Abstract
Background
Adolescence is a peak time for uptake of both tobacco and marijuana (dual use). This study aimed to identify clusters of lifetime tobacco and marijuana use patterns and associated risk factors, and to determine whether dual tobacco and marijuana use is uniquely associated with greater risk than use of either tobacco or marijuana alone.
Method
High school students participated in a survey during Fall 2014 (N=976; 68% Hispanic; 57% parental education < high school). Items from national youth surveys were used to measure lifetime and current use of tobacco products, marijuana, alcohol, drug use, and other risk behaviors, and literature-based surveys were used to measure psychological constructs.
Results
Latent Class Analysis identified three clusters of lifetime tobacco use patterns (no tobacco, one or two products, and more than two products), each with a correspondingly distinct profile of risk behaviors; risk escalated with use of more tobacco products. Multinomial modeling characterized personal, environmental, and behavioral correlates of dual lifetime tobacco and marijuana use, including lower parental monitoring, lower grades, higher guilt, higher lifetime alcohol and drug use, and more substance use by friends, in reference to single lifetime use of either tobacco or marijuana.
Conclusion
Broader use of tobacco (i.e., more products) was associated with numerous risk factors. Dual lifetime use of tobacco and marijuana was associated with numerous risks compared to single use of either tobacco or marijuana. Longitudinal work is needed to understand temporal relationships between risk variables to determine optimal timing for interventions to reduce harmful behaviors.
Keywords: poly tobacco use, dual tobacco and marijuana use, co-use, multi-product use, comorbid substance use, co-occurring substance use, electronic cigarettes
1. Introduction
There is growing recognition of the high co-occurrence between tobacco and marijuana use (Agrawal et al., 2012; Berg et al., 2015; Enofe et al., 2014; Pinsker et al., 2013; Schauer et al., 2016; Sutfin et al., 2012; White et al., 2015; Yates et al., 2014). Tobacco use typically precedes marijuana use (Beenstock and Rahav, 2002; Kandel and Kandel, 2015), implicating tobacco use as a risk factor for marijuana use. Nearly half of high school students report having tried a tobacco product (Arrazola et al., 2014), and adolescents with even infrequent tobacco use demonstrate symptoms of nicotine dependence (Apelberg et al., 2014; Caraballo et al., 2009). Prospective studies have demonstrated that tobacco use during adolescence is linked with regular tobacco use in adulthood (Orlando et al., 2004; Windle and Windle, 2012). Furthermore, early tobacco use is associated with nicotine dependence (Kendler et al., 2013), highlighting the need to focus tobacco prevention and control efforts in adolescence.
As the political climate for marijuana use becomes more favorable in the United States, there is concern that already high rates of marijuana use will climb (Cerda et al., 2012; Hasin et al., 2015; National Institute on Drug Abuse, 2014; Rolle et al., 2015). Recent national estimates of lifetime marijuana use among high school students is 38.6% (Kann, 2016). Deleterious effects of marijuana use among adolescents include compromised brain development and impaired cognitive ability (Camchong et al., 2016; Hanson et al., 2010). The harmful consequences of marijuana use parallel those of tobacco use in several ways, including risk for dependence and exposure to toxicants such as carbon monoxide and carcinogens from combustion (Meier and Hatsukami, 2016) and elevated respiratory symptoms (Joshi et al., 2014; Yayan and Rasche, 2016). There is evidence of an additive risk of dual tobacco and marijuana use in that dual users experience higher incidence of cannabis dependence and greater difficulty with marijuana cessation compared to users of marijuana only (Montgomery, 2015; Peters et al., 2012). Additionally, the prospect of increased toxicant exposure is greater with dual use of combustible tobacco and marijuana given the dose-response relationship between these substances and toxicant exposure (Bliss, 1935).
Previous studies have demonstrated a gradient relationship between tobacco and marijuana use among adolescents (Creamer et al., 2016; Kristjansson et al., 2015; Wills et al., 2015). High school students with no lifetime use of tobacco show the lowest incidence of risk behaviors including marijuana use. Risk is incrementally higher among users of a single tobacco product and highest among dual tobacco product users (Creamer et al., 2016; Kristjansson et al., 2015; Wills et al., 2015). While these studies are pivotal in establishing a gradient relationship between tobacco and marijuana use, they did not include a broad assessment of tobacco products. Multiple tobacco product use among adolescents is common (Arrazola et al., 2014; Neff et al., 2015), particularly in ethnic minorities (Arrazola et al., 2014; Harrell et al., 2016; Neff et al., 2015; Trinidad et al., 2017), and is associated with higher levels of nicotine dependence (Ali et al., 2016; Apelberg et al., 2014; Lanza and Vasilenko, 2015). This highlights the need for comprehensive tobacco product assessment in this population.
Better understanding the relationship between tobacco product and marijuana use, and isolating correlates of dual tobacco and marijuana use, will contribute to identification of potential intervention targets. This has proved a fruitful pathway in understanding dual use of marijuana with other substances, such as alcohol. Dual use of alcohol and marijuana has been linked to a variety of environmental and behavioral risk factors (Dir et al., 2018; Green et al., 2017; Lipperman-Kreda et al., 2017). Additive effects of dual alcohol and marijuana use have also been identified (Dubois et al., 2015). One model that has been used to explain dual use of substances is the Addiction Vulnerability Hypothesis, which maintains that the presence of biological factors predispose individuals to substance abuse (Rabin and George, 2015). Evidence for this model includes common genetic factors likely to impact multiple addictive behaviors (Agrawal et al., 2010; Hicks et al., 2011; Philibert et al., 2009).
This study aims to identify clusters of lifetime tobacco and marijuana use patterns and associated protective and risk factors, and to determine whether dual tobacco and marijuana use is uniquely associated with greater risk than use of either tobacco or marijuana alone among a diverse sample of adolescents. Our selection of variables is driven by Social Cognitive Theory and each domain (personal, environmental, and behavioral) is represented in our conceptual model (Bandura, 1986). It was hypothesized that broader tobacco use would be incrementally linked with greater risk factors, and that dual tobacco and marijuana use would be associated with higher risks than use of either product alone.
2. Method
Participants were students in grades 9–12 enrolled in Physical Education classes during Fall 2014 at a southwestern high school with a total enrollment of 2,532. According to the 2012–2013 School Accountability Report, 51% of the students are classified as socioeconomically disadvantaged (free or reduced lunch).
Students received a packet of written material that included an invitation letter describing the study, two copies of the consent/assent form, and a form to provide contact information for a raffle drawing (two $50 gift cards) and receive study results. All written invitation and consent material was provided in English and Spanish. Of the 1291 students who received an invitation to participate, 996 returned paperwork indicating parental consent and child assent (77.1% response rate).
An online survey was administered during class time on three block periods (two hour periods) days. The survey took an average of 60 minutes to complete. No student identifiers were obtained in data collection. All researchers completed online human subjects training, and the study was approved by the University’s Institutional Review Board.
2.1. Measures
Our measurement plan was guided by Social Cognitive Theory, which maintains that personal, environmental, and behavioral factors impact health behavior (Bandura, 1986). We selected measures from each domain that have been linked to adolescent behavior in previous work and aimed for representation of both protective and risk factors. Lifetime tobacco, marijuana, and other substance use is a focal point given evidence that trying a cigarette even once is linked to later smoking (Birge et al., 2017; Fidler et al., 2006) and is consistent with the broader literature that has characterized lifetime use of tobacco and marijuana (Agrawal et al., 2012).
2.1.1. Demographic items
Demographic data included age, sex, race/ethnicity, parental education, and class standing. Participants who identified as Hispanic or Latino were classified as such regardless of race. All other participants were classified as non-Hispanic White, or non-Hispanic “other” which included African American, Asian, Native American, Native Hawaiian or Pacific Islander, or other.
2.1.2. Personal factors
Depressive symptoms were measured with the 20-item CES-D (Radloff, 1977; α = 0.96 study sample), perceived stress with the ten-item Perceived Stress scale (Cohen et al., 1994) (α = 0.78 study sample); guilt measured with a ten-item scale (Marschall et al., 1994) (α = 0.93 study sample), personal responsibility measured with a 26-item scale (Connelly-Brejank et al., 2012) (α = 0.81 study sample); self-reliance measured with a ten-item scale (Greenberger et al., 1975) (α = 0.85 study sample); social commitment measured with an 11-item scale (Greenberger et al., 1975) (α = 0.82 study sample); self-esteem measured with the ten-item Rosenberg Self-Esteem scale (Rosenberg, 1979) (α = 0.83 study sample); and hope measured with the six-item Children’s Hope Scale (Snyder et al., 1997) (α = 0.94 study sample).
2.1.3. Environmental factors
Parental monitoring was measured with a six-item scale (Kopak et al., 2011) (α = 0.96 study sample). Bullying was measured with an item from the YRBS, “During the past 12 months, have you ever been electronically bullied? (Count being bullied through email, chat rooms, instant messaging, websites, or texting).” Peer use of substances was assessed with the question, “Think about your close friends, do they use any of the following?” with a list of illicit substances, alcohol, tobacco, and marijuana. A composite variable for friends who use drugs was created by counting the number of illicit substances endorsed (yes/no).
2.1.4. Behavioral factors
Tobacco use was assessed with items from the National Youth Tobacco Survey (Centers for Disease Control, 2012). Lifetime (ever tried) and current use (number of past 30 days) of the following products was assessed: cigarettes; cigars, cigarillos, or little cigars; chewing tobacco, snuff, or dip; smoking tobacco in a pipe; electronic cigarettes; hookah or waterpipe; dissolvable products; clove cigarettes; bidis; snus; roll your own cigarettes, or some other new tobacco products not listed. Marijuana use was assessed with items from the Youth Risk Behavior Survey (YRBS) (Centers for Disease Control, 2015). Lifetime use was assessed with the item, “During your life, how many times have you used marijuana?” (0 to 100 or more times). Current use was assessed with the item, “During the past 30 days, how many times did you use marijuana?” (0 to 40 or more times). Lifetime and current use of alcohol and other drugs were assessed with items from the YRBS. A comprehensive list of drugs was provided, and a composite variable for drug use was created by counting the number of other drugs used, for lifetime use, and current use, respectively. Academic performance was assessed with the item, “During the past 12 months, how would you describe your grades in school?” Response options ranged from mostly A’s to mostly F’s. Participants were also asked to report their current GPA. These two academic performance items were strongly correlated (r=0.79), and given less missing data from the question about grades in school, this item was used in analyses. A history of legal issues was assessed with the question, “Have you ever been arrested?” Riding in a car with someone who had been drinking alcohol was measured with an item from the YRBS (past 30 days).
2.2. Analyses
To investigate a gradient relationship between the full spectrum of lifetime tobacco products and marijuana use and other risk behaviors, we used Latent Class Analysis (LCA) in Mplus V5.21 to identify classes or clusters of students who differ distinctively regarding history of tobacco product use (Hagenaars and McCutcheon, 2002; Muthén and Muthén, 1998). We used students’ responses to a range of behavioral factors to reveal meaningful clusters of students who share common and distinctive patterns or profiles based on their tobacco product use. We used multinomial modeling to characterize the personal, environmental, personal, and behavioral correlates of dual tobacco and marijuana lifetime use (Tabachnick and Fidell, 2007).
3. Results
Data were screened for outliers and missing data. Responses from 20 surveys were un-usable due to issues such as profanity in responses; surveys from 40 participants contained too much missing tobacco product use data to be reliably analyzed. The final analytic sample consisted of the 936 students with valid tobacco product use data. With the exception of academic performance (grades) and history of being cyberbullied, there were less than 8% data missing across our predictor variables.
3.1. Participant characteristics
Students ranged in age from 13 through 19 (M = 15.37, SD = 1.10) years, and approximately one third of the sample were freshmen (32%), 27% were sophomores, 27% were juniors, and 11% were seniors. The sample was 60% female, and the majority of the sample (68%) identified as Hispanic, 16% as non-Hispanic White, and 16% or non-Hispanic “other” which included African American, Asian, Native American, Native Hawaiian or Pacific Islander, or other. Parents’ education was quantified as the highest level of education for whomever (either mother or father) data were reported; 57% of participants came from homes with the highest education attained by a parent was a high school diploma or GED or less.
3.2. Tobacco use
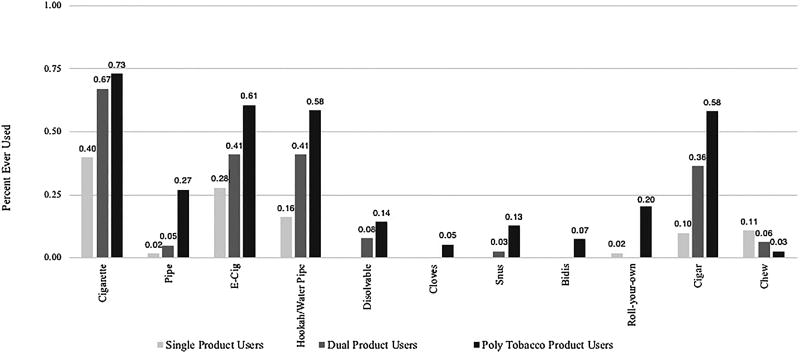
Rates of lifetime tobacco use were as follows: 60% never user of any product, 13% ever user of one product (single use), 9% ever user of two products (dual use), and 18% ever user of more than two products (poly use). The most frequently used products were cigarettes, electronic cigarettes, hookah/water pipe, chew/snuff/dip, and cigars/little cigars/cigarillos. All other single use of products was 1.5% or less (see Figure 1). Descriptive and cluster analyses revealed no dominant clusters of tobacco product use. The most frequent combinations of multiple products used included cigarettes, electronic cigarettes, hookah/water pipe, and cigars, and cigarettes, electronic cigarettes, and hookah/water pipe.
Figure 1.
Rates of tobacco product use across single, dual, and poly product users
3.3 Patterns of tobacco product use
We used latent class analyses in Mplus v5.1 to identify classes or clusters of lifetime tobacco use patterns and associated risk factors. Our goal was to identify behaviorally meaningful groups of students based on their history of tobacco product use, rather than to arbitrarily divide or combine students based on number of products used. We compared the model fit of a single class model (baseline or null hypothesis), and two, and three class models all with age as a covariate. We compared the Bayesian Information Criteria (BIC) and Akaike Information Criteria (AIC) of the three models and compared the fit of the two and three cluster models with the Vuong-Lo-Mendell-Rubin test and concluded that the three-class or cluster model was the best statistical fit to the data and the most descriptive model. We labeled the clusters by their predominant pattern of tobacco use history. For each student, Mplus estimates the probability of belonging to each of the three clusters of tobacco use and then categorizes each student into the single most likely or predominant cluster. Sixty percent of the students in our sample had no history of tobacco use and were categorized in the first cluster. The second cluster combined the students who had used one or two different tobacco products. The third cluster comprised poly users, students who had used more than two tobacco products (see Table 1). The number of tobacco products used by the poly users ranged from three to nine; the majority of poly users had used either three tobacco (35%) or four products (30%). We examined both lifetime and current (last 30 days) marijuana use across students in the three clusters to examine the gradient relationship between tobacco use behaviors and marijuana and other drug use and associated risky behaviors.
Table 1.
Latent Class Analysis Identifying Tobacco Use Clusters of Associated Risk Behaviors.
| Sample (N = 929) |
Cluster 1 (No Tobacco Products) 57% n = 528 |
Cluster 2 (One or Two Tobacco Products) 18% n = 167 |
Cluster 3 (Poly Tobacco Products) 25% n = 234 |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Lifetime | Current | Lifetime | Current | Lifetime | Current | Lifetime | Current | |
| Lifetime Tobacco | ||||||||
| No Tobacco | 60% | 1.00 | 0.00 | 0.12 | ||||
| One Tobacco Product | 13% | 0.00 | 0.65 | 0.08 | ||||
| Two Tobacco Products | 9% | 0.00 | 0.24 | 0.18 | ||||
| Poly Tobacco | 18% | 0.00 | 0.10 | 0.63 | ||||
| Marijuana and Other Drugs | ||||||||
| Marijuana | 34% | 17% | 0.07 | 0.02 | 0.36 | 0.14 | 0.95 | 0.65 |
| Alcohol - | 49% | 22% | 0.27 | 0.06 | 0.54 | 0.19 | 0.95 | 0.69 |
| Drugs – | 17% | 8% | 0.02 | 0.01 | 0.11 | 0.03 | 0.55 | 0.34 |
| Friends who use | 50% | 0.31 | 0.50 | 0.92 | ||||
| Marijuana | ||||||||
| Friends who use drugs | 24% | 0.11 | 0.14 | 0.60 | ||||
| Behaviors | ||||||||
| Been Cyberbullied | 9% | 0.07 | 0.06 | 0.17 | ||||
| Ridden in car with drunk driver | 16% | 0.09 | 0.14 | 0.32 | ||||
| Arrested - Lifetime | 8% | 0.02 | 0.03 | 0.26 | ||||
| Grades | ||||||||
| Mostly As and Bs | 60% | 0.71 | 0.56 | 0.39 | ||||
| Mostly Cs | 27% | 0.23 | 0.25 | 0.37 | ||||
| Mostly Ds and Fs | 13% | 0.07 | 0.19 | 0.23 | ||||
Notes: % denotes percentage of the total non-missing sample responding “yes” to the corresponding question. Decimals under each cluster denote the probability of a student in given cluster responding “yes” to the question. Age was used as a covaiate. Bolded percentages represent current marijuana, alcohol, and other drug use.
3.4. Patterns of tobacco and marijuana co-use
There was a clear gradient pattern of increased likelihood of both lifetime and current marijuana use across the three clusters of tobacco product users. The profile of students who had never used tobacco products was qualitativley different than those who had used one or two products, and those who had used more than two products. The profiles of one and two product users were indistinguishable from each other. While 34% percent of the students in our sample had ever used marijuana (17% in the past 30 days), very few students who do not use tobacco products use marijuana. Those students who had never used tobacco products had a probability of .07 of ever using marijuana and a probability of .02 of current marijuana use. The students in the one or two tobacco product cluster were more representative of the sample overall, having a probability of .36 of lifetime marijuana use and .14 of current use. The probability of both lifetime and current marijuana use jumps substantially in the poly tobacco use cluster where students have a probability of .95 and .65 for lifetime and current marijuana use respectively.
We used current and lifetime tobacco and marijuana use as our indicators of use rather than frequency of use given the low overall frequency of tobacco and marijuana use in our sample. For example, 73% of the students who had ever used a tobacco product had smoked less than five cigarettes in their lifetime. Sixty-five percent of the marijuana smokers in our sample had smoked it just once. Despite the fact that the majority of our ever tobacco and marijuana users do so infrequently, three distinct profiles of drug, alcohol, and risky behaviors emerged as the number of tobacco products used increased. Additionally, even a single use of cigarettes is a robust predictor of subsequent smoking (Birge et al., 2017; Fidler et al., 2006).
3.5. Incremental link between tobacco product use and other risk behaviors
Distinct profiles of drug and alcohol use, and risky behaviors emerged across these three clusters of tobacco product use. The first column in Table 1 indicates the rate of each behavior or attribute across the full sample. For example, 49% of the students in our sample had consumed alcohol during their lifetime, whereas only 16% had ridden in a car with a drunk driver in the past year. The numbers in the three cluster columns denote the probability of a student from that particular cluster engaging in each of the behaviors. For example, a student in the no tobacco cluster has a .27 probability of having ever used alcohol, compared with a student in the one or two tobacco product cluster who has a .54 probability of alcohol use. The probability of alcohol use jumps to .95 for students in the poly-use cluster. The bolded percentages represent current marijuana, alcohol, and other drug use.
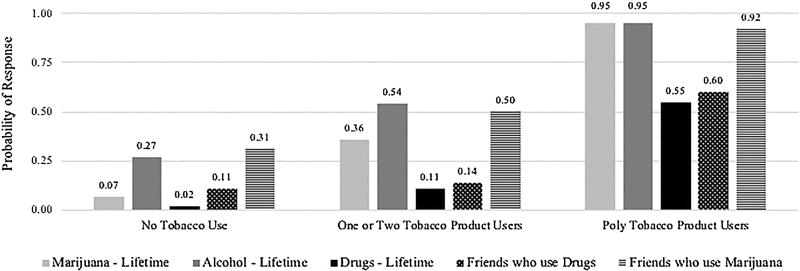
Table 1 and Figure 2 illustrate the increase in the probability of lifetime marijuana and other drug use associated with the incremental use of tobacco products. A gradient pattern similar to the one observed for marijuana use was observed for alcohol and other drugs, with never-tobacco product users displaying the lowest risk, single and dual tobacco product users showing incrementally higher risk, and poly tobacco users displaying the highest risk. For example, the students in the never used tobacco cluster were unlikely to have ever used alcohol, recreational drugs, or have friends who used drugs (probabilities = .27, .02, and .11 respectively). Contrast this to the students in the poly tobacco product use cluster, who almost certainly had used alcohol, likely had used recreational drugs, and had friends who used drugs (probability = .95, .55, and .60 respectively).
Figure 2.
Profiles of drug and alcohol use across three tobacco use clusters
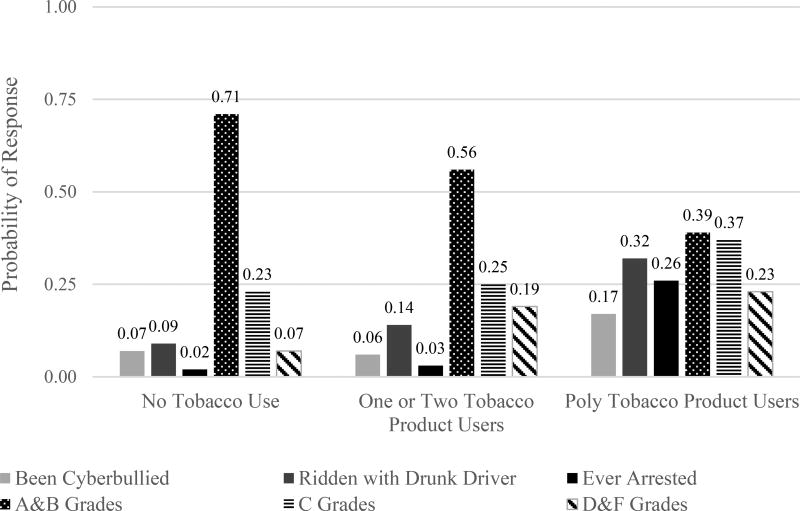
Figure 3 illustrates that behavioral risk variables demonstrated the same gradient pattern of results. Students who had never used tobacco products were the most likely to be doing well academically and earning As and Bs, whereas those in the poly user cluster were the mostly likely to be earning Ds and Fs. While the overall rates of being cyberbullied, riding in a car with a drunk driver, and ever being arrested were very low in our sample, poly tobacco users were the most likely to engage in these risky behaviors.
Figure 3.
Profiles of behavioral risk factors across three tobacco use clusters
Whereas some research reveals demographic trends in patterns of tobacco and marijuana use (Bombard et al., 2009; Ramo, et al., 2013; White et al., 2015), we found no significant differences in the students’ representation in each cluster by their demographics. This held true regardless of using age as a covariate. Male students were not over or underrepresented in any of the clusters, χ2 (2) = 0.03, p = .86. Similarly, students were represented equally across the clusters regardless of the highest education of their parents χ2 (8) = 11.18, p = .19 or their ethnicity χ2 (4) = 6.39, p = .17.
3.6. Correlates of tobacco and marijuana dual use
Latent class analysis revealed a clear gradient relationship between lifetime tobacco product and marijuana use with meaningful clusters of students based on no, one or two, and poly tobacco product use. Poly tobacco product users were almost certain to have used marijuana (.95), users of one or two tobacco products had a probability of .36 of marijuana use, and students who had never used tobacco had a negligible chance (.07) of having used or currently using marijuana.
We conducted three independent multinomial regression analyses to identify the link between the behavioral, environmental, and personal risk factors and tobacco and marijuana co-use. We classified our sample into three groups by lifetime tobacco and marijuana use: no tobacco or marijuana use (53%), either tobacco or marijuana use (19%), or both tobacco and marijuana use (28%). We used the students in the either tobacco or marijuana group as the reference group for our analyses to differentiate the impact of predictor variables on the relative odds of never using tobacco or marijuana (no use) compared with using either tobacco or marijuana (single use), and the relative odds of being a co-user versus a tobacco or marijuana user. The odds ratio for each variable indicates how the risk of the outcome (e.g., not drinking) falling in the comparison group (lifetime user of ether tobacco or marijuana) compares to the risk of not drinking falling in one referent group (no tobacco or marijuana use) or the other (tobacco and marijuana use), to changes with the variable in question. A significant odds ratio greater than one means that the risk of the outcome being in the comparison group relative to the risk of the outcome being in the reference group is greater as the variable increases. In other words, the comparison outcome is more likely. A significant odds ratio of less than one indicates that the risk of the outcome falling in the comparison group relative to the risk of the outcome falling in the reference group decreases as the variable increases. In our case the odds ratios of the binary variables (e.g., lifetime alcohol use; yes/no) indicate the relative odds of not engaging in that behavior.
3.7. Behavioral correlates
Behavioral variables accounted for the largest amount of variance in tobacco and marijuana use and co-use. No history of drug use or drinking and not getting low grades (mainly Ds and Fs) was associated with both higher odds of using no tobacco products or marijuana, and lower odds of dual tobacco and marijuana use. Specifically, the odds of never using drugs is almost six times higher for students who have never used tobacco or marijuana than for those who have used tobacco or marijuana or both. Similarly, the odds of never having consumed alcohol is four times higher for students who have never used tobacco or marijuana than for those who have used either tobacco or marijuana. The odds of abstaining from drugs or alcohol is significantly lower for students who have used both tobacco or marijuana compared with those who have used either tobacco or marijuana., but not both (see Table 2 for coefficients).
Table 2.
Multinomial Regression Equation Predicting Tobacco and Marijuana Co-Use from Behavioral Variables.
| Either Tobacco or Marijuana (Lifetime) Use vs. |
OR | p | 95% CI | |
|---|---|---|---|---|
| Behavioral | ||||
| No Drug Use | No Use | 5.76 | 0.00 | [2.20, 15.11] |
| Co-Use | 0.19 | 0.00 | [0.10, 0.36] | |
| No Alcohol Use | No Use | 4.05 | 0.00 | [2.67, 6.16] |
| Co-Use | 0.26 | 0.00 | [0.14, 0.46] | |
| Never ridden in car with drunk driver | No Use | 0.65 | 0.22 | [0.33, 1.29] |
| Co-Use | 0.45 | 0.02 | [0.23, 0.90] | |
| Never Arrested | No Use | 1.93 | 0.22 | [0.68, 5.48] |
| Co-Use | 0.45 | 0.08 | [0.19, 1.09] | |
| Grades: Mostly As and Bs | Reference Group | |||
| Grades: Mostly Cs | No Use | 0.77 | 0.28 | [0.48, 1.24] |
| Co-Use | 1.09 | 0.77 | [0.63, 1.89] | |
| Grades: Mostly Ds and Fs | No Use | 0.32 | 0.00 | [0.16, 0.61] |
| Co-Use | 2.36 | 0.01 | [1.22, 4.57] |
Notes: Psuedo R2 = .496, N = 936
Comparison group = Users of either tobacco or marijuana - but not both. Age was used as a covaiate.
3.8. Environmental correlates
Parental monitoring, not having friends who used marijuana, and never having been cyberbullied all resulted in significantly greater odds of never using tobacco or marijuana, compared with using one or the other but not both. Parental monitoring, not having friends who used marijuana, and not having friends who used drugs decreased the odds of using both tobacco and marijuana. These effects were smaller than the effects of the behavioral variables (see Table 3).
Table 3.
Multinomial Regression Equation Predicting Tobacco and Marijuana Co-Use from Environmental Variables.
| Either Tobacco or Marijuana (Lifetime) Use vs. |
OR | p | 95% CI | |
|---|---|---|---|---|
| Environmental | ||||
| Parental Monitoring | No-Use | 1.09 | 0.01 | [1.03, 1.15] |
| Co-Use | 0.90 | 0.00 | [0.85, 0.96] | |
| No friends who use drugs | No Use | 0.83 | 0.52 | [0.47, 1.47] |
| Co-Use | 0.43 | 0.00 | [0.25, 0.74] | |
| No friends who use marijuana | No Use | 2.77 | 0.00 | [1.82, 4.24] |
| Co-Use | 0.30 | 0.00 | [0.17, 0.52] | |
| Never been cyberbullied | No Use | 1.83 | 0.07 | [0.94, 3.57] |
| Co-Use | 0.96 | 0.91 | [0.48, 1.92] |
Notes: Psuedo R2 = .360, N = 936
Comparison group = Users of either tobacco or marijuana - but not both. Age was used as a covaiate.
Personal variables were the most weakly associated with patterns of tobacco and marijuana use. Lower levels of depression, higher social commitment, and lower perceived stress increased the odds of not using either tobacco or marijuana compared with using one or the other. Guilt increased the odds of using both tobacco and marijuana compared with using one or the other (see Table 4).
Table 4.
Multinomial Regression Equation Predicting Tobacco and Marijuana Co-Use from Personal Variables.
| Either Tobacco or Marijuana (Lifetime) Use vs. |
OR | p | 95% CI | |
|---|---|---|---|---|
| Personal | ||||
| Depression CESD- R | No Use | 0.82 | 0.05 | [0.68, 0.10] |
| Co-Use | 1.00 | 0.95 | [0.98, 1.02] | |
| Self-Reliance | No Use | 0.97 | 0.12 | [0.93, 1.00] |
| Co-Use | 0.98 | 0.38 | [0.94, 1.03] | |
| Social Commitment | No Use | 1.03 | 0.08 | [1.00, 1.07] |
| Co-Use | 0.99 | 0.53 | [0.95, 1.03] | |
| Self-Esteem | No Use | 1.00 | 0.97 | [0.95, 1.05] |
| Co-Use | 0.98 | 0.53 | [0.92, 1.04] | |
| Hope | No Use | 1.01 | 0.41 | [0.98, 1.05] |
| Co-Use | 0.99 | 0.72 | [0.96, 1.03] | |
| Guilt | No Use | 1.02 | 0.19 | [0.99, 1.06] |
| Co-Use | 1.05 | 0.00 | [1.02, 1.06] | |
| Perceived Stress | No Use | 0.98 | 0.03 | [0.97, 1.06] |
| Co-Use | 1.01 | 0.66 | [0.96, 1.06] | |
| Personal Responsibility | No Use | 1.01 | 0.18 | [0.99, 1.04] |
| Co-Use | 0.99 | 0.25 | [0.96, 1.01] |
Notes: Psuedo R2 = .153, N = 936
Comparison group = Users of either tobacco or marijuana - but not both. Age was used as a covaiate.
We also analyzed the behavioral, environmental, and personal variables in a single model (again using age as a covariate) to assess their unique contributions to predicting tobacco and marijuana use (see Table 5). The behavioral variables never drinking, never taken drugs, and not having friends who use marijuana emerged as the strongest predictors of both no use and co-use groups. Guilt was the only significant personal variable, increasing the odds of co-use compared with single product use.
Table 5.
Multinomial Regression Predicting Tobacco and Marijuana Co-use from Behavioral, Environmental, and Personal Variables.
| Either Tobacco or Marijuana (Lifetime) Use vs. |
OR | p | 95% CI | |
|---|---|---|---|---|
| Behavioral | ||||
| No Drug Use | No Use | 4.99 | .002 | [1.81, 13.67] |
| Co-Use | 0.26 | .001. | [0.13, 0.53] | |
| No Alcohol Use | No Use | 3.42 | .001 | [2.07, 5.63] |
| Co-Use | 0.38 | .005 | [0.19, 0.74] | |
| Never ridden in car with drunk driver | No Use | 0.68 | .317 | [0.32, 1.44] |
| Co-Use | 0.47 | .050 | [0.22, 1.00] | |
| Never Arrested | No Use | 2.01 | .243 | [0.61, 5.79] |
| Co-Use | 0.51 | .165 | [0.19, 1.33] | |
| Grades: Mostly As and Bs | Reference Group | |||
| Grades: Mostly Cs | No Use | 0.82 | .492 | [0.46, 1.47] |
| Co-Use | 1.04 | .914 | [0.53, 2.03] | |
| Grades: Mostly Ds and Fs | No Use | 0.24 | .001 | [0.11, 0.53] |
| Co-Use | 1.82 | .157 | [0.79, 4.17] | |
| Environmental | ||||
| Parental Monitoring | No-Use | 1.03 | .387 | [0.99, 1.12] |
| Co-Use | 0.93 | .083 | [0.85, 1.01] | |
| Friends who use drugs | No Use | 0.69 | .301 | [0.34, 1.39] |
| Co-Use | 0.55 | .078 | [0.28, 1.07] | |
| Friends who use Marijuana | No Use | 2.71 | .001 | [1.43, 3.83] |
| Co-Use | 0.43 | .012 | [0.22, 0.83] | |
| Been Cyberbullied | No Use | 2.17 | .068 | [0.96, 4.94] |
| Co-Use | 1.33 | .516 | [0.57, 3.12] | |
| Personal | ||||
| Depression CESD- R | No Use | 0.98 | .083 | [0.97, 1.00] |
| Co-Use | 0.99 | .404 | [0.969, 1.01] | |
| Self-Reliance | No Use | 0.98 | .501 | [0.94, 1.02] |
| Co-Use | 0.97 | .225 | [0.91, 1.02] | |
| Social Commitment | No Use | 1.04 | .053 | [1.00, 1.08] |
| Co-Use | 1.03 | .325 | [0.98, 1.08] | |
| Self-Esteem | No Use | 1.01 | .798 | [0.95, 1.07] |
| Co-Use | 1.04 | .350 | [0.96, 1.12] | |
| Hope | No Use | 1.01 | .508 | [0.97, 1.05] |
| Co-Use | 1.01 | .636 | [0.86, 1.06 | |
| Guilt | No Use | 1.02 | .232 | [0.99, 1.07] |
| Co-Use | 1.05 | .021 | [1.01, 1.10] | |
| Perceived Stress | No Use | 1.04 | .102 | [0.99, 1.10] |
| Co-Use | 0.99 | .629 | [0.93, 1.05] | |
| Personal Responsibility | No Use | 0.99 | .561 | [0.97, 1.02] |
| Co-Use | 1.00 | .800 | [0.97, 1.04] |
Notes:
Psuedo R2 = .576, N = 936
Comparison group = Users of either tobacco or marijuana - but not both. Age was used as a covariate.
4. Discussion
Three clusters of high school students’ lifetime tobacco use patterns emerged, each with a correspondingly distinct profile of risk behaviors demonstrating a gradient relationship. The probability of lifetime substance use and other behavioral risk factors increased with each tobacco use pattern. Latent class analysis of a comprehensive range of tobacco products revealed a novel framework given that single and dual tobacco product users clustered into one group and poly-tobacco users into another. Most previous studies have distinguished single product users from dual or poly users combined (Creamer et al., 2016; L. Neff et al., 2015; Osibogun et al., 2017; Pacek et al., 2016; Schauer et al., 2016; Wills et al., 2015). The finding that single and dual tobacco product users were indistinguishable and poly tobacco users were in a class of their own may reflect the wide variety of tobacco products currently available. Additionally, dual tobacco and marijuana use was linked to multiple personal, environmental, and behavioral risk factors in comparison to single use of either product; in turn, never users of either tobacco or marijuana displayed lower risk and greater protective factors compared to single users of either tobacco or marijuana. Behavioral factors were the most robust correlates across Social Cognitive Theory domains.
Findings from this study suggest that broader use of tobacco (i.e., more products) is associated with numerous risk factors. This extends recent work on the link between single use of new/emerging products such as electronic cigarettes among young adults with risky behaviors including other substance use (Cohn et al., 2015; Lessard et al., 2014; Saddleson et al., 2015) and psychosocial risk indicators including sensation seeking and positive urgency components of impulsivity (Doran and Trim, 2015). Our findings also complement existing research finding that dual cigarette and electronic cigarette use (Kristjansson et al., 2015; Wills et al., 2015) as well as use of multiple products including cigarettes, pipes, cigars, chewing tobacco, and/or bidis is associated with increased risk behavior (Bombard et al., 2009).
Our findings extend the literature to a full range of tobacco products, which is important due to the rapidly changing tobacco industry and aggressive marketing toward youth (USDHHS, 2012). Our results largely parallel those from a large, representative adolescent survey conducted during the same time period as the present study regarding relative frequency of tobacco product use (Kasza et al., 2017). Cigarettes were used most frequently, followed by e-cigarettes, hookah, and cigars/little cigars/cigarillos. Our study sample varied slightly from the first wave of PATH with chew/snuff/dip being reported more frequently among single product users. This may reflect a regional difference given a large military presence in the study area (Peterson et al., 2007), or may be an artifact of a smaller sample size. Given increased risks associated with multiple tobacco product use, the variety of new and emerging tobacco products on the market (USDHHS, 2014), and adolescents’ interest in new products (Arrazola et al., 2014; Harrell et al., 2016; Trinidad et al., 2017), policy makers must be vigilant to regulate promotion toward youth. Mass media campaigns emphasizing risks associated with dual tobacco and marijuana use and price increases are effective techniques for reducing adolescent smoking initiation (USDHHS, 2012) and should be inclusive of multiple tobacco products. Increasing the minimum age to purchase tobacco products from 18 to 21 (Tobacco 21), also shows promise reducing tobacco initiation (USDHHS, 2012; Winickoff et al., 2014) and pursuit by more states is a warranted goal.
This study also identified risk factors associated with dual lifetime use of tobacco and marijuana compared to single use of either tobacco or marijuana. Findings are consistent with studies of non-U.S. adolescents, which found that dual use of cigarettes and marijuana (Georgiades and Boyle, 2007; Suris et al., 2007) is associated with greater psychosocial problems than use of marijuana alone (Peters et al., 2012). Additionally, previous work has documented that substance use is higher among dual users of cigarettes and marijuana compared to cigarette-only users (Ramo et al., 2013). Our work extends the few existing studies to a diverse sample of U.S. adolescents, and includes a comprehensive assessment of tobacco products.
Of the three domains of measured Social Cognitive Theory variables, certain environmental factors lend themselves to group-based interventions. For example, lower parental monitoring was linked with dual tobacco or marijuana use and provides an actionable target for preventive interventions that increase attention and tracking of adolescent activity in unsupervised situations and outside of the home (Dishion and McMahon, 1998). As the transition from childhood to adolescence occurs, the need for parental monitoring to adapt to developmental changes that include more time spent outside of the home, such as in school or before/after school, increases (Dishion and McMahon, 1998). Such things as participation in organized after school activities and structured peer groups are measurable actions that parents can use to enhance parental monitoring. This complements prospective work which has found that unsupervised time with peers over the course of high school is linked to greater substance use by the end of high school (Lee and Vandell, 2015).
Similarly, less exposure to cyberbullying was linked to never use of tobacco or marijuana and could also be targeted in educational approaches that enhance responsive skills. There is a need to educate adolescents regarding healthy and safe use of technology and what constitutes misuse. This can be achieved through formal prevention program delivery (e.g., school wide campaigns) or through in class delivery by teachers discussing the appropriate use of electronic media, identifying what cyberbullying is, and how to address it if it is encountered (Snakenborg et al., 2011).
When considering study implications, it should be considered that the effect sizes for environmental (and personal) factors linking with tobacco and marijuana use were smaller than for behavioral factors. Nonetheless, both environmental and personal factors are viable targets for preventive and clinical interventions, which may affect not only tobacco and marijuana use, but their strongest behavioral correlates of alcohol and other drug use. There is evidence that environmental factors, such as stress, predict addictive behaviors prospectively and that the reverse relationship is not as strong (Walsh, 2013), and that improving personal protective factors are linked with adaptive substance use outcomes (Brown et al., 2008, 2013). However, longitudinal work is needed to understand temporal relationships between risk and protective variables with tobacco and marijuana use and determine optimal timing for interventions to reduce harmful behaviors.
Study results must be considered in light of the significant limitation of sampling of students at a single high school. Although the ethnic diversity of this high school was a strength, particularly given elevated rates of emerging tobacco product use among ethnic minority adolescents (Arrazola et al., 2014; Harrell et al., 2016; Neff et al., 2015; Trinidad et al., 2017), replication of this study at multiple schools and in additional geographic areas is recommended. Additionally, although current use of tobacco and marijuana were assessed, this data was unable to be fully integrated into analyses due to low overall frequency yielding estimates unreliable. Despite this limitation, the study results fit within the broader literature that has characterized lifetime use of tobacco and marijuana (Agrawal et al., 2012).
Dual use of tobacco and marijuana is becoming increasingly common, and presents a health risk (Meier and Hatsukami, 2016) as well as a challenge for marijuana use treatment (Haney et al., 2013; Peters et al., 2012). Tobacco use is recognized as typically preceding marijuana use (Beenstock and Rahav, 2002; Kandel and Kandel, 2015), and has also been identified as a mediating factor between marijuana use and dependence (Hindocha et al., 2015). This body of work suggests the need for continued tobacco regulatory efforts toward youth, with particular vigilance toward new and emerging products (Arrazola et al., 2014; Harrell et al., 2016; Trinidad et al., 2017; USDHHS, 2012, 2014). Given evidence that trying a cigarette even once is linked to later smoking (Birge et al., 2017; Fidler et al., 2006), it is paramount that concerted regulatory actions toward preventing youth experimentation with tobacco be undertaken. Additionally, future work should include an assessment of co-administration of tobacco and marijuana (i.e., use of tobacco and marijuana at the same time) given elevated risks and increased subjective effects (Schauer et al., 2017).
Highlights.
Three clusters of adolescent lifetime tobacco use patterns were identified
Each tobacco cluster had a distinct profile of risk behaviors
Risk escalated with use of more tobacco products
Dual tobacco and marijuana use was riskier than single use of either product
Acknowledgments
We are grateful for the support and assistance of the faculty and administrators at the study site. This study required the time and talents of many CSUSM students and their significant contributions are greatly appreciated: Ashley Emami, Alexa Kliebenstein, Kathryn Shaw, Jamie West, Isaura Alvarez, Keith Burton, Charlotte Carpentier, Christina Drumm, Marissalyn Gonzalez, Melissa Gary, Amy Hartwell, Dustin Kessler, Victoria Lamb, Derek Mateo, Linda Nieto, Rachael Nosewicz, Madeline Rayon, Caroline Robison, Alexis Saucedo, Rachel Schulte, Danica Taylor, Heather Thompson, and Jackie Velazquez. Finally, we are grateful to the students who participated in this research. The following individuals assisted with the preparation of data, figures, and tables: Laura Gasca, Alyssa Victory, Jessica Steffan, Josefa Gregorio, Leslie Lopez, and Cayla Christensen.
Role of the Funding Source
This study was supported by grants from California State University San Marcos (SH and KP). MJS was supported by RISE GM-64783 and NARCH GM106376-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
KP, AW, MJS, SH, and DR conceptualized the study; CR, MJS, GH, and DR conducted literature search and summarized literature; CR and AW conducted data analyses and wrote results; AW created tables and figures; KP wrote the abstract, introduction, methods, and discussion. All authors provided input on the writing of the paper and have approved of the submission.
Conflicts of Interest
None declared.
References
- Agrawal A, Budney AJ, Lynskey MT. The co- occurring use and misuse of cannabis and tobacco: A review. Addiction. 2012;107:1221–1233. doi: 10.1111/j.1360-0443.2012.03837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Silberg JL, Lynskey MT, Maes HH, Eaves LJ. Mechanisms underlying the lifetime co-occurrence of tobacco and cannabis use in adolescent and young adult twins. Drug Alcohol Depend. 2010;108:49–55. doi: 10.1016/j.drugalcdep.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali M, Gray TR, Martinez DJ, Curry LE, Horn KA. Risk profiles of youth single, dual, and poly tobacco users. Nicotine Tob. Res. 2016;18:1614–1621. doi: 10.1093/ntr/ntw028. [DOI] [PubMed] [Google Scholar]
- Apelberg BJ, Corey CG, Hoffman AC, Schroeder MJ, Husten CG, Caraballo RS, Backinger CL. Symptoms of tobacco dependence among middle and high school tobacco users: Results from the 2012 National Youth Tobacco Survey. Am. J. Prev. Med. 2014;47(Suppl. 1):S4–14. doi: 10.1016/j.amepre.2014.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrazola RA, Neff LJ, Kennedy SM, Holder-Hayes E, Jones CD. Tobacco use among middle and high school students--United States, 2013. MMWR Morb. Mortal. Wkly. Rep. 2014;63:1021–1026. [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Beenstock M, Rahav G. Testing Gateway Theory: Do cigarette prices affect illicit drug use? J. Health Econ. 2002;21:679–698. doi: 10.1016/s0167-6296(02)00009-7. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Stratton E, Schauer GL, Lewis M, Wang Y, Windle M, Kegler M. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst. Use Misuse. 2015;50:79–89. doi: 10.3109/10826084.2014.958857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birge M, Duffy S, Miler JA, Hajek P. What proportion of people who try one cigarette become daily smokers? A meta analysis of representative surveys. Nicotine Tob. Res. 2017 doi: 10.1093/ntr/ntx243. [published online]. doi: doi.org/10.1093/ntr/ntx243. [DOI] [PubMed] [Google Scholar]
- Bliss C. The comparison of dosage-mortality data. Annal. Applied Biol. 1935;22:307–333. [Google Scholar]
- Bombard JM, Pederson LL, Koval JJ, O'Hegarty M. How are lifetime polytobacco users different than current cigarette-only users? Results from a Canadian young adult population. Addict. Behav. 2009;34:1069–1072. doi: 10.1016/j.addbeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Camchong J, Lim KO, Kumra S. Adverse effects of cannabis on adolescent brain development: A longitudinal study. Cereb. Cortex. 2016;27:1922–1930. doi: 10.1093/cercor/bhw015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caraballo RS, Novak SP, Asman K. Linking quantity and frequency profiles of cigarette smoking to the presence of nicotine dependence symptoms among adolescent smokers: Findings from the 2004 National Youth Tobacco Survey. Nicotine Tob. Res. 2009;11:49–57. doi: 10.1093/ntr/ntn008. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed on 16 March 2016];National Youth Tobacco Survey (NYTS) 2012 Retrieved from http://www.cdc.gov/tobacco/data_statistics/surveys/nyts.
- Centers for Disease Control and Prevention. [Accessed on 16 March 2016];2015 State and Local Youth Risk Behavior Survey. 2015 Retrieved from ftp://ftp.cdc.gov/pub/data/yrbs/2015/2015_hs_questionnaire.pdf.
- Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. Measuring stress: A guide for health and social scientists. Oxford University Press; Oxford: 1994. [Google Scholar]
- Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, Mermelstein R. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict. Behav. 2015;48:79–88. doi: 10.1016/j.addbeh.2015.02.005. [DOI] [PubMed] [Google Scholar]
- Connelly-Brejank S, Hamill S, Diaz C, Merlino K, Young B. Personal responsibility in college students: Development of a new scale; Paper presented at the Western Psychological Association; San Francisco, CA. 2012. [Google Scholar]
- Creamer MR, Portillo GV, Clendennen SL, Perry CL. Is adolescent poly-tobacco use associated with alcohol and other drug use? Am. J. Health Behav. 2016;40:117–122. doi: 10.5993/ajhb.40.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dir AL, Gilmore AK, Moreland AD, Davidson TM, Borkman AL, Rheingold AA, Danielson CK. What's the harm? Alcohol and marijuana use and perceived risks of unprotected sex among adolescents and young adults. Addict. Behav. 2018;76:281–284. doi: 10.1016/j.addbeh.2017.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clin. Child Fam. Psychol. Rev. 1998;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Doran N, Trim RS. Correlates of other tobacco use in a community sample of young adults. Addict. Behav. 2015;51:131–135. doi: 10.1016/j.addbeh.2015.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois S, Mullen N, Weaver B, Bédard M. The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forens. Sci. Int. 2015;248:94–100. doi: 10.1016/j.forsciint.2014.12.018. [DOI] [PubMed] [Google Scholar]
- Enofe N, Berg CJ, Nehl EJ. Alternative tobacco use among college students: Who is at highest risk? Am. J. Health Behav. 2014;38:180–189. doi: 10.5993/ajhb.38.2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler J, Wardle J, Brodersen NH, Jarvis M, West R. Vulnerability to smoking after trying a single cigarette can lie dormant for three years or more. Tobacco Control. 2006;15:205–209. doi: 10.1136/tc.2005.014894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiades K, Boyle MH. Adolescent tobacco and cannabis use: Young adult outcomes from the Ontario Child Health Study. J. Child Psychol. Psychiatry. 2007;48:724–731. doi: 10.1111/j.1469-7610.2007.01740.x. [DOI] [PubMed] [Google Scholar]
- Green KM, Musci RJ, Matson PA, Johnson RM, Reboussin BA, Ialongo NS. Developmental patterns of adolescent marijuana and alcohol use and their joint association with sexual risk behavior and outcomes in young adulthood. J. Urban Health. 2017;94:115–124. doi: 10.1007/s11524-016-0108-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberger E, Josselson R, Knerr C, Knerr B. The measurement and structure of psychosocial maturity. J. Youth Adolesc. 1975;4:127–143. doi: 10.1007/BF01537437. [DOI] [PubMed] [Google Scholar]
- Hagenaars JA, McCutcheon AL. Applied latent class analysis. Cambridge University Press; Cambridge: 2002. [Google Scholar]
- Haney M, Bedi G, Cooper ZD, Glass A, Vosburg SK, Comer SD, Foltin RW. Predictors of marijuana relapse in the human laboratory: Robust impact of tobacco cigarette smoking status. Biol. Psychiatry. 2013;73:242–248. doi: 10.1016/j.biopsych.2012.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson KL, Winward JL, Schweinsburg AD, Medina KL, Brown SA, Tapert SF. Longitudinal study of cognition among adolescent marijuana users over three weeks of abstinence. Addict. Behav. 2010;35:970–976. doi: 10.1016/j.addbeh.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell PT, Naqvi SMH, Plunk AD, Ji M, Martins SS. Patterns of youth tobacco and polytobacco usage: The shift to alternative tobacco products. Am. J. Drug Alcohol Abuse. 2016;43:693–702. doi: 10.1080/00952990.2016.1225072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, Schalet BD, Malone SM, Iacono WG, McGue M. Psychometric and genetic architecture of substance use disorder and behavioral disinhibition measures for gene association studies. Behav. Genet. 2011;41:459–475. doi: 10.1007/s10519-010-9417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindocha C, Shaban ND, Freeman TP, Das RK, Gale G, Schafer G, Falconer CJ, Morgan CJ, Curran HV. Associations between cigarette smoking and cannabis dependence: A longitudinal study of young cannabis users in the United Kingdom. Drug Alcohol Depend. 2015;148:165–171. doi: 10.1016/j.drugalcdep.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi M, Joshi A, Bartter T. Marijuana and lung diseases. Curr. Opin. Pulm. Med. 2014;20:173–179. doi: 10.1097/MCP.0000000000000026. [DOI] [PubMed] [Google Scholar]
- Kandel D, Kandel E. The Gateway Hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Paediatrica. 2015;104:130–137. doi: 10.1111/apa.12851. [DOI] [PubMed] [Google Scholar]
- Kann L. Youth risk behavior surveillance—United States, 2015. MMWR Morb. Mortal. Wkly. Rep. Surveill. Summ. 2016;65:1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings M, Sharma E, Pearson JL, Green VR, Kaufman AR, Bansal-Travers M, Travers MJ, Kwan J, Tworek C, Cheng Y, Yang L, Pharris-Ciurej N, van Bemmel DM, Backinger CL, Compton WL, Hyland AJ. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 2017;376:342–353. doi: 10.1056/NEJMsa1607538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Myers J, Damaj MI, Chen X. Early smoking onset and risk for subsequent nicotine dependence: A monozygotic co-twin control study. Am. J. Psychiatry. 2013;170:408–413. doi: 10.1176/appi.ajp.2012.12030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopak AM, Ayers S, Lopez V, Stevenson P. Parental monitoring, alcohol, and marijuana use among Hispanic and non-Hispanic white adolescents: Findings from the Arizona Youth Survey. J. Drug Issues. 2011;41:461–486. doi: 10.1177/002204261104100402. [DOI] [Google Scholar]
- Kristjansson AL, Mann MJ, Sigfusdottir ID. Licit and illicit substance use by adolescent e-cigarette users compared with conventional cigarette smokers, dual users, and nonusers. J. Adolesc. Health. 2015;57:562–564. doi: 10.1016/j.jadohealth.2015.07.014. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA. New methods shed light on age of onset as a risk factor for nicotine dependence. Addict. Behav. 2015;50:161–164. doi: 10.1016/j.addbeh.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KT, Vandell DL. Out-of-school time and adolescent substance use. J. Adolesc. Health. 2015;57:523–529. doi: 10.1016/j.jadohealth.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessard J, Henrie J, Livingston JA, Leonard KE, Colder CR, Eiden RD. Correlates of ever having used electronic cigarettes among older adolescent children of alcoholic fathers. Nicotine Tob. Res. 2014;16:1656–1660. doi: 10.1093/ntr/ntu148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Gruenewald PJ, Grube JW, Bersamin M. Adolescents, alcohol, and marijuana: Context characteristics and problems associated with simultaneous use. Drug Alcohol Depend. 2017;179:55–60. doi: 10.1016/j.drugalcdep.2017.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschall D, Sanftner J, Tangney J. The state shame and guilt scale (SSGS) George Mason University; Fairfax, VA: 1994. [Google Scholar]
- Meier E, Hatsukami DK. A review of the additive health risk of cannabis and tobacco co-use. Drug Alcohol Depend. 2016;166:6–12. doi: 10.1016/j.drugalcdep.2016.07.013. [DOI] [PubMed] [Google Scholar]
- Montgomery L. Marijuana and tobacco use and co-use among African Americans: Results from the 2013 National Survey on Drug Use and Health. Addict. Behav. 2015;51:18–23. doi: 10.1016/j.addbeh.2015.06.046. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus User's Guide. 7. Muthén and Muthén; Los Angeles: 1998. [Google Scholar]
- National Institute on Drug Abuse. DrugFact: Nationwide trends. 2014 Retrieved from https://www.drugabuse.gov/publications/drugfacts/nationwide-trends.
- Neff L, Arrazola R, Caraballo R, Corey C, Cox S, King B. Frequency of tobacco use among middle and high school students—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2015;64:1061–1065. doi: 10.15585/mmwr.mm6438a1. [DOI] [PubMed] [Google Scholar]
- Neff LJ, Arrazola RA, Caraballo RS, Corey CG, Cox S, King BA, Choiniere CJ, Husten CG. Frequency of tobacco use among middle and high school students--United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2015;64:1061–1065. doi: 10.15585/mmwr.mm6438a1. [DOI] [PubMed] [Google Scholar]
- Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J. Consult. Clin. Psychol. 2004;72:400–410. doi: 10.1037/0022-006x.72.3.400. [DOI] [PubMed] [Google Scholar]
- Osibogun O, Jaber R, Bahelah R, Taleb ZB, Maziak W. Poly-tobacco use among young adults in the United States: Findings from the Population Assessment on Tobacco and Health Study, 2013–2014. Annals Epidemiol. 2017;27:535. [Google Scholar]
- Pacek LR, Sweitzer MM, McClernon FJ. Non-cigarette tobacco and poly-tobacco use among persons living with HIV drawn from a nationally representative sample. Drug Alcohol Depend. 2016;162:251–255. doi: 10.1016/j.drugalcdep.2016.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Budney AJ, Carroll KM. Clinical correlates of co-occurring cannabis and tobacco use: A systematic review. Addiction. 2012;107:1404–1417. doi: 10.1111/j.1360-0443.2012.03843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson AL, Severson HH, Andrews JA, Gott SP, Cigrang JA, Gordon JS, Hunter CM, Martin GC. Smokeless tobacco use in military personnel. Mil. Med. 2007;172:1300–1305. doi: 10.7205/milmed.172.12.1300. [DOI] [PubMed] [Google Scholar]
- Philibert RA, Gunter TD, Beach SR, Brody GH, Hollenbeck N, Andersen A, Adams W. The role of GABRA2 on risk for alcohol, nicotine and cannabis dependence in the Iowa adoption studies. Psychiatric Genet. 2009;19:91. doi: 10.1097/YPG.0b013e3283208026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinsker EA, Berg CJ, Nehl EJ, Prokhorov AV, Buchanan TS, Ahluwalia JS. Intent to quit among daily and non-daily college student smokers. Health Educ. Res. 2013;28:313–325. doi: 10.1093/her/cys116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin RA, George TP. A review of co-morbid tobacco and cannabis use disorders: Possible mechanisms to explain high rates of co- use. Am. J. Addict. 2015;24:105–116. doi: 10.1111/ajad.12186. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Ramo DE, Delucchi KL, Hall SM, Liu H, Prochaska JJ. Marijuana and tobacco co-use in young adults: patterns and thoughts about use. J. Stud. Alcohol Drugs. 2013;74:301–310. doi: 10.15288/jsad.2013.74.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolle IV, Kennedy SM, Agaku I, Jones SE, Bunnell R, Caraballo R, Xu X, Schauer G, McAfee T. Cigarette, cigar, and marijuana use among high school students - United States, 1997–2013. MMWR Morb. Mortal. Wkly. Rep. 2015;64:1136–1141. doi: 10.15585/mmwr.mm6440a2. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the self. Basic; New York: 1979. [Google Scholar]
- Saddleson ML, Kozlowski LT, Giovino GA, Hawk LW, Murphy JM, MacLean MG, agoniewicz ML, Homish GG, Wrotniak BH, Mahoney MC. Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug Alcohol Depend. 2015;149:25–30. doi: 10.1016/j.drugalcdep.2015.01.001. [DOI] [PubMed] [Google Scholar]
- Schauer G, Rosenberry Z, Peters E. Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addict. Behav. 2017;64:200–211. doi: 10.1016/j.addbeh.2016.09.001. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M. Differences in tobacco product use among past month adult marijuana users and nonusers: Findings from the 2003-2012 National Survey on Drug Use and Health. Nicotine Tob. Res. 2016;18:281–288. doi: 10.1093/ntr/ntv093. [DOI] [PubMed] [Google Scholar]
- Snakenborg J, Van Acker R, Gable RA. Cyberbullying: Prevention and intervention to protect our children and youth. Prev. Sch. Fail. 2011;55:88–95. [Google Scholar]
- Snyder CR, Hoza B, Pelham WE, Rapoff M, Ware L, Danovsky M. The development and validation of the Children's Hope Scale. J. Pediatr. Psychol. 1997;22:399–421. doi: 10.1093/jpepsy/22.3.399. [DOI] [PubMed] [Google Scholar]
- Suris J, Akre C, Berchtold A, Jeannin A, Michaud PA. Some go without a cigarette: Characteristics of cannabis users who have never smoked tobacco. Arch. Pediatr. Adolesc. Med. 2007;161:1042–1047. doi: 10.1001/archpedi.161.11.1042. [DOI] [PubMed] [Google Scholar]
- Sutfin EL, McCoy TP, Berg CJ, Champion H, Helme DW, O'Brien MC, Wolfson M. Tobacco use by college students: A comparison of daily and nondaily smokers. Am. J. Health Behav. 2012;36:218–229. doi: 10.5993/ajhb.36.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using multivariate statistics. Pearson; New York City: 2007. pp. 402–407. [Google Scholar]
- Trinidad DR, Pierce JP, Sargent JD, White MM, Strong DR, Portnoy DB, Green VR, Stanton CA, Choi K, Bansal-Travers M, Shi Y, Pearson JL, Kaufman AR, Borek N, Coleman BN, Hyland A, Carusi C, Kealey S, Leas E, Noble ML, Messer K. Susceptibility to tobacco product use among youth in wave 1 of the Population Assessment of Tobacco and Health (PATH) study. Prev. Med. 2017;101:8–14. doi: 10.1016/j.ypmed.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services (USDHHS) Preventing tobacco use among youth and young adults: A report of the Surgeon General, 2012. US Department of Health and Human Services; Atlanta, GA: 2012. Retrieved from https://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/index.html. [Google Scholar]
- US Department of Health and Human Services (USDHHS) The health consequences of smoking - 50 years of progress: A Report of the Surgeon General. US Department of Health and Human Services; Atlanta, GA: 2014. Retrieved from https://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html. [Google Scholar]
- White J, Walton D, Walker N. Exploring comorbid use of marijuana, tobacco, and alcohol among 14 to 15-year-olds: Findings from a national survey on adolescent substance use. BMC Public Health. 2015;15:233. doi: 10.1186/s12889-015-1585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135:e43–51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Windle RC. Early onset problem behaviors and alcohol, tobacco, and other substance use disorders in young adulthood. Drug Alcohol Depend. 2012;121:152–158. doi: 10.1016/j.drugalcdep.2011.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winickoff JP, Gottlieb M, Mello MM. Tobacco 21—an idea whose time has come. N. Engl. J. Med. 2014;370:295–297. doi: 10.1056/NEJMp1314626. [DOI] [PubMed] [Google Scholar]
- Yates EA, Dubray J, Schwartz R, Kirst M, Lacombe-Duncan A, Suwal J, Hatcher J. Patterns of cigarillo use among Canadian young adults in two urban settings. Can. J. Public Health. 2014;105:e11–14. doi: 10.17269/cjph.105.3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yayan J, Rasche K. Damaging effects of cannabis use on the lungs. Adv. Exp. Med. Biol. 2016;952:31–34. doi: 10.1007/5584_2016_71. [DOI] [PubMed] [Google Scholar]