Abstract
Purpose
The purpose of this study was to investigate the disclosure incidence of cancer diagnosis to patients before chemotherapy, to survey the attitudes of the patients and their families and related influencing factors toward disclosure of cancer diagnosis, and to compare the anxiety and depression levels between the disclosure and non-disclosure patients.
Participants and methods
A prospective cohort study was conducted at a tertiary hospital in China. A consecutive series of patients who had been diagnosed with malignancy by pathology and their family member were included in our study from March 2017 to December 2017. Patients’ situation, preferences, and their family members’ preferences were investigated by a self-designed questionnaire following a semi-structured interview. The Chinese version of HADS for anxiety and depression was used to test the patients’ psychological distress. Binary logistic regression was used to analyze the related influencing factors of patients’ disclosure of their diagnosis.
Results
A total of 124 pairs of patients and their family members were analyzed. Of the 124 patients, 47 (37.90%) patients knew about their cancer diagnosis and 77 (62.10%) patients did not know about their cancer diagnosis before chemotherapy. There were more patients than family members who wanted the patients to be informed about the diagnosis of terminal illness (91.9% vs 53.2%, P<0.01). Binary logistic regression analysis showed that patients with university education (odds ratio [OR], 15.322; 95% confidence interval [CI], 1.781–131.781; P<0.05), patients having equal or above average annual income (OR, 5.170; 95% CI, 1.842–14.514; P<0.01) were more likely informed about cancer diagnosis before chemotherapy. Higher anxiety level was found in diagnosis non-disclosure group (P<0.05) and no significant difference in depression score between two groups (P>0.05).
Conclusion
More than half of the patients did not know their exact diagnosis before chemotherapy in China. Educational level and economic status may be influencing factors for the disclosure of cancer diagnosis. Patients and their family members had different preferences toward diagnosis disclosure.
Keywords: cancer, diagnosis disclosure, China, patient, family member
Introduction
In China, one of the most common problems in caring for patients with cancer is the non-disclosure of diagnosis to the patients.1,2 According to the Law of the People’s Republic of China on Medical Practitioners, medical personnel should tell the truth to the patients and their families, but they are obligated to pay attention to avoid adverse consequences of telling the truth. The law imposes a legal responsibility on medical professionals for any adverse effect for patients because of the disclosure of diagnosis.3 Thus, in China when disclosing a life-threatening diagnosis such as cancer to a patient, “family consent for disclosure” approach is adopted by the physicians.4 Therefore, in China, the family members become the principal receivers of bad news, and they play a decisive role in disclosing the diagnosis to the patients. Moreover, the family prefers to hide cancer diagnosis from the patient in order to protect him or her from perceived emotional harm. The family members usually inform the physician not to disclose the diagnosis information directly to the patient. However, the cancer patients’ true preference on their diagnosis in China should be paid attention to.
In the Western world, patient autonomy and the right of self-determination are much valued by the physicians.5 Medical personnel inform patients of their cancer diagnosis and the complete details of their disease once it has been confirmed, and the patients have the right to decide whether to be treated.6 It is not the same thing in the non-Western countries.7,8 Ruhnke et al’s study found that different from American patients, Japanese did not demand the cancer diagnosis be completely disclosed.9 Patients in Saudi Arabia would prefer the family to be informed to assist them in taking treatment-related decisions.10 But in recent years, patient-individualized non-paternalistic trend is being seen in non-Western cultures, although it is an early stage.6,10 Rajasooriyar et al’s recent study found that in Sri Lanka, although patients and their family members’ views and expectations of the disclosure of diagnosis and prognosis differed, a majority of patients wanted to be told directly about their diagnosis rather than to learn of it from a relative.8 Limited studies have been conducted on cancer patients’ preference for diagnosis disclosure in China. Thus, it is necessary to know the Chinese patients’ preference regarding diagnosis disclosure in order to provide recommendations that could be given to physicians.
Previous studies have found that diagnoses were disclosed in 35.8%–50.3% of the cancer patients in China.11,12 Wang et al’s investigation found that more educated patients were most likely to be aware of their cancer diagnosis.11 Other influencing factors that could affect the patients’ disclosure of cancer diagnosis need to be investigated. In China, family member’s preference may be an important factor that affects reveling the truth to patients with cancer. A previous study showed that the family members preferred to withhold the diagnosis in order to protect cancer patients’ psychological health.13 Previous studies have reported 23.1%–66.0% of family members who preferred to withhold the cancer diagnosis from the patient.13–15 Besides Wang et al’s study which found that the educational status of patients and the age of their family members were the factors influencing the attitudes toward disclosure, limited studies evaluated the factors that influenced the family’s attitude to diagnosis disclosure.3 Thus, the purposes of this study were to investigate the disclosure incidence of cancer patients who were to carry out chemotherapy and to survey the patient’s and their family’s attitudes and related influencing factors toward cancer diagnosis disclosure.
Does disclosure of a cancer diagnosis benefit Chinese cancer patient? The answer is far from evidence-based. Although disclosure of a life-threatening diagnosis can be emotionally overwhelming for patients, studies have shown that there were many benefits of diagnosis disclosure for cancer patients such as improving pain management, reducing anxiety and depression, and better cooperation and adherence to treatment protocols.16–19 Studies in Asian countries have yielded conflicting findings because of the different cultural surroundings and different stages of the cancer.4,20,21 Fan et al’s study12 has demonstrated that patients who did not know their diagnosis exhibited better physical and emotional quality of life compared with those who had known of their diagnosis. Few studies have been done in China on the influence on patients who have knowledge about their cancer diagnosis. Thus, another aim of our study was to compare the anxiety and depression level between the disclosure and non-disclosure patients to find the influence of diagnosis disclosure in cancer patients.
Participants and methods
Participants
This is a prospective cohort study conducted in a tertiary hospital that has 123 beds for chemotherapy in Shandong Province of China. A consecutive series of patients who had been diagnosed with malignancies by pathology and their family member who was the principal caregiver were included in our study from March 2017 to December 2017. Inclusion criteria for patient eligibility included the following: 1) diagnosed with malignancy and admitted to have the first chemotherapy, 2) aged 18–80 years, 3) well-oriented to time and place and had no history of mental disorder or cognitive dysfunction. Inclusion criteria for family members included the following: 1) older than 18 years, 2) without psychiatric disease or cognitive dysfunction. The family member who was the principal caregiver was preferably the patient’s spouse, and in the situation of where spouse was not available, parents, sons, or daughters were asked to participate in the study. This study was approved by the Ethics Committee of Weifang People’s Hospital (Approval No. 2016-023-01). All the participants received a detailed explanation regarding the aim of the study. Written informed consent was obtained from every participant.
Data collection procedure
On the day of patient admission, our trained researchers had an interview with the patients and their family separately by using designed semi-structured interview forms. Because of the stigma associated with cancer in Chinese culture, it is offensive to ask about one’s cancer directly, especially when we did not know whether the patient was aware of his or her diagnosis.2 Therefore, a pre-configured interview to understand the patient and the family’s conditions is very important. To avoid giving a hint to their disease, we used terminal illness instead of cancer to those patients who were not aware of their diagnosis.
The semi-structured interview form for the patient comprises the following questions: 1) Do you know why you are coming to hospital? 2) Have you had an operation? 3) What kind of treatment have you done? 4) Are you hospitalized for further examination or treatment? 5) Do you know the exact content of the examination (treatment)? 6) Do you think the patient should be informed of his or her diagnosis directly to himself or herself instead of the family? 7) Do you have any other requirements? The semi-structured interview form for the family comprises the following: 1) How much do you know about the patient’s condition? (2) Do you think the patient now knows his or her diagnosis? 3.1) What channel does the patient know his diagnosis by? (If the answer to question 2 is yes)? 3.2) Does the patient himself or herself do not want to know or you do not want to let the patient know (if the answer of question 2 is no)? The researchers then asked the patients and the family members on demographic characteristics followed by questions related to diagnostic disclosure and their preferences (Questionnaire 1). The researchers read the description of the question to the participant and asked the participant to indicate his or her preference from a list of possible responses. Through the semi-structured interview, we can know whether the patients are aware of their exact diagnosis. Patients’ medical information was obtained by searching electronic medical records that include the primary diagnosis and the stage of cancer.
Questionnaires
Questionnaire 1 that was mentioned above consisted of questions regarding demographic characteristics: sex, age, educational level, marriage status, type of medical insurance, and questions regarding the participants’ preferences on truth disclosure. The questions on patient’s and the family’s current condition of breaking bad news and preferences were different, which mainly include: 1) current condition of cancer diagnosis disclosure (disclosure or non-disclosure); 2) the person and the appropriate person to inform the diagnosis, and the most important reason; 3) the place and the appropriate place; and 4) the time and the appropriate time to inform the diagnosis. A pilot study was conducted by using the questionnaire in 10 cancer patients and 10 family members for clarity and ease of comprehension before being used. According to previous interview, the patients were divided into diagnosis disclosure group and diagnosis non-disclosure group. Diagnosis disclosure group included patients who knew that they had a malignancy and needed chemotherapy. Diagnosis non-disclosure group included patients who did not know that they had a malignancy. The content validity of the questionnaire was 0.93, and the Cronbach’s α reliability of the total questionnaire was 0.72.
To test the patients’ psychological distress, the Chinese version of Hospital Anxiety and Depression Scale (HADS) for anxiety and depression was used in the study.22 The HADS consists of 14 items, of which seven items indicating anxiety and seven items indicating depression. The items are rated on 4-point response scales ranging from 0 to 3, which results in scale values between 0 and 21 for each scale. Three ranges were defined by the original test authors: 0–7 (non-cases of anxiety and depression), 8–10 (doubtful cases of anxiety and depression), and 11–21 (cases of anxiety and depression).
Data analysis
All the data were recorded and analyzed by SPSS version 19.0 (IBM Corporation, Armonk, NY, USA). Descriptive statistics such as frequencies, percentages, means, and standard deviations were used to describe participants’ characteristics. Chi-square test was used to evaluate the difference of enumeration data and two independent sample t-test was used to compare the difference of measurement data between the diagnosis disclosure group and non-disclosure group. Logistic regression analysis was used to examine associations between the patients’ and family members’ characteristics and actual diagnostic disclosure (aware vs unaware). The significance level was set at 0.05.
Results
Patients’ and family members’ characteristics
From March 2017 to December 2017, a total of 134 cancer patients and 134 family members were recruited, of whom 124 cancer patients and 130 family members completed the questionnaire, with effective responses rate of 91.04% and 97.01%, respectively. Ten patients and four family members chose not to participate or the questionnaire was unfinished. We analyzed the 124 pairs of patients and their family members. The mean age of the patients was 51.86±10.60 years (ranged from 27 to 73 years). The mean age of the family members was 49.30±10.81 years (ranged from 24 to 75 years). The characteristics of the participants are shown in Table 1 and 2. A total of 47 (37.90%) patients knew about their cancer diagnosis and 77 (62.10%) patients did not know about their cancer diagnosis before chemotherapy according to our interview. According to the interview, of the 47 patients who knew about their diagnosis, 43 of their family members reported the same as the patients and four thought that the patients did not know their diagnosis. Of the 77 patients who did not know about their diagnosis, 75 of their family members reported the same as the patients and two thought that they had known the diagnosis. The patients were divided into two subgroups according to the awareness of the diagnosis.
Table 1.
Characteristics of patients
| Variable | Diagnosis disclosure group (N=47), (n,%) | Diagnosis non-disclosure group (N=77), (n,%) | P-value |
|---|---|---|---|
| Gender | 0.351 | ||
| Male | 16(34.0) | 33(42.86) | |
| Female | 31(66.0) | 44(57.14) | |
| Mean age (years) | 47.98±8.64 | 54.2±11.03 | 0.001 |
| Age | 0.000 | ||
| 18–40 years | 9(19.1) | 10(13.0) | |
| 41–60 years | 38(85.9) | 39(50.6) | |
| >60 years | 0 | 28(36.4) | |
| Marriage status | 0.406 | ||
| Married | 43(91.5) | 66(85.7) | |
| Not married | 4(8.5) | 11(14.3) | |
| Education level | 0.000 | ||
| Elementary school | 1(2.1) | 18(23.4) | |
| Middle school | 17(36.2) | 35(45.4) | |
| University | 29(61.7) | 24(31.2) | |
| Type of medical insurance | 0.809 | ||
| Urban workers | 17(36.2) | 32(41.5) | |
| Urban resident | 20(42.6) | 26 (33.8) | |
| Rural resident | 9(19.1) | 17(22.1) | |
| None | 1(2.1) | 2(2.6) | |
| Annual income | 0.000 | ||
| Below average | 9(19.1) | 46(59.7) | |
| Equal or above average | 38(80.9) | 31(40.3) | |
| Cancer diagnosis | 0.822 | ||
| Breast Cancer | 12(25.5) | 20(26.0) | |
| Lung Cancer | 9(19.1) | 18(23.4) | |
| Gastrointestinal Cancer | 15(31.9) | 26(33.8) | |
| Other | 11(23.4) | 13(16.9) | |
| Cancer stage | 0.806 | ||
| II | 9(19.1) | 14(18.2) | |
| III | 20(42.6) | 29(37.7) | |
| IV | 18(38.3) | 34(44.1) | |
| Types of chemotherapy | 0.950 | ||
| Adjuvant | 15(31.9) | 26(33.8) | |
| Neoadjuvant | 5(10.6) | 9(11.7) | |
| Palliative | 27(57.4) | 42(54.5) |
Note: “Not married” included single, divorced or widowed.
Table 2.
Characteristics of family members
| Variable | Diagnosis disclosure group (N=47), (n,%) | Diagnosis non-disclosure group (N=77), (n,%) | P-value |
|---|---|---|---|
| Gender | 0.684 | ||
| Male | 28(59.6) | 43(55.8) | |
| Female | 19(40.4) | 34(44.2) | |
| Mean age | 49.45±11.02 | 49.21±10.74 | 0.905 |
| Age | 0.710 | ||
| 18–40 years | 11(23.4) | 20(26.0) | |
| 41–60 years | 29(61.7) | 42(54.5) | |
| >60 years | 7(14.9) | 15(19.5) | |
| Education Level | 0.237 | ||
| Elementary school | 3(6.4) | 13(16.9) | |
| Middle school | 28(59.6) | 40(51.9) | |
| University | 16(34.0) | 24(31.2) | |
| Relationship to patient | 0.055 | ||
| Spouse | 34(72.3) | 42(54.5) | |
| Child | 5(10.6) | 22(28.6) | |
| Other relatives | 8(17.0) | 13(16.9) |
Patients’ and family members’ preference to diagnosis disclosure
Patients’ and family members’ preferences toward diagnosis disclosure are shown in Table 3. It was found that more patients than family members wanted the patients to be told the diagnosis of terminal illness (cancer) (91.9% vs 53.2%, P<0.01; Figure 1A). The patients were more likely than family members to think that the medical staff was the appropriate person to inform the diagnosis (64.9% vs 33.8%, P<0.01; Figure 1B). The patient group was more likely to believe that the patients should be informed of the terminal illness (cancer) immediately after confirmation of diagnosis than from the member of the family (64.0% vs 26.2%, P<0.01; Figure 1C).
Table 3.
Patients’ and the family members’ preferences toward diagnosis disclosure
| Question | Diagnosis disclosure group
|
Diagnosis non-disclosure group
|
||
|---|---|---|---|---|
| Patients, n (%) | Family members, n (%) | Patients, n (%) | Family member, n (%) | |
| Did you (the patient) know the accurate diagnosis? | ||||
| Yes | 47(100) | 43(91.5) | 0 | 2(2.6) |
| No | 0 | 4(8.5) | 77(100) | 75(97.4) |
| Should the patients be told the truth of terminal illness? | ||||
| Yes | 47(100) | 40(85.1) | 67(87.0) | 25(32.5) |
| No | 0 | 7(14.9) | 10(13.0) | 52(67.5) |
| What channel did you know of your diagnosis? | ||||
| Medical staff | 10(21.3) | |||
| Family member | 30(63.8) | |||
| By myself or others | 7(14.9) | |||
| Who should disclose the terminal diagnosis to patients? | ||||
| Medical staff | 30(63.8) | 17(42.5) | 44(65.7) | 5(20.0) |
| Family member | 17(36.2) | 23(57.5) | 23(34.3) | 20(80.0) |
| When did you know your diagnosis? | ||||
| After the diagnosis confirmation | 19(40.4) | |||
| Till before this hospitalization | 28(59.6) | |||
| When do you think the terminal illness patients be told their diagnosis? | ||||
| Immediately after diagnosis confirmation | 32(68.1) | 16(40.0) | 41(61.2) | 1(4.0) |
| Gradually according to the therapy | 15(31.9) | 24(60.0) | 26(38.8) | 24(96.0) |
Figure 1.
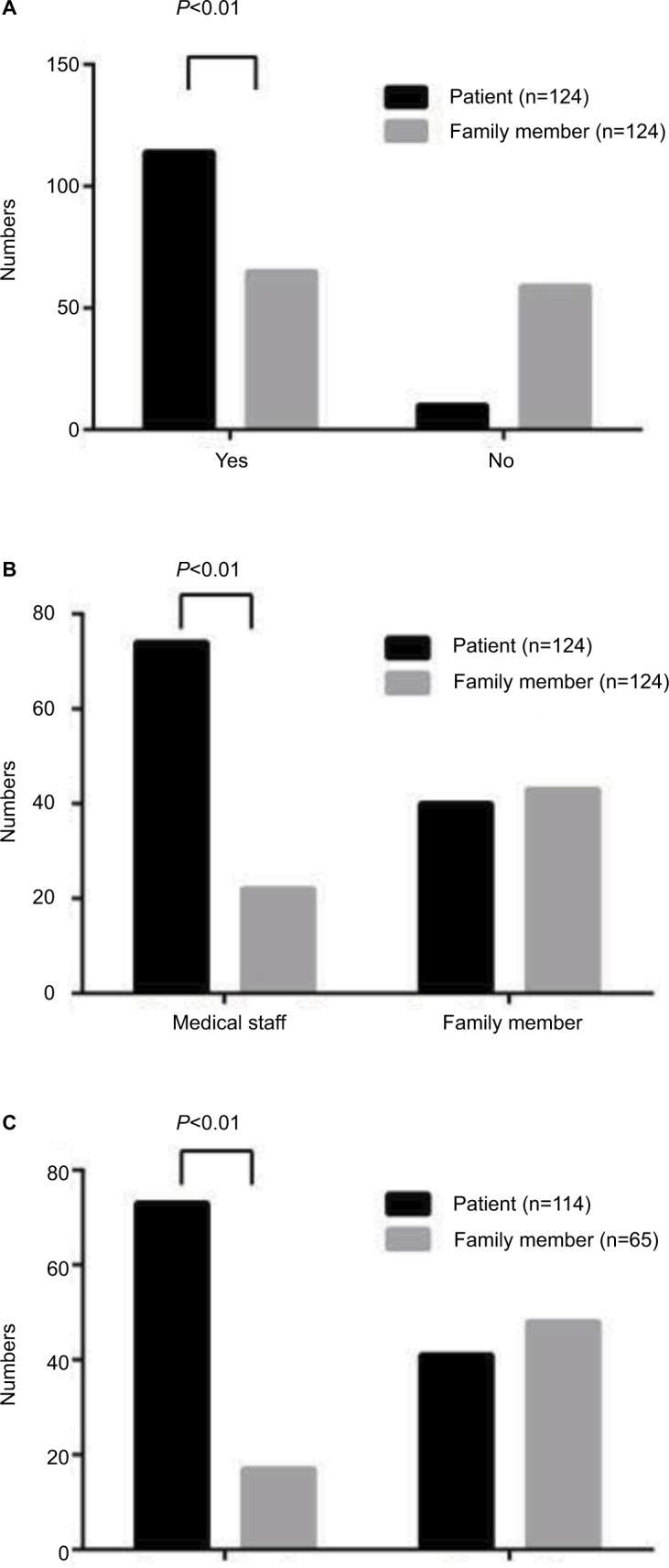
The numbers of patients and family members that answered: (A) Should the patients be told the truth of terminal illness? (B) Who should disclose the terminal diagnosis to patients? (C) When do you think the patients with terminal illness be told their diagnosis?
Influencing factors for patients’ diagnosis disclosure before chemotherapy
Univariate analysis showed that age, patient’s education level, and annual income were significantly different between diagnosis disclosure group and diagnosis non-disclosure group before chemotherapy (Tables 1 and 2). Binary logistic regression analysis showed that patients with university education (odds ratio [OR], 15.322; 95% confidence interval [CI], 1.781–131.781; P<0.05) and patients having equal or above average annual income (OR, 5.170; 95% CI, 1.842–14.514; P<0.01) were more likely to be informed about the cancer diagnosis before chemotherapy. In the binary logistic regression analysis, we excluded factors that were not associated in the univariate analysis and only included those variables that had significant associations (P<0.1) in the univariate analysis with diagnosis disclosure (ie, age, education level, annual income, and relationship to patients). Table 4 summarizes the detailed data.
Table 4.
Binary logistic regression analyses of factors influencing patients’ diagnosis disclosure before chemotherapy
| Variable | OR/Exp (B) | P-value | 95% CI |
|---|---|---|---|
| Education Level | |||
| Elementary school | Ref | ||
| Middle school | 7.300 | 0.072 | 0.838–63.622 |
| University | 15.322 | 0.013 | 1.781–131.781 |
| Annual income | |||
| Below average | Ref | ||
| Equal or above average | 5.170 | 0.002 | 1.842–14.514 |
| Relationship to patients | |||
| Spouse | Ref | ||
| Child | 0.529 | 0.348 | 0.140–2.001 |
| Other relatives | 0.854 | 0.790 | 0.267–2.733 |
| Age | 0.997 | 0.925 | 0.947–1.051 |
Abbreviations: OR, odd ratio; CI, confidence interval; Ref, reference.
Patients’ anxiety and depression between disclosure and non-disclosure group
Upon comparison of the patients’ anxiety and depression between the diagnosis disclosure group and diagnosis nondisclosure group, there was a higher anxiety level in diagnosis non-disclosure group (P<0.05) and no significant difference in depression score between two groups (P>0.05). Table 5 summarizes the detailed data.
Table 5.
Patients’ anxiety and depression level between diagnosis disclosure group and non-disclosure group
| Variable | Diagnosis disclosure group (mean ± SD) | Diagnosis non-disclosure group (mean ± SD) | P-value |
|---|---|---|---|
| Anxiety | 5.02±3.50 | 7.06±5.59 | 0.014 |
| Depression | 6.04±4.96 | 6.13±4.34 | 0.918 |
Abbreviations: SD, standard deviation.
Discussion
Our study has found that less than half (37.90%) of the Chinese patients with cancer did not know their cancer diagnosis before chemotherapy, with the trend that younger, more educated, and patients with more annual income were more likely to have knowledge of their cancer diagnosis before chemotherapy by univariate analysis. Binary logistic regression showed that patients with university education and patients having equal or above average annual income were more likely aware of the cancer diagnosis before chemotherapy. The percentage of patients who were conscious of their cancer diagnosis was generally consistent with those of previous studies of Chinese people4,11 and those done in other Asian countries.17,19,21 It should be noted that our study was conducted before the patients received chemotherapy. It is likely that more patients would have become aware of their situation when time passed by. These similar results indicated that although diagnosis disclosure was considered a patient’s right and an important practice in Western countries, it is not the same thing in the Asian countries, especially China. The reason may be the cultural difference. Cultures in Asia and the Middle Eastern countries consider cancer diagnosis non-disclosure as more humane, so as not to distress or to demoralize the individual.23 In China, although there is Tort Liability Law which emphasizes the patient’s right to learn the truth of their diagnosis, the Law on Medical Practitioners published in 2010 declares that medical personnel are obligated to pay attention to avoid adverse consequences following the truth-telling. Thus, to avoid the probable adverse consequence, a “family consent for disclosure” approach is commonly adopted. Families in China usually play a decisive role in disclosing patient’s cancer diagnosis because physicians are not encouraged to tell the truth to cancer patients directly. Although the trend to disclose the truth to patients is increasing globally, the law in China and the universal lack of medical personnel and their truth-telling skills in China make a different situation where “family consent for disclosure” approach is generally used.24 With regard to the influence factors for the diagnosis disclosure before chemotherapy, our finding was consistent with the previous studies. Jie et al’s study found that patients who were younger and more educated were more likely to become aware of their cancer diagnosis.4 Similar to our findings, Wang et al’s study also found that patients with a higher educational level were less likely to have had their cancer diagnosis concealed from them.11 The patients with college education tried on their own through the Internet or medical records to find the truth although the family tried to conceal the cancer diagnosis.11 An interesting finding in our study by the interview was that the patients of poor economic status did not want to find out the truth because they worried about the medical expenses and were more likely to give up treatment when they felt that their disease was incurable. This is similar to a previous report from China25 and a report from Korea.15
Another important finding of our study is the different preferences toward diagnosis disclosure between patients and their family members. We investigated the patients and the family members’ preferences on terminal illness diagnosis disclosure and found that 91.9% of the patient group wanted to be told the truth if they had a terminal illness, whereas only 53.2% of the family group thought the patients should be told the truth of terminal illness. Physicians should realize that there are different attitudes to diagnosis disclosure between patients and family members. Disclosure of cancer diagnosis can help the patients to conduct their own decision making for therapy methods. Our study also showed that the patients were more likely than the family members to think that the medical staff was the appropriate person to inform the diagnosis and more likely to believe that the patients should be informed of the terminal illness immediately after diagnosis confirmation than the family member group. The different preferences between the patients and family members make it necessary to conduct a first consultation to ask the patient whether he or she wants to be aware of a terminal illness such as cancer. This raises a question of how to communicate with cancer patients about the issue. Like the Western countries, the issue of how to disclose the truth is more important than whether or not to do so, which is the main problem in China.15 An interesting finding in our study is that although the patients had already known about the cancer diagnosis, four family members still thought that they did not know anything. Moreover, although the patients did not know about the cancer diagnosis, two family members thought they had known about the diagnosis. Family members want to protect patients from bad news to give them hope, but sometimes there is a lack of communication between patient and their family members. Choosing disclosure or non-disclosure according to patient’s preference instead of the family member’s preference is the best way to solve such problem.
Our study has found that there was a higher anxiety level in diagnosis non-disclosure group and no significant difference in depression score between the two groups. Qian and Hou’s study found that disclosure of diagnosis did not affect the anxiety or depression level in patients with lung cancer.26 Our study found that the diagnosis disclosure group had lower anxiety level. This ran against some reports which were conducted in India and Turkey showing that patients who received a cancer diagnosis had a significantly higher psychiatric morbidity than those left unaware of their diagnosis.27,28 The explanation of our result is as follows. First, although the patients did not know the exact diagnosis, they searched online for the symptoms associated with cancer, doubted the diagnosis which the family revealed, and became worried. Some patients tried hard to ask other patients or read their medical records. Hence, even if the doctors would withhold the truth, the patients could see through their “white lies.” The patients and the doctors can sometimes reach a tacit agreement not to reveal the truth.26 Second, the studies above were carried out more than 10 years ago, and now the long-term survival rate becomes better and better. Patients aware of the diagnosis are less likely to experience severe depression and anxiety. Third, the patients who knew their cancer diagnosis showed their control over their situation and tried hard to have coping strategies.
There were several limitations in our study. Whether diagnosis disclosure has been done was determined by the interview with the patients, and some patients did not want to talk about the theme and refused to participate in the study. Second, we did not compare preferences between the patients and family members one to one, by pair analysis. Third, we only investigated the relationship between psychological distress and patients’ situation for disclosure/non-disclosure of cancer diagnosis before chemotherapy. The patients’ psychological situation can change along with the chemotherapy, which needs a long-term follow-up and future study.
Conclusion
In summary, our study found that less than half of patients knew their exact diagnosis before chemotherapy in China. Educational level and economic status may be the influencing factors for patients’ diagnosis disclosure. Patients and their family members had different preferences toward diagnosis disclosure. There were more patients than family members who wanted the patients to be told the diagnosis of terminal illness. Patients who were informed the truth did not have more psychological distress compared with the non-disclosure group. We recommend that disclosing the truth to cancer patients should be normally carried out on the basis of productive communication strategies. We suggest that further studies on the strategies to cancer diagnosis disclosure should be done.
Acknowledgments
This research was funded by Qingdao Post-doctoral Application Research Project and Weifang Health Development Project (2017wsjs068) of China.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Tse CY, Chong A, Fok SY. Breaking bad news: a Chinese perspective. Palliat Med. 2003;17(4):339–343. doi: 10.1191/0269216303pm751oa. [DOI] [PubMed] [Google Scholar]
- 2.Jie B, Feng ZZ, Qiu Y, Zhang YQ. Association between socio-demographic factors, coping style, illness perceptions and preference for disclosure/nondisclosure of diagnosis in Chinese patients with hepatocellular carcinoma. J Health Psychol. 2017 May 1; doi: 10.1177/1359105317707258. Epub. [DOI] [PubMed] [Google Scholar]
- 3.Wang DC, Peng X, Guo CB, Su YJ. When clinicians telling the truth is de facto discouraged, what is the family’s attitude towards disclosing to a relative their cancer diagnosis? Support Care Cancer. 2013;21(4):1089–1095. doi: 10.1007/s00520-012-1629-y. [DOI] [PubMed] [Google Scholar]
- 4.Jie B, Qiu Y, Feng Z-Z, Zhu S-N. Impact of disclosure of diagnosis and patient autonomy on quality of life and illness perceptions in Chinese patients with liver cancer. Psychooncology. 2016;25(8):927–932. doi: 10.1002/pon.4036. [DOI] [PubMed] [Google Scholar]
- 5.Baile WF, Lenzi R, Parker PA, Buckman R, Cohen L. Oncologists’ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol. 2002;20(8):2189–2196. doi: 10.1200/JCO.2002.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Al Qadire M. Disclosure of cancer diagnosis: an individualized and non-paternalistic approach is preferred. J Cancer Educ. 2017 Feb 25; doi: 10.1007/s13187-017-1192-9. Epub. [DOI] [PubMed] [Google Scholar]
- 7.Wuensch A, Tang L, Goelz T, et al. Breaking bad news in China – the dilemma of patients’ autonomy and traditional norms. A first communication skills training for Chinese oncologists and caretakers. Psychooncology. 2013;22(5):1192–1195. doi: 10.1002/pon.3112. [DOI] [PubMed] [Google Scholar]
- 8.Rajasooriyar C, Kelly J, Sivakumar T, et al. Breaking bad news in ethnic settings: perspectives of patients and families in Northern Sri Lanka. J Global Oncol. 2017;3(3):250–256. doi: 10.1200/JGO.2016.005355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruhnke GW, Wilson SR, Akamatsu T, et al. Ethical decision making and patient autonomy: a comparison of physicians and patients in Japan and the United States. Chest. 2000;118(4):1172–1182. doi: 10.1378/chest.118.4.1172. [DOI] [PubMed] [Google Scholar]
- 10.Mobeireek AF, Al-Kassimi F, Al-Zahrani K, et al. Information disclosure and decision-making: the Middle East versus the Far East and the West. J Med Ethics. 2008;34(4):225–229. doi: 10.1136/jme.2006.019638. [DOI] [PubMed] [Google Scholar]
- 11.Wang DC, Guo CB, Peng X, Su YJ, Chen F. Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China. Support Care Cancer. 2011;19(8):1191–1195. doi: 10.1007/s00520-010-0937-3. [DOI] [PubMed] [Google Scholar]
- 12.Fan X, Huang H, Luo Q, Zhou J, Tan G, Yong N. Quality of life in Chinese home-based advanced cancer patients: does awareness of cancer diagnosis matter? J Palliat Med. 2011;14(10):1104–1108. doi: 10.1089/jpm.2011.0111. [DOI] [PubMed] [Google Scholar]
- 13.Jiang Y, Liu C, Li JY, et al. Different attitudes of Chinese patients and their families toward truth telling of different stages of cancer. Psychooncology. 2007;16(10):928–936. doi: 10.1002/pon.1156. [DOI] [PubMed] [Google Scholar]
- 14.Ozdogan M, Samur M, Bozcuk HS, et al. “Do not tell”: what factors affect relatives’ attitudes to honest disclosure of diagnosis to cancer patients? Support Care Cancer. 2004;12(7):497–502. doi: 10.1007/s00520-004-0633-2. [DOI] [PubMed] [Google Scholar]
- 15.Yun YH, Lee CG, Kim SY, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol. 2004;22(2):307–314. doi: 10.1200/JCO.2004.07.053. [DOI] [PubMed] [Google Scholar]
- 16.Motlagh A, Yaraei N, Mafi AR, et al. Attitude of cancer patients toward diagnosis disclosure and their preference for clinical decision-making: a national survey. Arch Iran Med. 2014;17(4):232–240. [PubMed] [Google Scholar]
- 17.Chittem M, Norman P, Harris PR. Relationships between perceived diagnostic disclosure, patient characteristics, psychological distress and illness perceptions in Indian cancer patients. Psychooncology. 2013;22(6):1375–1380. doi: 10.1002/pon.3149. [DOI] [PubMed] [Google Scholar]
- 18.Degi CL. Non-disclosure of cancer diagnosis: an examination of personal, medical, and psychosocial factors. Suppor Care Cancer. 2009;17(8):1101–1107. doi: 10.1007/s00520-008-0568-0. [DOI] [PubMed] [Google Scholar]
- 19.Montazeri A, Tavoli A, Mohagheghi MA, Roshan R, Tavoli Z. Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer. 2009(9):39. doi: 10.1186/1471-2407-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maeda Y, Hagihara A, Kobori E, Nakayama T. Psychological process from hospitalization to death among uninformed terminal liver cancer patients in Japan. BMC Palliat Care. 2006(5):6. doi: 10.1186/1472-684X-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin CC. Disclosure of the cancer diagnosis as it relates to the quality of pain management among patients with cancer pain in Taiwan. J Pain Sympt Manage. 1999;18(5):331–337. doi: 10.1016/s0885-3924(99)00091-3. [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.de Pentheny O’Kelly C, Urch C, Brown EA. The impact of culture and religion on truth telling at the end of life. Nephrol Dial Transplant. 2011;26(12):3838–3842. doi: 10.1093/ndt/gfr630. [DOI] [PubMed] [Google Scholar]
- 24.Wang SY, Chen CH, Chen YS, Huang HL. The attitude toward truth telling of cancer in Taiwan. J Psychosom Res. 2004;57(1):53–58. doi: 10.1016/S0022-3999(03)00566-X. [DOI] [PubMed] [Google Scholar]
- 25.Li J, Yuan XL, Gao XH, Yang XM, Jing P, Yu SY. Whether, when, and who to disclose bad news to patients with cancer: a survey in 150 pairs of hospitalized patients with cancer and family members in China. Psychooncology. 2012;21(7):778–784. doi: 10.1002/pon.1979. [DOI] [PubMed] [Google Scholar]
- 26.Qian H, Hou L. Psychological impact of revealing a diagnosis of lung cancer to patients in China. J Thorac Dis. 2016;8(10):2879–2884. doi: 10.21037/jtd.2016.10.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alexander PJ, Dinesh N, Vidyasagar MS. Psychiatric morbidity among cancer patients and its relationship with awareness of illness and expectations about treatment outcome. Acta Oncol. 1993;32(6):623–626. doi: 10.3109/02841869309092441. [DOI] [PubMed] [Google Scholar]
- 28.Atesci FC, Baltalarli B, Oguzhanoglu NK, Karadag F, Ozdel O, Karagoz N. Psychiatric morbidity among cancer patients and awareness of illness. Support Care Cancer. 2004;12(3):161–167. doi: 10.1007/s00520-003-0585-y. [DOI] [PubMed] [Google Scholar]


