Abstract
Previous findings suggest immigrant patients have lower trust in their physicians, and perceive nonverbal communication differently compared to non-immigrant patients. We tested discrepancies in trust and the impact of non-verbal behavior between immigrants and non-immigrants in The Netherlands. Nonverbal communication of an oncologist was systematically varied in an experimental video vignettes design. Breast cancer patients (n = 34) and healthy women (n = 34) viewed one of eight video versions and evaluated trust and perceived friendliness of the oncologist. In a matched control design, women with immigrant and non-immigrant backgrounds were paired. Immigrant women reported stronger trust. Nonverbal communication by the oncologist did not influence trust differently for immigrants compared to for non-immigrants. However, smiling strongly enhanced perceived friendliness for non-immigrants, but not for immigrants. Immigrant patients’ strong trust levels may be formed a priori, instead of based on physicians’ communication. Physicians may need to make extra efforts to optimize their communication.
Electronic supplementary material
The online version of this article (doi:10.1007/s10903-017-0580-x) contains supplementary material, which is available to authorized users.
Keywords: Trust, Nonverbal communication, Immigrants, Cross-cultural comparison, Oncology
Introduction
Patients need to trust their physicians when confronted with illness and associated treatments. If trust levels are high, patients are likely to experience more satisfaction about their care, suffer less anxiety, and be more adherent to recommendations [1–8]. With a cancer diagnosis, trust is even more essential, because of the heavy physical and psychological burden associated with the disease.
Disparities in Trust
Traditionally, patients’ trust in physicians has been strong. However, several subgroups have been identified with lower trust levels [9]. Patients with ethnic minority backgrounds may be particularly vulnerable to diminished trust in their physician [10]. In the United States (US), lower trust levels were found among African American and/or Latino patients compared to Caucasians [11–17]. For African American patients in particular, this has been explained from a historical perspective: a legacy of being discriminated against in medical research still substantially affects African American patients’ trust in medical research and clinicians [18]. However, there exists only limited research that substantiates lower trust for other minority patient groups in and outside the US. Moreover, preliminary findings in some patient groups, e.g., Chinese migrants in the US and South Asian migrants in the United Kingdom, do not corroborate ethnic disparities in trust [19, 20]. Thus, it is uncertain whether trust levels are lower among ethnic minority patients in general or only in specific subgroups.
The largest ethnic minorities in The Netherlands are of Turkish, Moroccan and Surinamese descent. Their education level and SES are below average, overall [21, 22]. Therefore, and because of cultural differences and language problems, these patients are vulnerable within the health care context [23]. On one hand, results from US minority groups suggest lower trust among these patients. On the other hand, patients with lower education levels and lower SES may feel more dependent and thus experience a greater need and willingness to trust their physicians [12, 24, 25]. We do not know how trust levels among these immigrant patients compare to those of non-immigrants.
Physicians’ Communication and Patients’ Trust Levels
In addition to socio-demographic factors, differences in trust between population groups may arise from variation between patients in how they perceive their physician’s communication. Physicians’ communication is known to be influential for patients’ levels of trust [26]. However, while its nonverbal aspects, i.e., how messages are conveyed, are known to be at least equally relevant for trust, most research so far focuses on the impact of verbal communication, i.e., what the physician says [27].
Findings from qualitative research suggest that nonverbal communication might even be more meaningful for immigrant patients [28]. First, many immigrant patients have, on average, lower language proficiency, and may be forced to rely more strongly on the nonverbal aspects of the physician’s message [28]. Second, intercultural differences strongly influence the manifestation, meaning and interpretation of nonverbal communication. For example, Turkey, Surinam and Arabic countries are traditionally more ‘high context’ cultures than the Dutch culture, meaning more attention and weight are placed on the nonverbal aspects of a message [29]. This manifests in more direct and longer eye contact [30, 31], as well as less physical distance and more direct body orientations in high context cultures [31, 32]. Moreover, patients from high context cultures have been found to attach high value to the physician’s smiling behavior [28].
Study Aim
The three nonverbal behaviors mentioned above, i.e., amount of eye contact, body posture and smiling, may thus be more relevant to Dutch immigrant patients’ trust than for that of non-immigrants. As part of a larger experimental study on the influence of nonverbal communication on breast cancer patients’ trust in the oncologist, we investigated differences between Dutch patients with non-immigrant (i.e., Dutch) and immigrant (i.e., non-Western, mostly Turkish, Moroccan, Surinam) backgrounds. We compared between these two groups (1) their levels of trust in the oncologist, and (2) how strongly an oncologists’ nonverbal communication influenced their trust.
Methods
Design
This study was part of a larger experimental project [33]. In that study, the effects of nonverbal communication behaviors on breast cancer patients’ trust in an oncologist were tested using eight variants of a video vignette depicting a medical consultation. The validity of this methodology has been well documented [34]. For the present analysis, we selected all women in the sample with non-Western ethnic minority backgrounds. We employed a case-control design using individual matching to optimize power [35, 36]. The case-control design allows for statistical analyses using a repeated measures design, comparing data from cases with controls as if they were measured repeatedly in the same person. Each woman with an immigrant background was matched to a woman with non-immigrant background from the larger sample [37], based on three criteria: (1) being a breast cancer patient or a healthy woman, (2) the observed variant of the video vignette, and (3) age. If no perfect match was available on all criteria, we matched on the first two criteria, and selected the closest available match in age.
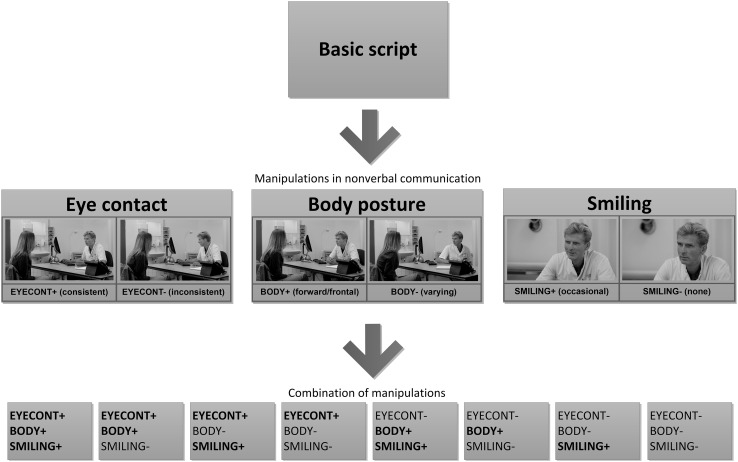
Development of Video Vignettes
Development and validation of video vignettes is described in detail in Online Appendix A. First, a basic vignette was developed, depicting an initial consultation between a medical oncologist and a breast cancer patient addressing neo-adjuvant treatment for breast cancer. Next, eight variants of the video were created, identical except for variations in the oncologist’s amount of eye contact (consistent vs. inconsistent), body posture (forward leaning and frontal vs. varying between forward and backward leaning), and smiling (occasional smiling vs. no smiling) (see Fig. 1).
Fig. 1.
Development of the eight different video variants
Participants
Both breast cancer patients and women without breast cancer participated as analogue patients (AP), i.e., viewing the video while imagining themselves to be the patient [34, 38]. We recruited patients as well as healthy women to test whether both groups were equally suitable to act as AP. As earlier analyses showed no significant differences, we performed the current analyses for the two groups combined [33]. Participants were recruited through (migrant) breast cancer patient organizations, hospital outpatient clinics, snowballing methods and general practitioners. Further details on recruitment are specified elsewhere [33]. For the larger study, power analysis suggested a minimum sample size of 160 was required. In total, 214 participants were recruited, of whom 147 were breast cancer patients. For the present analyses, we selected all women with immigrant backgrounds from the larger sample (n = 34) and matched them to an equal number of non-immigrants (n = 34).
Procedure
AP were identified by the physician (for GP and outpatient clinics) or by a patient organization contact person (for snowballing method, migrant and non-migrant breast cancer patient organization) and asked for permission to be contacted by the researcher. Next, the researcher informed them by telephone, and they received a link to the online experiment. Women without an internet connection or non-proficient in the Dutch language (n = 5) were visited at home by the researcher. First, patients filled in a questionnaire assessing their background characteristics (T0). Next, they viewed one randomly assigned variant of the video vignettes. After viewing the video, they completed a second questionnaire evaluating the observed oncologist (T1).
Measures
As background characteristics, age, education level, ethnicity and religion were assessed. As a background measure, trust in health care was assessed using a single item (‘How much trust do you have in the current Dutch health-care system?’, no trust at all = 1 to complete trust = 5) [39].
As a manipulation check, AP rated their perception of the oncologist’s amount of eye contact, physical distance (to assess body posture), and smiling behavior (3 single items, 5-point Likert scale). Moreover, three items measured how realistic, credible and likely to happen in real life AP perceived the events in the video (7-point Likert scale). Engagement with the video was assessed using the Video Engagement Scale (VES; 15 items, 7-point Likert scale; reliability α=0.93) [40]. For a subsample of migrant women who had difficulty completing the questionnaires because of limited Dutch language proficiency (n = 13), engagement was measured using a single global item (‘I was well able to engage in the video’; completely disagree = 1 to completely agree = 7) to reduce questionnaire burden.
The primary outcome, trust in the observed oncologist, was assessed using the 18-item Trust in Oncologist Scale [41, 42]. Reliability of the scale was α=0.96. Secondary outcomes were AP’s (1) Reported likelihood of recommending the oncologist to others and (2) Perceived affectivity of the oncologist, i.e., perceived competence, friendliness, hurry and honesty (5-point Likert scale).
Analyses
Analyses were conducted using SPSS 20.0 [43]. Differences between cases (migrant women) and controls (majority women) on background and outcome variables were tested using paired-samples t-tests. Interactions between cultural background and nonverbal communication behaviors on trust were tested using repeated measures ANOVA. In these analyses, immigrants and non-immigrants were considered as a repeated factor instead of the factor time. Results were considered significant if p < .05. Sensitivity analysis indicated that with our sample size (n = 68), when conducting a repeated measures ANOVA with two groups, we would have a power of 0.80 to detect effects with a minimum effect size of F = 0.17. The hospital’s Medical Ethics Committee granted approval for this study to be conducted.
Results
Participants
The sample consisted of 34 immigrants and 34 non-immigrants (N = 68; see Table 1). Mean age was 52 (SD = 9.88; range 27–85). Immigrants were predominantly from Morocco (n = 11), Surinam (n = 10), and Turkey (n = 4). The remaining 9 immigrants were from Bulgaria, Curaçao, Malaysia, Nigeria, Saudi Arabia, Slovakia, Sudan, Sweden and Tunesia (n = 1 each). Non-immigrants were on average higher educated (t(66)= −2.12, p < .05). Immigrants were more likely to be religious than non-immigrants (t(65) = 4.96, p < .001).
Table 1.
Sample characteristics (N = 68)
| Immigrant (n = 34) | Non-immigrant (n = 34) | |||
|---|---|---|---|---|
| Median (range) | SD | Median (range) | SD | |
| Age (n = 68) | 52 (27–85) | 11 | 52 (31–80) | 9 |
| N | % | N | % | |
| Educational level (n = 68)* | ||||
| None/primary school | 9 | 27 | 1 | 3 |
| Secondary/lower level vocat. school | 12 | 35 | 17 | 50 |
| College/university | 13 | 38 | 16 | 47 |
| Current living situation (n = 68) | ||||
| Alone | 6 | 18 | 3 | 9 |
| With partner | 7 | 21 | 14 | 41 |
| With partner and children | 15 | 44 | 16 | 47 |
| Other | 6 | 17 | 1 | 3 |
| Religion (n= 68)*** | ||||
| None | 20 | 59 | 3 | 9 |
| Islamic | 0 | 0 | 18 | 53 |
| Christian | 13 | 38 | 9 | 27 |
| Hindu | 0 | 0 | 2 | 6 |
| Other | 1 | 3 | 2 | 6 |
| Mean (range) | SD | Mean (range) | SD | |
| Trust in health care (n = 63) | 3.61 (1–5) | 0.70 | 3.24 (1–5) | 0.80 |
| Trust in own treating oncologist (n = 31) | 4.28 (3.28–4.94) | 0.50 | 4.21 (2.67–5.00) | 0.60 |
*Indicates difference between the two groups at α = 0.05
***Indicates difference between the two groups at α = 0.001
Manipulation check
Matching between immigrants and non-immigrants was perfect for the first two criteria, i.e., breast cancer patient or a healthy woman and which of the video variants was viewed. For age, the maximum difference between immigrants and non-immigrants was 13 years, and for most (25/34 pairs) < 4 years. On average, participants rated the observed video as realistic (M = 5.33, SD = 1.65), credible (M = 5.33, SD = 1.59) and likely to happen in real life (M = 5.86, SD = 1.31). T-tests revealed no differences in these scores between women with immigrant and non-immigrant backgrounds. The oncologist in the ‘consistent eye contact’ conditions was perceived as having more eye contact than the one in the ‘inconsistent eye contact’ conditions (M = 3.87 vs. 3.38, t(61)= −1.81, p = .08). The oncologist in the ‘forward leaning posture’ conditions was perceived as having slightly less physical distance than the one in the ‘varying body posture’ conditions, although not significantly so (M = 3.46 vs. 3.11, t(61) = 1.27, p = .21). The oncologist in the ‘smiling’ conditions was perceived as smiling significantly more than in the ‘no smiling’ conditions (M = 3.38 vs. 2.06, t(61)= −5.73, p < .001). Mean score for engagement with the video (n = 61) was 4.79 (SD = 1.29, range 1.27–7.00).
Descriptive characteristics
Mean trust in health care and patients’ mean level of trust in their own treating oncologist are displayed in Table 1. Mean trust in the observed oncologist was 3.41 (SD = 0.78, range 1.72–5.00). Willingness to recommend the observed oncologist to others was 3.10 (SD = 1.00, range 1–5). Mean score for participants’ affective perception of the observed oncologist were: for perceived competence 3.87 (SD = 0.79, range 2–5), for friendliness 3.44 (SD = 1.01, range 1–5), for hurriedness 3.11 (SD = 1.33, range 1–5) and for honesty 3.90 (SD = 0.76, range 2–5).
Trust and Affective Perceptions Among Women with Immigrant vs. Non-Immigrant Backgrounds
Immigrants reported stronger trust in the observed oncologist (M = 3.56, SD = 0.72) than non-immigrants (M = 3.24, SD = 0.80; t(33) = 2.51, p = .02). Willingness to recommend the observed oncologist to others did not differ between the two groups (t(28) = 1.36, p = .18). Participants’ affective perception of the oncologist did not differ significantly for competence (t(28) = 0.66, p = .52), friendliness (t(28) = 0.34, p = .74), or hurriedness (t(28)= −1.23, p = .23). However, immigrants perceived the oncologist as more honest (M = 4.07, SD = 0.70) than non-immigrants (M = 3.76, SD = 0.83; t(28) = 2.07, p < .05).
The Influence of the Physician’s Nonverbal Communication
Main effects of nonverbal communication by the observed oncologist on participants’ trust are reported in Table 2. A forward leaning body posture led to significantly stronger trust than a varying body posture (p < .05), and to an increased likelihood of recommending the oncologist to others (p < .05). Consistent eye contact resulted in slightly increased trust (p = .08) and a slightly higher likelihood of recommending the oncologist to others (p = .06) compared to inconsistent eye contact.
Table 2.
Main effects of nonverbal communication by the oncologist on trust and likelihood of recommending the oncologist (N = 68)
| Trust | Likelihood of recommending | |||
|---|---|---|---|---|
| M (SD) | T (df, p) | M (SD) | T (df, p) | |
| Eye contact | ||||
| Consistent | 3.53 (0.75) | 3.28 (0.97) | ||
| Inconsistent | 3.19 (0.76) | −1.76 (66, 0.08) | 2.79 (0.98) | −1.94 (61, 0.06) |
| Body posture | ||||
| Forward leaning | 3.59 (0.77) | 3.31 (0.96) | ||
| Varying | 3.16 (0.72) | −2.39 (66, 0.02) | 2.82 (0.98) | −2.00 (61, 0.05) |
| Smiling | ||||
| Yes | 3.52 (0.75) | 3.24 (1.02) | ||
| No | 3.29 (0.79) | −1.22 (61, 0.23) | 2.97 (0.97) | −1.08 (61, 0.29) |
The Impact of Nonverbal Communication for Women with Immigrant vs. Non-Immigrant Backgrounds
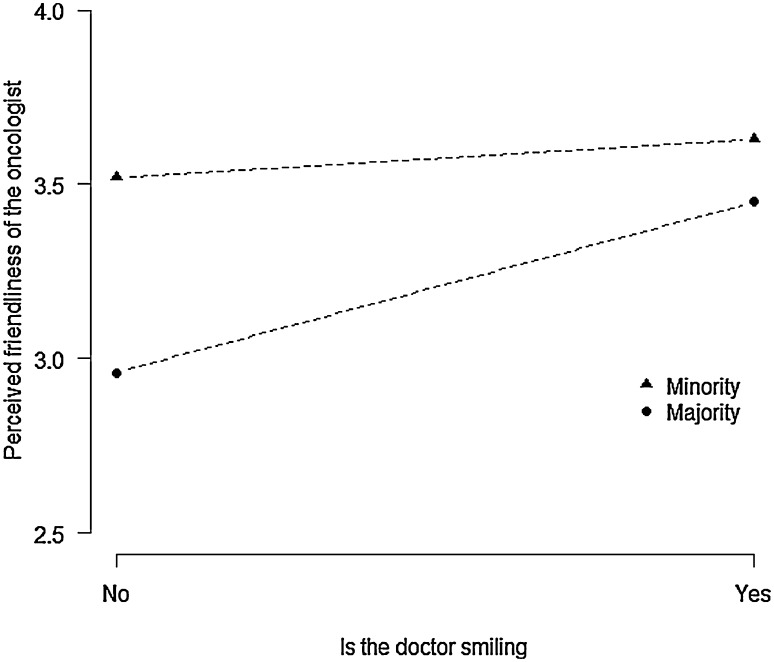
The effects of the oncologist's nonverbal communication on trust did not differ between immigrants and non-immigrants for eye contact (F(1,21) = 0.00, p = .99), body posture (F(1,21) = 0.54, p = .47), or smiling (F(1,21) = 1.17, p = .29) (see Table 3). Similarly, there was no effect on the secondary outcomes likelihood of recommending the oncologist to others, competence, hurry and honesty (not displayed). However, smiling did not influence the perceived friendliness of the oncologist for immigrants, but strongly enhanced perceived friendliness among non-immigrants (F(1,21) = 20.62, p < .001) (see Table 4 and Fig. 2).
Table 3.
Differential effects of the physician’s nonverbal communication on trust for women with immigrant vs. non-immigrant backgrounds
| Non-immigrant (n = 34) | Immigrant (n = 34) | |||
|---|---|---|---|---|
| M (SE) | 95% CI | M (SE) | 95% CI | |
| Eye contact | ||||
| Consistent eye contact | 3.30 (0.22) | (2.84–3.76) | 3.67 (0.20) | (3.26–4.07) |
| Inconsistent eye contact | 3.11 (0.26) | (2.57–3.66) | 3.49 (0.23) | (3.01–3.97) |
| Body posture | ||||
| Forward leaning | 3.43 (0.25) | (2.92–3.94) | 3.67 (0.22) | (3.22–4.12) |
| Varying | 2.98 (0.24) | (2.48–3.48) | 3.49 (0.23) | (3.01–3.97) |
| Smiling | ||||
| Occasional smiling | 3.45 (0.24) | (2.95–3.96) | 3.63 (0.21) | (3.19–4.07) |
| No smiling | 2.96 (0.25) | (2.45–3.47) | 3.52 (0.22) | (3.07–3.97) |
Table 4.
Differential effects of the physician’s nonverbal communication on perceived friendliness of the oncologist for migrant vs. majority women
| Majority (n = 34) | Migrant (n = 34) | |||
|---|---|---|---|---|
| M (SE) | 95% CI | M (SE) | 95% CI | |
| Eye contact | ||||
| Consistent eye contact | 3.53 (0.28) | (2.96–4.11) | 3.16 (0.26) | (2.62–3.69) |
| Inconsistent eye contact | 3.46 (0.33) | (2.78–4.14) | 3.48 (0.30) | (2.85–4.11) |
| Body posture | ||||
| Forward leaning | 3.66 (0.31) | (3.02–4.29) | 3.59 (0.28) | (3.01–4.18) |
| Varying | 3.33 (0.30) | (2.71–3.96) | 3.04 (0.28) | (2.46–3.62) |
| Smiling | ||||
| Occasional smiling | 3.40 (0.30) | (2.77–4.02) | 3.98 (0.28) | (3.40–4.56) |
| No smiling | 3.59 (0.31) | (2.96–4.23) | 2.66 (0.28) | (2.07–3.24) |
Fig. 2.
Interaction between oncologist smiling behavior and participant ethnic background on perceived friendliness of the oncologist
Discussion
We found stronger trust in an oncologist among immigrant women compared to non-immigrants. Little evidence was found that the oncologist’s nonverbal communication influences trust differentially between the two groups. However, smiling by the oncologist strongly enhanced perceived friendliness for non-immigrants, but not for immigrants.
The observed higher trust levels among immigrants deviate from results among US minority patient samples, which have consistently demonstrated lower trust among ethnic minorities. This discrepancy may be ascribed to the respective sample compositions: trust of US Latino/African American patients cannot be directly compared to that of immigrants in the Netherlands. Especially for US African American patients, historical discrepancies in medical care may determine how trust is constructed [18]. Such historical factors may be less relevant for immigrant groups in the Netherlands. On the contrary, these patients may feel a strong need to trust their physician. This ‘need to trust’ has been previously encountered among many patients, particularly of lower socio-economic status [44]. Immigrant patients could experience an even stronger need to trust due to cultural and language barriers. Although such a need to trust can be functional, it may also discourage physicians and patients from stimulating patients’ active involvement in their treatment [45]. Ultimately, this may limit immigrant patients’ autonomy and result in a more authoritarian treatment relationship with their physician.
An alternative explanation for the finding that immigrant women report stronger trust, is social desirability. These women may have felt less at liberty to express their honest opinion about oncologists’ behavior than women with majority backgrounds. Many non-Western cultures place a higher value on dependency than do Western societies, which more strongly emphasize individuality and autonomy [46]. As a consequence, these immigrants may have viewed the physician as more authoritative and not expected to play an assertive role in the medical consultation [45]. Moreover, immigrants’ relative indirectness and reduced assertiveness may have extended to questionnaire responses: it could have caused them to report strong trust, while keeping their more critical thoughts to themselves [47]. Although the anonymity of patients’ responses was emphasized, the Trust in Oncologist Scale may have failed to tap into immigrants’ actual inner evaluation of the observed oncologist.
Finally, sampling issues could account for the reported differences in trust levels. Recruitment of women with immigrant backgrounds proved extremely difficult. This is a common problem in research among Dutch ethnic minority groups [48], as well as in other countries [49, 50]. Patients’ hesitance to participate in research may stem from a lack of familiarity with, or trust in research. We were able to reach women who would have been difficult to recruit otherwise, e.g., with limited mastery of the Dutch language, by establishing alternative recruitment routes, for example, through a GP who kept in frequent contact with his patients. As a result, however, our sample may have included a disproportional number of highly trusting women, with a positive outlook on research and the medical community. Future studies could aim to recruit larger and more representative samples, to examine the robustness of the present findings. Recruitment can be maximized with sufficient budget, time and persistence [48]. Specifically, attempts should be made to find the right entry points and establishing trust in the community of interest [49].
In previous qualitative work, women with Turkish and Arabic backgrounds placed a strong emphasis on the oncologist’s facial expression, particularly on smiling, for the establishment of their trust [28]. Thus, we hypothesized immigrant women to attach importance to nonverbal signals, because of their cultural background and/or insufficient comprehension of verbal aspects of the message due to language difficulties [28, 29]. The opposite was found for perceived friendliness in the present study: smiling by the oncologist strongly increased perceived friendliness of the oncologists for non-immigrants, but not for immigrants. Possibly, the type of smiles expressed by the oncologist did not align with immigrant women’s preferences. The oncologist’s smiles were sympathetic, mostly. Different types of signals may be conveyed through smiling, e.g., support, optimism, sadness or encouragement. Possibly, immigrant women in general attach more value to the types of smiles that radiate optimism and support, thus instilling a sense of hope [28, 51, 52]. Moreover, a ‘sympathetic smile’ may for these women have reduced their perception of oncologist’s authority and, consequently, have come at the expense of their trust.
Alternatively, immigrants in our study may have been less critical of the oncologist’s communicative behavior than non-immigrants. This would correspond with the higher overall trust levels found among immigrants in our sample. These women may have felt a need to trust, leading to its establishment a priori, instead of based on the oncologist’s communicative behavior. In other words: vulnerability may create a level of trust so high that there is little room for improvement or that improvement is not visible because of ceiling effects [44, 53]. Possibly, among immigrants with lower trust levels, more marked effects of smiling on trust or perceived friendliness would be visible. Non-immigrants may hold the oncologist more accountable for his actions, hence the increase of perceived friendliness as a result of occasional smiling. An alternative explanation for immigrants’ less critical stance, may be that they were less able to place themselves in the patient’s shoes. The patient in the video had a non-immigrant background, hence immigrants possibly had more difficulty identifying with her.
An important limitation of this study is its sample size. Although the matched control design added to the study’s power, the relatively small sample limited the power to detect smaller effects. Thus, the results should not be interpreted as definitive evidence. Moreover, due to this limited sample size, variations in cultural and religious backgrounds of the participants may have influenced the results. For example, participants were not matched based on religion or religiosity, whereas this attribute may predict how people view their doctors, and how well they are willing and able to create trusting relations [54]. More studies in larger samples are needed to rule out this bias and examine whether these findings are consistent across different cultural backgrounds and religions. Additionally, more heterogeneous samples could be recruited to test how effects extrapolate, for example, to male migrants or female physicians. Another limitation is that participants’ previous experiences with healthcare and physicians in particular were not assessed in the current study. Such experiences may influence patients’ expectations of physicians’ communication and hence explain differences in trust and perceptions of nonverbal behavior. Future research should include this factor to enable better interpretation of results. A final limitation is our video vignettes design. The validity of this design has been repeatedly supported [34]. Nevertheless, it also entails inherent limitations. For example, this design does not enable participants to actually interact with the physician in the video. Results from this experimental study should therefore be corroborated by observational research in clinical practice.
New Contribution to the Literature
In conclusion, this study is one of the first to experimentally examine how trust in a physician is established differentially for women with immigrant vs. non-immigrant backgrounds. Our results suggest that recommendations for physicians’ optimal nonverbal communication, e.g., maintaining frequent eye contact, and a patient-oriented, forward leaning body posture, can be maintained across patient groups. The higher reported trust among immigrant women contradict alarming evidence of weak levels of trust in this population. These findings, however, also call for caution among health care professionals: if such high trust levels stem from patients’ vulnerability, these patients may not hold their physicians fully accountable for their communicative behaviors. Physicians may need to make extra efforts to optimize their nonverbal and verbal communication behavior. Ultimately, this could help immigrant patients establishment a form of trust that is more deliberate, thus creating more open and genuine interaction.
Electronic supplementary material
Below is the link to the electronic supplementary material. This appendix was published as supplementary material previously in Breast Cancer Research and Treatment (doi:10.1007/s10549-015-3486-0)
Acknowledgements
This study was made possible by financial support from the Dutch Pink Ribbon foundation (http://www.pinkribbon.nl), Grant Number 2011.WO29.C114. We thank all participating patients and healthy women for their contribution to this study. Moreover, we are grateful to dr. Douwe de Vries, ms. Lide van der Vegt, dr. Geertjan van Tienhoven and dr. Nina Bijker for their invaluable help in patient recruitment.
Funding
This study was funded by the Dutch Pink Ribbon foundation (http://www.pinkribbon.nl), Grant Number 2011.WO29.C114.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s10903-017-0580-x) contains supplementary material, which is available to authorized users.
Contributor Information
Marij A. Hillen, Phone: +31.20.566.4631, Email: M.A.Hillen@amc.uva.nl
Hanneke C. J. M. de Haes, Email: J.C.deHaes@amc.uva.nl
Mathilde G. E. Verdam, Email: M.G.E.Verdam@amc.uva.nl
Ellen M. A. Smets, Email: E.M.Smets@amc.uva.nl
References
- 1.Bernstein M, Potvin D, Martin DK. A qualitative study of attitudes toward error in patients facing brain tumour surgery. Can J Neurol Sci. 2004;31:208–212. doi: 10.1017/S0317167100053841. [DOI] [PubMed] [Google Scholar]
- 2.Knifed E, July J, Bernstein M. Neurosurgery patients’ feelings about the role of residents in their care: a qualitative case study. J Neurosurg. 2008;108:287–291. doi: 10.3171/JNS/2008/108/2/0287. [DOI] [PubMed] [Google Scholar]
- 3.Charles C, Gafny A, Whelan T. Self-reported use of shared decision making among breast cancer specialists and perceived barriers and facilitators to implementing this approach. Health Expect. 2004;7:338–348. doi: 10.1111/j.1369-7625.2004.00299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geller G, Strauss M, Bernhardt BA, Holtzman NA. “Decoding” informed consent. Insights from women regarding breast cancer susceptibility testing. Hastings Cent Rep. 1997;27:28–33. doi: 10.2307/3527625. [DOI] [PubMed] [Google Scholar]
- 5.Shepherd HL, Tattersall MH, Butow PN. Physician-identified factors affecting patient participation in reaching treatment decisions. J Clin Oncol. 2008;26:1724–1731. doi: 10.1200/JCO.2007.13.5566. [DOI] [PubMed] [Google Scholar]
- 6.Freedman TG. Prescriptions for health providers: from cancer patients. Cancer Nurs. 2003;26:323–330. doi: 10.1097/00002820-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Reid CM, Gooberman-Hill R, Hanks GW. Opioid analgesics for cancer pain: symptom control for the living or comfort for the dying? A qualitative study to investigate the factors influencing the decision to accept morphine for pain caused by cancer. Ann Oncol. 2008;19:44–48. doi: 10.1093/annonc/mdm462. [DOI] [PubMed] [Google Scholar]
- 8.Sharf BF, Stelljes LA, Gordon HS. ‘A little bitty spot and I’am a big man’: patients’ perspectives on refusing diagnosis or treatment for lung cancer. Psychooncology. 2005;14:636–646. doi: 10.1002/pon.885. [DOI] [PubMed] [Google Scholar]
- 9.Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician-a review. Psychooncology. 2011;20:227–241. doi: 10.1002/pon.1745. [DOI] [PubMed] [Google Scholar]
- 10.Suurmond J, Uiters E, de Bruijne MC, et al. Negative health care experiences of immigrant patients: a qualitative study. BMC Health Serv Res. 2011;11:10. doi: 10.1186/1472-6963-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berrios-Rivera JP, Street RL, Popa-Lisseanu MGG, et al. Trust in physicians and elements of the medical interaction in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum. 2006;55:385–393. doi: 10.1002/art.21988. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter WR, Godley PA, Clark JA, et al. Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer. 2009;115:5048–5059. doi: 10.1002/cncr.24539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Do YK, Carpenter WR, Spain P, et al. Race, healthcare access and physician trust among prostate cancer patients. Cancer Cause Control. 2010;21:31–40. doi: 10.1007/s10552-009-9431-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–1163. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 15.Gordon HS, Street RL, Jr, Sharf BF, et al. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 16.Keating NL, Gandhi TK, Orav EJ, et al. Patient characteristics and experiences associated with trust in specialist physicians. Arch Intern Med. 2004;164:1015–1020. doi: 10.1001/archinte.164.9.1015. [DOI] [PubMed] [Google Scholar]
- 17.Saha S, Jacobs EA, Moore RD, Beach MC. Trust in physicians and racial disparities in HIV care. Aids Patient Care Stds. 2010;24:415–420. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep. 2003;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lord K, Ibrahim K, Rudd N, et al. Measuring trust in healthcare professionals - a study of ethnically diverse UK cancer patients. Clin Oncol 2011. [DOI] [PubMed]
- 20.Simon MA, Zhang M, Dong X. Trust in physicians among U.S. chinese older adults. J Gerontol A Biol Sci Med Sci. 2015;69:s46–s53. doi: 10.1093/gerona/glu174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.CBS. Allochtonen in Nederland 2012 [Immigrants in The Netherlands 2012]. In. Den Haag: Centraal Bureau voor de Statistiek 2012.
- 22.CBS. Inkomensongelijkheid; particuliere huishoudens naar diverse kenmerken [Income inequality; private households for diverse characteristics]. In. 2014.
- 23.Stronks K, Ravelli AC, Reijneveld S. Immigrants in the Netherlands: equal access for equal needs? J Epidemiol Commun Health. 2001;55:701–707. doi: 10.1136/jech.55.10.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meyer SB, Ward PR, Jiwa M. Does prognosis and socioeconomic status impact on trust in physicians? Interviews with patients with coronary disease in South Australia. BMJ open. 2012;2:e001389. doi: 10.1136/bmjopen-2012-001389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riva S, Monti M, Iannello P, et al. Preliminary mixed-method investigation of trust and hidden signals in medical consultations. Plos ONE. 2014;9:e90941. doi: 10.1371/journal.pone.0090941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hillen MA, De Haes HCJM, Stalpers LJA, et al. How can communication by oncologists enhance patients’ trust? An experimental study. Ann Oncol. 2014;25:896–901. doi: 10.1093/annonc/mdu027. [DOI] [PubMed] [Google Scholar]
- 27.Burgoon JK, Bacue AE. Nonverbal communication skills. In: Green JO, Burleson BR, editors. Handbook of communication and social interaction skills. Mahwah: Erlbaum; 2003. pp. 179–219. [Google Scholar]
- 28.Hillen MA, El Temna S, van der Vloodt J, et al. Vertrouwen van Turkse en Arabische allochtonen in hun oncoloog [Trust of Turkish and Arabic ethnic minority patients in their Dutch oncologist] Nederlands Tijdschrift voor Geneeskundeyr [Dutch J Med] 2013;157:828–833. [PubMed] [Google Scholar]
- 29.Knapp ML, Hall JA. Nonverbal communication in human interaction. Boston: Wadsworth Publishing; 2009. [Google Scholar]
- 30.Hall ET. A system for the notation of proxemic behaviors. Am Anthropolt. 1963;65:1003–1026. doi: 10.1525/aa.1963.65.5.02a00020. [DOI] [Google Scholar]
- 31.Watson OM, Graves TD. Quantitative research in proxemic behavior1. Am Anthropol. 1966;68:971–985. doi: 10.1525/aa.1966.68.4.02a00070. [DOI] [Google Scholar]
- 32.Matsumoto D. Culture and nonverbal behavior. Handbook of nonverbal communication 2006;219–35
- 33.Hillen MA, de Haes JCJM, van Tienhoven G, et al. All eyes on the patient—the influence of oncologists’ nonverbal communication on breast cancer patients’ trust. Breast Cancer Res Tr. 2015;153:161–171. doi: 10.1007/s10549-015-3486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Vliet LM, Verheul W, Van der Wall E, Bensing JM. The validity of using analogue patients in practitioner-patient communication research: systematic review and meta-analysis. J Gen Intern Med. 2012;27:1528–1543. doi: 10.1007/s11606-012-2111-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dupont WD. Power calculations for matched case-control studies. Biometrics 1988;1157–68. [PubMed]
- 36.Breslow NE, Day N. Statistical methods in cancer research vol 1-the analysis of case-control studies. Geneva, 1980,1980. [PubMed]
- 37.Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of controls in case-control studies: III. Design options. Am J Epidemiol. 1992;135:1042–1050. doi: 10.1093/oxfordjournals.aje.a116398. [DOI] [PubMed] [Google Scholar]
- 38.Van Vliet LM, Hillen MA, Van der Wall E, et al. How to create and administer scripted video-vignettes in an experimental study on disclosure of a palliative breast cancer diagnosis. Patient Educ Couns. 2013;91:56–64. doi: 10.1016/j.pec.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 39.Straten GFM, Friele RD, Groenewegen PP. Public trust in Dutch health care. Social Sci Med. 2002;55:227–234. doi: 10.1016/S0277-9536(01)00163-0. [DOI] [PubMed] [Google Scholar]
- 40.Visser LN, Hillen MA, Verdam MG et al. Assessing engagement while viewing video vignettes; validation of the Video Engagement Scale (VES). Patient Educ Counsel 2015. [DOI] [PubMed]
- 41.Hillen MA, cce Koning, Wilmink JW, et al. Assessing cancer patients’ trust in their oncologist: development and validation of the Trust in Oncologist Scale (TiOS) Support Care Cancer. 2012;20:1787–1795. doi: 10.1007/s00520-011-1276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hillen MA, Butow PN, Tattersall MHN, et al. Validation of the english version of the trust in oncologist scale (TiOS) Patient Educ Couns. 2013;91:25–28. doi: 10.1016/j.pec.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 43.IBM . SPSS statistics for windows, Version 20.0. In. Armonk: IBM Corp; 2011. [Google Scholar]
- 44.Hillen MA, Onderwater AT, Van Zwieten MCB, et al. Disentangling cancer patients’ trust in their oncologist: A qualitative study. Psychooncology. 2012;21:392–399. doi: 10.1002/pon.1910. [DOI] [PubMed] [Google Scholar]
- 45.Suurmond J, Seeleman C. Shared decision-making in an intercultural context. Barriers in the interaction between physicians and immigrant patients. Patient Educ Couns. 2006;60:253–259. doi: 10.1016/j.pec.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 46.Trill MD, Holland J. Cross-cultural differences in the care of patients with cancer. A review. Gen Hosp Psychiatry. 1993;15:21–30. doi: 10.1016/0163-8343(93)90087-5. [DOI] [PubMed] [Google Scholar]
- 47.Nichalkovit T, Hill JM, Holland JC. The effects of culture on illness behaviour and medical care: Asian and American differences. Gen Hosp Psychiat. 1993;15:41–50. doi: 10.1016/0163-8343(93)90090-B. [DOI] [PubMed] [Google Scholar]
- 48.Hoopman R, Terwee CB, Muller MJ, et al. Methodological challenges in quality of life research among Turkish and Moroccan ethnic minority cancer patients: translation, recruitment and ethical issues. Ethn Health. 2009;14:237–253. doi: 10.1080/13557850802398832. [DOI] [PubMed] [Google Scholar]
- 49.Moreno-John G, Gachie A, Fleming CM, et al. Ethnic minority older adults participating in clinical research: developing trust. J Aging Health. 2004;16:93S123S. doi: 10.1177/0898264304268151. [DOI] [PubMed] [Google Scholar]
- 50.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 51.Meeuwesen L, Harmsen JAM, Bernsen RMD, Bruijnzeels MA. Do Dutch doctors communicate differently with immigrant patients than with Dutch patients? Soc Sci Med. 2006;63:2407–2417. doi: 10.1016/j.socscimed.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 52.Van Wieringen JCM, Harmsen JAM, Bruijnzeels MA. Intercultural communication in general practice. Eur J Pub Health. 2002;12:63–68. doi: 10.1093/eurpub/12.1.63. [DOI] [PubMed] [Google Scholar]
- 53.Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med. 2000;51:657–668. doi: 10.1016/S0277-9536(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 54.Tarn DM, Meredith LS, Kagawa-Singer M, et al. Trust in one’s physician: the role of ethnic match, autonomy, acculturation, and religiosity among Japanese and Japanese Americans. Ann Fam Med. 2005;3:339–347. doi: 10.1370/afm.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.