Abstract
Purpose
To compare patient reported outcome measures (PROMs) during the first postoperative year between isolated anterior cruciate ligament (ACL) reconstruction and ACL reconstruction with concomitant meniscal intervention.
Methods
Patients who underwent primary ACL reconstruction at Capio Artro Clinic, Stockholm, Sweden, between 1st Jan 2001 and 31st Dec 2014 without concomitant injuries others than meniscal and/or cartilage lesions were included. Five groups of meniscal treatment simultaneously to ACL reconstruction were established; medial meniscal (MM) resection, MM repair, lateral meniscal (LM) resection, LM repair, and MM + LM resection. Patients treated with isolated ACL reconstruction formed a separate group. Preoperative, 6-month and 1-year Knee Injury and Osteoarthritis Outcome Score (KOOS), and Lysholm knee score and Tegner Activity scale were collected. Differences in the change over time were analyzed with an ANOVA for repeated measurements with age at surgery, gender, and cartilage injury as covariates. A univariate ANOVA was applied to analyze PROMs between groups at the final follow-up.
Results
A total of 6398 patients were included (56.8% males, mean age 28.5 ± 10.2 years). The KOOS improved across all subscales for all treatment groups. The mean change over time differed significantly between groups for the subscales symptoms (p = 0.017) and activities in daily living (ADL) (p < 0.001). Symptoms was least improved in the MM repair group, while the MM + LM resection group showed the largest improvement. For the ADL subscale, the isolated ACL reconstruction group showed the least improvement and the MM + LM resection group showed the major improvement. At 1-year follow-up, a significant difference between the groups was found for the subscale symptoms (p = 0.019), where the MM repair group reported the lowest score [mean 78.4 (95% CI 76.3–80.5)]. No significant differences were found between groups in change of the Lysholm score over time; however, at 6 months, the difference between groups was significant (p = 0.006) with the meniscal repair groups reporting the lowest scores.
Conclusion
Patients with concomitant meniscal resection are able to reach the same subjective knee function as isolated ACL reconstructions as early as 6 months postoperatively. However, patients with meniscal repair may have slightly worse subjective knee function at both 6- and 12-month follow-up. These findings could help clinicians to set realistic short-term expectations for patients undergoing ACL reconstruction with simultaneous meniscal intervention.
Level of evidence
3.
Keywords: Anterior cruciate ligament, ACL, Meniscus, Meniscal repair, Meniscal resection, Reconstruction, Surgery
Introduction
The risk for simultaneous injury to the menisci in the occurrence of an anterior cruciate ligament (ACL) injury is substantial [1, 2]. The menisci are important structures for load transmission and are fundamental for preserved knee-health. Deficiency of the menisci can result in increased knee laxity [3–5] which in turn may lead to higher stress forces on the ACL [6] and perhaps abnormal cartilage load. In a long-term perspective, patients suffering from combined ACL and meniscal tears have been shown to present with a higher prevalence of osteoarthritis (OA) compared with patients with an isolated ACL injury [7, 8]. Therefore, thorough consideration regarding appropriate treatment for the meniscus is important in order to preserve its function and prevent the development of OA.
Long-term (5–10 years) comparisons of treatment strategies for meniscal tears have concluded that meniscal resection results in a higher postoperative rate of radiographic OA compared to meniscal repair [9–12]. Although the radiographic findings of OA are not always accompanied by symptomatic OA [13, 14], a resection of the meniscus seems to result in worse patient reported outcome compared to repair at long-term follow-up [11, 12]. However, a recent study highlighted that these long-term effects of meniscal resection may not exist in the short-term [15]. At 2-year follow-up, patients who had undergone any of; medial meniscal (MM) resection, lateral meniscal (LM) resection or LM repair in addition to ACL reconstruction reported similar Knee injury and Osteoarthritis Outcome Score (KOOS) as patients receiving an isolated ACL reconstruction. In contrary to previous long-term studies, a simultaneous MM repair was shown to result in significantly lower scores. This study also revealed that all meniscal treatment groups, except the LM resection, reported significantly lower preoperative scores compared to isolated ACL reconstruction and that these differences were equalized for all treatment groups except for the MM repair group, at 2-year follow-up [15]. Knowledge about the short-term effects on subjective knee function after concurrent meniscal resection or repair in ACL reconstruction is important in clinical practice. Patients with combined meniscal injuries may present worse symptoms preoperatively, but with correct treatment and rehabilitation following surgery they have large potential to improve and “catch up” with patients of an isolated ACL injury. The purpose of this study was to compare patient reported outcome measures (PROMs) during the first postoperative year between isolated ACL reconstruction and combined ACL reconstruction and meniscal intervention in order to increase the awareness of the outcome during the time of rehabilitation. It was hypothesized that presence of meniscal injury would influence preoperative PROMs negatively; however, the short-term outcome would be comparable to patients with an isolated ACL reconstruction.
Materials and methods
This retrospective cohort study was conducted at Capio Artro Clinic, Sophiahemmet, Stockholm, Sweden. Patients aged 13 years or older who underwent primary ACL reconstruction using bone-patellar-tendon-bone (BPTB) or hamstring tendon (HT) autografts during the study period 1st Jan 2001 to 31st Dec 2014 and did not present with any concomitant injuries other than meniscal and/or cartilage lesions were considered eligible. The study period was chosen since registration of meniscal injuries in the local registry started in 2001, and, in order to get a proper 1-year follow-up, patients undergoing surgery later than 31st Dec 2014 could not be included. Patients with contralateral or revision ACL reconstruction were excluded, as well as patients with untreated meniscal injury and patients receiving more than one type of meniscal treatment such as combinations of repair and resection. However, combined MM + LM resections were included and analyzed as a separate treatment group.
Surgical technique and rehabilitation
For the ACL reconstructions performed with HT graft, the semitendinosus was primarily harvested and prepared as a triple or a quadruple graft. If the graft width was insufficient (less than 8 mm), the gracilis tendon was additionally harvested and combined with the semitendinosus graft. The graft was fixed with an Endobutton fixation device (Smith & Nephew, Andover, Mass, USA) on the femoral side and Ultrabraid (Smith & Nephew, Andover, Mass, USA) or Ethibond no. 2 sutures (Ethicon Inc, USA) tied over an AO bicortical screw with a washer on the tibial side. For patients undergoing reconstruction with BPTB graft, the central third of the patellar tendon was harvested with two bone blocks. The graft was fixed with Endobutton fixation device (Smith & Nephew, Andover, Mass, USA) on the femoral side and with an interference screw on the tibial side (Softsilk, Smith and Nephew, Andover, Mass, USA). Meniscal repair was performed with an all-inside arthroscopic technique using FasT-Fix suture anchor device (Smith and Nephew, Andover, Mass, USA) or inside-out technique in the dorsal or middle thirds of the meniscus, and with outside-in technique in the anterior third of the meniscus.
All patients were recommended the same rehabilitation protocol. In case of isolated ACL reconstruction or ACL reconstruction with simultaneous meniscus resection, full weight bearing was recommended as tolerated and the early rehabilitation phase emphasized on regained range of motion (ROM), reduction of swelling, and gait correction. A carefully progressive program with increased strengthening and proprioceptive exercises followed. Rehabilitation was restricted to closed chain exercises during the first 3 months. Patients treated with meniscal repair wore a hinged knee brace for 6 weeks. Flexion was limited from 0° to 30° the first 2 weeks, 0°–60° week 3–4, and 0°–90° week 5 and 6. Starting from the 7th week, the brace was discontinued and progressive weight bearing was allowed. Return to sports was recommended at earliest 6 months postoperatively depending on type of sport and knee function.
Outcome
Outcome measurements in this study were the Knee injury and Osteoarthritis Outcome Score (KOOS) [16, 17], the Lysholm knee score [18] and the Tegner activity scale [18, 19]. The KOOS has been validated to determine subjective outcome in patients with knee injuries and knee osteoarthritis. It is divided into five subscales—pain, symptoms, activities in daily living (ADL), function in sport and recreation, and knee-related quality of life (QoL). A score of 0 represents the worst possible outcome while 100 is the maximum score for a subscale. The Lysholm score comprises eight condition-specific domains which are summarized as a score ranging from 0 (worst) to 100 (best). The Tegner score ranges from 0 to 10, with 0 indicating severe disability and 10 indicating participation in competitive knee-demanding sports at elite level. Preoperative data were obtained for all outcomes. The Lysholm and Tegner scores were evaluated at 6 months follow-up, and the KOOS at 1-year follow-up. Only patients with available data at both the aforementioned follow-ups as well as preoperatively were included in analyzes of changes over time. For the KOOS, the number of patients with available data differed between the five subscales; hence, the study sample for each subscale was slightly different. Any missing data was addressed according to KOOS user guide 1.1 [20].
Data sources and measurement
All ACL reconstructions performed at Capio Artro Clinic, Stockholm are registered in the clinic’s local registry. The registry is divided into separate parts for the surgeon and the patient. Regarding the surgeon’s part, data are reported prospectively into the database immediately following surgery. Compliance is 100% since the system automatically requires accurate reporting of the surgical data by the surgeon to be able to proceed to the patient’s medical record. Details regarding the surgery such as graft choice, fixation methods, concomitant injuries, and all interventions and procedures to the knee are reported. Information about date of surgery, length of surgery, and any previous surgeries to the ipsilateral or contralateral knee are also recorded.
Prior to surgery, patients are asked to complete surveys including KOOS, Lysholm and Tegner, and the results are transferred into the database by hospital employees. All patients are offered a follow-up appointment with a physiotherapist 6 months after surgery during which the Lysholm and Tegner questionnaires are completed again. The KOOS questionnaire for 1-year follow-up is distributed via the Swedish national knee ligament register (SNKLR).
This study was conducted according to the WMA Declaration of Helsinki. Investigators had only access to unidentified data and the study was approved by the Regional Ethics Committee, Karolinska Institutet (Diarienumber 2016/1613-31/2).
Statistical analysis
All data were analyzed using IBM SPSS Statistics (Version 23.0, IBM Corp, Armonk, New York, USA). Tables and diagrams were generated using Microsoft Excel for Windows (Version 14.0.7, Microsoft Corp, Redmond, Washington, USA). Demographic and clinical data as well as PROMs were summarized with standard descriptive statistics, such as frequency, mean, and standard deviation. Differences between groups in baseline characteristics were analyzed. For the variable age, one-way ANOVA followed by post hoc Tukey HSD test was performed. The Chi square test was used for the variables gender and concomitant cartilage lesion. Differences in change over time were analyzed with an ANOVA for repeated measurements (Group * Time) with age at surgery, gender, and cartilage injury as covariates. In addition, an analysis of difference between groups at the final follow-up for each outcome was analyzed by applying a univariate ANOVA with age at surgery, gender, and cartilage injury as covariates. The applied covariates were chosen since several previous register studies from Scandinavia have indicated that these factors could influence PROMs after ACL reconstruction [21–24]. A significance level of 5 percent (two-tailed) was used.
Results
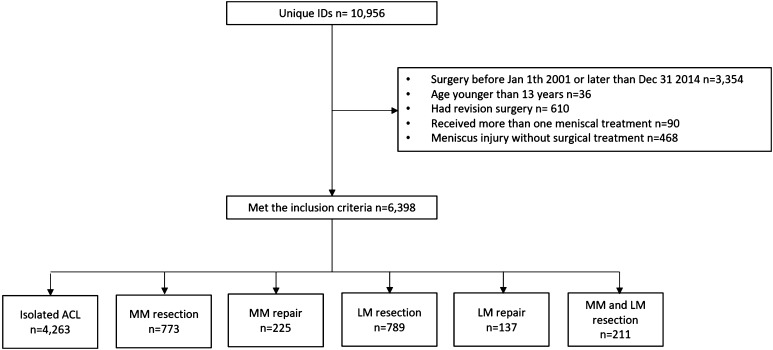
A total of 10,956 patients were reviewed for eligibility in the local database, of which 6,398 met inclusion criteria. The study population consisted of 56.8% males with a mean age of 28.5 ± 10.2 years. Six groups were generated depending on meniscal treatment; Isolated ACL reconstruction, MM resection, MM repair, LM resection, LM repair, and combined MM + LM resection (Fig. 1). In two treatment groups, the proportions of gender differed significantly (p < 0.001). The MM repair group had significantly more women (53.8%) while the combined MM + LM resection group consisted of significantly fewer women (35.1%). Further, there was a significant difference in age among the treatment groups (p < 0.001). Patients in the LM repair group were the youngest, while the oldest mean age was found for the MM + LM resection and the MM resection groups. The demographic data are presented in detail in Table 1.
Fig. 1.
Flow-chart of patient-inclusion process. ACL anterior cruciate ligament, MM medial meniscus, LM lateral meniscus
Table 1.
Demographic data for study population
| Isolated ACL | MM resection | MM repair | LM resection | LM repair | MM + LM resection | Total cohort | |
|---|---|---|---|---|---|---|---|
| Number (%) | 4263 (66.6) | 773 (12.1) | 225 (3.5) | 789 (12.3) | 137 (2.1) | 211 (3.3) | 6398 (100.0) |
| Age at surgery (mean ± SD) | 28.3 ± 10.0 | 32.5 ± 10.5 | 24.5 ± 8.9 | 27.2 ± 9.4 | 22.2 ± 9.4 | 31.8 ± 11.4 | 28.5 ± 10.2 |
| Gender, no. (%) | |||||||
| Male | 2319 (54.5) | 483 (62.5) | 104 (46.2) | 513 (65.0) | 78 (56.9) | 137 (64.9) | 3634 (56.8) |
| Female | 1944 (45.6) | 290 (37.5) | 121 (53.8) | 276 (35.0) | 59 (43.1) | 74 (35.1) | 2764 (43.2) |
| Chondral lesion, no. (%) | 612 (14.4) | 217 (28.1) | 57 (25.3) | 178 (22.6) | 32 (23.4) | 69 (32.7) | 1165 (18.2) |
| Time from injury to surgery | |||||||
| Number of patients with available data | 3474 | 633 | 214 | 680 | 134 | 169 | 5304 |
| Days (mean ± SD) | 449 ± 825 | 795 ± 1220 | 441 ± 918 | 413 ± 747 | 389 ± 829 | 738 ± 1089 | 493 ± 893 |
| Baseline Tegner activity score | |||||||
| Number of patients with available data | 3005 | 588 | 190 | 605 | 115 | 156 | 4659 |
| Tegner score, median (range) | 7 (0–10) | 7 (1–10) | 7 (1–10) | 8 (0–10) | 8 (1–10) | 7 (0–10) | 7 (0–10) |
ACL anterior cruciate ligament, MM medial meniscus, LM lateral meniscus, SD standard deviation, No number
Knee injury and osteoarthritis outcome score
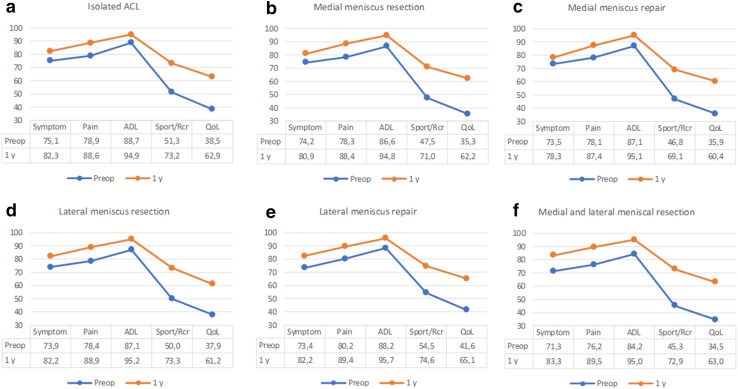
The proportion of patients with available KOOS data both preoperatively and at 1 year for each subscale was as follows: symptoms 87.4%, pain 86.3%, ADL 86.1%, sport and recreation 81.8%, QoL 84.0%. Throughout all treatment groups, the lowest preoperative KOOS scores were found in the subscales sport and recreation and QoL (Fig. 2 a–f). The KOOS improved for all treatment groups across all subscales during the 1-year follow-up (Fig. 2a–f). For the subscales symptoms and ADL, the mean change over time differed significantly between the groups (p = 0.017 and p < 0.001, respectively). Symptoms was least improved in the MM repair group while the MM + LM resection group showed the largest improvement. For the ADL, the isolated ACL reconstruction group showed the smallest improvement, whereas the MM + LM resection group showed the largest (Table 2). At 1-year follow-up, a significant difference between the groups was found only for the subscale symptoms (p = 0.019). The lowest score in symptoms was found in the MM repair group [mean 78.4 (95% CI 76.3–80.5)] while the mean score of the other groups ranged from 81.5 to 83.6 (analysis adjusted for age, gender, and cartilage).
Fig. 2.
a–f Unadjusted preoperative and 1-year Knee Injury Osteoarthritis Outcome Score displayed for each treatment group, respectively. Note that the scale on the y-axis starts at a score of 30. Preop preoperative, y year, ACL anterior cruciate ligament, ADL activities in daily living, Sport/Rcr sports and recreation, QoL quality of life
Table 2.
Mean change from preoperative score to 1-year follow-up presented for each KOOS subscale
| Isolated ACL (n = 3486–3727) | MM resection (n = 646–688) | MM repair (n = 186–196) | LM resection (n = 647–695) | LM repair (n = 104–113) | MM + LM resection (n = 162–176) | p value | |
|---|---|---|---|---|---|---|---|
| Symptom | 7.1 | 6.9 | 4.6 | 8.1 | 8.4 | 12.2 | 0.017 |
| Pain | 9.6 | 10.7 | 8.6 | 10.5 | 8.5 | 13.9 | n.s |
| ADL | 6.2 | 8.2 | 8.0 | 8.2 | 7.7 | 10.7 | < 0.001 |
| Sport/Rcr | 21.9 | 23.7 | 21.9 | 23.3 | 19.9 | 27.7 | n.s |
| QoL | 24.5 | 26.6 | 24.6 | 23.6 | 24.0 | 28.3 | n.s |
Covariates applied to the model are age, gender and cartilage injury
ACL anterior cruciate ligament, MM medial meniscus, LM lateral meniscus, ADL activities in daily living, Sport/Rcr sports and recreation, QoL quality of life, n.s non-significant
Lysholm score
In total, 83.9% of the study population had valid data on the Lysholm knee score both preoperatively and at 6 months follow-up. All treatment groups improved and no difference in improvement between the groups was observed (p = 0.113) (Table 3). In the additional analysis of solely, the Lysholm score at 6 months, the Lysholm score differed significantly between the groups at this time point (p = 0.006). The LM and the MM repair groups reported the lowest mean scores (68.2 and 71.7 points, respectively), while the other groups reported mean scores ranging from 75.2 to 76.8 points.
Table 3.
Mean Lysholm score at baseline, at 6 months postoperatively, and the mean change between these timepoints for each treatment group, respectively
| Isolated ACL n = 3595 | MM resection n = 663 | MM repair n = 179 | LM resection n = 660 | LM repair n = 107 | MM + LM resection n = 166 | p value | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Baseline | 68.2 ± 20.7 | 63.7 ± 21.6 | 65.2 ± 24.0 | 67.3 ± 20.9 | 64.8 ± 24.8 | 62.2 ± 20.9 | n.s |
| 6 months | 76.9 ± 27.2 | 74.9 ± 28.3 | 72.4 ± 29.5 | 77.3 ± 26.5 | 70.0 ± 34.3 | 74.0 ± 30.3 | |
| Changea | 8.7 | 11.4 | 6.8 | 9.8 | 4.6 | 11.9 |
ACL anterior cruciate ligament, MM medial meniscus, LM lateral meniscus, SD standard deviation, n.s non-significant
aCovariates applied to the model for change over time (preoperative to 6 months postoperatively) are age, gender, and cartilage injury
Tegner activity score
At 6 months, the Tegner activity score had decreased from the pre-injury score throughout all treatments groups. No significant differences were found between the groups (data not shown).
Discussion
The most important finding of the present study was that patients treated with meniscal repair report inferior short-term PROMs compared with meniscal resection in the setting of primary ACL reconstruction. Medial or lateral meniscal repair was shown to result in small but significantly inferior results in the Lysholm score at 6 months postoperatively, and the medial repair group also reported a significantly lower score in the KOOS subscale symptoms at 1-year follow-up. Nevertheless, patients with concomitant meniscal injuries improve considerably over the first postoperative year and are generally able to reach the same subjective knee function as an isolated ACL injury.
A similar analysis to the present study with 2-year follow-up from the Norwegian knee ligament registry showed that patients treated with MM repair in addition to ACL reconstruction had significantly lower scores in the KOOS subscales symptom and QoL compared with isolated ACL reconstruction, a finding not seen for any other meniscal treatment group [15]. This study confirms these findings, since the only difference between the groups was seen in the KOOS symptoms subscale, where the MM repair group reported significantly lower scores. The current study investigated the 1-year KOOS score, however, a recent study reported that the 1-year KOOS is equivalent to the 2-year score for patients with and without concomitant meniscal injury [25]. Thus, these findings are likely representative for the first 2 years after surgery. Furthermore, this study showed that significant differences exist with regard to the change in the first year improvement of KOOS, especially for the combined MM + LM resection group. This group was found to improve significantly more in the subscales symptoms and ADL compared to the other groups, suggesting that these patients may be more symptomatic preoperatively but are treated effectively with meniscal resection and can achieve similar KOOS in the short-term perspective as compared with other treatment groups.
The Lysholm score was evaluated 6 months postoperatively and adds knowledge with regard to the subjective outcome during rehabilitation. Although no differences were seen in change over time from the preoperative to the postoperative score between the groups, a tendency towards a slightly inferior improvement was seen in the LM repair group and, at 6-month follow-up, both meniscal repair groups reported lower scores. The postoperative management of meniscal repairs is more restraint compared with both isolated ACL reconstructions and/or meniscal resections due to concerns that weight bearing and knee flexion may cause gapping of the meniscus and generate intolerable tension and hoop stress [26, 27]. However, controversies exist since previous studies have reported similar results between restricted and accelerated rehabilitation following meniscal repair, implicating safety of a more aggressive accelerated rehab [27–30]. Biomechanical studies have shown that unrestricted ROM do not place undue stress on meniscal repairs [31] and simulated gait may actually produce compression, not gapping, of some meniscal tear types [32]. In fact, it has been suggested that functional stresses applied to the meniscus when implementing an accelerated rehabilitation protocol may promote healing of the repair [33] and instead, it has been emphasized that early unlimited ROM is important to avoid complications following a concomitant ligamentous procedure [31, 32]. The current study shows that even though a restricted and slow rehab is chosen after meniscal repair, the patients will reach a fair, but slightly lower Lysholm score compared with isolated ACL reconstruction, as early as 6 months after surgery. Based on the KOOS at 1-year follow-up, the subjective function is clinically similar among all groups, regardless of meniscal treatment.
Most importantly, this study confirms that meniscal resection is an effective procedure in the short-term. However, this finding particularly highlights the importance of further care of these patients in order to prevent OA, since long-term studies are conclusive regarding the increased risk of OA following meniscal resection [7, 9, 11, 12, 34]. A well-functioning knee in the short-term after meniscal resection increases the possibilities for the patients to participate in sports with the risk of high loads to the knee and subsequent OA. Therefore, clinicians should inform patients about their prognosis to enable this patient population to make wise future choices for preserved knee-health. Continued follow-up of this population is desirable in order to counter the development of OA at an early stage, as well as for research-related purposes and gained insight. Furthermore, preservation of the menisci is advocated whenever possible. This is particularly applied to the younger population, which is in concordance with the results of this study since the resection groups consisted of significantly older patients [35, 36].
This study is strengthened by the large study population. Moreover, all patients received the same rehabilitation recommendations and the surgery was standardized. These characteristics make this study different from previous studies on national registries which include patients operated at different clinics with different surgical techniques and rehabilitation protocols. The main limitation with this study is that although the patients were grouped according to meniscal treatment, nothing is known about the characteristics of the lesion. Neither is the proportion of meniscal removal in the resection groups known since the registry does not contain this information. The indications for choice of meniscal treatment are unknown with the inevitable consequence of possible selection bias. Furthermore, it should be emphasized that the outcome measures in this study may not be capable of discriminating subjective differences that are clinically important. The KOOS has been frequently used to study outcome after ACL reconstruction; however, differences in outcome reported by previous studies are many times less than the minimal detectable change [25, 37]. The KOOS as an outcome measure may therefore be difficult to interpret and the findings of this study should be treated with caution, keeping the intrinsic limitations associated with PROMs in mind. Nevertheless, it is important for clinicians to have knowledge of the patients’ perspective on knee function in order to individualize the rehabilitative care and to inform the patients and set realistic expectations regarding the short-term prognosis after ACL reconstruction with concomitant meniscal treatment.
Conclusion
Patients with concomitant meniscal resection are able to reach the same subjective knee function as isolated ACL reconstructions as early as 6 months postoperatively. However, patients with meniscal repair may have slightly worse subjective knee function at both 6- and 12-month follow-up. These findings could help clinicians to set realistic short-term expectations for patients undergoing ACL reconstruction with simultaneous meniscal intervention.
Acknowledgements
We thank Gunnar Edman for his contribution to the statistical analysis.
Compliance with ethical standards
Conflict of interest
Each author declares that no possible conflict of interest (financial or non-financial) exist in connection with this study.
Funding
This study received funding for study purpose from Capio research fund and Sophiahemmet research fund.
Ethical approval
The study was approved by the Regional Ethics Committee, Karolinska Institutet, Diarie number: 2016/1613-31/2.
References
- 1.Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(1):123–130. doi: 10.1016/j.arthro.2011.08.292. [DOI] [PubMed] [Google Scholar]
- 2.Sayampanathan AA, Howe BK, Bin Abd Razak HR, Chi CH, Tan AH. Epidemiology of surgically managed anterior cruciate ligament ruptures in a sports surgery practice. J Orthop Surg (Hong Kong) 2017;25(1):2309499016684289. doi: 10.1177/2309499016684289. [DOI] [PubMed] [Google Scholar]
- 3.Magnussen RA, Reinke EK, Huston LJ, Group M, Hewett TE, Spindler KP. Factors associated with high-grade Lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(6):1080–1085. doi: 10.1016/j.arthro.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, Lopomo N, Samuelsson K, Irrgang JJ. The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. 2016;44(12):3126–3131. doi: 10.1177/0363546516659649. [DOI] [PubMed] [Google Scholar]
- 5.Robb C, Kempshall P, Getgood A, Standell H, Sprowson A, Thompson P, Spalding T. Meniscal integrity predicts laxity of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3683–3690. doi: 10.1007/s00167-014-3277-x. [DOI] [PubMed] [Google Scholar]
- 6.Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29(2):226–231. doi: 10.1177/03635465010290021801. [DOI] [PubMed] [Google Scholar]
- 7.Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976. doi: 10.1007/s00167-012-2251-8. [DOI] [PubMed] [Google Scholar]
- 8.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 9.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 10.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. doi: 10.1055/s-0030-1247773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melton JT, Murray JR, Karim A, Pandit H, Wandless F, Thomas NP. Meniscal repair in anterior cruciate ligament reconstruction: a long-term outcome study. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1729–1734. doi: 10.1007/s00167-011-1501-5. [DOI] [PubMed] [Google Scholar]
- 12.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28(4):446–452. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 13.Andersson-Molina H, Karlsson H, Rockborn P. Arthroscopic partial and total meniscectomy: a long-term follow-up study with matched controls. Arthroscopy. 2002;18(2):183–189. doi: 10.1053/jars.2002.30435. [DOI] [PubMed] [Google Scholar]
- 14.Petty CA, Lubowitz JH. Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8years’ follow-up. Arthroscopy. 2011;27(3):419–424. doi: 10.1016/j.arthro.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade CM, Dornan GJ, Granan LP, LaPrade RF, Engebretsen L. Outcomes after anterior cruciate ligament reconstruction using the norwegian knee ligament registry of 4691 patients: how does meniscal repair or resection affect short-term outcomes? Am J Sports Med. 2015;43(7):1591–1597. doi: 10.1177/0363546515577364. [DOI] [PubMed] [Google Scholar]
- 16.Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports. 1998;8(6):439–448. doi: 10.1111/j.1600-0838.1998.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 17.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 18.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 19.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 20.The KOOS user guide 1.1 (2012) The Knee Osteoarthritis Outcome Score 2017
- 21.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med. 2010;38(7):1334–1342. doi: 10.1177/0363546510361218. [DOI] [PubMed] [Google Scholar]
- 22.Desai N, Bjornsson H, Samuelsson K, Karlsson J, Forssblad M. Outcomes after ACL reconstruction with focus on older patients: results from the Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):379–386. doi: 10.1007/s00167-013-2803-6. [DOI] [PubMed] [Google Scholar]
- 23.Fauno P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the danish registry of knee ligament reconstruction. Orthop J Sports Med. 2014;2(10):2325967114552405. doi: 10.1177/2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu F, Krupic F, Desai N, Westin O, Samuelsson K (2017) Increased odds of patient-reported success at 2 years after anterior cruciate ligament reconstruction in patients without cartilage lesions: a cohort study from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2017 Jun 7. 10.1007/s00167-017-4592-9 [DOI] [PMC free article] [PubMed]
- 25.Samuelsson K, Magnussen RA, Alentorn-Geli E, Krupic F, Spindler KP, Johansson C, Karlsson J (2017) Equivalent knee injury and Osteoarthritis Outcome Scores 12 and 24 month after anterior cruciate ligament reconstruction—results From the Swedish National Knee Ligament Register. Am J Sports Med. 2017 Jul;45(9):2085–2091 [DOI] [PubMed]
- 26.Cavanaugh JT, Killian SE. Rehabilitation following meniscal repair. Curr Rev Musculoskelet Med. 2012;5(1):46–58. doi: 10.1007/s12178-011-9110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Donnell K, Freedman KB, Tjoumakaris FP (2016) Rehabilitation protocols after isolated meniscal repair. Am J Sports Med:363546516667578 [DOI] [PubMed]
- 28.Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy. 1994;10(2):206–210. doi: 10.1016/S0749-8063(05)80095-7. [DOI] [PubMed] [Google Scholar]
- 29.Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy. 1997;13(4):433–437. doi: 10.1016/S0749-8063(97)90120-1. [DOI] [PubMed] [Google Scholar]
- 30.Mariani PP, Santori N, Adriani E, Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy. 1996;12(6):680–686. doi: 10.1016/S0749-8063(96)90170-X. [DOI] [PubMed] [Google Scholar]
- 31.Lin DL, Ruh SS, Jones HL, Karim A, Noble PC, McCulloch PC. Does high knee flexion cause separation of meniscal repairs? Am J Sports Med. 2013;41(9):2143–2150. doi: 10.1177/0363546513496216. [DOI] [PubMed] [Google Scholar]
- 32.McCulloch PC, Jones HL, Hamilton K, Hogen MG, Gold JE, Noble PC. Does simulated walking cause gapping of meniscal repairs? J Exp Orthop. 2016;3(1):11. doi: 10.1186/s40634-016-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dowdy PA, Miniaci A, Arnoczky SP, Fowler PJ, Boughner DR. The effect of cast immobilization on meniscal healing. An experimental study in the dog. Am J Sports Med. 1995;23(6):721–728. doi: 10.1177/036354659502300615. [DOI] [PubMed] [Google Scholar]
- 34.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 35.Monk P, Garfjeld Roberts P, Palmer AJ, Bayliss L, Mafi R, Beard D, Hopewell S, Price A. The urgent need for evidence in arthroscopic meniscal surgery. Am J Sports Med. 2017;45(4):965–973. doi: 10.1177/0363546516650180. [DOI] [PubMed] [Google Scholar]
- 36.Starke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy. 2009;25(9):1033–1044. doi: 10.1016/j.arthro.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):117–124. doi: 10.1007/s00167-008-0654-3. [DOI] [PubMed] [Google Scholar]