Abstract
Purpose
Tummy Time is preventive positioning designed to strengthen an infant’s neck and upper body muscles and minimize musculoskeletal disorders, including positional plagiocephaly. Latino parents with limited English proficiency (LEP) may experience barriers to receiving instruction on this important health-promotion strategy. Study aims included 1) adaptation and implementation of a Spanish-language version of Tummy Time; 2) evaluation of participant Tummy Time knowledge; and 3) assessment of efficacy and acceptability of the Spanish language intervention.
Design and Methods
This feasibility study involved translation of educational materials into Spanish, creation of Spanish-language print materials, and training of bilingual research assistants to deliver the educational intervention. Participants were 21 Latino expectant and current parents with self-identified LEP. Participants completed brief pre- and post-tests and performed a return demonstration.
Results
Participant knowledge of Tummy Time increased post-intervention. Program evaluation and on-site observations supported feasibility and acceptability.
Conclusions
The cultural and linguistic tailoring of targeted educational interventions is a feasible and potentially effective strategy to overcome barriers experienced by parents with limited English proficiency and may contribute to improved infant health outcomes.
Practice Implications
To be effective, health education programs must be tailored to the target population. Pediatric nurses and nurse practitioners should be aware that populations with LEP face many barriers that may inhibit their ability to participate in and understand health promotion educational activities. While translating interventions can mitigate language barriers, providers should also evaluate and address other barriers such as time constraints, transportation issues, and trust.
Introduction
In 1992, the American Academy of Pediatrics (AAP) launched the “Back to Sleep,” (now known as “Safe to Sleep”) public awareness program (Zachry & Kitzmann, 2011), aimed at decreasing the incidence of sudden infant death syndrome (SIDS). SIDS is the unexplained death of an infant less than one year of age, after other causes (e.g., infection, congenital disorders, trauma) have been ruled out through thorough investigation (Burnett & Bechtel, 2014). Although the specific causes of SIDS are unclear and most likely multifactorial, SIDS is positively correlated with a prone sleeping position among infants (Adams, Good, & DeFranco, 2009).
An effective preventive intervention to address this easily modifiable risk factor is to place newborn infants to sleep in a supine position (American Academy of Pediatrics, 2017). The drop in SIDS by over 50% in the United States over the past 25 years is evidence of the success of the widespread implementation of the Back to Sleep campaign (Adams, Ward, & Garcia, 2015). However, widespread adoption of exclusive placement of infants in a supine position has had unintended consequences for infants, including slower attainment of developmental milestones (e.g., rolling over, crawling, sitting or standing up), cognitive and organizational skills delays, eye-tracking problems, behavioral issues, and an increase in skull deformities and torticollis (Cabrera-Martos et al., 2015; Lack of ‘Tummy Time’ leads to motor delays in infants, PTs say, 2013). Skull deformities such as positional plagiocephaly can develop during pregnancy due to in utero positioning, or gradually over the first few months of life due to prolonged supine positioning. Positional plagiocephaly, (also known as deformational plagiocephaly and plagiocephaly without synostosis) is an asymmetric flattening of the occiput that occurs when the baby’s soft skull is molded due to pressure on the back of the head (Laughlin, Luerssen, & Dias, 2011). Torticollis, or a shortening of neck muscles on one side, often accompanies plagiocephaly. This shortening of the neck muscles causes the baby’s head to tilt and neck to turn in a twisted position, and is often uncomfortable or even painful. These conditions are more than cosmetic; plagiocephaly and torticollis are associated with an increased incidence in otitis media, dental malocclusion, and visual field defects (Stevens, 2012). Treatment for infants with severe cases of plagiocephaly often involves helmet therapy over a period of 8 to 18 months, with costs ranging from $2000 to $4000 (Van Wijk et al., 2014). Infants with torticollis frequently require physical therapy treatment for neck stretching exercises and positional changes (Laughlin et al., 2011).
Tummy Time
Recognizing the need for prevention of untoward consequences of the Back to Sleep infant positioning recommendations, the AAP recommended the implementation of Tummy Time, an intervention aimed at strengthening and stretching an infant’s neck and upper body muscles (American Academy of Pediatrics, 2016). Tummy Time is brief, effective, inexpensive, and suitable for most forms of plagiocephaly and torticollis, regardless of whether the conditions developed in utero or secondary to positioning after birth. Easily implemented by parents and caregivers, Tummy Time involves an adult playing and interacting with an infant placed in a prone position while awake, two to three times a day for about three to five minutes each time, with the duration of time gradually increasing as the infant gains strength (American Academy of Pediatrics, 2017). The Tummy Time program includes neck stretching exercises appropriate for torticollis (Gupta, 2014). These activities also prepare the infant for developmental advances, such as sliding on the abdomen, crawling, and lifting the head and neck (Back to Sleep, Tummy to Play, 2011).
Significance
Given that the positive impact effect of Tummy Time activities occurs primarily between birth and six months of age, early parental education is crucial (Gupta, 2014). However, many post-partum mothers do not receive complete and appropriate positioning information from health care providers, resulting in confusion and uncertainty (Koren, Reece, Kahn-D’angelo, & Medeiros, 2010). Findings from prior research indicates that even when parents and caregivers are aware of the concept of Tummy Time, they may not understand the rationale for the positioning, may not know how to correctly implement Tummy Time, or may not persist with prone placement because of the infant’s initial resistance to positioning (Zachry & Kitzmann, 2011).
Latino parents with limited English proficiency in South Carolina (SC) are a population at potential risk for not implementing Tummy Time effectively with their infants due to language barriers, cultural beliefs, poverty, challenges navigating the US healthcare system, and documentation status (Escarce & Kapur, 2006). The Latino community in SC has grown by 150% since 2000, the largest increase in any ethnic group (Brown & Lopez, 2013). As of 2010, 5% of South Carolinians identified as Latino, and of these, 47% were born outside of the US. Among foreign-born Latinos in the state, the majority (58%) were from Mexico, followed by Colombia, Cuba, Honduras, and Guatemala as the most commonly cited countries of origin (South Carolina Latino population statistics, 2010). The vast majority (72%) reported Spanish as the predominant language in the home (Demographic Profile of Latinos in South Carolina, 2014).
Compared to other racial/ethnic groups, Latinas in the US are less likely to receive early and adequate prenatal care than other ethnic groups (McDonald, Suellentrop, Paulozzi, & Morrow, 2008). In SC, barriers to care include Latinas’ limited access to health insurance and other resources such as health information, putting them at risk for poorer birth outcomes (Torres, Smithwick, Luchok, & Rodman-Rice, 2012). Young Latino parents and caregivers are more likely to employ high risk infant sleeping practices, including co-sleeping and prone positioning (Duzinski et al., 2013). Given the median age of Latinos in SC is 26 (Demographic Profile of Latinos in South Carolina, 2014), there was a clear need for a culturally and linguistically targeted and tailored Tummy Time educational intervention for Latinas in childbearing age.
Purpose
The purpose of this feasibility study was to evaluate a culturally and linguistically appropriate, Spanish language version of Tummy Time education with limited English proficient Latinos, including parents, expectant parents, and other infant caregivers, such as grandparents, extended family members, or friends. Specific aims were to 1) adapt, implement, and evaluate a Spanish language educational Tummy Time intervention; 2) assess Tummy Time knowledge and confidence levels among Latino parents and caregivers exposed to the educational intervention; and 3) assess the efficacy and acceptability of the Spanish-language Tummy Time intervention among Latinos with limited English proficiency. This study, which ran from December 2015 through February 2016, was conducted in the large and growing Latino communities in both urban and rural communities. West Columbia (Richland County, urban) and Lancaster (Lancaster County, rural), South Carolina, experienced a 120% and 266% increase in the Latino population, respectively, from 2000 to 2011 (Demographic Profile of Latinos in South Carolina, 2011). Institutional Review Board (IRB) permission was obtained from the Office of Research Compliance at the University of South Carolina.
Design and Methods
Intervention Adaptation
The Spanish-language intervention materials were adapted from culturally and linguistically adapted materials originally developed by an interdisciplinary health sciences student group. Known as the Tummy Time Project (2015), this English-language intervention was developed and implemented with a goal of educating SC parents and caregivers in the prevention of torticollis and positional plagiocephaly.
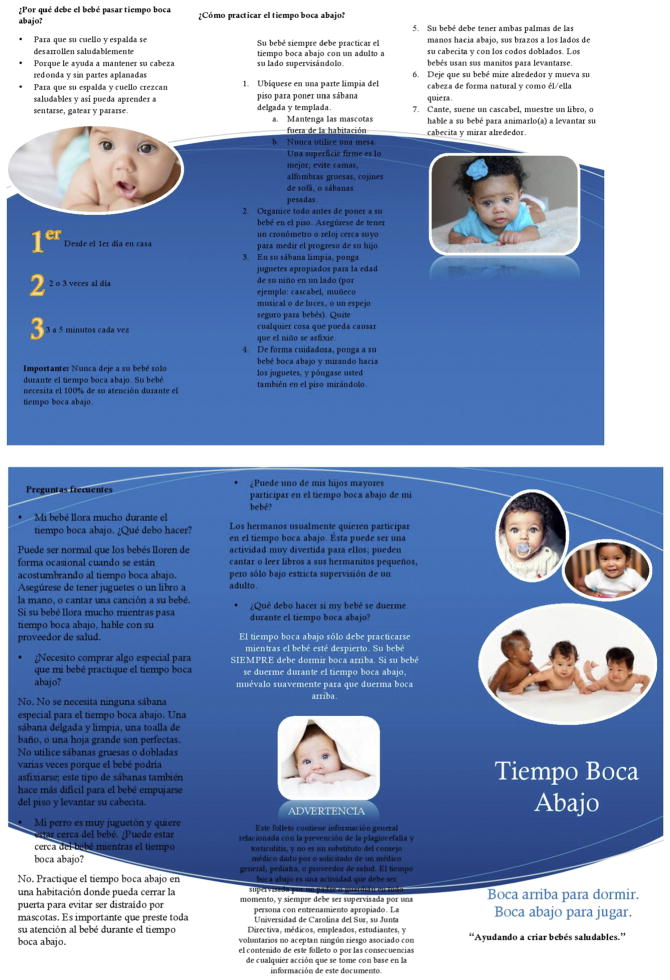
The Spanish-language intervention team began the process of adapting the materials after receiving instruction on how to teach the intervention from Tummy Time Project representatives, as well as permission to translate the print materials. First, face validity of all print materials was determined by the second author (a certified pediatric nurse practitioner). As the target population originated from Mexico, two bilingual (English-Spanish) and bicultural (Mexico-US) research assistants, along with the first author, adapted and translated into Spanish an English-language Tummy Time brochure (Fig. 1) highlighting the rationale for Tummy Time and steps. They then completed the process for a pledge card (Fig. 2) to implement the intervention that the participants could share with the infant’s primary healthcare provider. Finally, they translated into Spanish the AAP based (2016) pre- and post-intervention test, developed by Tummy Time representatives to evaluate existing knowledge and uptake of new information by English-language participants. All translated materials were subsequently back-translated and checked for accuracy by the second and third authors, both with backgrounds in medical translation.
Fig. 1.
Spanish language brochure.
Fig. 2.
Pledge card.
Participant Recruitment
Participants were recruited from a Catholic church in Lancaster, SC; a Methodist church in Columbia, SC; a clinic offering obstetric services in Columbia, SC; and through snowball referrals. Organizational officials from these facilities all agreed to participant recruitment at these sites. Participant inclusion criteria included 1) parents, expectant parents, or caregivers of infants who self-identified as Latino or Hispanic, 2) self-identified Spanish as first language; 3) self-identified limited English proficiency; and 4) residing in South Carolina. While we did collect basic demographics, no identifying information was obtained, and the surveys were identified with a numerical code rather than a name to protect their privacy. Participants received a monetary incentive in the form of a five dollar Walmart gift card after completing the post-intervention test. We conducted 14 sessions of the Tummy Time educational intervention for 21 adults. As this was a feasibility study, the goal for the sample size was at least 12, and determined by availability and willingness of participants, which was challenging in this vulnerable population (Julious, 2005). The majority (n = 20) of the participants were women, three of whom were currently pregnant; the remaining participant was a father.
Intervention
After providing written informed consent and completing the pre-intervention test, the two trained bilingual and bicultural research assistants administered the Tummy Time educational intervention, which consisted of the following components:
Explain the concept of Tummy Time, using simple, non-medical terminology.
Reinforce that parents should first discuss Tummy Time with the infant’s primary care provider, as it is not approved for all babies.
Instruct parents that Tummy Time is performed to promote healthy and strong neck and back growth; promotion of learning to sit, crawl, and stand; and keeping the head round without flat spots.
Stress the importance of assuring the child was awake and supervised by a responsible adult at all times during Tummy Time, which is reiterated by the saying, “Back to sleep; Tummy to play,” or “Boca arriba para dormir; Boca abajo para jugar” (American Academy of Pediatrics, 2016). This also addresses the fear that many parents have involving putting their baby on his/her stomach.
Review the 1, 2, 3 s: Tummy Time on day one (1) at home from the hospital; two (2) to three times a day; for three (3) to five minutes at a time.
List the steps as they are shown in the brochure (Fig. 1) while demonstrating with a life-size baby doll, thin receiving blanket, and a rattle.
Include as many of the answers to the frequently asked questions (see Fig. 1) as possible.
Encourage the participants to perform Tummy Time with the props –life-size baby doll, thin receiving blanket, and rattle – for reassurance and consolidation of the teaching.
Encourage participants to ask any questions or address any concerns they may have had, and make note of any comments or suggestions.
Administer post-intervention test.
Ensure each participant has a pledge card (Fig. 2) and brochure before they leave, so that they will have a reminder of the Tummy Time steps, and to encourage discussion with their child’s healthcare provider.
On-site Observations
Research assistants also made observations on participants’ return demonstrations of correct positioning using a baby doll, as well as informal discussions with and between participants. The research team reviewed observational notes to assess implementation fidelity and acceptability.
Data Analysis
The pre- and post-test data were analyzed using IBM SPSS (v. 23); a one-tailed Wilcoxon signed rank test was calculated to assess whether the participants demonstrated significant improvement in their knowledge regarding Tummy Time. The Wilcoxon signed rank test is a non-parametric test suitable for small sample sizes and repeated observations from the same participant.
Results
The results of the pre/post-test data indicated an increase in knowledge (z = −2.03, p = 0.04). Prior to participation, the majority of participants reported never having heard of “Tummy Time” as a branded activity, although most did have some knowledge of some of the types of activities involved. For example, most intuitively understood why their baby should do Tummy Time and what to do if their baby fell asleep during Tummy Time, that they should not do Tummy Time right after feedings, and that they should speak to a healthcare provider before performing Tummy Time (Table 1).
Table 1.
Pre- and post-intervention test results.
| Pre- and post-test questions | Pre-test correct responses n (%) |
Post-test correct responses n (%) |
|---|---|---|
| What is Tummy Time? | 17 (81%) | 15 (71%) |
| How often should my baby do Tummy Time? | 4 (19%) | 21 (100%) |
| Why should my baby do Tummy Time? | 15 (71%) | 21 (100%) |
| What do I do if my baby falls asleep during Tummy Time? | 14 (78%) | 18 (86%) |
| I should start doing Tummy Time with my infant as soon as we get home from the hospital (T or F). | 9 (43%) | 19 (90%) |
| I should do Tummy Time with my baby right after feedings (T or F). | 17 (81%) | 18 (86%) |
| I should speak to my child’s primary care provider before performing Tummy Time (T or F). | 15 (71%) | 19 (90%) |
The most common knowledge deficits were when to start and how often to implement Tummy Time (highlighted in Table 4). These questions also had the most significant increases in knowledge, which is most likely due to the emphasis placed on the “1, 2, 3 s” of Tummy Time (as described above in Intervention) stressed in the educational intervention.
On-site Observations
Following the educational intervention, all participants correctly performed the return demonstration when given the opportunity. Although initially somewhat hesitant, participants demonstrated increasing confidence as the research assistants answered participant questions and offered reassurance during the return demonstrations. Informal conversations revealed that the participants said they were thankful for this information, as it could improve the lives of their children, and expressed a readiness to perform this intervention at home. Several participants referred names of neighbors as potential participants, facilitating the study recruitment process. Participants appreciated the ease and benefits of the instruction provided.
Discussion
Limitations and Lessons Learned
This initial feasibility study has several limitations. Given the small, self-selected convenience sample, the results are not generalizable.
Challenges included conducting the recruitment and intervention in in clinic waiting rooms, due to interruptions when participants were called for their appointment. As a result, parts of the intervention had to be repeated for three participants after conclusion of their clinic visits. Although they required more time and planning, the snowball referrals were more culturally acceptable, yielded more ready participation, and resulted in smoother intervention implementation. These one-on-one encounters enhanced communication between the research assistants and participants, and were associated with increased confidence, readiness, and desire to perform Tummy Time after the instruction concluded.
The results are also limited in that the pre-/post-test was only evaluated for face validity; future work is needed to develop reliable and valid measures. As post-tests and observations were completed immediately after the intervention, it is not known if knowledge uptake and adoption of the Tummy Time intervention persisted beyond this time period. However, as this study was focused on demonstrating the feasibility of implementing this intervention, future research should ascertain persistence of practice and whether the participants shared the pledge card with their child’s healthcare provider.
Practice Implications
Health education programs should be tailored to the target population. For effective implementation of health promotion initiatives, pediatric nurses and nurse practitioners should be aware of the multiple barriers that individuals with limited English proficiency face. In addition to translating interventions, providers should also evaluate and address other barriers such as time constraints, transportation issues, and trust to mitigate linguistic and cultural barriers. Additionally, regularly offering culturally and linguistically tailored Tummy Time instruction in Latino neighborhoods, and Latino-serving primary care and well-baby clinics, churches, schools, daycares, and community centers may contribute to lower rates of torticollis, positional plagiocephaly, and developmental delays.
Conclusions
Despite these limitations, this research demonstrated potential benefit for Latino parents with limited English proficiency, who have unique barriers that can prevent them from appropriately implementing the steps with their newborns. Patient education is an important step in mitigating health disparities and requires culturally and linguistically tailored approaches to equip each patient effectively with the knowledge and confidence required to understand and perform health promotion activities. This feasibility study demonstrated that a culturally and linguistically tailored Tummy Time intervention, accompanied by the translated brochure and pledge card, enhanced parental and caregiver aware ness of the importance and ease of implementing Tummy Time. The pre-post test results and on-site observations indicated acceptability of the intervention. The results will be used to guide a future educational program to be implemented by health sciences student and clinic volunteers, and could be replicated by other interested organizations, such as local churches and Hispanic-serving clinics.
Acknowledgments
Funding
This work was supported by the University of South Carolina Honors College Senior Thesis Research Grant.
We would like to acknowledge the contributions of Dr. Lidia Navarrete in recruiting participants and offering classroom space at the Good Samaritan Clinic, and Ana Gallego for the Spanish language translation and adoption of the Tummy Time materials. We also acknowledge the Tummy Time Team, an interdisciplinary health sciences student group, who created the English language version of the brochure, pledge card, and test that we used in this study.
Footnotes
Conflicts of Interest
None to declare.
References
- Adams SM, Good MW, DeFranco GM. Sudden infant death syndrome. American Family Physician. 2009;79(10):870–874. (Retrieved 4/6/2017, from http://www.aafp.org/afp/2009/0515/p870.html) [PubMed] [Google Scholar]
- Adams SM, Ward CE, Garcia KL. Sudden infant death syndrome. American Family Physician. 2015 Jun 1;91(11):778–783. (Retrieved 4/6/2017, from http://www.aafp.org/afp/2015/0601/p778.html) [PubMed] [Google Scholar]
- American Academy of Pediatrics. Tummy time. (Retrieved 4/6/2017, from https://www.aap.org/en-us/about-the-aap/aap-press-room/aap-press-room-media-center/Pages/Tummy-Time.aspx)
- American Academy of Pediatrics. Reduce the risk of SIDS and suffocation. 2017 (Retrieved 4/6/2017, from https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Preventing-SIDS.aspx)
- Back to Sleep, Tummy to Play. 2011 (Retrieved 4/6/2017, from https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Back-to-Sleep-Tummy-to-Play.aspx)
- Brown A, Lopez MH. Mapping the Latino population, by state, county and city. 2013 (Retrieved 4/6/2017, from http://www.pewhispanic.org/2013/08/29/mapping-the-latino-population-by-state-county-and-city/)
- Burnett LB, Bechtel KA. Sudden infant death syndrome differential diagnoses. 2014 (Retrieved 4/6/2017, from http://emedicine.medscape.com/article/804412-differential)
- Cabrera-Martos I, Valenza MC, Valenza-Demet G, Benítez-Feliponi Á, Robles-Vizcaíno C, Ruíz-Extremera Á. Impact of torticollis associated with plagiocephaly on infants’ motor development. The Journal of Craniofacial Surgery. 2015;26(1):151–156. doi: 10.1097/scs.0000000000001402611. [DOI] [PubMed] [Google Scholar]
- Demographic profile of Latinos in South Carolina. 2014 (Retrieved 4/6/2017, from http://www.pewhispanic.org/states/state/sc/)
- Duzinski SV, Yuma-Guerrero PJ, Fung A, Brown JM, Wheeler T, Barczyk AN, Lawson KA. Sleep Behaviors of infants and young children: Associated demographic and acculturation characteristics among hispanic teen mothers. Journal of Trauma Nursing. 2013;20(4):189–198. doi: 10.1097/jtn.0000000000000011. [DOI] [PubMed] [Google Scholar]
- Escarce JJ, Kapur K. Hispanics and the future of America. 2006 doi: 10.17226/11539. Retrieved 4/6/2017. [DOI] [Google Scholar]
- Gupta RC. Infant torticollis. 2014 (Retrieved 4/6/2017, from http://kidshealth.org/en/parents/torticollis.html)
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics. 2005;4:287–291. [Google Scholar]
- Koren A, Reece SM, Kahn-D’angelo L, Medeiros D. Parental information and behaviors and provider practices related to tummy time and back to sleep. Journal of Pediatric Health Care. 2010;24(4):222–230. doi: 10.1016/j.pedhc.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Lack of ‘Tummy Time’ leads to motor delays in infants, PTs say. 2013 (Retrieved 4/6/2017, from http://www.apta.org/Media/Releases/Consumer/2008/8/6/)
- Laughlin J, Luerssen TG, Dias MS. Prevention and management of positional skull deformities in infants. Pediatrics. 2011;128(6):1236–1241. doi: 10.1542/peds.2011. [DOI] [PubMed] [Google Scholar]
- McDonald J, Suellentrop K, Paulozzi L, Morrow B. Reproductive health of the rapidly growing Latino population: Data from the pregnancy risk assessment monitoring system, 2002. Maternal and Child Health Journal. 2008;12:343–356. doi: 10.1007/s10995-007-0244-x. [DOI] [PubMed] [Google Scholar]
- South Carolina Latino population statistics. 2010 (Retrieved 4/6/2017, from http://www.schcc.org/resources/statistics/24-south-carolina-hispanic-populationstatistics)
- Stevens P. Beyond cosmetic concerns: Functional deficits associated with deformational plagiocephaly. 2012 (Retrieved 4/6/2017, from http://www.oandp.com/articles/2012-04_02.asp)
- Torres ME, Smithwick J, Luchok KJ, Rodman-Rice G. Reducing maternal and child health disparities among Latino immigrants in South Carolina through a tailored, culturally appropriate and participant-driven initiative. Californian Journal of Health Promotion. 2012;10(2):1–14. [Google Scholar]
- Tummy Time Project. 2015 (Retrieved 4/6/2017, from https://www.facebook.com/tummytimesc/?fref=ts)
- Van Wijk RM, Van Vlimmeren LA, Groothuis-Oudshoorn CGM, Van der Ploeg CPB, IJzerman MJ, Boere-Boonekamp MM. Helmet therapy in infants with positional skull deformation: Randomised controlled trial. The BMJ. 2014;348:g2741. doi: 10.1136/bmj.g2741723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachry AH, Kitzmann KM. Caregiver awareness of prone play recommendations. American Journal of Occupational Therapy. 2011;65(1):101–105. doi: 10.5014/ajot.2011.09100. [DOI] [PubMed] [Google Scholar]