Abstract
Introduction
Uganda has rapidly increased access to antimalarial medicines in an effort to address the huge malaria disease burden. Pharmacovigilance information is important to guide policy decisions.
Objectives
The purpose of this study was to establish the burden of adverse drug reactions (ADRs) and associated risk factors for developing ADRs to artemisinin-based antimalarial treatment in Uganda.
Methods
An active follow-up study was conducted between April and July 2017 in a cohort of patients receiving treatment for uncomplicated malaria in the Iganga, Mayuge, and Kampala districts.
Results
A total of 782 patients with a median age of 22 years (58.6% females) were recruited into this study, with the majority recruited from public health facilities (97%). Diagnostic tests before treatment were performed for 76% of patients, and 97% of patients received artemether/lumefantrine. The prevalence of ADRs was 22.5% (176/782); however, the total number of ADRs was 245 since some patients reported more than one ADR. The most commonly reported reactions were general body weakness (24%), headache (13%), and dizziness (11%). Women were more likely to develop an ADR (adjusted odds ratio [aOR] 1.8, 95% confidence interval [CI] 1.1–2.9), urban dwellers were more likely to develop an ADR than rural residents (aOR 9.9, 95% CI 5.4–17.9), and patients with comorbidities were more likely to develop an ADR than those without (aOR 7.4, 95% CI 4.4–12.3).
Conclusion
The burden of ADRs is high among women and in patients from urban settings and those with comorbidities. Such risk factors need to be considered in order to optimise therapy. Close monitoring of ADRs is key in implementation of the malaria treatment policy.
Electronic supplementary material
The online version of this article (10.1007/s40264-018-0659-x) contains supplementary material, which is available to authorized users.
Key Points
| Active follow-up studies present a viable avenue for establishing the burden of adverse drug reactions (ADRs) at the community level for ADRs reported by either patients or health workers. |
| With limited resources, it is possible to conduct active surveillance of ADRs for malaria patients in the community, with minimal loss to follow-up. |
| Health service delivery in both the private sector and in rural areas ought to be reviewed and improved so as to optimise therapy, especially in the treatment of malaria in children. |
Introduction
Pharmacovigilance has been defined as “the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem [1]. In Africa, approximately 40 countries have a pharmacovigilance centre with a clear mandate and organisational structure, either as a full or associate member of the World Health Organisation (WHO) programme of international drug monitoring [2]. The Uganda National Pharmacovigilance Centre (NPC) has been part of this programme for 10 years now. By September 2017, all of Africa contributed 0.9% of the 15.5 million individual case safety reports (ICSRs) in the global database [3]. The rate of reporting suspected ADRs in Uganda is approximately 10 per million inhabitants annually, which is below the 200 per million inhabitants frequently used as the standard for a well-performing system [4].
The change in the malaria treatment policy thrice in 6 years, based on evidence generated in-country that increased the accessibility of artemisinin-based combination therapy (ACT) up to community level, brought to the fore the need to establish the current pharmacovigilance system [7, 8]. This system was to monitor safety of the newly introduced ACTs, as well as all medicines. The suspected adverse drug reactions (ADRs) form was disseminated widely and incorporated into the national treatment guideline documents. Health workers were sensitised on the importance of pharmacovigilance of all drugs, with emphasis on the new ACTs and use of rapid diagnostic test kits prior to the treatment of malaria [9–11]. The current 2016 Uganda Clinical Guidelines identify first-line treatment for uncomplicated malaria as either artemether/lumefantrine (AL) or artesunate/amodiaquine (AS/AQ), second-line treatment as dihydroartemisinin/piperaquine (DHP), and quinine tablets in case second-line therapy is not available [12].
In 2014, Uganda introduced a new pharmacovigilance regulation that makes it mandatory for health professionals to report all suspected ADRs encountered during their practice [5]. There is a network of 14 regional pharmacovigilance centres (RPCs) based in the referral hospitals. The ADR data are entered into VigiFlow®, a web-based ICSR management tool used in the WHO Programme for International Drug Monitoring (PIDM) and maintained by the Uppsala Monitoring Centre (UMC) [6], at either the RPCs or the NPC. Since March 2016, healthcare professionals can enter the forms directly into Vigiflow® using the electronic reporting tool. There is a move towards establishing direct patient reporting of adverse reactions in Uganda.
The general public seeks care and treatment from the private sector as a first point of call, but many of these outlets have limited infrastructure and skills to give good-quality service, including reporting adverse events [13–15]. How patient-reported safety information is handled will determine future performance measurements of good-quality healthcare [16]. There is a growing body of evidence showing that patients who are more motivated have better health outcomes and care-seeking experiences. Policies and interventions aimed at strengthening patients’ roles in managing their healthcare can contribute to improved outcomes, and patient motivation can and should be measured as an intermediate outcome of care that is linked to improved outcomes [13]. There is a huge disease burden, which has led to greater medicines access in resource-limited healthcare systems that have weak regulatory systems. Therefore, the need to generate pharmacovigilance data is important to inform treatment policy decisions. The purpose of this study was to establish the burden of ADRs and associated risk factors for developing ADRs to artemisinin-based antimalarial treatment in Uganda. This study also sought to assess the proportion of suspected ADRs that could have been prevented.
Methodology
Design and Study Sites
This was an observational, active, follow-up study that was conducted in a cohort of subjects taking antimalarial drugs between April and July 2017. The study was conducted in randomly selected public and private health facilities and/or drug outlets in the Kampala and Iganga/Mayuge districts, representing urban and rural settings, respectively. The rural districts host the Iganga/Mayuge Health and Demographic Surveillance Site (IMHDSS) of Makerere University Centre for Health and Population Research (MUCHAP), which is an open population-based cohort serving as a platform for research and research training that longitudinally generates population-based data. The IMHDSS comprises 65 villages and 17,000 households, with a total population of 89,000 served by 17 community-based public health facilities in the Iganga and Mayuge districts [17]. Over 90% of the population resides in the rural areas. Iganga and Mayuge share a similar malaria burden and have received similar malaria control interventions from Uganda’s health sector.
According to the 2016 demographic health survey, Kampala is an urban district [18]. This urban population varies, from communities that can afford the option of private healthcare to those that seek treatment from the free public health services, private drug outlets, and ordinary shops [13, 19]. Kampala has slum settlements and the swamps have been encroached on in many parts of the city, which poses challenges for malaria reduction efforts and, consequently, high use of antimalarial drugs in such areas.
Sampling and Sample-Size Level
Random sampling was undertaken for health facilities or drug outlets and all public health facilities in the districts. A sample of the private sector drug outlets recognised by local community leaders as a regular source of healthcare were also randomly selected. The number of respondents selected from each facility or outlet catchment area was estimated using the Scheaffer formula of elementary survey sampling [20]. We assumed a proportion (p) with an acceptable level of 0.5, testing at the 0.05 level, and 80% power to detect a difference of at least 10% in the burden of ADRs between urban and rural settings, which gave a sample size of 384 in both the rural and urban groups. Considering a 5% anticipated loss to follow-up, the final sample for the study was 806 respondents. A large number was sampled from the urban population because of expected loss to follow-up due to mobility of people in the urban setting.
Patient Recruitment and Follow-Up
Patients treated for uncomplicated malaria and consenting to participation in the study by signing the informed consent form were enrolled. All patients with uncomplicated malaria confirmed by either a rapid diagnostic test or microscopy, or clinical assessment based on the presence of fever or a history of fever within the previous 24 h, were consecutively included in the study. All patients with complicated malaria were not included. Data were collected using a questionnaire administered face-to-face and filled in by trained research assistants. The questionnaires (see electronic supplementary material [ESM] 1) were pretested prior to the main data collection. Patient phone contact details were obtained at the time of filling in the pretreatment questionnaire that was used to capture the baseline clinical, demographic and treatment data. Patients were followed-up using phone calls, and health facility or home visits using a post-treatment questionnaire to capture their experience after treatment. A follow-up was made on days 3, 7 and 14. Using phone calls, patients reported whether they had developed an adverse drug event and the subsequent treatment outcome. Clinical outcome assessment was used for those visiting the facility or those visited at home to determine whether they were cured or not and whether they had developed an adverse drug event after taking an antimalarial drug. An adverse event is defined as any untoward medical occurence in a patient administered a medicinal product and which does not necessarily have to have a causal relationship with the treatment, including worsening of the clinical condition [21]. During follow-up, the national form for reporting suspected ADRs was filled in following identification of an ADR (see ESM 2).
Outcome Definition
An ADR is defined as a noxious and unintended response to a medicine [19]. All adverse events reported by participants were recorded by research assistants and assessed for suspected ADRs by trained professionals especially trained in pharmacovigilance. In this study, the suspected ADRs were either reported by patients or recorded by healthcare workers, and all were assessed by the principal investigator. The Naranjo algorithm (see ESM 3) was used for causality assessment of the suspected ADRs [22]. The event was classified as a suspected ADR if the two healthcare professionals agreed. In the case of no consensus, an expert view was sought from a clinician with experience in malaria treatment. All suspected ADRs were also categorised according to the Medical Dictionary for Regulatory Activities (MedDRA) System Organ Class (SOC) [23]. More than one drug can be suspected of having contributed to the outcome for each ADR. The generated ADRs were compared with those in the manufacturer’s product characteristics.
Method for Determining Preventability of Adverse Drug Reactions (ADRs)
To assess the preventability of ADRs, the P-method developed by the WHO Collaborating Centre for Pharmacovigilance in Rabat, Morocco, was adapted for this study. For the identified possible or probable ADRs, a score card adapted from the P-method (see ESM 4) was used to assess those ADRs that could have been prevented [24]. The score card categorised the factors associated with the ADR according to either health professional practice, quality of the drug, or patient characteristics. Factors related to professional practice investigated included incorrect dose, incorrect route of drug administration, and incorrect drug administration duration, among others. Factors associated with the quality of the drugs administered, including poor quality and counterfeit products, were assessed as part of the score card. Patient characteristics including noncompliance and self-medication with non-over-the-counter drugs were also assessed in the preventability analysis.
In this study, the ICSRs of patients taking antimalarials were assessed using the P-method to ascertain if they were due to medication errors and were hence preventable. The method was applied to the reported suspected adverse reactions after causality assessment using the Naranjo algorithm. Risk factors that increased the likelihood of the occurrence of ADRs were assessed using the 20 criteria in the P-method. A root-cause analysis was then conducted and the details of errors were tabulated.
Statistical Analysis
Data were collected and reviewed daily by the investigators. Data were double-entered into EpiData screens and checked for variations, which were then cross-checked with the raw data and corrected. Data were then exported to STATA for analysis. A line list was created to check for any gaps or inconsistencies. A comparison was made between the rural and urban health facilities with respect to the variables collected in terms of demographic characteristics, ownership of the facilities, malaria diagnostic testing and results prior to antimalarial treatment, the type of drugs administered, and comorbid disease conditions. The outcome variable was defined as developing an ADR or not. Univariate analysis was performed to get the frequencies of the variables in each group, while bivariate analysis was used to investigate associations. The findings were then subjected to multinomial logistic regression to assess potential risk factors for developing ADRs. Results were presented in tables using frequencies, associations, and adjusted odds ratios (ORs) with confidence intervals (CIs) and p values. Those variables whose association p value was < 0.05 were taken to be significant.
Results
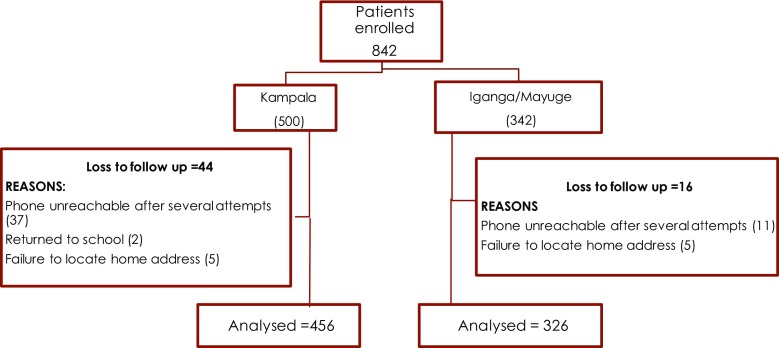
A total of 842 patients were recruited into the study from public and private health facilities; however, 60 patients (7%) did not have a post-treatment interview to assess adverse reactions due to loss to follow-up and were therefore not included in the final analysis data set. Of these 60 patients, 44 were from Kampala and 16 were from the Iganga/Mayuge area. The reasons for exclusion included phone contacts being unreachable after several trials and an inability to locate the homes of the patients. The flow diagram presented in Fig. 1 shows patient recruitment and follow-up from the two study areas.
Fig. 1.
Patient recruitment and follow-up
Participants in this study were followed up either by phone (91%), returning to the health facility, or a home visit. Seventy-nine of the patients in rural areas (Iganga/Mayuge) were followed up using phone calls, 11% returned to the health facility for follow-up, and 10% were visited at home. All patients in Kampala were followed up by phone, with the exception of three who visited a health facility and one who was visited at home.
Description of the Study Population
Overall, 782 (93%) patients were successfully followed up at least 3 days post-treatment. Analysis was conducted for those patients who completed the post-treatment questionnaire and is described in Table 1. Twenty-five pregnancies were reported—eight in the first trimester, nine in the second trimester, and another eight in the third trimester.
Table 1.
Characteristics of the respondents
| Variable | Kampala (urban) [n = 456 (58%)] | Iganga/Mayuge (rural) [n = 326 (42%)] | Total [N = 782] |
|---|---|---|---|
| Age, years [median (minimum–maximum)] | 25 (1–78) | 17 (1–73) | 22 (1–78) |
| Age groups, years | |||
| 0–4 | 49 (38.0) | 80 (62.0) | 129 |
| 5–10 | 64 (56.6) | 49 (43.4) | 113 |
| 11–18 | 29 (35.4) | 53 (64.6) | 82 |
| 19–29 | 145 (63.9) | 82 (36.1) | 227 |
| 30–39 | 97 (73.5) | 35 (26.5) | 132 |
| ≥ 40 | 72 (72.7) | 27 (27.3) | 99 |
| Sex | |||
| Male | 223 (68.8) | 101 (31.2) | 324 |
| Female | 233 (50.8) | 225 (49.1) | 458 |
| Pregnant women | 9 (36.0) | 16 (64.0) | 25 |
| First trimester | 4 (50.0) | 4 (50.0) | 8 |
| Second trimester | 3 (33.3) | 6 (66.7) | 9 |
| Third trimester | 2 (25.0) | 6 (75.0) | 8 |
| Facility ownership | |||
| Private | 23 (100.0) | 0 (0.0) | 23 |
| Public | 433 (57.0) | 326 (43.0) | 759 |
| Malaria diagnostic test performed | 272 (45.6) | 325 (54.4) | 597 |
| Test results | |||
| Negative | 40 (97.6) | 1 (2.4) | 41 |
| Positive | 232 (41.7) | 324 (58.3) | 556 |
| Not performed | 184 (99.5) | 1 (0.5) | 185 |
| Antimalarial drugs | |||
| First-line ACTs | 441 (58.0) | 320 (42.0) | 761 |
| Other antimalarial | 15 (71.4) | 6 (28.6) | 21 |
| Presence of comorbidities | 216 (64.7) | 118 (35.3) | 334 |
| HIV/AIDS | 72 (60.5) | 47 (39.5) | 119 |
| Tuberculosis | 79 (75.2) | 26 (24.8) | 105 |
| Peptic ulcers | 45 (62.5) | 27 (37.5) | 72 |
| Asthma | 19 (82.6) | 4 (17.4) | 23 |
| Hypertension | 1 (6.7) | 14 (93.3) | 15 |
The data in parentheses, apart from the first line are percentages
ACT artemisinin-based combination therapies
The majority (97%) of patients were recruited from public health facilities, and no patients from private health facilities were recruited from the rural area. Patients from urban settings (60%) were tested for malaria using microscopy or Rapid Diagnostic Kit (RDT) and by clinical assessment (40%) before treatment was administered, while all patients in the Iganga/Mayuge study site were tested using microscopy or RDT. All patients in this study received antimalarial treatment irrespective of whether or not a malaria diagnostic test was conducted prior to treatment. The majority of patients (97%) were prescribed AL. Of the 597 patients who were tested, 15% (40/272) from the Kampala region, compared with 0.3% (1/325), received treatment despite negative malaria test results. Ninety-seven percent of patients received first-line ACT antimalarial drugs. It was found that 57% (448/782) of patients were being treated for malaria only—64% from the rural area and approximately 53% from Kampala.
More patients from the urban setting reported comorbidities (64.7%) than from the rural study area (35.3%). The comorbidities reported among the 334 patients were HIV/AIDS (35.6%), tuberculosis (31.4%), peptic ulcers (21.5%), asthma (7%) and hypertension (4.5%).
Utilisation of Antimalarials in Pregnancy
Of the 458 women in the study, 25 (5.5%) used an antimalarial during pregnancy, of whom 21 used AL (84%). Eight pregnant women were in their first trimester, and, of those, three were treated with injectable artesunate and five with an oral ACT. Only one pregnant woman was treated with quinine in her second trimester, and eight were treated with an ACT in the same trimester. The other pregnant women were treated with AL in their third trimester.
The Burden of ADRs
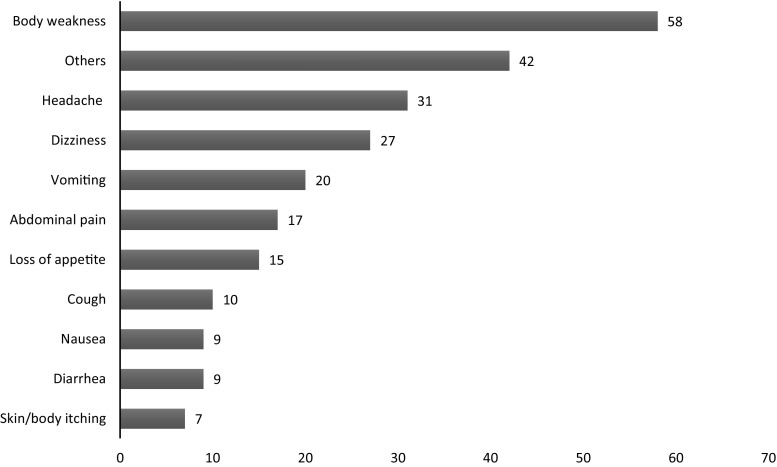
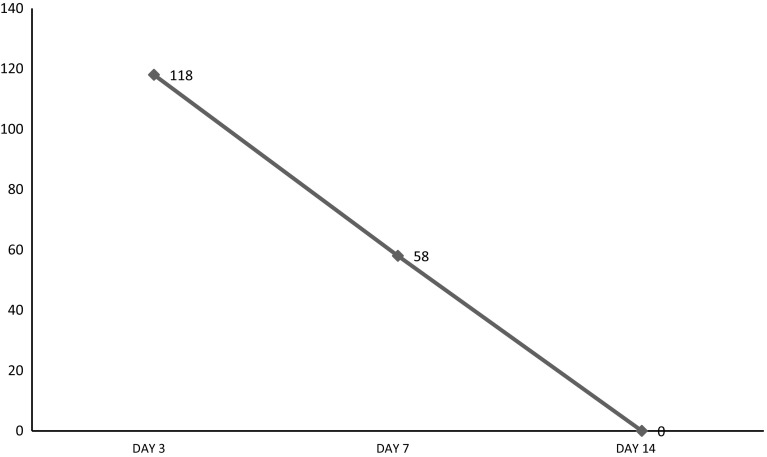
Of 782 patients who were successfully followed up, 22.5% (n = 176) developed ADRs subsequent to antimalarial treatment. Table 2 shows the distribution of suspected ADRs by the antimalarial drugs administered. Some patients reported more than one ADR, with a total of 245 ADRs being reported, as depicted in Fig. 2. The most commonly reported ADRs to antimalarials were body weakness (n = 58), headache (n = 31), dizziness (n = 27), vomiting (n = 20), abdominal pain (n = 17), loss of appetite (n = 15), cough (n = 10), diarrhoea (n = 9), nausea (n = 9), skin and body itching (n = 7), and others (n = 42). Other reported adverse reactions included cold, drowsiness, skin rash, high temperature, joint pain, backache, chest pain, convulsion, insomnia, oral sores, bitterness in the mouth, body pain, chills, diaphoresis, flu, heart burn, palpitations, stomach gas and yellowish urine (a percentage of 17.1%). Figure 3 shows the trend of adverse events reported on each day of follow-up. The SOC distribution of the reported ADRs according to MedDRA were gastrointestinal disorders (30.6%), musculoskeletal and connective tissue disorders (26.9%), nervous system disorders (26.5%), skin and subcutaneous tissue disorders (5.7%), and respiratory, thoracic and mediastinal disorders (4.1%), with the rest contributing up to 6%. All ICSRs were assessed for causality according to the Naranjo algorithm. Twelve ICSRs were classified as doubtful, 209 reports as possibly related, and 24 as probably related to the antimalarial treatment.
Table 2.
Antimalarial drugs and the respective ADRs reported
| Drug name | No. of patients | No. of patients reporting at least one suspected ADR (%) |
|---|---|---|
| ALU | 761 | 174 (22.9) |
| ASAQ | 11 | 2 (18.2) |
| DHAPQ | 3 | 0 (0) |
| Others | 7 | 0 (0) |
| Total | 782 | 176 (22.5) |
ADRs adverse drug reactions, ALU artemether/lumefantrine, ASAQ artesunate/amodiaquine, DHAPQ dihydroartemisinin/piperaquine
Fig. 2.
Commonly reported adverse drug reactions
Fig. 3.
Number of reported events on follow-up days
Risk Factors for Developing an ADR After Taking an Antimalarial Treatment
The findings were subjected to multinomial logistic regressions for potential risk factors for developing an ADR after taking an antimalarial drug. From the results presented in Table 3, sex was statistically significant, with women at higher risk of developing ADRs than men (OR 1.8, 95% CI 1.1–2.9). Patients from Kampala were found to be at higher risk of developing ADRs than those from Iganga/Mayuge (OR 9.9, 95% CI 5.4–17.9), and patients who had comorbidities were seven times more likely to develop adverse reactions than those who did not (OR 7.4, 95% CI 4.4–12.3).
Table 3.
Analysis of the determinants of developing an ADR after taking an antimalarial
| Variables | Total no. of patients (%) | Unadjusted OR | 95% CI | p value | Adjusted OR | 95% CI | p value |
|---|---|---|---|---|---|---|---|
| Total | 782 | ||||||
| Age groups, years | |||||||
| 0–18 | 324 (41.4) | 1.0 | – | – | – | – | – |
| ≥ 19 | 458 (58.6) | 1.9 | 1.3–2.8 | 0.00 | 1.5 | 0.9–2.5 | 0.09 |
| Sex | |||||||
| Male | 324 (41.4) | 1.0 | – | – | |||
| Female | 458 (58.6) | 1.1 | 0.7–1.4 | 0.87 | 1.8 | 1.1–2.9 | 0.03 |
| Facility type | |||||||
| Public | 759 (93.2) | 1.0 | – | – | |||
| Private | 23 (2.9) | 1.2 | 0.5–3.2 | 0.68 | 2.117 | 0.6–7.3 | 0.24 |
| Residence | |||||||
| Iganga/Mayuge | 456 (58.3) | 1.0 | – | – | |||
| Kampala | 326 (41.7) | 7.1 | 4.4–11.3 | 0.00 | 9.9 | 5.4–17.9 | 0.00 |
| Diagnostic test results | |||||||
| Negative | 41 (5.2) | 1.0 | – | – | – | – | – |
| Positive | 556 (71.1) | 1.7 | 0.8–3.5 | 0.13 | 1.5 | 0.6–3.4 | 0.36 |
| No test performed | 185 (23.7) | 1.3 | 0.03–2.9 | 0.42 | 3.8 | 1.7–6.2 | 0.21 |
| Antimalarial drugs | |||||||
| Other antimalarials | 21 (2.7) | 1.0 | |||||
| First-line ACTs | 761 (97.3) | 1.8 | 0.5–6.1 | 0.37 | 2.4 | 0.4–14.3 | 0.32 |
| Comorbidities | |||||||
| No | 448 (57.3) | 1.0 | – | – | – | – | – |
| Yes | 334 (42.7) | 8.6 | 5.7–12.9 | 0.00 | 7.4 | 4.4–12.3 | 0.00 |
OR odds ratio, ADR adverse drug reaction, ACT artemisinin-based combination therapy, CI confidence interval
Determinants of Developing an ADR After Taking Any Medicine Within the Past 14 Days
Patients were asked if they had taken any medicine in the 14 days prior to their visit to the drug outlet. A multinomial logistic regression analysis was carried out to assess the determinants of developing an ADR after taking any medicine within the past 14 days, and it was found that urban residents were 2.5-fold more likely to develop adverse reactions than those from rural areas (OR 2.5, 95% CI 1.38–4.54), as shown in Table 4.
Table 4.
Determinants of developing an ADR after taking any medicine within the past 14 days
| Variables | No. of observations (%) | Unadjusted OR | 95% CI | p value | Adjusted OR | 95% CI | p value |
|---|---|---|---|---|---|---|---|
| Total | 782 | ||||||
| Age groups, years | |||||||
| ≥ 19 | 458 (58.6) | 1.00 | – | – | – | – | – |
| 0–18 | 324 (41.4) | 1.04 | 0.63–1.70 | 0.88 | 1.34 | 0.80–2.24 | 0.27 |
| Sex | |||||||
| Male | 324 (41.4) | 1.00 | – | – | |||
| Female | 458 (58.6) | 1.03 | 0.63–1.69 | 0.91 | 1.19 | 0.72–1.99 | 0.48 |
| Facility type | |||||||
| Public | 759 (93.2) | 1.00 | – | – | |||
| Private | 23 (2.9) | 2.92 | 1.05–8.11 | 0.40 | 2.19 | 0.77–6.19 | 0.14 |
| Residence | |||||||
| Iganga/Mayuge | 456 (58.3) | 1.00 | – | – | |||
| Kampala | 326 (41.7) | 2.44 | 1.43–4.31 | 0.00 | 2.50 | 1.38–4.54 | 0.00 |
| Comorbidities | |||||||
| No | 448 (57.3) | 1.00 | – | – | – | – | – |
| Yes | 334 (42.7) | 1.4 | 0.9–2.3 | 0.16 | 1.32 | 0.81–2.17 | 0.28 |
OR odds ratio, ADR adverse drug reaction, CI confidence interval
Preventability of the ADRs
The criteria for preventability assessment according to the P-method was applied to all suspected ADRs that were possibly and probably related to antimalarials. The proportion of ADRs that could have been prevented was found to be 3% (7/233) [see Table 5 below]. All seven errors were due to inappropriate dosing of patients and inadvertent drug administration. Among these errors, three were patients who were administered intravenous artesunate, which is recommended for severe malaria according to Ugandan treatment guidelines. In addition, patients were administered a dose less than what is recommended in the summary of product characteristics. The remaining four errors were children administered an overdose of artemether-lumefantrine according to their weight in the same treatment guidelines.
Table 5.
List of medication errors identified
| Patient initials | Age, years | Weight, kg | Daily dose of ACT administered | Total dose administered | Recommended dose of artemisinin-based antimalarial treatment | Total recommended dose | Absolute difference = total dose administered − total recommended dose(% dose difference from recommended dose) |
|---|---|---|---|---|---|---|---|
| NR | 21 | 53.0 | 120 mg intravenous artesunate | 120 mg | 127.2 mg intravenous artesunate (2.4 mg/kg) | 127.2 mg | 7.2 mg intravenous artesunate (6% less) |
| KF | 25 | 55.0 | 120 mg intravenous artesunate | 120 mg | 132.0 mg intravenous artesunate (2.4 mg/kg) | 132.0 mg | 12.0 mg intravenous artesunate (9% less) |
| MF | 24 | 60.0 | 120 mg intravenous artesunate | 120 mg | 144.0 mg intravenous artesunate (2.4 mg/kg) | 144.0 mg | 24 mg intravenous artesunate (17% less) |
| AM | 06 | 20.0 | Three tablets twice daily (60 mg artemether/360 mg lumefantrine) | 360 mg artemether/2160 mg lumefantrine | Two tablets twice daily (weight 15–24 kg, 3–7 years) | 240 mg artemether/1440 mg lumefantrine | 120 mg artemether/720 mg Lumefantrine (50% more) |
| NRH | 03 | 14.2 | Two tablets twice daily (40 mg artemether/240 mg lumefantrine) | 240 mg artemether/1440 mg lumefantrine | One tablet twice daily (weight 5–14 kg, 4 months–3 years) | 120 mg artemether/720 mg lumefantrine | 120 mg artemether/720 mg lumefantrine (100% more) |
| NF | 06 | 19.0 | Three tablets twice daily (60 mg artemether/360 mg lumefantrine) | 360 mg artemether/2160 mg lumefantrine | Two tablets twice daily (weight 15–24 kg, 3–7 years) | 240 mg artemether/1440 mg lumefantrine | 120 mg artemether/720 mg lumefantrine (50% more) |
| MV | 09 | 27.0 | Two tablets twice daily (40 mg artemether/240 mg lumefantrine) | 240 mg artemether/1440 mg lumefantrine | Three tablets twice daily (weight 25–34 kg, 7–12 years) | 360 mg artemether/2160 mg lumefantrine | 120 mg artemether/720 mg lumefantrine (50% less) |
Discussion
The burden of suspected ADRs following exposure to antimalarial treatment of almost one in every four patients taking antimalarial drugs is high. A Ugandan study established the burden of ADRs in the hospital setting [25], however this is the first study to document the burden of ADRs to antimalarial drugs in the community setting with an active follow-up methodology. ACTs for uncomplicated malaria are available at the community level and this study was set to understand the issues around the implementation of this policy. The majority of patients were prescribed AL that is administered at home for 3 days. Giving community members and patients the opportunity to participate in their own healthcare by reporting suspected ADRs is an important step in building trust in the country’s health system. Pharmacovigilance in the community setting introduced a platform to identify and mitigate ADRs. The risk factors associated with developing an ADR after taking antimalarial drugs were highlighted as sex, area of residence and comorbidities.
The most commonly reported reactions in our study were general body weakness, headache, dizziness, vomiting, abdominal pain and loss of appetite, among others. The burden reported from other ACT safety studies was up to 5% for clinical trials and postmarketing studies [26–30]. The reported reactions to the most commonly used drug (AL) were of a similar type to those in the summary of product characteristics [26, 27, 30]. Postmarketing studies conducted in other parts of Africa also revealed a similar pattern of the most commonly reported ADRs [31, 32]. The Ugandan ADR reports for the AL substance, including instances where AL is reported as a concomitant medication in Vigilyze, exhibits a different pattern of more than 50% skin and subcutaneous disorders. Our study revealed that the most affected SOCs were the gastrointestinal system, the musculoskeletal and connective tissue, and the nervous system. The Vigilyze reports are mainly from healthcare professionals, whereas our study had direct contact with patients. These results emphasize the need to establish a system for direct patient reporting of suspected ADRs.
Women had an 80% higher risk of developing ADRs than men, similar to other studies that reported a greater risk of between 50 and 70% for females [32–35]. The higher risk could be due to the innate biological, physiological, immunological, pharmacogenetic, pharmacokinetic and pharmacodynamic differences between the two sexes [36–38]. An alternative explanation is that women have had a lower inclusion rate into clinical trials, yet these are the only data available to compare with postmarketing studies. The higher risk for women could also be explained by the generally higher compliance level to healthcare, resulting in a higher tendency to communicating adverse reactions much earlier than men. Sex-related differences in the use of medicines also contribute to the ADR risk profile for women, given that they use oral contraceptives, iron and other supplements during pregnancy, hormones, and other products for menopausal women. Medicines are administered, even during the first trimester of pregnancy, with less caution than is required. In this study, we found that 8 of 25 self-reported pregnant women received ACTs in their first trimester, when all medicines must be avoided. This finding means that there should be more monitoring of ADRs for women and more sensitisation about these issues should be done. Many more women could be taking other drugs during their first trimester and more research in drug utilisation is needed. Registries should be established to study the long-term effect of ACTs on these babies when they are born. A better understanding of the sex-related differences and the mechanism of how these affect drug response is needed so as to optimise drug therapy in both men and women.
Our study found that patients in urban areas were more likely to report ADRs to antimalarial treatment than those in the rural areas. This is possibly because the urban population is more enlightened, has more access to information, better health infrastructure and more experienced health workers, which makes it easier to detect, identify and report the suspected ADRs than in rural areas. Other studies have also found that the difference in health-seeking behaviour between the urban and rural populations, where urban households are more likely to consult, be admitted to hospital, report illness, and spend relatively more on healthcare, increases the burden of ADRs in urban settings [39]. According to the 2014 national census report, the bulk of Uganda’s population lives in rural areas such as Iganga/Mayuge, and is mainly composed of women [45]. The literacy rate of rural women (63%) is much lower than that of their urban counterparts (84%). The urban population reported more comorbidities than those from rural areas. A similar pattern in the rural–urban divide of private and public health facilities has been revealed by other studies [38–42, 44]. This has policy implications for access to medicines because the urban population is approximately one-fifth of the Ugandan population, yet it has 80% of the private health facilities [43]. There must be some redistribution of health service delivery and re-equipping private sector health facilities to provide better services to the rural areas. A country-wide sensitisation programme for pharmacovigilance would be a useful tool to aid this redistribution and improved interaction with the healthcare system; however, pharmacovigilance messages must be customised to the rural setting so as to achieve the best results.
It was found that patients with comorbidities were more likely to report an adverse reaction than those without comorbidities. A study from Nigeria indicated that patients with comorbidity were threefold more likely to have ADRs than those without [46]. The difference in the magnitude of the risk could be due to the differences in the case-control study design they used and also the fact that our study evaluated treatment of a single malaria episode with comorbidities. The Nigerian study retrospectively looked at ACT safety data that had been collected in a large cohort of patients over a long period of time. Comorbidity increases the risk to ADRs as multiple diseases often means more medicines used; however, this increased use is also riddled with polypharmacy. Various studies have found that HIV increases the risk of malaria infection and clinical malaria in adults, especially in those with advanced immunosuppression [46, 47]. In our study, the comorbidities reported were HIV/AIDS, tuberculosis, peptic ulcers, asthma and hypertension. Some studies have suggested that the interactions of all antiretrovirals with AL may require higher doses for HIV patients, and possibly tuberculosis patients [46–50]; however, this effect was outside the scope of this study. The importance of this finding is that healthcare providers must closely monitor patients with comorbidity so as to optimise their therapy and prevent adverse reactions.
The proportion of medication errors found in our study was 3% of all possible ADRs. All errors identified were due to dosing. This finding was lower than the 11% found in Morocco [51]. The explanation for such a low level of error could be that in an outpatient or community setting, the other types of errors are difficult to identify, given that even the health worker’s suspicion index for disease is low. The culture of documenting patient history and all that happens during the course of treatment is a challenge in Uganda, more so in an outpatient setting. There were many missed opportunities to capture medication errors as practitioners fear to implicate themselves, as some Ugandan researchers established [52]. In three cases, underdosing was seen for intravenous artesunate, a practice that could potentially contribute to antimicrobial drug resistance. The magnitude of this practice in other parts of the country is not clear; however, it is important to note that the practice of administering injectable artesunate for uncomplicated malaria is not recommended by the guidelines. Four of the cases were overdosed up to twice the recommended dose for AL tablets. The extra medication administered to the four children identified in this study could have treated up to three children with similar age and weight. This has implications for cost savings for the national malaria control programme if, for every four doses of tablets for children, up to seven children could be treated. Drug utilisation studies ought to be conducted to assess the actual and potential cost savings of current treatment practices for children in Uganda. A system, as well as policies and procedures, need to be developed to detect and prevent error in Ugandan health facilities and drug outlets.
This study had limitations. The 7% rate of loss to follow-up was slightly more than expected; however, it was not such a big loss considering that the study was a form of active surveillance of malaria patients in the community. Most patients preferred to be followed up on the phone. Second, during filling in of the pretreatment forms, patients were asked about their medication history based on the past 14 days, which could have introduced some recall bias. Although the interviewers were trained to probe for information on concomitant medication, there seems to have been an underdeclaration on herbal medication being used, especially by the rural communities. Third, there were few private healthcare facilities because many of them that were included in the study had a lower patient load. In fact, we did not interview any patients attending private health facilities in the rural areas. It is also important to note that a few of the private health facilities were hesitant to participate in the study, which could have introduced some bias, but these cases were minimal. Limitations in sample size have hampered a more stratified analysis according to facility types. The results may only be generalisable to areas with similar distribution of private facilities and operational capabilities. Another limitation related to sample size was pregnancy. Since this was an active follow-up study, the method of identification was self-report and this could have led to either an under- or overestimate of its effect on developing an ADR; however, this could not be ascertained due to the small numbers identified. Furthermore, the classification of Iganga/Mayuge as a rural area may be a bit misleading as several studies have been conducted in the health demographic surveillance site, as was evidenced by the lower rate (4%) of patients lost to follow-up compared with the Kampala region (8%). The results of this study need to be generalised with caution in this respect.
Conclusions
ACTs are still highly effective in the treatment of uncomplicated malaria, however the concerns regarding safety and tolerability seem to be increasing, with more experience in the general population [53]. The burden of one ADR for every four patients taking ACTs for uncomplicated malaria is high. The pattern of ADRs reported is also different from what is in the current national pharmacovigilance database filled in by healthcare professionals. In this study, women were more predisposed to developing ADRs, as well as patients with other underlying disease conditions. These special cases need to be studied further so that appropriate steps can be taken to protect them. Another area that needs to be considered in optimising therapy to the majority of Ugandans is the treatment-seeking behaviour of urban versus rural dwellers. In addition, looking at the types of medication errors that have been identified, future studies should investigate emerging drug resistance and its risk factors. More areas for research include drug utilisation and cost-analysis studies for pediatric drug treatment. The policy and practices of malaria treatment should be reviewed so as to identify areas that can be strengthened.
Finally, this study has demonstrated that active surveillance of patients in the community can be done without any major loss to follow-up, and the methods used in this study are less resource-demanding compared with cohort event monitoring and postregistration clinical trials. It will provide important lessons for active monitoring of treatment in resource-limited settings.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors express their profound gratitude to all patients who participated in this study. We are very grateful to the National Drug Authority for funding this study and to the Makerere University Centre for Health and Population Research team for letting us use the IgangaMayuge Health and Demographic Surveillance Site as a platform for data collection and data processing. Gratitude also goes to all research assistants who spent long hours during data collection and analysis. Finally, we thank the study participants in Iganga, Mayuge districts and Kampala Capital City Authority as well as leadership in those areas for allowing us to access all public health facilities at our convenience.
Compliance with Ethical Standards
Ethical clearance was obtained from the Mildmay Uganda Research Ethics Committee (REC REF 0604-2017) and the Uganda National Council for Science and Technology (HS 2247), which provides ethics research clearance at the national level in accordance with the World Medical Association Helsinki Declaration. Approval for the study was obtained from the National Drug Authority and Makerere University Centre for Health and Population Research.
Funding
No sources of funding were used to assist in the preparation of this study.
Conflicts of interest
Helen Byomire Ndagije, Victoria Nambasa, Leonard Manirakiza, Donna Kusemererwa, Dan Kajungu, Niko Speybroeck and Sten Olsson have no conflicts of interest that are directly relevant to the content of this study.
Footnotes
Electronic supplementary material
The online version of this article (10.1007/s40264-018-0659-x) contains supplementary material, which is available to authorized users.
A comment to this article is available online at https://doi.org/10.1007/s40264-018-0677-8.
References
- 1.World Health Organization. The Importance of Pharmacovigilance: Safety Monitoring of medicinal products. World Health Organization; 2002. Available at: http://apps.who.int/medicinedocs/pdf/s4893e/s4893e.pdf.
- 2.Uppsala Monitoring Centre. Members of the WHO Programme for International Drug Monitoring [cited 27 Feb 2018]. Available at: https://www.who-umc.org/global-pharmacovigilance/members/who-programme-members/.
- 3.Uppsala Monitoring Centre. Vigilyze Statistics for Africa. 2017 [cited 2 Oct 2017]. Available at: https://vigilyze.who-umc.org/#/.
- 4.Olsson S. The role of the WHO programme on International Drug Monitoring in coordinating worldwide drug safety efforts. Drug Saf. 1998;19(1):1–10. doi: 10.2165/00002018-199819010-00001. [DOI] [PubMed] [Google Scholar]
- 5.The Uganda Gazette. The National Drug Policy and Authority (Pharmacovigilance) Regulations, 2014. Pub.L. No. 37 Uganda; 2014; pp. 1263–72. Available at: http://www.nda.or.ug/files/downloads/PharmacovigilanceRegulation.pdf.
- 6.Uppsala Monitoring Centre. Vigiflow. 2017 [cited 11 Sep 2017]. Available at: https://www.who-umc.org/global-pharmacovigilance/vigiflow/about-vigiflow/.
- 7.Nabyonga-Orem J, Ssengooba F, MacQ J, Criel B. Malaria treatment policy change in Uganda: what role did evidence play? Malar J. 2014;13(1):345. doi: 10.1186/1475-2875-13-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ACTwatch. Household Survey Uganda 2012 Survey Report. Kampala; 2012. Available at: http://www.actwatch.info/sites/default/files/content/publications/attachments/ACTwatch Uganda2013OSReferenceDocument18Aug2015.pdf.
- 9.Bastiaens GJH, Bousema T, Leslie T. Scale-up of malaria rapid diagnostic tests and artemisinin-based combination therapy: challenges and perspectives in Sub-Saharan Africa. PLoS Med. 2014;11(1):e1001590. doi: 10.1371/journal.pmed.1001590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fink G, Dickens WT, Jordan M, Cohen JL. Access to subsidized ACT and malaria treatment: evidence from the first year of the AMFm program in six districts in Uganda. Health Policy Plan. 2014;29:517–527. doi: 10.1093/heapol/czt041. [DOI] [PubMed] [Google Scholar]
- 11.Mbonye AK, Magnussen P, Chandler CIR, Hansen KS, Lal S, Cundill B, et al. Introducing rapid diagnostic tests for malaria into drug shops in Uganda: design and implementation of a cluster randomized trial. Trials. 2014;15(1):303. doi: 10.1186/1745-6215-15-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministry of Health Uganda . Uganda Clinical Guidelines, National Guidelines for management of Common conditions. Kampala: Ministry of Health Uganda; 2016. [Google Scholar]
- 13.Konde-Lule J, Gitta SN, Lindfors A, Okuonzi S, Onama VON, Forsberg BC. Private and public health care in rural areas of Uganda. BMC Int Health Hum Rights. 2010;10:29–36. doi: 10.1186/1472-698X-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rutebemberwa E, Pariyo G, Peterson S, Tomson G, Kallander K. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malar J. 2009;8(1):45. doi: 10.1186/1475-2875-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodman C, Brieger W, Unwin A, Mills A, Meek S, Greer G. Medicine sellers and malaria treatment in sub-Saharan Africa: what do they do and how can their practice be improved? Am J Trop Med Hyg. 2007;77(Suppl. 6):203–218. [PMC free article] [PubMed] [Google Scholar]
- 16.Persell SD. Envisioning the Next Generation of Performance Measures for Ambulatory Care. Expert Commentary. 2009 [cited 3 Oct 2016]. Available at: https://www.qualitymeasures.ahrq.gov/expert/expert-commentary/16455.
- 17.Uganda Bureau of Statistics (2016). National Population and Housing Census Report 2014. Available at: http://www.ubos.org/onlinefiles/uploads/ubos/NPHC/2014NationalCensusMainReport.pdf.
- 18.Uganda Bureau of Statistics. Uganda Demographic and Health Survey. Kampala: Uganda Bureau of Statistics; 2016. Available at: http://www.ubos.org/onlinefiles/uploads/ubos/pdf documents/Uganda_DHS_2016_KIR.pdf.
- 19.Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. 2012;9(6):19. doi: 10.1371/journal.pmed.1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scheaffer RL, Mendenhall W III, Ott RL, Bergson-Michelson. In: Cnxkett C, Day A, Nemer J, editors. Elementary survey sampling. 6th ed. Belmont, CA: Duxbury Press, Thompson Corporation; 2006. p. 265–300.
- 21.Uppsala Monitoring Centre. Glossary of pharmacovigilance terms. 2017 [cited 27 Feb 2018]. Available at: https://www.who-umc.org/global-pharmacovigilance/global-pharmacovigilance/glossary/.
- 22.Naranjo C, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts E, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 23.The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. Medical Dictionary for Drug Regulatory Activities [cited 2 Oct 2017]. Available at: https://www.meddra.org.
- 24.Bencheikh RS, Benabdallah G. Medication errors: pharmacovigilance centres in detection and prevention. Br J Clin Pharmacol. 2009;67:687–690. doi: 10.1111/j.1365-2125.2009.03426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kiguba R, Karamagi C, Bird SM. Antibiotic-associated suspected adverse drug reactions among hospitalized patients in Uganda: a prospective cohort study. Pharmacol Res Perspect. 2017;5(2):e00298. doi: 10.1002/prp2.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Novartis. Summary of Product Characteristics for Coartem (Artemether/Lumefantrine) Tablets. 2009 [cited 2 Oct 2017]. Available at: https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/coartem.pdf.
- 27.Alfasigma S.p.A. Summary of Product Characteristics of Eurartesim tablets. 2011 [cited 2 Oct 2017]. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001199/WC500118113.pdf.
- 28.Byakika-Kibwika P, Lamorde M, Mayanja-Kizza H, Khoo S, Merry C, Van geertruyden J-P. Artemether-lumefantrine combination therapy for treatment of uncomplicated malaria: the potential for complex interactions with antiretroviral drugs in hiv-infected individuals. Malar Res Treat. 2011;2011:703730. [DOI] [PMC free article] [PubMed]
- 29.Adisa R, Fakeye TO, Dike D. Evaluation of adverse drug reactions to artemisinin-based combination therapy in a Nigeria university community. Trop J Pharm Res. 2008;7(2):937–944. doi: 10.4314/tjpr.v7i2.14680. [DOI] [Google Scholar]
- 30.World Health Organisation. Summary of Product Characteristics for Lumartem (Artemether/Lumefantrine) Tablets. 2012 [cited 2 Oct 2017]. Available at: https://extranet.who.int/prequal/sites/default/files/documents/MA064part4v2.pdf.
- 31.Dodoo ANO, Fogg C, Nartey ET, Ferreira GLC, Adjei GO, Kudzi W, et al. Profile of adverse events in patients receiving treatment for malaria in urban Ghana: a cohort-event monitoring study. Drug Saf. 2014;37(6):433–448. doi: 10.1007/s40264-014-0164-9. [DOI] [PubMed] [Google Scholar]
- 32.Kalilani-Phiri LV, Lungu D, Coghlan R. Knowledge and malaria treatment practices using artemisinin combination therapy (ACT) in Malawi: survey of health professionals. Malar J. 2011;10:279. doi: 10.1186/1475-2875-10-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lucca J, Ramesh M, Ram D. Gender differences in the occurrences and pattern of adverse drug reactions in psychiatric patients: a prospective observational study. Trop J Med Res. 2017;20(1):84–90. doi: 10.4103/1119-0388.198134. [DOI] [Google Scholar]
- 34.Franconi F, Brunelleschi S, Steardo L, Cuomo V. Gender differences in drug responses. Pharmacol Res. 2007;55:81–95. doi: 10.1016/j.phrs.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Rademaker M. Do women have more adverse drug reactions? Am J Clin Dermatol. 2001;2:349–351. doi: 10.2165/00128071-200102060-00001. [DOI] [PubMed] [Google Scholar]
- 36.Pouyanne P, Haramburu F, Imbs JL, Bégaud B. Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. French Pharmacovigilance Centres. BMJ. 2000;320(7241):1036. doi: 10.1136/bmj.320.7241.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aichhorn W, Whitworth AB, Weiss EM, Marksteiner J. Second-generation antipsychotics: is there evidence for sex differences in pharmacokinetic and adverse effect profiles? Drug Saf. 2006;29:587–598. doi: 10.2165/00002018-200629070-00004. [DOI] [PubMed] [Google Scholar]
- 38.Thompson R, Miller N, Witter S. Health-seeking behaviour and rural/urban variation in Kazakhstan. Health Econ. 2003;12(7):553–564. doi: 10.1002/hec.749. [DOI] [PubMed] [Google Scholar]
- 39.Whitley H, Lindsey W. Sex-based differences in drug activity. Am Fam Physician. 2009;80(11):1254–1258. [PubMed] [Google Scholar]
- 40.Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009;48(3):143–157. doi: 10.2165/00003088-200948030-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rutebemberwa E, Buregyeya E, Lal S, Clarke SE, Hansen KS, Magnussen P, et al. Assessing the potential of rural and urban private facilities in implementing child health interventions in Mukono district, central Uganda-a cross sectional study. BMC Health Serv Res. 2016;16(1):268. doi: 10.1186/s12913-016-1529-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Konde-Lule J, Gitta SN, Lindfors A, Okuonzi S, Onama VO, Forsberg BC. Private and public health care in rural areas of Uganda. BMC Int Health Hum Rights. 2010;10(1):29. doi: 10.1186/1472-698X-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Konde-lule J, Okuonzi S, Matsiko C, Mukanga D, Onama V, Gitta SN. The potential of the private sector to improve health outcomes in Uganda. Kampala; 2006.
- 44.Wafula FN, Miriti EM, Goodman CA. Examining characteristics, knowledge and regulatory practices of specialized drug shops in Sub-Saharan Africa: a systematic review of the literature. BMC Health Serv Res. 2012;12:223. doi: 10.1186/1472-6963-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Population secretariat. The State of Uganda Population Report (2014) Kampala: Ministry of Finance, Planning and Economic Development; 2014.
- 46.Bassi PU, Osakwe AI, Ogar CK, Elagbaje C, Nwankwo BB, Balogun ST, et al. Impact of comorbidity on adverse drug reaction profile in a cohort of patients treated with artemisinin combination therapies for uncomplicated malaria in Nigeria. Pharmacol Res Perspect. 2017;5(2):e00302. doi: 10.1002/prp2.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mehta U, Durrheim DN, Blockman M, Kredo T, Gounden R, Barnes KI. Adverse drug reactions in adult medical inpatients in a South African hospital serving a community with a high HIV/AIDS prevalence: prospective observational study. Br J Clin Pharmacol. 2008;65(3):396–406. doi: 10.1111/j.1365-2125.2007.03034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whitworth J, Morgan D, Quigley M, Smith A, Mayanja B, Eotu H, et al. Effect of HIV-1 and increasing immunosuppression on malaria parasitaemia and clinical episodes in adults in rural Uganda: a cohort study. Lancet. 2000;356(9235):1051–1056. doi: 10.1016/S0140-6736(00)02727-6. [DOI] [PubMed] [Google Scholar]
- 49.Byakika-Kibwika P, Lamorde M, Mayito J, Nabukeera L, Namakula R, Mayanja-Kizza H, et al. Significant pharmacokinetic interactions between artemether/lumefantrine and efavirenz or nevirapine in HIV-infected Ugandan adults. J Antimicrob Chemother. 2012;67(9):2213–2221. doi: 10.1093/jac/dks207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoglund RM, Byakika-Kibwika P, Lamorde M, Merry C, Ashton M, Hanpithakpong W, et al. Artemether-lumefantrine co-administration with antiretrovirals: population pharmacokinetics and dosing implications. Br J Clin Pharmacol. 2015;79(4):636–649. doi: 10.1111/bcp.12529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jennane N, Madani N, Oulderrkhis R, Abidi K, Khoudri I, Belayachi J, et al. Incidence of medication errors in a Moroccan medical intensive care unit. Int Arch Med. 2011;4:32. doi: 10.1186/1755-7682-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kiguba R, Waako P, Ndagije HB, Karamagi C. Medication error disclosure and attitudes to reporting by healthcare professionals in a sub-saharan African setting: a survey in Uganda. Drugs Real World Outcomes. 2015;2(3):273–287. doi: 10.1007/s40801-015-0032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Solmi M, Murru A, Pacchiarotti I, Undurraga J, Veronese N, Fornaro M, et al. Safety, tolerability, and risks associated with first-and second-generation antipsychotics: a state-of-the-art clinical review. Ther Clin Risk Manag. 2017;13:757–777. doi: 10.2147/TCRM.S117321. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.