Abstract
Background
Resource allocation in patient care relies heavily on individual judgements of healthcare professionals. Such professionals perform coordinating functions by managing the timing and execution of a multitude of care processes for multiple patients. Based on advances in simulation, new technologies that could be used for establishing realistic representations have been developed. These simulations can be used to facilitate understanding of various situations, coordination training and education in logistics, decision-making processes, and design aspects of the healthcare system. However, no study in the literature has synthesized the types of simulations models available for non-technical skills training and coordination of care.
Methods
A systematic literature review, following the PRISMA guidelines, was performed to identify simulation models that could be used for training individuals in operative logistical coordination that occurs on a daily basis. This article reviewed papers of simulation in healthcare logistics presented in the Web of Science Core Collections, ACM digital library, and JSTOR databases. We conducted a screening process to gather relevant papers as the knowledge foundation of our literature study. The screening process involved a query-based identification of papers and an assessment of relevance and quality.
Results
Two hundred ninety-four papers met the inclusion criteria. The review showed that different types of simulation models can be used for constructing scenarios for addressing different types of problems, primarily for training and education sessions. The papers identified were classified according to their utilized paradigm and focus areas. (1) Discrete-event simulation in single-category and single-unit scenarios formed the most dominant approach to developing healthcare simulations and dominated all other categories by a large margin. (2) As we approached a systems perspective (cross-departmental and cross-institutional), discrete-event simulation became less popular and is complemented by system dynamics or hybrid modeling. (3) Agent-based simulations and participatory simulations have increased in absolute terms, but the share of these modeling techniques among all simulations in this field remains low.
Conclusions
An extensive study analyzing the literature on simulation in healthcare logistics indicates a growth in the number of examples demonstrating how simulation can be used in healthcare settings. Results show that the majority of studies create situations in which non-technical skills of managers, coordinators, and decision makers can be trained. However, more system-level and complex system-based approaches are limited and use methods other than discrete-event simulation.
Keywords: Quality, Safety, Logistical simulations, Non-technical skills
Background
Quality and safety in healthcare depend on the successful interaction between multiple teams, individuals, and support processes aimed at making the right resources, such as medications, medical equipment, information, and people, available at the right time [1, 2]. Furthermore, in many healthcare settings, resource utilization must be prioritized such that the person most in need of a resource from a medical perspective will receive it. The cost of failure is high, both in terms of personal tragedies as well as the socio-economic burden of increased costs due to prolonged treatments or hospital stay [3].
Many of the everyday decisions regarding how resources will be used for patient care are made by individuals and networks of people performing coordinating functions, in the sense that they manage the timing and execution of many care processes of multiple patients. Their decisions often depend on judgements combining perspectives on the relevant medical conditions, the resources at hand, and the urgency of the situation; their decisions also depend on receiving information to help make sense of the situation as well as managing high stakes and competing goals [4].
Little is known about how these prioritizing and coordination skills are learned, how people performing them build their mental system models, what information and strategies they use, and which work practices are most successful. Most of the individuals performing coordination tasks are trained on the job in an unsystematic manner, and the knowledge remains, for the most part, tacit.
Simulation in healthcare is well known as a method for training individuals and teams in escalating situations surrounding individual patients [5]. To create meaningful simulations for training the non-technical skills used in coordination [6], there is a need to develop simulations of logistical challenges in a systematic manner as well as to describe and develop learning outcomes for the non-technical skills used in coordination. To support this development, it is important to know what types of logistical problems can be addressed by what types of simulations.
Logistics is one of many growing fields in healthcare management. This trend is driven by various societal impacts; population growth and an aging society have already put pressure on the operation of healthcare systems [7, 8]. While healthcare logistics has been defined in various ways by researchers, in this paper, we define it as “operational handlings for the delivery of care, including its supportive services, from origination to recipient.” Focusing on the recipient of services, healthcare logistics could be patient-centric or material-centric. Patient-centric logistics relate to patient flows through the healthcare system. In this context, quality, safety, and efficiency of services for patients are keywords. Material-centric logistics address the positioning, storage, and circulation of goods and materials, such as blood and pharmaceutical products, within the hospital or the healthcare system.
Computer-based simulation plays an important role in the operational support of healthcare logistics. Generally, simulation can be useful in the design of complex social-technical systems [9]. As an innovative technology for adding analytical capacity, simulation can be used as an intermediate test in the (re)design of organizational rules and structures, workflow process management, performance, and avoidance of human errors [10, 11]. More specifically, according to Jun et al. [12], simulation could provide benefits such as more effective redesign or innovation, deeper insights into barriers and incentives to adoption, and provision of an environment to “bench-test” final products prior to formal release. A change or improvement in real systems, however, might be expensive or dangerous, and balancing resource allocations is a central non-technical skill for healthcare professionals. Simulation adds value by providing a solution for training individuals to solve customized problems in a virtual, persuasive environment.
The application of discrete-event simulation in healthcare began to grow considerably at the end of the 1990s [12]; however, it remains unknown what type of simulations could be used to train, develop, and test non-technical aspects of coordination. Many types of simulation paradigms exist today. Discrete-event simulation, system dynamics, and agent-based simulation are the most utilized tools for modeling and analyzing systems according to the user’s interests and the specific task addressed. Discrete-event simulation is a tool for assessing the efficiency of delivery structures, forecasting changes in patient flow and examining resource efficiency in staffing [12]. System dynamics focus on the effect of structure on behavior [13]. Instead of addressing individual transactions, system dynamics is commonly used for higher level problems, such as strategic decision making, management controls, or policy changes [14]. Agent-based simulation is based on a “bottom-up” construction for the provision of emergent phenomena based on individual interactions of resource units [15].
Literature reviews have been conducted with explicit focus on the application of simulation in patient flow or material flow. However, previous literature reviews have been limited in at least one of the following aspects: (1) Reviews usually address simulation of healthcare logistics in a very narrow manner, analyzing a single key aspect such as low stakeholder engagement [16], a single simulation technique [17], or a single department; (2) most reviews have examined papers published before 2012.
This study is a continuation of the work by Dieckmann et al. [6], with a focus on the identification of available simulation models to provide meaningful training of non-technical skills in healthcare logistics. This is the perspective through which the literature was reviewed and understood. Given the large number of training simulations published, it is of interest to explore the diversity in this genre. The objective of this study is to provide a systematic literature review to answer the following research question:
What types of simulation models are currently available for training non-technical skills in handling logistical issues?
Methods
Search strategy
To answer the research question, the Web of Science Core Collection, the ACM Digital Library, and JSTOR were searched to retrieve articles focusing on simulation in healthcare logistics between 1998 and 2017. We utilized papers from these three databases because all of them rigorously select core journals and the keynote proceedings of conferences. The search terms were divided into the following two categories: patient-centric queries and material-centric queries. The papers were screened following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.
The keywords were formulated by the individual reviewers to identify papers on relevant simulation techniques and investigated systems, as summarized in Table 1. Keywords such as “healthcare,” “patient flow,” “pharma*,” “blood,” and “drug” specify the issues addressed. Keywords such as “simulation,” “system dynamics,” “simulator,” and “game” specify the research methods implemented.
Table 1.
Queries used for the different databases
| Database | Patient-centric queries | Material-centric queries |
|---|---|---|
| Web of Science Core Collection | TI = ((“healthcare” OR “health SAME care”) AND (“system SAME dynamics” OR “patient SAME flow” OR “gam*”) | TI = (“healthcare” OR “health SAME care OR care”) AND TS = (“pharma*” OR “blood” OR “drug”) AND TI = (“simulation” OR “system SAME dynamic*” OR “simulator*” OR “gam*”) |
| ACM | recordAbstract:(+(“health care” “healthcare”) + (“system dynamics” “patient flow” “gam*”)) | recordAbstract:(+(“hospital” “drug” “pharma*” “blood”) + (“simulation” “simulator*” “gam*”)) |
| JSTOR | ti:(“healthcare” OR “health care”) AND (“system dynamics” OR “patient flow” OR “game” OR “simulation”) | ti:((“drug” OR “hospital” OR “blood” OR “pharmaceutical”) AND (“system dynamics” OR “patient flow” OR “game” OR “simulation” OR “simulator”)) |
SAME, OR, and AND are logic operators of keywords
Paper inclusion criteria
The criteria for inclusion in this review were that studies addressed the research question and strive to improve the performance of healthcare logistics. As the focus was logistical issues in healthcare management, publications regarding epidemiology, nutrition process improvement, and statistical analysis of health programs were not included. Abstracts, book reviews of limited length, and papers not granting access to full texts were also discarded. In addition to these general requirements, criteria for classification were implemented:
Application-oriented paper. The paper employs at least one simulation technique and presents a detailed scenario, or experiment, of a real-world healthcare system.
Subjective and methodological paper. The paper focuses on subjective and methodological perspectives on simulation techniques but might not report a use case (Fig. 1).
Fig. 1.
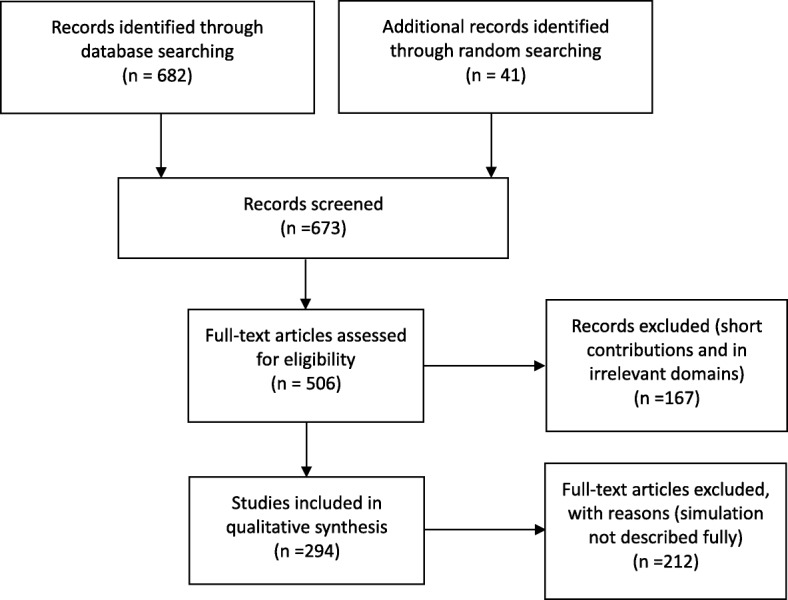
PRISMA flow diagram of assessment procedure and results: number of records included and excluded and reasons
The scope of the research and focus area were decided after the screening process. Simulation paradigms were classified based on statements from the authors; if no simulation technique was stated, the conceptualization framework was checked to determine its relevant category.
Results
Following the retrieval of papers, discarding of duplicates, and review by the authors, the total number of essential publications was 294. The search identified 248 patient-centric and 46 material-centric papers. The patient-centric spectrum included 214 problem-solving papers, among which 114 utilized discrete-event simulation. For material-centric papers, discrete-event simulation was the dominant simulation paradigm as well. The number of publications for the past 5 years remained high, reinforcing our supposition that there is much knowledge to be gained from recent publications. The repository is available in the declaration.
For qualitative analysis, representative papers, listed in Table 2, were identified. The papers featured statements of the relevant research questions or a description of the investigated system. We considered the number of publications utilizing different simulation techniques, scopes of research, and tools.
Table 2.
Catalog of papers
| Focused issue | Reference | Paradigm | Scale | Software | Representative main finding |
|---|---|---|---|---|---|
| Care pathway and appointment | [19–21, 25, 26, 28, 29, 43, 47, 50–87, 88–127] | DES (63); ABS (3); SD (3); mixed (4), Misc. (16) | Single department (65), Cross-departments (17), cross-institutional (7) | Arena (30); Simul8(5); FlexSim (5); AnyLogic (3); NetLogo (2); Witness (2); ProModel (1); C++(1); ProcessModel (1); Microsoft Excel (1); iThink (1); AutoMod (1); SLX (2); EDSim (1); Matlab (1); DGHPSim (1); ARIS (1); MedModel (3); OMNeT++ (1); Misc. (27) | These studies focus on modeling patient pathways from admission to discharge as acting the basis of direct intervention on patient flows. |
| Staffing decision making | [24, 35, 37, 42, 46, 49, 55, 128–202, 248] | DES (50); SD (3); ABS (3); gaming (1); mixed (26), Misc.(5) | Single department (56), cross-departments (22), cross-institutional (10) | Arena (22); FlexSim (7); AnyLogic (5); Simul8(3); MedModel (3); FDI (3); Matlab (2); ProModel (2); Tecnomatix Plant Simulation (2); ARCINFO (1); AutoMod (1); C++ (1); Petri Nets (1); Extend (1); Microsoft Excel (1); Netlogo (1); OMNeT++(1); Venism (1); SLX (1); SIMPROCESS (1); STELLA (1); ABFS (1); Java IDE (1); Misc. (27); | These studies use simulation for decision support of care capacities. |
| Work procedures | [203–214] | DES (8); Misc. (4) | Single department (7), cross-departments (5) | Arena (3); Simul8(2); ProModel (1); MedModel (1); OMNeT++ (1); ExtendSim (1); Misc. (3) | Simulation is used to identify impact factors in service procedures. |
| Specialized Transport | [215–222] | DES (2); ABS (1); Misc. (5) | Cross-institutional (8) | Arena (2); ArcGIS (1); Google Cloud (1); Microsoft Excel (1); Misc. (3) | These studies address handling of patients in the regional healthcare network. |
| Facility design | [223–230] | DES (4); ABS (2); mixed (1); Misc. (1) | Single department (2), cross-departments (1) | Unity (1); ProModel (1); NetLogo (1); Extend (1); Misc. (4) | These studies use simulations to analyze hospital infrastructure and its impact on the operation. |
| Healthcare systems | [231–235] | DES (1); ABS (2); Misc. (2) | Cross-institutional (5) | Arena (2); Python (1); AnyLogic (1); NetLogo (1) | These studies use simulations to support the modeling and analysis of improvements in the system perspective. |
| Supply chain | [236–243] | DES (5), gaming (1); Misc. (2) | Cross-departments (5), cross-institutional (3) | ExtendSim (1); GAMS (1); Matlab (1); Bonita Open Solution (1), Board game (1); Misc. (3) | The simulation model is generally used for recreating different actors in the supply chain network. |
| Inventory management | [244–258] | DES (8); mixed (2); Misc. (5) | Single department (3), cross-departments (1), cross-institutional (11) | Simul8 (2); Arena (2); C++(1); CSIM18 (1); Java (1); JSL (1); SCA (1); Misc. (6) | These studies explore different inventory or replacement polities for material handling. |
| Network distribution and dispatching | [32, 259–264] | DES (4); gaming (2); ABS (1); Misc. (3) | Cross-departments (2), cross-institutional (8) | Microsoft Excel (2); Arena (1); MedModel (1); ProModel (1); JADE (1); VBA (1); Misc. (3) | These studies use simulations for operational transport. |
| Network configuration | [265–267] | DES (1); Misc. (2) | Cross-institutional (3) | Arena (1); Misc. (2) | These studies focus on the design of the network. |
| Procurement logistics | [27, 268, 269] | SD (1); Misc. (2) | Cross-department (1), cross-institutional (2) | Qnet2000 (1); iThink (1); Misc. (1) | Simulation is used for understanding the interactive rule between service vendor and recipient. |
| Misc. | [31, 36, 38, 270–281] | DES (4); SD (3); ABS (1); gaming (1); mixed (3); Misc. (4) | Single department (5), cross-departments (4), cross-institutional (7) | Arena (4); AnyLogic (2); iThink (2); Simul8 (1); NetLogo (1); Microsoft Excel (1); Powersim (1); Misc. (4) | |
| Methodology | [12–15, 39, 282–286, 287–305] | Reviews, surveys, and methodological reflections and comparisons of logistics simulations in other sectors. | |||
Following the screening process, we identified the question levels and the categories of addressed issues. The following question levels were derived: single department/unit, cross-department/unit, and cross-institutional. The category single department/unit included studies that model operation within a single department in an organization. The category cross-department/unit included studies that simulate multiple departments/units within the same organization. The category cross-institutional included the simulation modeling of interactions and flows between healthcare service providers in a large-scale network with widespread distribution regions. We identified the following categories of addressed issues: care pathway and appointment, staffing decision making, work procedures, specialized transport, facility design, healthcare systems, supply chain, inventory management, network distribution and dispatching, network configuration, procurement logistics, methodological contributions, and miscellaneous. The facility design was considered because architectural planning is a strategic decision that has a durable and profound effect on healthcare operation. The miscellaneous category included all research publications that we were not able to clearly classify into at least one of the abovementioned categories.
Logistical simulations—review
Discrete-event simulation
Discrete-event simulation has been applied to model and analyze all aspects of logistics management in healthcare. In particular, patient flow management and planning of staffing requirement are effective applications of this simulation technology. Our profiling of the literature is mostly in line with the findings of previous literature reviews; that is, discrete-event simulation is a useful tool with respect to improving patient flow, managing bed capacity, and scheduling and utilizing of resources [16, 17]. DeRienzo et al. addressed the effect of nursing capacity by comparing different nursing sizes and demonstrated the applicability of supporting healthcare managers in handling operative tasks [18]. Devapriya et al. also developed a decision-supporting tool based on discrete-event simulation for the strategic planning of hospital bed capacity [19]. Bhattacharjee et al. analyzed appointment scheduling policies for patients to be treated by a medical scanning machine [20]. Vasilakis et al. developed a discrete-event simulation to study how long it took for patients to obtain their appointments from their referral [21]. Jørgensen et al. investigated internal blood logistics in hospitals and evaluated the effects of various management controls on the waiting times for accessing blood samples [22]. This simulation paradigm is most suitable for the realistic representation of processes in health services for analyzing “what-if” scenarios and assessing the performance of a logistical system.
System dynamics
System dynamics is used for organizational simulations. The paradigm is a mechanism-driven one for making decisions strategically for health services and resources from a global perspective. For instance, Rashwan et al. developed a system dynamics simulation to study bed blocking in Irish hospitals [23]. The focus was twofold: testing the policies for solving delayed discharges and envisaging the counterproductive and unintended consequences of these new policies [24]. Brailsford et al. simulated patient flow perspectives to identify system-wide bottlenecks [25]. Through the simulation, Lane et al. showed that the daily variation of used hospital bed capacity could not be balanced in the long run by simply increasing capacity; instead, optimal design of flows should be the core of the operation technology [26]. One paper investigated logistical outsourcing [27] and deployed system dynamics simulation with a sensitivity analysis for the evaluation and analysis of sustainability and economic performance. Content holders can use system dynamics simulation to envisage the complexity and identify opportunities and risks of the policies and management controls proposed.
Agent-based simulation
Agent-based simulation could be considered a means of soft computing in healthcare logistics. Agent-based simulation provides a gateway for understanding the behavior of distributed and connected service providers. The associated modeling and analysis are able to handle engineering system problems in complex networks. As an example, this paradigm was introduced to solve the coordination and collaboration difficulty of caregivers in a mental healthcare system [28]. The positive effect of coordination technology was confirmed by such modeling considerations. The local decision rules of caregivers were relevant for operative decision making with respect to successful provision of home help, a conclusion drawn from Marcon et al.’s work [29]. Bidding decisions made by distributers and suppliers in the pharmaceutical industry were studied in Jetly et al.’s work [30]. The performance of a multi-site network was simulated with pre-selected indicators, including the number of released products, degree of consolidation, and the return on assets. Multi-agent systems are not only effective for modeling flows between providers; they could also be applied in hospital environments. In Marin et al.’s work, patients, nurses, doctors, and the department as the manager are specified as agents with simple behavior rules [31]. With the support of multi-agent languages, the properties and relationships of actors could be simulated and validated for a specific social-technical environment.
Game and participatory simulation
Games and participatory simulation are life-like media that facilitate experimental learning. The use of such media enables the development of non-technical teamwork skills. For instance, Mustafee and Katsaliaki developed a pedagogical business game that simulated the blood supply chain [32, 33]. The players were encouraged to propose different solutions, taking costs, time-efficiency, and stock levels of products into account. Focusing on quality of service in healthcare, a web-based organizational simulation was built and deployed for training referral and diagnostic skills [34]. The results showed that the usefulness of information on symptoms, diseases, and severity levels is associated with the perception of information sources. A board game provided valuable insight into the adoption of future technology in hospital logistical work [15]. Regarding the practical settings of two hospitals, the adoption of wearable technologies was reflected through role play. Such role playing could also be used to analyze the working environment in wards [35].
Hybrid modeling
Hybrid modeling is the efficient combination of various simulation modeling techniques described. Most hybrid modeling involves coupling discrete-event simulation and system dynamics. Two case studies, concerning infection control and regional social care system engineering, were simulated using hybrid models [36]. Zulkepli modeled an integrated ICU by combining system dynamics and discrete-event simulation [37]. The greatest advantage of hybrid modeling is the ability to integrate different simulation approaches and empirical data from different sources [38].
Analysis of trends
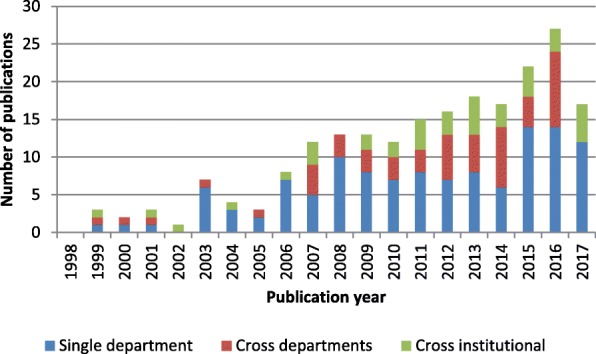
Discrete-event simulation has been the most prominent paradigm for modeling patient-centric logistics over the past decade. Between 2008 and 2017, as presented in Fig. 2, more than half of the included papers used discrete-event simulation. However, the distribution of simulation techniques among different periods showed growing methodological diversity in recent years. The presence of system dynamics is observed in all periods, although the number of publications remained small. Agent-based simulation, games, and hybrid modeling were utilized only in the last decade. The specific simulation paradigm used was not stated in some studies, especially between 1998 and 2007, during which the majority of the methods used were classified as miscellaneous. Game-based methods were used in a few studies. Thus, interactive simulations are still quite new and rarely used.
Fig. 2.

Simulation paradigms for patient-centric logistics
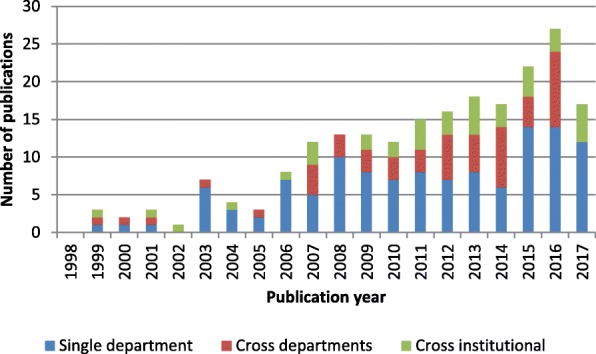
The single category was the predominant level addressed in all periods, as shown in Fig. 3. Between 2008 and 2012, the majority of studies addressed logistical issues at the single-unit level. The systems perspective was introduced between 2013 and 2017. Work addressing logistics issues at the cross-departmental and cross-institutional levels formed half of all research efforts. However, cross-institutional issues remained largely underexplored in the literature compared with other problems studied.
Fig. 3.
Research scope for patient-centric logistics
Discrete-event simulation was the most prominent simulation paradigm in material-centric approaches as well, as shown in Fig. 4. The research theme started to develop in 2006, after which the number of publications and the diversity of the utilized paradigms increased. Despite the growth, six of 16 papers utilized discrete-event simulation, and only three papers utilized system dynamics, agent-based simulation, and/or hybrid modeling.
Fig. 4.
Simulation paradigms for material-centric logistics
Compared with patient-centric logistics, material-centric logistics was covered by a limited number of articles. Shah et al. had already stressed the underexplored potential of this area in 2004 [39]. We identified few publications on this subject during this period. The period 2013–2017 showed the largest output, but the volume was still not able to catch up with that of papers related to patient-centric logistics.
As shown in Fig. 5, a growing number of papers have analyzed material handling between multiple units. However, simulation design for cross- and single-department logistics was lacking over the last 5 years, despite studies reporting on the need for improving hospital internal supply chains to reduce costs [40].
Fig. 5.
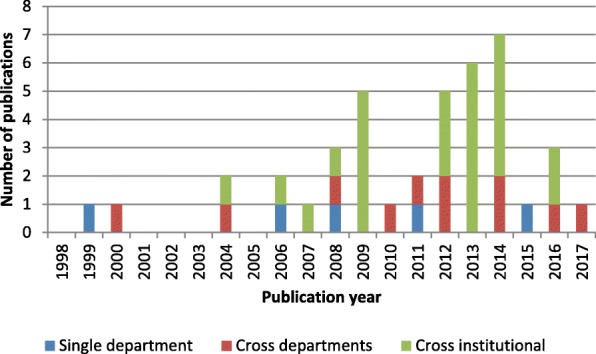
Research scope for material-centric logistics
Discussions
The literature review demonstrated that different simulation techniques could be utilized for different educational purposes, as summarized in Table 3. Discrete-event simulation is suitable for operational problems, whereas strategic issues are better explored by system dynamics. Agent-based simulation stands out as a versatile tool because that agent method is object-oriented and flexible for describing the anatomy of complex systems formed by multiple actors. Healthcare logistics is a complex socio-technical system characterized by interconnected components and non-rational operation management. Agent-based simulation can explicitly model the interaction between system components, facilitating the understanding of overall performance under uncertainty and dynamics.
Table 3.
Guidelines for selecting a suitable logistical simulation model for training purposes
| Discrete-event simulation | System dynamics | Agent-based simulation | Game and participatory simulation | |
|---|---|---|---|---|
| Level of training | Operational | Strategic | All | Tactical, operational |
| Training purpose | Process management and innovation | Planning | Reasoning, negotiation, distributed management | Experience, awareness, perception |
| Lower boundary of technical preparation | Qualitative workflow | Casual loop | Objected-oriented programming | Low-tech material |
| Higher boundary of technical preparation | Differential equations | Agent system | High-tech graphic and interaction | |
| Applicable area | All | Staffing decision making, procurement logistics | Staffing decision making, transport, hospital design, network distribution and dispatching | Staffing decision making, supply chain management, network distribution and dispatching |
| Tools | Arena, Simio, Simu8, AnyLogic | Venism, AnyLogic | NetLogo, AnyLogic | Boards, unity |
Games and participatory simulation are particularly useful for training at the tactical level because games help identify productive or counterproductive human actions. The strength of the agent-based method is the modeling and analysis of human behavior [33, 41]. Healthcare logistics are largely characterized by non-rational operative decision making by medical personnel regarding needs of their patients. By modeling decisions at the agent level, it is possible to obtain insight into the reasoning process of decisions being made [42]. By involving these operational experts in participatory simulations, we can assess their perception of processes and healthcare system operations [43]. This effort delivers insight at another level of abstraction than technical, often discrete-event-based, simulations can provide.
Regarding training purposes, agent-based simulation and games are suitable for training negotiation and coordination in logistics, whereas discrete-event simulation and system dynamics can be utilized for reducing the uncertainty of decision-making processes by adding details to the model.
Participatory simulation is valuable for validating various simulators that model complex systems. The advantage of participatory simulation corresponds to the delivery structure of the investigated system, as healthcare logistics is carried out by collaborative efforts in which different professionals, knowledge, and skills work together.
Discrete-event simulation has the lowest requirement of technological preparation and is found to support all areas [26, 44–46]. System dynamics and agent-based simulation might require formal methods and mathematics pertaining to system design, such as differential equations [47], decision theories [48], and game-based approaches [33].
Conclusions
Complex socio-technical systems, such as air traffic controls [49], routinely apply flow and logistical simulations. The studies examined in this review indicate a growing practice of implementing simulation in healthcare settings to create situations in which the non-technical skills of managers, coordinators, and decision makers can be trained and developed. Building on existing concepts from other industries [50], future applications might be hands-on training of teams using gaming and participatory simulation alongside empirical data to create situations for training tricky decision making, for strategic planning, and for exploring the effect of decisions on other parts of the system [51].
Our review yielded many examples of applications in healthcare, indicating that the issues of training of strategic or operational coordination and decision making in healthcare can all be addressed by simulation. The orthogonal simulation techniques are discrete-event simulation, system dynamics, agent-based simulation, game, and participatory simulation. For patient-centric logistics, discrete-event simulation in single-department/unit scenarios is the most dominant form of simulation, the maturity of which takes the lead over other categories by a large margin. As a systems perspective was applied, discrete-event simulation became less popular and was compensated for by system dynamics or hybrid modeling. The literature review showed that tools for logistical simulations vary in this field, with tools such as AnyLogic, Arena, NetLogo, and board games implemented most frequently. This is an extensive study analyzing the growth in the use of simulation in healthcare settings.
Lack of standardization
The number of miscellaneous simulations was significant, although discrete-event simulation, system dynamics, and agent-based simulation were well-established and well-standardized simulation techniques in many software packages. Most of the miscellaneous simulations were custom-made solutions. A focal point of these papers was implementing the modular design of protocols, revealing a lack of standards. Compared with processes in many other industries, healthcare processes are less standardized, and thus, composition of services varies. We believe that much effort could be saved by employing standardization in both healthcare processes and simulation formulism.
Lack of identification for material-centric logistics
In the domain of material-centric logistics, the focus is on inventory management and network distribution. A general lack of articles indicated limited research effort. One reason is that material-centric logistics is not an independent research stream yet—in many cases, the analysis of material-centric logistics is attached to a larger research project pertaining to physical distribution and logistical management.
Lack of complex system modeling and simulation
System dynamics, agent-based simulation, and hybrid modeling were underdeveloped for handling the complexity of social-technical systems. Digital transformation would change many aspects of the human-technology interaction in the provision of health services. A knowledge gap exists between the promise of future delivery of care that abolishes institutional boundaries and the current methods for testing and demonstrating functionalities. To bridge this gap, we require a better understanding of interconnected relationships between care providers and extensions to model individual-level requirements.
Limitations
The review has limitations. The search terms were formulated by the authors. As a result, the data search might not have been comprehensive. To eliminate the risk of omitting important contributions, the search terms combined keywords related to content and scientific methods, respectively. Second, although both journal and conference contributions were considered, the exclusion of abstracts and posters might lead to publication bias according to the Assessment of Multiple Systematic Reviews (AMSTAR) checklist for assessing the quality of systematic reviews. Because the aim of the review was to identify logistical simulations for training and education purposes, the exclusion is understandable for the short contributions that are not able to document the simulation models in a detailed manner. Therefore, publication bias is not prevalent in our literature review. The review only analyzed papers published since 1998. This approach was taken because the growth in the use of healthcare simulations started as Jun et al. surveyed the practical application of discrete-event simulation in healthcare [12], which was noted by Persson and Persson [52]. Therefore, a synthesis of the literature after 1998 should not distort the analysis.
General conclusion
The overview demonstrates that the simulation models available are mainly event-based, which is understandable. The strict regulations and rules associated with the medical field make process simulation particularly suited to handling issues in this area. These perceptions, together with the lack of literature on using agent-based simulation and participatory simulation, suggest a research direction involving the development of ontologies, architectures, and terminologies for their better acceptance in training and education of non-technical skills, with more problem-solving studies performed to demonstrate the corresponding benefits.
It is worth noting that the growth of digitalized healthcare occurs in parallel with the demographic change into an aging society. Currently, digital transformation, provision of homecare, and de-institutionalization are transferring practical applications into the decentralized paradigm. This effort requires coordination between caregivers and stakeholders. Agent-based simulation and participatory simulation can support comprehensive engineering to achieve quality and safety improvements. Therefore, agent-based simulation and participatory simulation are promising approaches for better handling healthcare logistics given current societal trends.
Acknowledgments
Funding
This work is supported by the Stockholm County Council, in the design of the study and collection, analysis, interpretation of data, and writing the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABS
Agent-based simulation
- DES
Discrete-event simulation
- Misc
Miscellaneous
- Mixed
Hybrid simulation
- SD
Systems dynamics
Authors’ contributions
CZ, TG, and SM designed the study and located the articles from the databases. CZ and TG performed the screening process. CZ, TG, SM, KH, and JH analyzed and interpreted the systematic review results. CZ and TG were responsible for writing the paper. KH, JH, and SM were the major contributors for revising the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chen Zhang, Phone: 0765914787, Email: chenzh@kth.se.
Thomas Grandits, Email: grandits@kth.se.
Karin Pukk Härenstam, Email: karin.pukk-harenstam@sll.se.
Jannicke Baalsrud Hauge, Email: jmbh@kth.se.
Sebastiaan Meijer, Email: smeijer@kth.se.
References
- 1.Klein G, Feltovich PJ, Bradshaw JM, Woods DD. Common ground and coordination in joint activity. In: Rouse WB, Boff KR, editors. Organizational simulation. New Jersey: Wiley; 2005. p. 139–84.
- 2.Vincent C, Amalberti R. Safety strategies in hospitals. In: Safer healthcare. Cham: Springer International Publishing. p. 73–91.
- 3.Nemeth CP, Nunnally M, O’Connor MF, Brandwijk M, Kowalsky J, Cook RI. Regularly irregular: how groups reconcile cross-cutting agendas and demand in healthcare. Cogn Tech Work. 2007;9:139–148. doi: 10.1007/s10111-006-0058-4. [DOI] [Google Scholar]
- 4.Macrae C, Draycott T. Delivering high reliability in maternity care: in situ simulation as a source of organisational resilience. Saf Sci. 2016. 10.1016/j.ssci.2016.10.019.
- 5.Crichton M, O’Connor P, Flin R. Safety at the sharp end: a guide to non-technical skills. Hampshire: Ashgate Publishing, Ltd; 2013.
- 6.Dieckmann P, Zeltner LG, Helsø A-M. “Hand-it-on”: an innovative simulation on the relation of non-technical skills to healthcare. Adv Simul. 2016;1:30. doi: 10.1186/s41077-016-0031-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ulmanen P, Szebehely M. From the state to the family or to the market? Consequences of reduced residential eldercare in Sweden: from the state to the family. Int J Soc Welf. 2015;24:81–92. doi: 10.1111/ijsw.12108. [DOI] [Google Scholar]
- 8.Hagihara A, Hasegawa M, Hinohara Y, Abe T, Motoi M. The aging population and future demand for emergency ambulances in Japan. Intern Emerg Med. 2013;8:431–437. doi: 10.1007/s11739-013-0956-4. [DOI] [PubMed] [Google Scholar]
- 9.Kriz WC. Creating effective learning environments and learning organizations through gaming simulation design. Simul Gaming. 2003;34:495–511. doi: 10.1177/1046878103258201. [DOI] [Google Scholar]
- 10.Kriz WC. Types of gaming simulation applications. Simul Gaming. 2017;48:3–7. doi: 10.1177/1046878117689860. [DOI] [Google Scholar]
- 11.Meijer S. The power of sponges: comparing high-tech and low-tech gaming for innovation. Simul Gaming. 2015;46:512–535. doi: 10.1177/1046878115594520. [DOI] [Google Scholar]
- 12.Jun JB, Jacobson SH, Swisher JR. Application of discrete-event simulation in health care clinics: a survey. J Oper Res Soc. 1999;50:109–123. doi: 10.1057/palgrave.jors.2600669. [DOI] [Google Scholar]
- 13.Brailsford SC. Proceedings of the winter simulation conference. 2008. System dynamics: what’s in it for healthcare simulation modelers; pp. 1478–1483. [Google Scholar]
- 14.Koelling P, Schwandt MJ. Proceedings of the winter simulation conference. 2005. Health systems: a dynamic system-benefits from system dynamics; pp. 1321–1327. [Google Scholar]
- 15.Mustafee N, Katsaliaki K, Taylor SJE. Profiling literature in healthcare simulation. Simulation. 2010;86:543–548. doi: 10.1177/0037549709359090. [DOI] [Google Scholar]
- 16.Schaefer JJ, Vanderbilt AA, Cason CL, Bauman EB, Glavin RJ, Lee FW, et al. Literature review: instructional design and pedagogy science in healthcare simulation. Simul Healthc. 2011;6:30–41. doi: 10.1097/SIH.0b013e31822237b4. [DOI] [PubMed] [Google Scholar]
- 17.Nestel D, Groom J, Eikeland-Husebø S, OʼDonnell JM. Simulation for learning and teaching procedural skills: the state of the science. Simul Healthc. 2011;6:10–13. doi: 10.1097/SIH.0b013e318227ce96. [DOI] [PubMed] [Google Scholar]
- 18.DeRienzo CM, Shaw RJ, Meanor P, Lada E, Ferranti J, Tanaka D. A discrete event simulation tool to support and predict hospital and clinic staffing. Health Informatics J. 2016;23:124–133. doi: 10.1177/1460458216628314. [DOI] [PubMed] [Google Scholar]
- 19.Devapriya P, Strömblad CTB, Bailey MD, Frazier S, Bulger J, Kemberling ST, et al. StratBAM: a discrete-event simulation model to support strategic hospital bed capacity decisions. J Med Syst. 2015;39:130. doi: 10.1007/s10916-015-0325-0. [DOI] [PubMed] [Google Scholar]
- 20.Bhattacharjee P, Ray PK. Simulation modelling and analysis of appointment system performance for multiple classes of patients in a hospital: a case study. Oper Res Health Care. 2016;8:71–84. doi: 10.1016/j.orhc.2015.07.005. [DOI] [Google Scholar]
- 21.Vasilakis C, Sobolev BG, Kuramoto L, Levy AR. A simulation study of scheduling clinic appointments in surgical care: individual surgeon versus pooled lists. J Oper Res Soc. 2007;58:202–211. doi: 10.1057/palgrave.jors.2602235. [DOI] [Google Scholar]
- 22.Jørgensen P, Jacobsen P, Poulsen JH. Identifying the potential of changes to blood sample logistics using simulation. Scand J Clin Lab Invest. 2013;73:279–285. doi: 10.3109/00365513.2013.773063. [DOI] [PubMed] [Google Scholar]
- 23.Rashwan W, Ragab MA, Abo-Hamad W, Arisha A. Proceedings of the winter simulation conference. 2013. Bed blockage in Irish hospitals: system dynamics methodology; pp. 3984–3985. [Google Scholar]
- 24.Rashwan W, Abo-Hamad W, Arisha A. A system dynamics view of the acute bed blockage problem in the Irish healthcare system. Eur J Oper Res. 2015;247:276–293. doi: 10.1016/j.ejor.2015.05.043. [DOI] [Google Scholar]
- 25.Brailsford SC, Lattimer VA, Tarnaras P, Turnbull JC. Emergency and on-demand health care: modelling a large complex system. J Oper Res Soc. 2004;55:34–42. doi: 10.1057/palgrave.jors.2601667. [DOI] [Google Scholar]
- 26.Lane DC, Monefeldt C, Rosenhead JV. Looking in the wrong place for healthcare improvements: a system dynamics study of an accident and emergency department. J Oper Res Soc. 2000;51:518–531. doi: 10.1057/palgrave.jors.2600892. [DOI] [Google Scholar]
- 27.Azzi A, Persona A, Sgarbossa F, Bonin M. Drug inventory management and distribution: outsourcing logistics to third-party providers. Strateg Outsourcing Int J. 2013;6:48–64. doi: 10.1108/17538291311316063. [DOI] [Google Scholar]
- 28.Kalton A, Falconer E, Docherty J, Alevras D, Brann D, Johnson K. Multi-agent-based simulation of a complex ecosystem of mental health care. J Med Syst. 2016;40:39. doi: 10.1007/s10916-015-0374-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marcon E, Chaabane S, Sallez Y, Bonte T, Trentesaux D. A multi-agent system based on reactive decision rules for solving the caregiver routing problem in home health care. Simul Model Pract Theory. 2017;74:134–151. doi: 10.1016/j.simpat.2017.03.006. [DOI] [Google Scholar]
- 30.Jetly G, Rossetti CL, Handfield R. A multi-agent simulation of the pharmaceutical supply chain. J Simul. 2012;6:215–226. doi: 10.1057/jos.2011.26. [DOI] [Google Scholar]
- 31.Escudero-Marin P, Pidd M. Proceedings of the winter simulation conference. 2011. Using ABMS to simulate emergency departments; pp. 1239–1250. [Google Scholar]
- 32.Mustafee N, Katsaliaki K. Proceedings of the winter simulation conference. 2010. The blood supply game; pp. 327–338. [Google Scholar]
- 33.Katsaliaki K, Mustafee N, Kumar S. A game-based approach towards facilitating decision making for perishable products: an example of blood supply chain. Expert Syst Appl. 2014;41:4043–4059. doi: 10.1016/j.eswa.2013.12.038. [DOI] [Google Scholar]
- 34.Basole RC, Bodner DA, Rouse WB. Healthcare management through organizational simulation. Decis Support Syst. 2013;55:552–563. doi: 10.1016/j.dss.2012.10.012. [DOI] [Google Scholar]
- 35.Mattarelli E, Fadel KJ, Weisband SP. Proceedings of conference on human factors in computing systems. 2006. Design of a role-playing game to study the trajectories of health care workers in an operating room; pp. 1091–1096. [Google Scholar]
- 36.Brailsford SC, Desai SM, Viana J. Proceedings of the winter simulation conference. 2010. Towards the holy grail: combining system dynamics and discrete-event simulation in healthcare; pp. 2293–2303. [Google Scholar]
- 37.Zulkepli J, Eldabi T, Mustafee N. Proceedings of the winter simulation conference. 2012. Hybrid simulation for modelling large systems: an example of integrated care model. [Google Scholar]
- 38.zen MB, Zabawa J. Proceedings of the winter simulation conference. 2016. Modeling healthcare demand using a hybrid simulation approach; pp. 1535–1546. [Google Scholar]
- 39.Shah N. Pharmaceutical supply chains: key issues and strategies for optimisation. Comput Chem Eng. 2004;28:929–941. doi: 10.1016/j.compchemeng.2003.09.022. [DOI] [Google Scholar]
- 40.Gaba DM. Adapting space science methods for describing and planning research in simulation in healthcare: science traceability and decadal surveys. Simul Healthc. 2012;7:27–31. doi: 10.1097/SIH.0b013e31823ca729. [DOI] [PubMed] [Google Scholar]
- 41.Liu Z, Rexachs D, Epelde F, Luque E. An agent-based model for quantitatively analyzing and predicting the complex behavior of emergency departments. J Comput Sci. 2017;21(Suppl C):11–23. doi: 10.1016/j.jocs.2017.05.015. [DOI] [Google Scholar]
- 42.Kolb EMW, Schoening S, Peck J, Lee T. Proceedings of the winter simulation conference. 2008. Reducing emergency department overcrowding: five patient buffer concepts in comparison; pp. 1516–1525. [Google Scholar]
- 43.Kotiadis K, Tako AA, Vasilakis C. A participative and facilitative conceptual modelling framework for discrete event simulation studies in healthcare. J Oper Res Soc. 2014;65:197–213. doi: 10.1057/jors.2012.176. [DOI] [Google Scholar]
- 44.Demir E, Gunal MM, Southern D. Demand and capacity modelling for acute services using discrete event simulation. Health Syst. 2017;6:33–40. doi: 10.1057/hs.2016.1. [DOI] [Google Scholar]
- 45.Reynolds M, Vasilakis C, McLeod M, Barber N, Mounsey A, Newton S, et al. Using discrete event simulation to design a more efficient hospital pharmacy for outpatients. Health Care Manag Sci. 2011;14:223–236. doi: 10.1007/s10729-011-9151-1. [DOI] [PubMed] [Google Scholar]
- 46.Pehlivan C, Augusto V, Xie X. Proceedings of the winter simulation conference. 2013. Admission control in a pure loss healthcare network: MDP and DES approach; pp. 54–65. [Google Scholar]
- 47.Medeiros DJ, Swenson E, DeFlitch C. Proceedings of the winter simulation conference. 2008. Improving patient flow in a hospital emergency department; pp. 1526–1531. [Google Scholar]
- 48.Ferrin DM, Miller MJ, McBroom DL. Proceedings of the winter simulation conference. 2007. Maximizing hospital finanacial impact and emergency department throughput with simulation; pp. 1566–1573. [Google Scholar]
- 49.Dehlendorff C, Kulahci M, Andersen KK. Designing simulation experiments with controllable and uncontrollable factors for applications in healthcare. Appl Stat. 2011;60:31–49. [Google Scholar]
- 50.Duguay C, Chetouane F. Modeling and improving emergency department systems using discrete event simulation. Simulation. 2007;83:311–320. doi: 10.1177/0037549707083111. [DOI] [Google Scholar]
- 51.Kittipittayakorn C, Ying K-C. Using the integration of discrete event and agent-based simulation to enhance outpatient service quality in an orthopedic department. J Healthc Eng. 2016;2016. [DOI] [PMC free article] [PubMed]
- 52.Persson MJ, Persson JA. Analysing management policies for operating room planning using simulation. Health Care Manag Sci. 2010;13:182–191. doi: 10.1007/s10729-009-9122-y. [DOI] [PubMed] [Google Scholar]
- 53.Guo M, Wagner M, West C. Proceedings of the winter simulation conference. 2004. Outpatient clinic scheduling—a simulation approach; pp. 1981–1987. [Google Scholar]
- 54.Wijewickrama A, Takakuwa S. Proceedings of the winter simulation conference. 2005. Simulation analysis of appointment scheduling in an outpatient department of internal medicine; pp. 2264–2273. [Google Scholar]
- 55.Johansson B, Jain S, Montoya-Torres J, Hngan J. Proceedings of the winter simulation conference. 2010. Integrating balanced scorecard and simulation modeling to improve emergency department performance in Irish hospitals; pp. 2340–2351. [Google Scholar]
- 56.Lin Y, Zhang J. Proceedings of the annual conference on genetic and evolutionary computation. 2011. An ant colony optimization approach for efficient admission scheduling of elective inpatients; pp. 15–16. [Google Scholar]
- 57.Helm JE, AhmadBeygi S, Van Oyen MP. Design and analysis of hospital admission control for operational effectiveness. Prod Oper Manag. 2011;20:359–374. doi: 10.1111/j.1937-5956.2011.01231.x. [DOI] [Google Scholar]
- 58.Yokouchi M, Aoki S, Sang H, Zhao R, Takakuwa S. Proceedings of the winter simulation conference. 2012. Operations analysis and appointment scheduling for an outpatient chemotherapy department. [Google Scholar]
- 59.Khurma N, Salamati F, Pasek ZJ. Proceedings of the winter simulation conference. 2013. Simulation of patient discharge process and its improvement; pp. 2452–2462. [Google Scholar]
- 60.Kooij R, Mes MRK, Hans EW. Proceedings of the winter simulation conference. 2014. Simulation framework to analyze operating room release mechanisms; pp. 1144–1155. [Google Scholar]
- 61.Huggins A, Claudio D, Waliullah M. Proceedings of the winter simulation conference. 2014. A detailed simulation model of an infusion treatment center; pp. 1198–1209. [Google Scholar]
- 62.Prodel M, Augusto V, Xie X. Proceedings of the winter simulation conference. 2014. Hospitalization admission control of emergency patients using markovian decision processes and discrete event simulation; pp. 1433–1444. [Google Scholar]
- 63.Giesen E, Ketter W, Zuidwijk R. Dynamic agent-based scheduling of treatments: evidence from the Dutch youth health care sector. In: Müller JP, Ketter W, Kaminka G, Wagner G, Bulling N, editors. Multiagent system technologies. Cham: Springer International Publishing; 2015. pp. 173–199. [Google Scholar]
- 64.Chen Y, Kuo YH, Balasubramanian H, Wen C. Proceedings of the winter simulation conference. 2015. Using simulation to examine appointment overbooking schemes for a medical imaging center; pp. 1307–1318. [Google Scholar]
- 65.Crowe S, Vasilakis C, Gallivan S, Bull C, Fenton M. Proceedings of the winter simulation conference. 2015. Informing the management of pediatric heart transplant waiting lists: complementary use of simulation and analytical modeling; pp. 1654–1665. [Google Scholar]
- 66.Chen P-S, Robielos RAC, Palaña PKVC, Valencia PLL, GY-H C. Scheduling patients’ appointments: allocation of healthcare service using simulation optimization. J Healthc Eng. 2015;6:259–280. doi: 10.1260/2040-2295.6.2.259. [DOI] [PubMed] [Google Scholar]
- 67.Kim S-H, Chan CW, Olivares M, Escobar G. ICU admission control: an empirical study of capacity allocation and its implication for patient outcomes. Manag Sci. 2015;61:19–38. doi: 10.1287/mnsc.2014.2057. [DOI] [Google Scholar]
- 68.Khanna S, Boyle J, Good N, Bell A, Lind J. Analysing the emergency department patient journey: discovery of bottlenecks to emergency department patient flow. Emerg Med Australas. 2017;29:18–23. doi: 10.1111/1742-6723.12693. [DOI] [PubMed] [Google Scholar]
- 69.Kim BBJ, Delbridge TR, Kendrick DB. Adjusting patients streaming initiated by a wait time threshold in emergency department for minimizing opportunity cost. Int J Health Care Qual Assur. 2017;30:516–527. doi: 10.1108/IJHCQA-10-2016-0155. [DOI] [PubMed] [Google Scholar]
- 70.Ozcan YA, Tànfani E, Testi A. Improving the performance of surgery-based clinical pathways: a simulation-optimization approach. Health Care Manag Sci. 2017;20:1–15. doi: 10.1007/s10729-016-9371-5. [DOI] [PubMed] [Google Scholar]
- 71.Bozzetto M, Rota S, Vigo V, Casucci F, Lomonte C, Morale W, et al. Clinical use of computational modeling for surgical planning of arteriovenous fistula for hemodialysis. BMC Med Inform Decis Mak. 2017;17:26. doi: 10.1186/s12911-017-0420-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vile JL, Allkins E, Frankish J, Garland S, Mizen P, Williams JE. Modelling patient flow in an emergency department to better understand demand management strategies. J Simul. 2017;11:115–127. doi: 10.1057/s41273-016-0004-2. [DOI] [Google Scholar]
- 73.Demir E, Southern D. Enabling better management of patients: discrete event simulation combined with the STAR approach. J Oper Res Soc. 2017;68:577–590. doi: 10.1057/s41274-016-0029-y. [DOI] [Google Scholar]
- 74.Chepenik L, Pinker E. The impact of increasing staff resources on patient flow in a psychiatric emergency service. Psychiatr Serv. 2017;68:470–475. doi: 10.1176/appi.ps.201600202. [DOI] [PubMed] [Google Scholar]
- 75.Saltzman R, Roeder T, Lambton J, Param L, Frost B, Fernandes R. The impact of a discharge holding area on the throughput of a pediatric unit. Serv Sci. 2017;9:121–135. doi: 10.1287/serv.2016.0167. [DOI] [Google Scholar]
- 76.Toth DJA, Khader K, Slayton RB, Kallen AJ, Gundlapalli AV, O’Hagan JJ, et al. The potential for interventions in a long-term acute care hospital to reduce transmission of carbapenem-resistant enterobacteriaceae in affiliated healthcare facilities. Clin Infect Dis. 2017;65:581–587. doi: 10.1093/cid/cix370. [DOI] [PubMed] [Google Scholar]
- 77.Steward D, Glass TF, Ferrand YB. Simulation-based design of ed operations with care streams to optimize care delivery and reduce length of stay in the emergency department. J Med Syst. 2017;41:162. doi: 10.1007/s10916-017-0804-6. [DOI] [PubMed] [Google Scholar]
- 78.Tako AA, Kotiadis K. PartiSim: a multi-methodology framework to support facilitated simulation modelling in healthcare. Eur J Oper Res. 2015;244:555–564. doi: 10.1016/j.ejor.2015.01.046. [DOI] [Google Scholar]
- 79.Monks T, Pearn K, Allen M. Proceedings of the winter simulation conference. 2015. Simulation of stroke care systems; pp. 1391–1402. [Google Scholar]
- 80.Djanatliev A, Meier F. Proceedings of the winter simulation conference. 2016. Hospital processes within an integrated system view: a hybrid simulation approach; pp. 1364–1375. [Google Scholar]
- 81.Alahäivälä T, Oinas-Kukkonen H. Understanding persuasion contexts in health gamification: a systematic analysis of gamified health behavior change support systems literature. Int J Med Inform. 2016;96:62–70. doi: 10.1016/j.ijmedinf.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 82.Zhong X, Lee HK, Li J. From production systems to health care delivery systems: a retrospective look on similarities, difficulties and opportunities. Int J Prod Res. 2017;55:4212–4227. doi: 10.1080/00207543.2016.1277276. [DOI] [Google Scholar]
- 83.Lim ME, Worster A, Goeree R, Tarride J-É. Simulating an emergency department: the importance of modeling the interactions between physicians and delegates in a discrete event simulation. BMC Med Inform Decis Mak. 2013;13:59. doi: 10.1186/1472-6947-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vanderby S, Carter MW. An evaluation of the applicability of system dynamics to patient flow modelling. J Oper Res Soc. 2010;61:1572–1581. doi: 10.1057/jors.2009.150. [DOI] [Google Scholar]
- 85.Chockalingam A, Jayakumar K, Lawley MA. Proceedings of the winter simulation conference. 2010. A stochastic control approach to avoiding emergency department overcrowding; pp. 2399–2411. [Google Scholar]
- 86.Djanatliev A, German R. Proceedings of the winter simulation conference. 2013. Prospective healthcare decision-making by combined system dynamics, discrete-event and agent-based simulation; pp. 270–281. [Google Scholar]
- 87.Wolstenholme E. A patient flow perspective of U.K. health services: exploring the case for new “intermediate care” initiatives. Syst Dyn Rev. 1999;15:253–271. doi: 10.1002/(SICI)1099-1727(199923)15:3<253::AID-SDR172>3.0.CO;2-P. [DOI] [Google Scholar]
- 88.Jansen FJA, Etman LFP, Rooda JE, Adan IJBF. Proceedings of the winter simulation conference. 2012. Aggregate simulation modeling of an MRI department using effective process times. [Google Scholar]
- 89.Zambrano F, Concha P, Ramis F, Neriz L, Bull M, Veloz P, et al. Proceedings of the winter simulation conference. 2016. Improving patient access to a public hospital complex using agent simulation; pp. 1277–1288. [Google Scholar]
- 90.Lamé G, Jouini O, Cardinal JS-L, Carvalho M, Tournigand C, Wolkenstein P. Proceedings of the winter simulation conference. 2016. Patient-hospital communication: a platform to improve outpatient chemotherapy; pp. 2099–2110. [Google Scholar]
- 91.April J, Better M, Glover F, Kelly J, Laguna M. Proceedings of the winter simulation conference. 2006. Enhancing business process management with simulation optimization; pp. 642–649. [Google Scholar]
- 92.Bowers J, Ghattas M, Mould G. Exploring alternative routes to realising the benefits of simulation in healthcare. J Oper Res Soc. 2012;63:1457–1466. doi: 10.1057/jors.2011.127. [DOI] [Google Scholar]
- 93.Chavis J, Cochran AL, Kocher KE, Washington VN, Zayas-Cabán G. Proceedings of the winter simulation conference. 2016. A simulation model of patient flow through the emergency department to determine the impact of a short stay unit on hospital congestion; pp. 1982–1993. [Google Scholar]
- 94.Patvivatsiri L. Proceedings of the winter simulation conference. 2006. A simulation model for bioterrorism preparedness in an emergency room; pp. 501–508. [Google Scholar]
- 95.Comas M, Castells X, Hoffmeister L, Román R, Cots F, Mar J, et al. Discrete-event simulation applied to analysis of waiting lists: evaluation of a prioritization system for cataract surgery. Value Health. 2008;11:1203–1213. doi: 10.1111/j.1524-4733.2008.00322.x. [DOI] [PubMed] [Google Scholar]
- 96.Kuhl ME. Proceedings of the winter simulation conference. 2012. A simulation study of patient flow for day of surgery admission. [Google Scholar]
- 97.Miller M, Ferrin D, Shahi N. Proceedings of the winter simulation conference. 2009. Estimating patient surge impact on boarding time in several regional emergency departments; pp. 1906–1915. [Google Scholar]
- 98.Roure M, Halley Q, Augusto V. Proceedings of the winter simulation conference. 2015. Modelling and simulation of an outpatient surgery unit; pp. 1525–1536. [Google Scholar]
- 99.Doğan NÖ, Unutulmaz O. Lean production in healthcare: a simulation-based value stream mapping in the physical therapy and rehabilitation department of a public hospital. Total Qual Manag Bus Excell. 2016;27:64–80. doi: 10.1080/14783363.2014.945312. [DOI] [Google Scholar]
- 100.Batarseh OG, Goldlust EJ, Day TE. Proceedings of the winter simulations conference. 2013. SysML for conceptual modeling and simulation for analysis: a case example of a highly granular model of an emergency department; pp. 2398–2409. [Google Scholar]
- 101.Schonherr O, Rose O. Proceedings of the winter simulation conference. 2011. A general model description for discrete processes; pp. 2201–2213. [Google Scholar]
- 102.Southard PB, Chandra C, Kumar S. RFID in healthcare: a six sigma DMAIC and simulation case study. Int J Health Care Qual Assur. 2012;25:291–321. doi: 10.1108/09526861211221491. [DOI] [PubMed] [Google Scholar]
- 103.Santibáñez P, Chow VS, French J, Puterman ML, Tyldesley S. Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Manag Sci. 2009;12:392–407. doi: 10.1007/s10729-009-9103-1. [DOI] [PubMed] [Google Scholar]
- 104.Konrad RA, Lawley MA. Proceedings of the winter simulation conference. 2009. Input modeling for hospital simulation models using electronic messages; pp. 134–147. [Google Scholar]
- 105.Hagtvedt R, Ferguson M, Griffin P, Jones GT, Keskinocak P. Proceedings of the winter simulation conference. 2009. Cooperative strategies to reduce ambulance diversion; pp. 1861–1874. [Google Scholar]
- 106.Maull RS, Smart PA, Harris A, AA-F K. An evaluation of ‘fast track’ in A&E: a discrete event simulation approach. Serv Ind J. 2009;29:923–941. doi: 10.1080/02642060902749534. [DOI] [Google Scholar]
- 107.Roberts SD. Proceedings of the winter simulation conference. 2011. Tutorial on the simulation of healthcare systems; pp. 1408–1419. [Google Scholar]
- 108.Hosseini S, Jannat S. Proceedings of the winter simulation conference. 2015. Discrete event simulation technique for evaluating performance of oncology department: a case study; pp. 1343–1354. [Google Scholar]
- 109.Levin S, Garifullin M. Simulating wait time in healthcare: accounting for transition process variability using survival analyses. In: Proceedings of the winter simulation conference. 2015. p. 1252–60.
- 110.Levin S, Dittus R, Aronsky D, Weinger M, France D. Evaluating the effects of increasing surgical volume on emergency department patient access. Qual Saf Health Care. 2011;20:146–152. doi: 10.1136/bmjqs.2008.030007. [DOI] [PubMed] [Google Scholar]
- 111.Mahapatra S, Koelling CP, Patvivatsiri L, Fraticelli B, Eitel D, Grove L. Proceedings of the winter simulation conference. 2003. Pairing emergency severity index5-level triage data with computer aided system design to improve emergency department access and throughput; pp. 1917–1925. [Google Scholar]
- 112.McClean S, Barton M, Garg L, Fullerton K. A modeling framework that combines Markov models and discrete-event simulation for stroke patient care. ACM Trans Model Comput Simul. 2011;21:25. doi: 10.1145/2000494.2000498. [DOI] [Google Scholar]
- 113.Reindl S, Mönch L, Mönch M, Scheider A. Proceedings of the winter simulation conference. 2009. Modeling and simulation of cataract surgery processes; pp. 1937–1945. [Google Scholar]
- 114.Takakuwa S, Wijewickrama A. Proceedings of the winter simulation conference. 2008. Optimizing staffing schedule in light of patient satisfaction for the whole outpatient hospital ward; pp. 1500–1508. [Google Scholar]
- 115.Takakuwa S, Katagiri D. Proceedings of the winter simulation conference. 2007. Modeling of patient flows in a large-scale outpatient hospital ward by making use of electronic medical records; pp. 1523–1531. [Google Scholar]
- 116.Takakuwa S, Shiozaki H. Proceedings of the winter simulation conference. 2004. Functional analysis for operating emergency department of a general hospital; pp. 2003–2011. [Google Scholar]
- 117.Coelli FC, Ferreira RB, Almeida RMVR, Pereira WCA. Computer simulation and discrete-event models in the analysis of a mammography clinic patient flow. Comput Methods Prog Biomed. 2007;87:201–207. doi: 10.1016/j.cmpb.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 118.Rohleder TR, Lewkonia P, Bischak DP, Duffy P, Hendijani R. Using simulation modeling to improve patient flow at an outpatient orthopedic clinic. Health Care Manag Sci. 2011;14:135–145. doi: 10.1007/s10729-010-9145-4. [DOI] [PubMed] [Google Scholar]
- 119.Wang T, Guinet A, Belaidi A, Besombes B. Modelling and simulation of emergency services with ARIS and Arena. Case study: the emergency department of Saint Joseph and Saint Luc Hospital. Prod Plan Control. 2009;20:484–495. doi: 10.1080/09537280902938605. [DOI] [Google Scholar]
- 120.Abo-Hamad W, Arisha A. Proceedings of the winter simulation conference. 2012. Multi-criteria framework for emergency department in Irish hospital. [Google Scholar]
- 121.Abo-Hamad W, Arisha A. Simulation-based framework to improve patient experience in an emergency department. Eur J Oper Res. 2013;224:154–166. doi: 10.1016/j.ejor.2012.07.028. [DOI] [Google Scholar]
- 122.Wang Y, Lee LH, Chew EP, Lam SSW, Low SK, Ong MEH, et al. Proceedings of the winter simulation conference. 2015. Multi-objective optimization for a hospital inpatient flow process via discrete event simulation; pp. 3622–3631. [Google Scholar]
- 123.Zhao Y, Peng Q, Strome T, Weldon E, Zhang M, Chochinov A. Bottleneck detection for improvement of emergency department efficiency. Bus Process Manag J. 2015;21:564–585. doi: 10.1108/BPMJ-06-2014-0060. [DOI] [Google Scholar]
- 124.Rashwan W, Habib H, Arisha A, Courtney G, Kennelly S. Proceedings of the winter simulation conference. 2016. An integrated approach of multi-objective optimization model for evaluating new supporting program in Irish hospitals; pp. 1904–1915. [Google Scholar]
- 125.Rashwan W, Arisha A. Proceedings of the winter simulation conference. 2015. Modeling behavior of nurses in clinical medical unit in university hospital: burnout implications; pp. 3880–3891. [Google Scholar]
- 126.Bair AE, Song WT, Chen Y, Morris BA. Proceedings of the spring computer simulation conference. 2009. The impact of inpatient boarding on emergency department crowding: a discrete-event simulation study. [Google Scholar]
- 127.Bountourelis T, Eckman D, Luangkesorn L, Schaefer A, Nabors SG, Clermont G. Proceedings of the winter simulation conference. 2012. Sensitivity analysis of an ICU simulation model. [Google Scholar]
- 128.Hamrock E, Paige K, Parks J, Scheulen J, Levin S. Discrete event simulation for healthcare organizations: a tool for decision making. J Healthc Manag. 2013;58:110–124. doi: 10.1097/00115514-201303000-00007. [DOI] [PubMed] [Google Scholar]
- 129.Centeno MA, Albacete C, Terzano DO, Carrillo M, Ogazon T. Proceedings of the winter simulation conference. 2000. Project and process improvements in healthcare organizations: a simulation study of the radiology department at JMH; pp. 1978–1984. [Google Scholar]
- 130.Ramis FJ, Palma JL, Baesler FF. Proceedings of the winter simulation conference. 2001. The use of simulation for process improvement at an ambulatory surgery center; pp. 1401–1404. [Google Scholar]
- 131.Pasin F, Jobin MH, Cordeau JF. An application of simulation to analyse resource sharing organisations among health-care organisations. Int J Oper Prod Manag. 2002;22:381–393. doi: 10.1108/01443570210420395. [DOI] [Google Scholar]
- 132.Wiinamaki A, Dronzek R. Proceedings of the winter simulation conference. 2003. Using simulation in the architectural concept phase of an emergency department design; pp. 1912–1916. [Google Scholar]
- 133.Samaha S, Armel WS, Starks DW. Proceedings of the winter simulation conference. 2003. The use of simulation to reduce the length of stay in an emergency department; pp. 1907–1911. [Google Scholar]
- 134.Blasak RE, Starks DW, Armel WS, Hayduk MC. Proceedings of the winter simulation conference. 2003. Healthcare process analysis: the use of simulation to evaluate hospital operations between the emergency department and a medical telemetry unit; pp. 1887–1893. [Google Scholar]
- 135.Baesler FF, Jahnsen HE, DaCosta M. Proceedings of the winter simulation conference. 2003. The use of simulation and design of experiments for estimating maximum capacity in an emergency room; pp. 1903–1906. [Google Scholar]
- 136.Centeno MA, Giachetti R, Linn R, Ismail AM. Proceedings of the winter simulation conference. 2003. A simulation-ilp based tool for scheduling ER staff; pp. 1930–1938. [Google Scholar]
- 137.Schenk JR, Huang D, Zheng N, Allen TT. Proceedings of the winter simulation conference. 2005. Multiple fidelity simulation optimization of hospital performance under high consequence event scenarios; pp. 936–942. [Google Scholar]
- 138.Spry CW, Lawley MA. Proceedings of the winter simulation conference. 2005. Evaluating hospital pharmacy staffing and work scheduling using simulation; pp. 2256–2263. [Google Scholar]
- 139.Hay AM, Valentin EC, Bijlsma RA. Proceedings of the winter simulation conference. 2006. Modeling emergency care in hospitals: a paradox-the patient should not drive the process; pp. 439–445. [Google Scholar]
- 140.Wijewickrama AKA, Takakuwa S. Proceedings of the winter simulation conference. 2006. Simulation analysis of an outpatient department of internal medicine in a university hospital; pp. 425–432. [Google Scholar]
- 141.Ballard SM, Kuhl ME. Proceedings of the winter simulation conference. 2006. The use of simulation to determine maximum capacity in the surgical suite operating room; pp. 433–438. [Google Scholar]
- 142.Taaffe K, Johnson M, Steinmann D. Proceedings of the winter simulation conference. 2006. Improving hospital evacuation planning using simulation; pp. 509–515. [Google Scholar]
- 143.VanBerkel PT, Blake JT. A comprehensive simulation for wait time reduction and capacity planning applied in general surgery. Health Care Manag Sci. 2007;10:373–385. doi: 10.1007/s10729-007-9035-6. [DOI] [PubMed] [Google Scholar]
- 144.Rico F, Salari E, Centeno G. Proceedings of the winter simulation conference. 2007. Emergency departments nurse allocation to face a pandemic influenza outbreak; pp. 1292–1298. [Google Scholar]
- 145.Miller M, Ferrin D, Ashby M, Flynn T, Shahi N. Proceedings of the winter simulation conference. 2007. Merging six emergency departments into one: a simulation approach; pp. 1574–1578. [Google Scholar]
- 146.Patvivatsiri L, Montes EJ, Jr, Xi O. Proceedings of the winter simulation conference. 2007. Modeling bioterrorism preparedness with simulation in rural healthcare system; pp. 1155–1160. [Google Scholar]
- 147.Paul JA, Hariharan G. Proceedings of the winter simulation conference. 2007. Hospital capacity planning for efficient disaster mitigation during a bioterrorist attack; pp. 1139–1147. [Google Scholar]
- 148.Song WT, Bair AE, Chih M. Proceedings of the winter simulation conference. 2008. A simulation study on the impact of physician starting time in a physical examination service; pp. 1553–1562. [Google Scholar]
- 149.Protil RM, Stroparo JR, Bichinho GL. Proceedings of the winter simulation conference. 2008. Applying computer simulation to increase the surgical center occupation rate at a university hospital in Curitiba-Brazil; pp. 1609–1616. [Google Scholar]
- 150.Nielsen AL, Hilwig H, Kissoon N, Teelucksingh S. Discrete event simulation as a tool in optimization of a professional complex adaptive system. Stud Health Technol Inform. 2008;136:247. [PubMed] [Google Scholar]
- 151.Huschka TR, Denton BT, Narr BJ, Thompson AC. Proceedings of the winter simulation conference. 2008. Using simulation in the implementation of an outpatient procedure center; pp. 1547–1552. [Google Scholar]
- 152.Oddoye JP, Jones DF, Tamiz M, Schmidt P. Combining simulation and goal programming for healthcare planning in a medical assessment unit. Eur J Oper Res. 2009;193:250–261. doi: 10.1016/j.ejor.2007.10.029. [DOI] [Google Scholar]
- 153.Raunak M, Osterweil L, Wise A, Clarke L, Henneman P. Proceedings of the international conference on software engineering. 2009. Simulating patient flow through an emergency department using process-driven discrete event simulation; pp. 73–83. [Google Scholar]
- 154.Efe K, Raghavan V, Choubey S. Proceedings of the winter simulation conference. 2009. Simulation modeling movable hospital assets managed with RFID sensors; pp. 2054–2064. [Google Scholar]
- 155.Ferrand Y, Magazine M, Rao U. Proceedings of the winter simulation conference. 2010. Comparing two operating-room-allocation policies for elective and emergency surgeries; pp. 2364–2374. [Google Scholar]
- 156.Zeltyn S, Marmor YN, Mandelbaum A, Carmeli B, Greenshpan O, Mesika Y, et al. Simulation-based models of emergency departments: operational, tactical, and strategic staffing. ACM Trans Model Comput Simul. 2011;21:24. doi: 10.1145/2000494.2000497. [DOI] [Google Scholar]
- 157.Weng S-J, Tsai B-S, Wang L-M, Chang C-Y, Gotcher D. Proceedings of the winter simulation conference. 2011. Using simulation and data envelopment analysis in optimal healthcare efficiency allocations; pp. 1295–1305. [Google Scholar]
- 158.Geis GL, Pio B, Pendergrass TL, Moyer MR, Patterson MD. Simulation to assess the safety of new healthcare teams and new facilities. Simul Healthc. 2011;6:125. doi: 10.1097/SIH.0b013e31820dff30. [DOI] [PubMed] [Google Scholar]
- 159.Cabrera E, Luque E, Taboada M, Epelde F, Iglesias ML. Proceedings of the winter simulation conference. 2012. ABMS optimization for emergency departments. [Google Scholar]
- 160.Kuo Y-H, Leung JM, Graham CA. Proceedings of the winter simulation conference. 2012. Simulation with data scarcity: developing a simulation model of a hospital emergency department. [Google Scholar]
- 161.Mustafee N, Lyons T, Rees P, Davies L, Ramsey M, Williams MD. Proceedings of the winter simulation conference. 2012. Planning of bed capacities in specialized and integrated care units: incorporating bed blockers in a simulation of surgical throughput. [Google Scholar]
- 162.Rashwan W, Ragab M, Abo-Hamad W, Arisha A. Proceedings of the winter simulation conference. 2013. Evaluating policy interventions for delayed discharge: a system dynamics approach; pp. 2463–2474. [Google Scholar]
- 163.Shin SY, Balasubramanian H, Brun Y, Henneman PL, Osterweil LJ. Proceedings of the international workshop on software engineering in health care. 2013. Resource scheduling through resource-aware simulation of emergency departments; pp. 64–70. [Google Scholar]
- 164.Amyot D. Proceedings of the summer computer simulation conference. 2013. Real-time simulations to support operational decision making in healthcare; pp. 64–70. [Google Scholar]
- 165.Verma S, Gupta A. Proceedings of the winter simulation conference. 2013. Improving services in outdoor patient departments by focusing on process parameters: a simulation approach; pp. 2250–2261. [Google Scholar]
- 166.Yaylali E, Simmons J, Taheri J. Systems engineering methods for enhancing the value stream in public health preparedness: the role of Markov models, simulation, and optimization. Public Health Rep. 2014;129:145–153. doi: 10.1177/00333549141296S419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Pinto LR, Perpétuo IHO, de Campos FCC, Ribeiro YCNMB. Proceedings of the winter simulation conference. 2014. Analysis of hospital bed capacity via queuing theory and simulation; pp. 1281–1292. [Google Scholar]
- 168.Ozen A, Balasubramanian H, Samra P, Ehresman M, Li H, Fairman T, et al. Proceedings of the winter simulation conference. 2014. The impact of hourly discharge rates and prioritization on timely access to inpatient beds; pp. 1210–1220. [Google Scholar]
- 169.Kalbasi A, Krishnamurthy D, Rolia J, Singhal S. Proceedings of the winter simulation conference. 2014. Simulation by example for complex systems; pp. 974–985. [Google Scholar]
- 170.Wurzer G, Lorenz WE. Proceedings of the symposium on simulation for architecture and urban design. 2014. Causality in hospital simulation based on utilization chains. [Google Scholar]
- 171.Aboueljinane L, Sahin E, Jemai Z, Marty J. A simulation study to improve the performance of an emergency medical service: application to the French Val-de-Marne department. Simul Model Pract Theory. 2014;47:46–59. doi: 10.1016/j.simpat.2014.05.007. [DOI] [Google Scholar]
- 172.Ghanes K, Jouini O, Jemai Z, Wargon M, Hellmann R, Thomas V, et al. Proceedings of the winter simulation conference. 2014. A comprehensive simulation modeling of an emergency department: a case study for simulation optimization of staffing levels; pp. 1421–1432. [Google Scholar]
- 173.Zhou Z, Wang Y, Li L. Proceedings of the IEEE international conference on networking, sensing and control. 2014. Process mining based modeling and analysis of workflows in clinical care—a case study in a Chicago outpatient clinic; pp. 590–595. [Google Scholar]
- 174.van Buuren M, Kommer GJ, van der Mei R, Bhulai S. Proceedings of the winter simulation conference. 2015. A simulation model for emergency medical services call centers; pp. 844–855. [Google Scholar]
- 175.Franck T, Augusto V, Xie X, Gonthier R, Achour E. Proceedings of the winter simulation conference. 2015. Performance evaluation of an integrated care for geriatric departments using discrete-event simulation; pp. 1331–1342. [Google Scholar]
- 176.Ghanes K, Wargon M, Jouini O, Jemai Z, Diakogiannis A, Hellmann R, et al. Simulation-based optimization of staffing levels in an emergency department. Simulation. 2015;91:942–953. doi: 10.1177/0037549715606808. [DOI] [Google Scholar]
- 177.Carmen R, Defraeye M, Van Nieuwenhuyse I. A decision support system for capacity planning in emergency departments. Int J Simul Model. 2015;14:299–312. doi: 10.2507/IJSIMM14(2)10.308. [DOI] [Google Scholar]
- 178.dos Santos M, Quintal RS, da PAC, Gomes CFS. Simulation of operation of an integrated information for emergency pre-hospital care in Rio de Janeiro municipality. Procedia Comput Sci. 2015;55:931–938. doi: 10.1016/j.procs.2015.07.111. [DOI] [Google Scholar]
- 179.Agor J, McKenzie K, Ozaltin O, Mayorga M, Parikh RS, Huddleston J. Proceedings of the winter simulation conference. 2016. Simulation of triaging patients into an internal medicine department to validate the use of an optimization based workload score; pp. 3708–3709. [Google Scholar]
- 180.Lee W, Shin K, Lee H-R, Shin H, Lee T. Proceedings of the winter simulation conference. 2016. A structured approach for constructing high fidelity ED simulation; pp. 1950–1960. [Google Scholar]
- 181.Pujowidianto NA, Lee LH, Pedrielli G, Chen C-H, Li H. Proceedings of the winter simulation conference. 2016. Constrained optimizaton for hospital bed allocation via discrete event simulation with nested partitions; pp. 1916–1925. [Google Scholar]
- 182.Augusto V, Xie X, Prodel M, Jouaneton B, Lamarsalle L. Proceedings of the winter simulation conference. 2016. Evaluation of discovered clinical pathways using process mining and joint agent-based discrete-event simulation; pp. 2135–2146. [Google Scholar]
- 183.Tiwari V, Sandberg WS. Proceedings of the winter simulation conference. 2016. Perioperative bed capacity planning guided by theory of constraints; pp. 1894–1903. [Google Scholar]
- 184.Thorwarth M, Rashwan W, Arisha A. An analytical representation of flexible resource allocation in hospitals. Flex Serv Manuf J. 2016;28:148–165. doi: 10.1007/s10696-015-9216-4. [DOI] [Google Scholar]
- 185.Kuo Y-H, Rado O, Lupia B, Leung JMY, Graham CA. Improving the efficiency of a hospital emergency department: a simulation study with indirectly imputed service-time distributions. Flex Serv Manuf J. 2016;28:120–147. doi: 10.1007/s10696-014-9198-7. [DOI] [Google Scholar]
- 186.Kadı D, Kuvvetli Y, Çolak S. Performance analysis of a university hospital blood laboratory via discrete event simulation. Simulation. 2016;92:473–484. doi: 10.1177/0037549716643167. [DOI] [Google Scholar]
- 187.Cimellaro GP, Piqué M. Resilience of a hospital emergency department under seismic event. Adv Struct Eng. 2016;19:825–836. doi: 10.1177/1369433216630441. [DOI] [Google Scholar]
- 188.Zhong X, Lee HK, Williams M, Kraft S, Sleeth J, Welnick R, et al. Staffing ratio analysis in primary care redesign: a simulation approach. In: Matta A, Sahin E, Li J, Guinet A, Vandaele NJ, et al., editors. Health care systems engineering for scientists and practitioners. New York: Springer; 2016. pp. 133–144. [Google Scholar]
- 189.Lambton J, Roeder T, Saltzman R, Param L, Fernandes R. Using simulation to model improvements in pediatric bed placement in an acute care hospital. Jona J Nurs Adm. 2017;47:88–93. doi: 10.1097/NNA.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 190.Bakker M, Tsui K-L. Dynamic resource allocation for efficient patient scheduling: a data-driven approach. J Syst Sci Syst Eng. 2017;26:448–462. doi: 10.1007/s11518-017-5347-3. [DOI] [Google Scholar]
- 191.Weng S-J, Xu Y-Y, Gotcher D, Wang L-M. Proceedings of the summer computer simulation conference. 2017. A pilot study of available bed forecasting system (ABFS) in the emergency healthcare network. [Google Scholar]
- 192.Tànfani E, Testi A. Proceedings of the IEEE workshop on health care management. 2010. Improving surgery department performance via simulation and optimization. [Google Scholar]
- 193.Friemann F, Schönsleben P. Reducing global supply chain risk exposure of pharmaceutical companies by further incorporating warehouse capacity planning into the strategic supply chain planning process. J Pharm Innov. 2016;11:162–176. doi: 10.1007/s12247-016-9249-6. [DOI] [Google Scholar]
- 194.Ramis FJ, Baesler F, Berho E, Neriz L, Sepulveda JA. Proceedings of the winter simulation conference. 2008. A simulator to improve waiting times at a medical imaging center; pp. 1572–1577. [Google Scholar]
- 195.Zeinali F, Mahootchi M, Sepehri MM. Resource planning in the emergency departments: a simulation-based metamodeling approach. Simul Model Pract Theory. 2015;53:123–138. doi: 10.1016/j.simpat.2015.02.002. [DOI] [Google Scholar]
- 196.Wang J, Zhong X, Li J, Howard PK. Modeling and analysis of care delivery services within patient rooms: a system-theoretic approach. IEEE Trans Autom Sci Eng. 2014;11:379–393. doi: 10.1109/TASE.2013.2242326. [DOI] [Google Scholar]
- 197.Luangkesorn KL, Bountourelis T, Schaefer A, Nabors S, Clermont G. Proceedings of the winter simulation conference. 2012. The case against utilization: deceptive performance measures in inpatient care capacity models. [Google Scholar]
- 198.Holm LB, Dahl FA. Proceedings of the winter simulation conference. 2010. Simulating the influence of a 45% increase in patient volume on the emergency department of Akershus University Hospital; pp. 2455–2461. [Google Scholar]
- 199.Miller MJ, Ferrin DM, Szymanski JM. Proceedings of the winter simulation conference. 2003. Simulating six sigma improvement ideas for a hospital emergency department; pp. 1926–1929. [Google Scholar]
- 200.Mackay M, Qin S, Clissold A, Hakendorf P, Ben-Tovim D, McDonnell G. Proceedings of the international congress on modelling and simulation. 2013. Patient flow simulation modelling-an approach conducive to multi-disciplinary collaboration towards hospital capacity management; pp. 50–56. [Google Scholar]
- 201.Mes M, Bruens M. Proceedings of the winter simulation conference. 2012. A generalized simulation model of an integrated emergency post. [Google Scholar]
- 202.Khurma N, Bacioiu GM, Pasek ZJ. Proceedings of the winter simulation conference. 2008. Simulation-based verification of lean improvement for emergency room process; pp. 1490–1499. [Google Scholar]
- 203.Centeno MA, Lee MA, Lopez E, Fernandez HR, Carrillo M, Ogazon T. Proceeding of the winter simulation conference. 2001. A simulation study of the labor and delivery rooms at JMH; pp. 1392–1400. [Google Scholar]
- 204.Ramakrishnan S, Nagarkar K, DeGennaro M, Srihari K, Courtney AK, Emick F. Proceedings of the winter simulation conference. 2004. A study of the CT scan area of a healthcare provider; pp. 2025–2031. [Google Scholar]
- 205.Ruohonen T, Neittaanmäki P, Teittinen J. Proceedings of the winter simulation conference. 2006. Simulation model for improving the operation of the emergency department of special health care; pp. 453–458. [Google Scholar]
- 206.Bountourelis T, Luangkesorn L, Schaefer A, Maillart L, Nabors SG, Clermont G. Proceedings of the winter simulation conference. 2011. Development and validation of a large scale ICU simulation model with blocking; pp. 1143–1153. [Google Scholar]
- 207.Al-Araidah O, Boran A, Wahsheh A. Reducing delay in healthcare delivery at outpatients clinics using discrete event simulation. Int J Simul Model. 2012;11:185–195. doi: 10.2507/IJSIMM11(4)2.211. [DOI] [Google Scholar]
- 208.Pasupathy R. Proceedings of the winter simulation conference. 2013. Performance evaluation in a laboratory medicine unit; pp. 3972–3973. [Google Scholar]
- 209.Taylor SJE, Abbott P, Young T, Grocott-Mason R. Proceedings of the winter simulation conference. 2014. Student modeling & simulation projects in healthcare: experiences with Hillingdon Hospital; pp. 3650–3661. [Google Scholar]
- 210.Oh C, Novotny AM, Carter PL, Ready RK, Campbell DD, Leckie MC. Use of a simulation-based decision support tool to improve emergency department throughput. Oper Res Health Care. 2016;9:29–39. doi: 10.1016/j.orhc.2016.03.002. [DOI] [Google Scholar]
- 211.Eskandari H, Riyahifard M, Khosravi S, Geiger CD. Proceedings of the winter simulation conference. 2011. Improving the emergency department performance using simulation and MCDM methods; pp. 1211–1222. [Google Scholar]
- 212.Mielczarek B, Uziałko J. Proceedings of the winter simulation conference. 2012. Using simulation to forecast the demand for hospital emergency services at the regional level. [Google Scholar]
- 213.Perimal-Lewis L. Proceedings of the Australasian workshop on health informatics and knowledge management. 2014. Health intelligence: discovering the process model using process mining by constructing start-to-end patient journeys; pp. 59–67. [Google Scholar]
- 214.Hosseini N, Taaffe K. Proceedings of the winter simulation conference. 2014. Evaluation of optimal scheduling policy for accommodating elective and non-elective surgery via simulation; pp. 1377–1386. [Google Scholar]
- 215.Esengul Tayfur TK. Proceedings of the winter simulation conference. 2007. Allocation of resources for hospital evacuations via simulation; pp. 1148–1154. [Google Scholar]
- 216.Ashby M, Miller M, Ferrin D, Flynn T. Proceedings of the winter simulation conference. 2007. Simulating the patient move: transitioning to a replacement hospital; pp. 1562–1565. [Google Scholar]
- 217.Pérez ES, Yepez LA, de la Mota IF. Proceedings of the summer computer simulation conference. 2010. Simulation and optimization of the pre-hospital care system of the National University of Mexico using travelling salesman problem algorithms; pp. 364–370. [Google Scholar]
- 218.Güttinger D, Godehardt E, Zinnen A. Proceedings of the 4th international ICST (Institute for Computer Sciences, social-informatics and telecommunications engineering) conference on simulation tools and techniques. 2011. Optimizing emergency supply for mass events; pp. 125–133. [Google Scholar]
- 219.Noreña D, Yamín L, Akhavan-Tabatabaei R, Ospina W. Proceedings of the winter simulation conference. 2011. Using discrete event simulation to evaluate the logistics of medical attention during the relief operations in an earthquake in Bogota; pp. 2666–2678. [Google Scholar]
- 220.Ullrich C, Van Utterbeeck F, Dejardin E, Debacker M, Dhondt E. Proceedings of the winter simulation conference. 2013. Pre-hospital simulation model for medical disaster management; pp. 2432–2433. [Google Scholar]
- 221.Noei S, Santana H, Sargolzaei A, Noei M. Proceedings of the international workshop on emerging multimedia applications and services for smart cities. 2014. Reducing traffic congestion using geo-fence technology: application for emergency car; pp. 15–20. [Google Scholar]
- 222.Moon I-C, Bae JW, Lee J, Kim D, Lee H, Lee T, et al. Proceedings of the winter simulation conference. 2015. EMSSIM: emergency medical service simulator with geographic and medical details; pp. 1272–1284. [Google Scholar]
- 223.Gibson IW. Proceedings of the winter simulation conference. 2007. An approach to hospital planning and design using discrete event simulation; pp. 1501–1509. [Google Scholar]
- 224.Miller MJ, Ferrin DM, Shahi N, LaVecchia R. Proceedings of the winter simulation conference. 2008. Allocating outpatient clinic services using simulation and linear programming; pp. 1637–1644. [Google Scholar]
- 225.Ashby M, Ferrin D, Miller M, Shahi N. Proceedings of the winter simulation conference. 2008. Discrete event simulation: optimizing patient flow and redesign in a replacement facility; pp. 1632–1636. [Google Scholar]
- 226.Boucherie RJ, Hans EW, Hartmann T. Proceedings of the winter simulation conference. 2012. Health care logistics and space: accounting for the physical build environment. [Google Scholar]
- 227.Wurzer G. In-process agent simulation for early stages of hospital planning. Math Comput Model Dyn Syst. 2013;19:331–343. doi: 10.1080/13873954.2012.761638. [DOI] [Google Scholar]
- 228.Wurzer G, Lorenz WE, Rössler M, Hafner I, Popper N, Glock BMODYPLAN. Proceedings of the symposium on simulation for architecture and urban design. 2015. Early-stage hospital simulation with emphasis on cross-clinical treatment chains; pp. 160–163. [Google Scholar]
- 229.Schaumann D, Pilosof NP, Date K, Kalay YE. A study of human behavior simulation in architectural design for healthcare facilities. Ann Dell Ist Super Sanita. 2016;52:24–32. doi: 10.4415/ANN_16_01_07. [DOI] [PubMed] [Google Scholar]
- 230.Cimellaro GP, Malavisi M, Mahin S. Using discrete event simulation models to evaluate resilience of an emergency department. J Earthq Eng. 2017;21:203–226. doi: 10.1080/13632469.2016.1172373. [DOI] [Google Scholar]
- 231.Pulat PS, Kasap S, Splinter GL. Simulation study of an ideal primary care delivery system. Simulation. 2001;76:78–86. doi: 10.1177/003754970107600203. [DOI] [Google Scholar]
- 232.Moeke D, van de Geer R, Koole G, Bekker R. On the performance of small-scale living facilities in nursing homes: a simulation approach. Oper Res Health Care. 2016;11:20–34. doi: 10.1016/j.orhc.2016.10.001. [DOI] [Google Scholar]
- 233.Maroufkhani A, Lanzarone E, Castelnovo C, Di Mascolo M. A discrete event simulation model for the admission of patients to a home care rehabilitation service. In: Matta A, Sahin E, Li J, Guinet A, Vandaele NJ, editors. Health care systems engineering for scientists and practitioners. New York: Springer; 2016. pp. 91–100. [Google Scholar]
- 234.Bhattacharjee P, Ray PK. Patient flow modelling and performance analysis of healthcare delivery processes in hospitals: a review and reflections. Comput Ind Eng. 2014;78:299–312. doi: 10.1016/j.cie.2014.04.016. [DOI] [Google Scholar]
- 235.Hu S, Heim JA. Proceedings of the winter simulation conference. 2014. Developing domain-specific simulation objects for modeling clinical laboratory operations; pp. 1341–1352. [Google Scholar]
- 236.Workman RW. Proceedings of the winter simulation conference. 2000. Simulation of the drug development process: a case study from the pharmaceutical industry; pp. 1995–1998. [Google Scholar]
- 237.Blau GE, Pekny JF, Varma VA, Bunch PR. Managing a portfolio of interdependent new product candidates in the pharmaceutical industry. J Prod Innov Manag. 2004;21:227–245. doi: 10.1111/j.0737-6782.2004.00075.x. [DOI] [Google Scholar]
- 238.Chen Y, Mockus L, Orcun S, Reklaitis GV. Simulation-optimization approach to clinical trial supply chain management with demand scenario forecast. Comput Chem Eng. 2012;40:82–96. doi: 10.1016/j.compchemeng.2012.01.007. [DOI] [Google Scholar]
- 239.Perez-Escobedo JL, Azzaro-Pantel C, Pibouleau L. Multiobjective strategies for New Product Development in the pharmaceutical industry. Comput Chem Eng. 2012;37:278–296. doi: 10.1016/j.compchemeng.2011.10.004. [DOI] [Google Scholar]
- 240.Chen Y, Pekny JF, Reklaitis GV. Integrated planning and optimization of clinical trial supply chain system with risk pooling. Ind Eng Chem Res. 2013;52:152–165. [Google Scholar]
- 241.El Afia A, Mezouar H. Proceedings of the international conference on big data, cloud and applications. 2017. A global mapping of the Moroccan supply chain of hospital drugs, and a simulation of the dispensation process. [Google Scholar]
- 242.Huyghe J, Nouwen M, Vanattenhoven J. Proceedings of the Nordic conference on human-computer interaction. 2016. Involving end-users in game based ideation: a case study in hospital logistics. [Google Scholar]
- 243.Best AM, Dixon CA, Kelton WD, Lindsell CJ, Ward MJ. Using discrete event computer simulation to improve patient flow in a Ghanaian acute care hospital. Am J Emerg Med. 2014;32:917–922. doi: 10.1016/j.ajem.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Caputo AC, Pelagagge PM. Management criteria of automated order picking systems in high-rotation high-volume distribution centers. Ind Manag Data Syst. 2006;106:1359–1383. doi: 10.1108/02635570610712627. [DOI] [Google Scholar]
- 245.Katsaliaki K, Brailsford SC. Using simulation to improve the blood supply chain. J Oper Res Soc. 2007;58:219–227. doi: 10.1057/palgrave.jors.2602195. [DOI] [Google Scholar]
- 246.Vila-Parrish AR, Ivy JS, King RE. Proceedings of the winter simulation conference. 2008. A simulation-based approach for inventory modeling of perishable pharmaceuticals; pp. 1532–1538. [Google Scholar]
- 247.Jung JY, Blau G, Pekny JF, Reklaitis GV, Eversdyk D. Integrated safety stock management for multi-stage supply chains under production capacity constraints. Comput Chem Eng. 2008;32:2570–2581. doi: 10.1016/j.compchemeng.2008.04.003. [DOI] [Google Scholar]
- 248.Mustafee N, Taylor SJE, Katsaliaki K, Brailsford S. Facilitating the analysis of a UK national blood service supply chain using distributed simulation. Simulation. 2009;85:113–128. doi: 10.1177/0037549708100530. [DOI] [Google Scholar]
- 249.Rossetti MD, Liu Y. Proceedings of the winter simulation conference. 2009. Simulating SKU proliferation in a health care supply chain; pp. 2365–2374. [Google Scholar]
- 250.Ren C, Wang W, He M, Shao B, Wang Q, Dong J. The use of simulation for Global Supply Network rationalization. In: Proceedings of IEEE international conference on service operations and logistics, and informatics. 2010. p. 276–81.
- 251.Babaï MZ, Syntetos AA, Dallery Y, Nikolopoulos K. Dynamic re-order point inventory control with lead-time uncertainty: analysis and empirical investigation. Int J Prod Res. 2009;47:2461–2483. doi: 10.1080/00207540701666824. [DOI] [Google Scholar]
- 252.Baesler F, Bastías A, Nemeth M, Martínez C. Proceedings of the winter simulation conference. 2012. Blood centre inventory analysis using discrete simulation. [Google Scholar]
- 253.Onggo BS. Proceedings of the winter simulation conference. 2014. Elements of a hybrid simulation model: a case study of the blood supply chain in low-and middle-income countries; pp. 1597–1607. [Google Scholar]
- 254.Gebicki M, Mooney E, Chen S-J, Mazur LM. Evaluation of hospital medication inventory policies. Health Care Manag Sci. 2014;17:215–229. doi: 10.1007/s10729-013-9251-1. [DOI] [PubMed] [Google Scholar]
- 255.Duan Q, Liao TW. Optimization of blood supply chain with shortened shelf lives and ABO compatibility. Int J Prod Econ. 2014;153:113–129. doi: 10.1016/j.ijpe.2014.02.012. [DOI] [Google Scholar]
- 256.Baesler F, Nemeth M, Martínez C, Bastías A. Analysis of inventory strategies for blood components in a regional blood center using process simulation. Transfusion. 2014;54:323–330. doi: 10.1111/trf.12287. [DOI] [PubMed] [Google Scholar]
- 257.Wang K-M, Ma Z-J. Age-based policy for blood transshipment during blood shortage. Transp Res Part E Logist Transp Rev. 2015;80:166–183. doi: 10.1016/j.tre.2015.05.007. [DOI] [Google Scholar]
- 258.Leung N-HZ, Chen A, Yadav P, Gallien J. The impact of inventory management on stock-outs of essential drugs in Sub-Saharan Africa: secondary analysis of a field experiment in Zambia. PLoS One. 2016;11:e0156026. doi: 10.1371/journal.pone.0156026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yurtkuran A, Emel E. Proceedings of the winter simulation conference. 2008. Simulation based decision-making for hospital pharmacy management; pp. 1539–1546. [Google Scholar]
- 260.Lee YM. Proceedings of the winter simulation conference. 2008. Analyzing dispensing plan for emergency medical supplies in the event of bioterrorism; pp. 2600–2608. [Google Scholar]
- 261.Lee YM, Ghosh S, Ettl M. Proceedings of the winter simulation conference. 2009. Simulating distribution of emergency relief supplies for disaster response operations; pp. 2797–2808. [Google Scholar]
- 262.Ozdamar L. Planning helicopter logistics in disaster relief. Spectrum. 2011;33:655–672. doi: 10.1007/s00291-011-0259-y. [DOI] [Google Scholar]
- 263.Kulkarni NS, Niranjan S. Proceedings of the winter simulations conference. 2013. Multi-echelon network optimization of pharmaceutical cold chains: a simulation study; pp. 3486–3498. [Google Scholar]
- 264.Postacchini L, Ciarapica FE, Bevilacqua M, Mazzuto G, Paciarotti C. A way for reducing drug supply chain cost for a hospital district: a case study. J Ind Eng Manag. 2016;9:207–230. [Google Scholar]
- 265.Abdelkafi C, Beck BHL, David B, Druck C, Horoho M. Balancing risk and costs to optimize the clinical supply chain-a step beyond simulation. J Pharm Innov. 2009;4:96–106. doi: 10.1007/s12247-009-9063-5. [DOI] [Google Scholar]
- 266.Alfonso E, Xie X, Augusto V, Garraud O. Modelling and simulation of blood collection systems: improvement of human resources allocation for better cost-effectiveness and reduction of candidate donor abandonment. Vox Sang. 2013;104:225–233. doi: 10.1111/vox.12001. [DOI] [PubMed] [Google Scholar]
- 267.Cho S-H, Jang H, Lee T, Turner J. Simultaneous location of trauma centers and helicopters for emergency medical service planning. Oper Res. 2014;62:751–771. doi: 10.1287/opre.2014.1287. [DOI] [Google Scholar]
- 268.Liao H-C, Chang H-H. The optimal approach for parameter settings based on adjustable contracting capacity for the hospital supply chain logistics system. Expert Syst Appl. 2011;38:4790–4797. doi: 10.1016/j.eswa.2010.09.168. [DOI] [Google Scholar]
- 269.Akcay A, Martagan T. Proceedings of the winter simulation conference. 2016. Stochastic simulation under input uncertainty for contract-manufacturer selection in pharmaceutical industry; pp. 2292–2303. [Google Scholar]
- 270.Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–426. doi: 10.1037/1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- 271.Royston G, Dost A, Townshend J, Turner H. Using system dynamics to help develop and implement policies and programmes in health care in England. Syst Dyn Rev. 1999;15:293–313. doi: 10.1002/(SICI)1099-1727(199923)15:3<293::AID-SDR169>3.0.CO;2-1. [DOI] [Google Scholar]
- 272.Mustafee N, Taylor SJE, Katsaliaki K, Brailsford S. Proceedings of the winter simulation conference. 2006. Distributed simulation with COTS simulation packages: a case study in health care supply chain simulation; pp. 1136–1142. [Google Scholar]
- 273.Muller J, Popke C, Urbat M, Zeier A, Plattner H. Proceedings of the international conference on advances in system simulation. 2009. A simulation of the pharmaceutical supply chain to provide realistic test data; pp. 44–49. [Google Scholar]
- 274.Devi SP, Rao KS, Krishnaswamy S, Wang S. System dynamics model for simulation of the dynamics of corneal transplants. OPSEARCH. 2010;47:284–292. doi: 10.1007/s12597-010-0023-0. [DOI] [Google Scholar]
- 275.Ng Adam TS, Sy C, Li J. Proceedings of the winter simulation conference. 2011. A system dynamics model of Singapore healthcare affordability; pp. 1306–1318. [Google Scholar]
- 276.Djanatliev A, German R, Kolominsky-Rabas P, Hofmann BM. Proceedings of the winter simulation conference. 2012. Hybrid simulation with loosely coupled system dynamics and agent-based models for prospective health technology assessments. [Google Scholar]
- 277.zen MB. Proceedings of the winter simulation conference. 2013. Estimating future demand for hospital emergency services at the regional level; pp. 2386–2397. [Google Scholar]
- 278.Elleuch H, Hachicha W, Chabchoub H. A combined approach for supply chain risk management: description and application to a real hospital pharmaceutical case study. J Risk Res. 2014;17:641–663. doi: 10.1080/13669877.2013.815653. [DOI] [Google Scholar]
- 279.Padilla JJ, Diallo SY, Kavak H, Sahin O, Sokolowski JA, Gore RJ. Semi-automated initialization of simulations: an application to healthcare. J Def Model Simul. 2015;13:171–182. doi: 10.1177/1548512914565503. [DOI] [Google Scholar]
- 280.Taaffe K, Zinouri N, Kamath AG. Proceedings of the winter simulation conference. 2016. Integrating simulation modeling and mobile technology to improve day-of-surgery patient care; pp. 2111–2112. [Google Scholar]
- 281.Pitt M, Monks T, Crowe S, Vasilakis C. Systems modelling and simulation in health service design, delivery and decision making. BMJ Qual Saf. 2016;25:38–45. doi: 10.1136/bmjqs-2015-004430. [DOI] [PubMed] [Google Scholar]
- 282.Jahangirian M, Borsci S, Shah SGS, Taylor SJE. Causal factors of low stakeholder engagement: a survey of expert opinions in the context of healthcare simulation projects. Simulation. 2015;91:511–526. doi: 10.1177/0037549715583150. [DOI] [Google Scholar]
- 283.Dangerfield BC. System dynamics applications to European health care issues. J Oper Res Soc. 1999;50:45–353. doi: 10.1057/palgrave.jors.2600729. [DOI] [Google Scholar]
- 284.Harrell CR, Price RN. Proceedings of the winter simulation conference. 2000. Healthcare simulation modeling and optimization using MedModel; pp. 203–207. [Google Scholar]
- 285.Joustra P, van der Sluis E, van Dijk NM. To pool or not to pool in hospitals: a theoretical and practical comparison for a radiotherapy outpatient department. Ann Oper Res. 2010;178:77–89. doi: 10.1007/s10479-009-0559-7. [DOI] [Google Scholar]
- 286.Morrison BP, Bird BC. Proceedings of the winter simulation conference. 2003. Healthcare process analysis: a methodology for modeling front office and patient care processes in ambulatory health care; pp. 1882–1886. [Google Scholar]
- 287.Baldwin LP, Eldabi T, Paul RJ. Simulation in healthcare management: a soft approach (MAPIU) Simul Model Pract Theory. 2004;12:541–557. doi: 10.1016/j.simpat.2004.02.003. [DOI] [Google Scholar]
- 288.White KP. Proceedings of the winter simulation conference. 2005. A survey of data resources for simulating patient flows in healthcare delivery systems; pp. 926–935. [Google Scholar]
- 289.Brailsford S. Overcoming the barriers to implementation of operations research simulation models in healthcare. Clin Investig Med Med Clin Exp. 2005;28:312–315. [PubMed] [Google Scholar]
- 290.Eldabi T, Paul RJ, Young T. Simulation modelling in healthcare: reviewing legacies and investigating futures. J Oper Res Soc. 2007;58:262–270. doi: 10.1057/palgrave.jors.2602222. [DOI] [Google Scholar]
- 291.Chahal K, Eldabi T. Proceedings of the winter simulation conference. 2008. Applicability of hybrid simulation to different modes of governance in UK healthcare; pp. 1469–1477. [Google Scholar]
- 292.Gupta D, Denton B. Appointment scheduling in health care: challenges and opportunities. IIE Trans. 2008;40:800–819. doi: 10.1080/07408170802165880. [DOI] [Google Scholar]
- 293.Brailsford SC, Harper PR, Patel B, Pitt M. An analysis of the academic literature on simulation and modelling in health care. J Simul. 2009;3:130–140. doi: 10.1057/jos.2009.10. [DOI] [Google Scholar]
- 294.Katsaliaki K, Mustafee N, Taylor SJE, Brailsford S. Comparing conventional and distributed approaches to simulation in a complex supply-chain health system. J Oper Res Soc. 2009;60:43–51. doi: 10.1057/palgrave.jors.2602531. [DOI] [Google Scholar]
- 295.Forsythe L. Action research, simulation, team communication, and bringing the tacit into voice society for simulation in healthcare. Simul Healthc. 2009;4:143–148. doi: 10.1097/SIH.0b013e3181986814. [DOI] [PubMed] [Google Scholar]
- 296.Seropian M, Lavey R. Design considerations for healthcare simulation facilities. Simul Healthc. 2010;5:338–345. doi: 10.1097/SIH.0b013e3181ec8f60. [DOI] [PubMed] [Google Scholar]
- 297.Katsaliaki K, Mustafee N. Applications of simulation within the healthcare context. J Oper Res Soc. 2011;62:1431–1451. doi: 10.1057/jors.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.LeBlanc VR, Manser T, Weinger MB, Musson D, Kutzin J, Howard SK. The study of factors affecting human and systems performance in healthcare using simulation. Simul Healthc. 2011;6:24–29. doi: 10.1097/SIH.0b013e318229f5c8. [DOI] [PubMed] [Google Scholar]
- 299.Beliën J, Forcé H. Supply chain management of blood products: a literature review. Eur J Oper Res. 2012;217:1–16. doi: 10.1016/j.ejor.2011.05.026. [DOI] [Google Scholar]
- 300.Jahangirian M, Naseer A, Stergioulas L, Young T, Eldabi T, Brailsford S, et al. Simulation in health-care: lessons from other sectors. Oper Res. 2012;12:45–55. [Google Scholar]
- 301.Hong TS, Shang PP, Arumugam M, Yusuff RM. Use of simulation to solve outpatient clinic problems: a review of the literature. South Afr J Ind Eng. 2013;24:27–42. [Google Scholar]
- 302.Holm LB, Dahl FA. Proceedings of the winter simulation conference. 2009. Simulating the effect of physician triage in the emergency department of Akershus University Hospital; pp. 1896–1905. [Google Scholar]
- 303.Günal MM, Pidd M. Proceedings of the winter simulation conference. 2008. DGHPSim: supporting smart thinking to improve hospital performance; pp. 1484–1489. [Google Scholar]
- 304.Yeon N, Lee T, Jang H. Proceedings of the winter simulation conference. 2010. Outpatients appointment scheduling with multi-doctor sharing resources; pp. 3318–3329. [Google Scholar]
- 305.Sugiyama T, Goryoda S, Inoue K, Sugiyama-Ihana N, Nishi N. Construction of a simulation model and evaluation of the effect of potential interventions on the incidence of diabetes and initiation of dialysis due to diabetic nephropathy in Japan. BMC Health Serv Res. 2017;17:833. doi: 10.1186/s12913-017-2784-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


