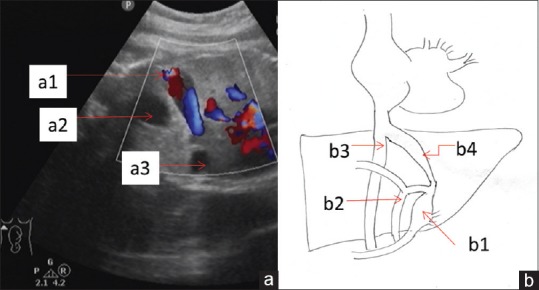
(a) Fetal abdominal ultrasound – color Doppler of umbilical vein varix (a1), bladder bubble (a2), and stomach bubble (a3). (b) Schematic course of umbilical vein. (b1) umbilical recess, (b2) portal vein, (b3) inferior vena cava, and (b4) ductus venosus
Discussion
The left umbilical vein enters the fetus at an umbilical ring and runs along the inferior border of the liver. It joins the portal system making the umbilical–portal system and enters the inferior vena cava through ductus venosus [Figure 2b]. Inherent weakness or an unsupported intra-abdominal portion of an umbilical vein makes it vulnerable to pressure changes, resulting in segmental dilatation of the vein.[5]
FIUVV is characterized as an anechoic fluid-filled mass oriented obliquely in a cephalocaudal direction between the abdominal wall and inferior border of the liver on ultrasound. It is measured from the outer edge to the opposite inner edge. Color and pulse Doppler detects venous flow within FIUVV and helps in distinguishing it from other sonolucent structures such as gallbladder, choledochal cyst, and urachal cyst. One must rule out associated fetal structural anomalies.[6]
FIUVV is associated with fetal aneuploidy (trisomy 9, 18, and 21) (up to 6.3%) and multiple malformations (up to 35.3%).[4] Cardiovascular and urogenital malformations are commonly associated abnormalities. A diaphragmatic hernia, pulmonary sequestration, ventriculomegaly, and echogenic bowel are also associated. Single umbilical artery or a pyelectasis is usually not taken into account to classify the associated malformations.[6] Documented complications are hydrops fetalis, low birth weight, and intrauterine fetal death.[1,5,7] We report here isolated umbilical vein varix with distal epispadias, which is a novel finding associated with FIUVV.
Its clinical impact depends on gestational age at detection, associated malformations, and flow characteristics in varix. The early appearance of varix (before 26 weeks) needs close monitoring for growth and flow abnormalities and is associated with significant risk of adverse outcome. In our case, FIUVV was suspected at 19 weeks and confirmed at 22 weeks. Fetal surveillance was regularly carried out by serial ultrasound and color Doppler. The large diameter of varix is a potential risk for thrombosis.[6] An increase in the size of FIUVV (11 mm) was noted during pregnancy. Turbulent flow is a bidirectional flow on color Doppler and reported up to 50% in the dilated segment of umbilical vein.[1,2,8] The adverse fetal outcome is possible in spite of close observation in FIUVV.[4,7,9,10] Cesarean delivery was performed when bidirectional flow was observed at 35 weeks. Similar management has been suggested in the literature.[7,8] The frequency of intrauterine growth restriction and intrauterine death is 3% and 0.7%, respectively. Chromosomal abnormalities and congenital malformation are observed at a frequency of 0.5 and 2%. The frequencies of fetal mortality, associated anomalies, and chromosomal abnormalities in the studies of FIUVV were observed to be higher [Table 1].
Table 1.
Comparison of different studies with fetal intra-abdominal umbilical vein varix
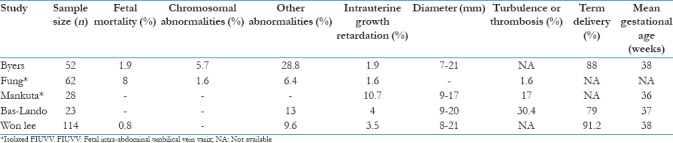
Associated malformations warrant further evaluation by neonatal karyotyping. The frequency of associated malformation is 9.6% without chromosomal anomaly.[5] One fetal demise and 91.2% term deliveries were observed. Similar findings have been observed for term deliveries without fetal or neonatal death. Close monitoring by fetal weekly with Doppler examination should be carried out to term. We recommend timely intervention in isolated FIUVV to prevent an adverse fetal outcome in cases of large size or turbulent flow in varix.
Conclusion
Although isolated FIUVV is associated with favorable outcome in many cases, close monitoring by ultrasound is essential to identify ominous signs. We recommend fetal surveillance and early delivery after fetal lung maturity in cases with the distinct increase in size and with turbulent flow. Neonatal ultrasound is advised to ascertain the diagnosis and to rule out an abnormal vascular connection.
Declaration of patient consent
The authors certify that they have obtained all appropriate consents from the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bas-Lando M, Rabinowitz R, Samueloff A, Latinsky B, Schimmel MS, Chen O, et al. The prenatal diagnosis of isolated fetal varix of the intra-abdominal umbilical vein is associated with favorable neonatal outcome at term: A case series. Arch Gynecol Obstet. 2013;288:33–9. doi: 10.1007/s00404-013-2743-x. [DOI] [PubMed] [Google Scholar]
- 2.Weissman A, Jakobi P, Bronshtein M, Goldstein I. Sonographic measurements of the umbilical cord and vessels during normal pregnancies. J Ultrasound Med. 1994;13:11–4. doi: 10.7863/jum.1994.13.1.11. [DOI] [PubMed] [Google Scholar]
- 3.Pamplona-Bueno L, Padilla-Iserte P, Ferri-Folch B, Juárez-Pallarés I, Gómez-Portero R, Perales-Marín A, et al. Fetal intra-abdominal umbilical vein varix: A Case report and literature review. J Obstet Gynaecol India. 2015;65:420–2. doi: 10.1007/s13224-015-0694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahony BS, McGahan JP, Nyberg DA, Reisner DP. Varix of the fetal intra-abdominal umbilical vein: Comparison with normal. J Ultrasound Med. 1992;11:73–6. doi: 10.7863/jum.1992.11.2.73. [DOI] [PubMed] [Google Scholar]
- 5.Lee SW, Kim MY, Kim JE, Chung JH, Lee HJ, Yoon JY, et al. Clinical characteristics and outcomes of antenatal fetal intra-abdominal umbilical vein varix detection. Obstet Gynecol Sci. 2014;57:181–6. doi: 10.5468/ogs.2014.57.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beraud E, Rozel C, Milon J, Darnault P. Umbilical vein varix: Importance of ante- and post-natal monitoring by ultrasound. Diagn Interv Imaging. 2015;96:21–6. doi: 10.1016/j.diii.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Valsky DV, Rosenak D, Hochner-Celnikier D, Porat S, Yagel S. Adverse outcome of isolated fetal intra-abdominal umbilical vein varix despite close monitoring. Prenat Diagn. 2004;24:451–4. doi: 10.1002/pd.897. [DOI] [PubMed] [Google Scholar]
- 8.Mankuta D, Nadjari M, Pomp G. Isolated fetal intra-abdominal umbilical vein varix: Clinical importance and recommendations. J Ultrasound Med. 2011;30:273–6. doi: 10.7863/jum.2011.30.2.273. [DOI] [PubMed] [Google Scholar]
- 9.Brookfield KF, Osmundson SS, Chetty S, Chueh J, Blumenfeld YJ, Barth RA, et al. Isolated umbilical vein varix with a poor outcome despite close fetal surveillance. J Ultrasound Med. 2013;32:1680–2. doi: 10.7863/ultra.32.9.1680. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization multicenter study on menstrual and ovulatory patterns in adolescent girls. II. Longitudinal study of menstrual patterns in the early postmenarcheal period, duration of bleeding episodes and menstrual cycles. World Health Organization task force on adolescent reproductive health. J Adolesc Health Care. 1986;7:236–44. [PubMed] [Google Scholar]


