Abstract
Background
ACL injuries are common among sports populations and achieving adequate lower extremity strength is important prior to return to play. Access to isokinetic testing equipment that measures lower extremity strength is limited. Screening tools that measure functional criteria are accessible to clinicians, however the tools' relationship to strength constructs have not been investigated in an ACL reconstructed (ACLR) population.
Purpose
The primary objective was to determine if relationships exist between isokinetic peak knee extension torque (PKET), peak knee flexion torque (PKFT), hamstring to quadriceps (HQ) ratios, and YBT-LQ performance following ACLR. The secondary objective was to observe differences in isokinetic strength ability between high and low performers on the YBT-LQ.
Study Design
Retrospective Chart Review
Methods
Medical records of forty-five ACL-reconstructed subjects, between five-12 months post-surgery were queried for functional assessment data collected during the institution's standard outcome testing battery. Variables of interest included: demographic and anthropomorphic measures, YBT-LQ performance, and involved limb isokinetic PKET, PKFT, and HQ ratios. Performance on each measure, as well as asymmetry between sides, was analyzed using a correlation matrix.
Results
Statistically significant (p<0.01) relationships were identified between YBT-LQ anterior reach asymmetry and the PKET deficit (r=0.264). PKET and PKFT on the involved limb correlated to performance of anterior reach (r=0.591, p<0.01)(r=0.493, p<0.01), posteromedial reach (r=0.498, p<0.01)(r=0.577, p<0.01), and posterolateral reach (r=0.294, p<0.05)(r=0.445, p<0.01) respectively. Similar relationships existed on the uninvolved side, but to a lesser extent. High and low performers on the YBT-LQ demonstrated lower and higher extension torque deficits, respectively.
Conclusion
While each test measures unique constructs, there are associations between components of the tests. In the ACLR population, both the YBT-LQ and isokinetic strength testing can expose asymmetries and impact return to play decision making.
Level of evidence
2b
Keywords: ACL, Y-Balance test lower quarter, isokinetic testing, return to sports
INTRODUCTION
ACL ruptures remain common among adolescents and young adults participating in sports resulting in about 150,000 to 200,000 ACL reconstructions performed each year.1 For an athlete to return to his or her selected sport or vigorous activity, ACL reconstruction surgery is often performed, followed by a rehabilitation program typically lasting six to 12 months.1,2,3,4 To date, there has been no consensus on criteria for return to sport nor have universal guidelines been established to determine readiness to return an athlete to previous level of sport, to decrease re-injury rates, or to preserve long-term joint health.1,2,4,5, In general, a combination of time after surgery, subjective report, graft laxity, joint range of motion, strength, and functional testing is commonly used to determine the athlete's physical readiness to return to prior level of activity.1,2,6,7,8
With regard to assessing strength, one commonly reported criteria is the patient's ability to demonstrate isokinetic quadriceps strength of at least 85% of the non-injured lower extremity and a hamstring to quadriceps (HQ) ratio of 2:3.6–10 Researchers have historically promoted isokinetic testing as the best tool for quantifying torque asymmetries in lower limb strength.11 However, isokinetic dynamometers are expensive, require additional time and training, and are often inaccessible in a majority of clinical settings. To improve feasibility of quantifying deficits in lower limb strength and function, it may be beneficial to establish a screening tool that would capture strength deficits that are similar to those measured during isokinetic testing. An abundance of lower extremity screening tools have been reported in the literature, most of which incorporate some level of functional or sport specific criteria.1,12 Poor performance on certain tests has been associated with an elevated risk of lower extremity injury.2,7,13 The Y Balance Test for the Lower Quarter (YBT-LQ) (a derivative of the anterior, posteromedial, and posterolateral reaches of the Star Excursion Balance Test (SEBT)) is one such test with good to excellent intra-rater and interrater reliability that has been used to predict injuries in high school athletes.14,15 Dynamic balance tests, such as the SEBT and the YBT-LQ, have been shown to be a reliable measure of an athlete's functional abilities.6,14,15,17 Specifically, the YBT-LQ is able to capture differences between the injured and non-injured limbs. This may expose asymmetries at the limit of the athlete's stability (much like what may be observed during athletic movements), which can be of benefit when returning an athlete from an injury.
Since the YBT-LQ is a functional outcome measure that can be easily utilized in the clinic, it may serve as a good evaluative tool in determining return to sport. As such, it is important to understand how it correlates with other commonly reported measures such as quadriceps and hamstring strength. To date, there are few reports that have investigated the relationship between lower extremity muscular ability and YBT-LQ performance.18,19,20 These include EMG studies of lower extremity musculature during the Star Excursion Balance Test as well as one study comparing YBT-LQ performance with eccentric isokinetic knee flexion and extension torque in healthy subjects. The primary objective was to determine if relationships exist between isokinetic peak knee extension torque (PKET), peak knee flexion torque (PKFT), hamstring to quadriceps (HQ) ratios, and YBT-LQ performance following ACLR. The secondary objective was to observe differences in isokinetic strength ability between high and low performers on the YBT-LQ.
METHODS
Study Design
The study involved a retrospective analysis of patient data at an outpatient hospital-based sports medicine physical therapy clinic. The study was approved by the Duke University Health System Institutional Review Board.
Subjects
Males and females age 15-35 years with primary ACL reconstruction either in isolation or in combination with a meniscal repair or meniscectomy were included. Surgical procedures took place between 01/01/2007 – 10/15/2013 by one of three surgeons and included hamstring grafts, bone-patellar tendon- bone grafts, and allografts. Exclusion criteria included subjects who had undergone a revision procedure.
Procedures
The subject's medical record was queried for functional assessment data which was collected between five and 12 months post-operatively as part of the institution's standard post-operative outcome testing battery. Demographic and anthropometric information was collected including: age, gender, laterality of injury, body mass index, surgical procedure and time after surgery. Key variables of interest for return to sport criteria included: isokinetic testing (concentric/concentric) performed at 60 degrees per second utilizing the Cybex Isokinetic Dynamometer (Humac®/Norm TM Testing and Rehabilitation System, Model 770 Computer Sports Medicine Inc, Medical Solutions Stoughton, MA) to obtain peak extensor and flexor torques, and HQ ratios. Isokinetic testing was administered by licensed physical therapists who underwent training for operating the testing equipment. YBT-LQ was performed utilizing the Y-Balance Test Kit™ (FunctionalMovement.com, Danville, VA) for maximum reach distance in the anterior, posteromedial, posterolateral directions. The composite score for each limb was calculated and normalized to limb length. YBT-LQ testing was administered by staff (physical therapists, athletic trainers, and biomechanics lab staff) who were certified through an online course and examination.
Isokinetic testing was conducted using the isokinetic dynamometer following the protocol outlined by Cardone et al, as per the user manual.21,22 Concentric knee flexion and extension movements were assessed at the angular velocities of 60, 180 and 240 degrees per second. Tests were performed in sitting while ensuring stabilization by applying straps to the trunk, waist, and thigh. The inferior resistance pad was placed at a level one inch proximal to the medial malleolus and the superior pad was placed an inch below the tibial tubercle. The lateral femoral condyle was used as an anatomic reference for the axis of rotation.22 The range of motion tested was 0-90 degrees. Five repetitions at 60 degrees per second, five repetitions at 180 degrees per second, and fifteen repetitions at 240 degrees per second were performed with a one minute rest interval between speeds. The patient was able to practice each speed for three repetitions prior to the test repetitions. Verbal motivation was provided during the test to encourage maximal effort. Torque values at the 60 degrees/second conditions were analyzed as this speed is most commonly reported in the literature.
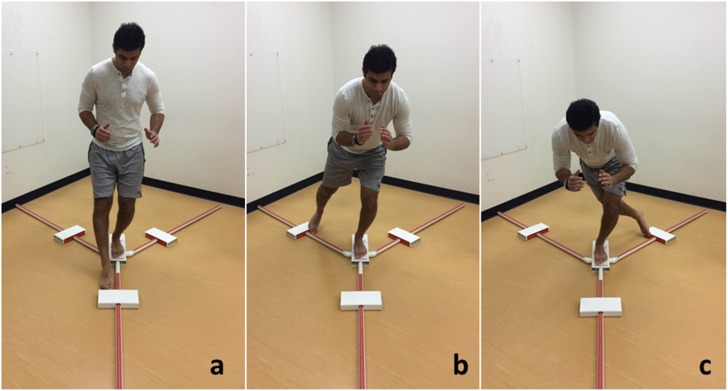
Testing for the YBT-LQ followed a standardized protocol in which the subject started by standing with one foot on a stance plate with the most distal aspect of the foot at the starting line and then reached with the opposite leg in anterior, posteromedial and posterolateral directions.12 (Figure 1) A standard number of practice trials (up to six) were allowed in order to minimize a learning effect. Each direction was repeated three times and the best repetition for each direction was recorded. The composite score, expressed as a percentage, was obtained by taking the average of the normalized reach scores ([anterior + posteromedial + posterolateral]*100/3*leg length).12
Figure 1.
Y-Balance Test of the Lower Quarter. The direction of reach is named relative to the stationary lower extremity- a. anterior reach, b. posteromedial reach, c. posterolateral reach.
In all cases, isokinetic testing and YBT-LQ were considered standard of practice within the facility in which data were captured. The tests were performed during the same week, and not in the same order. All subjects followed standardized post-operative ACL rehabilitation guidelines staged by both chronological and biological healing time frames and graft type. The first phase focused on graft protection, normalization of gait pattern, early ROM, swelling management, initial quadriceps activation and kinetic chain strengthening. The second phase focused on establishing symmetrical knee ROM, achievement of active knee hyperextension, improved lower extremity strength, and good stability with dynamic knee activities. The third phase focused on improving strength to >85% of the non-involved extremity, performance of advanced proprioception exercises, improved aerobic endurance, initiation of plyometric exercises and return to running and functional training. The fourth phase focused on establishing equal bilateral lower extremity strength, balance, proprioception, and power in the lower extremities and return to sport activities.
Sample Size
Sample size was not determined prior to the retrospective review. Rather, all eligible patients within the defined timeframe in which this testing was standard of practice were targeted.
Data Analysis
For the primary purpose, analysis was performed using IBM SPSS version 23.0. Means and standard deviations were used to describe overall group descriptive statistics, as well as reported by male and female sex. All variables were analyzed for normality using a Shapiro Wilk test and 40% of variables did not exhibit a normal distribution. A correlation matrix was run using Spearman Rho correlation statistics, a nonparametric equivalent to the Pearson Product test. Values close to -1 or + 1 suggested a strong association whereas value closer to 0 suggested no relationship. Relationships, as defined by Cohen, are 0.01-0.3 (weak), 0.3-0.5 (moderate), and 0.5-0.99 (strong).23 An alpha value of 0.05 was used to quantify statistical significance. To address the secondary purpose, the mean extensor and flexor peak torque values were calculated for the subjects who performed the anterior reach with an asymmetry of 1 or less (high performers) and an asymmetry of 4 or greater (low performers).
RESULTS
Data from the charts of 45 individuals who were seen from February 2011 to May 2014 was utilized. There were no more than seven days between the date of the isokinetic test and the date of the YBT-LQ test. Subjects were an average age of 21.1 ± 5.8 years and were primarily male (N=29, 22.6 ± 6.3 years). A total of 16 females (18.5 ± 3.6 years) were also included in the retrospective review. Demographics and anthropometrics for the subjects at the time of their surgery are detailed in Table 1. Correlations between isokinetic testing and YBT-LQ balance testing on the involved side (Table 2) and the uninvolved side (Table 3) are presented.
Table 1.
Descriptive values for male and female subjects.
| Gender | Number | Height (m) | Weight (kg) | Age at Time of Surgery | Months after Surgery Mean ± SD (range) | Laterality of Involved Limb |
|---|---|---|---|---|---|---|
| Female | 16 | 1.68 ± 0.06 | 66.52 ± 6.62 | 18.5 ± 3.6 yrs | 8.2 ± 2.0 (5.5 – 12.0) | 8 Left, 8 Right |
| Male | 29 | 1.78 ± 0.07 | 80.59 ± 12.44 | 22.6 ± 6.3 yrs | 7.2 ± 1.8 (5.5 – 12.0) | 14 Left, 15 Right |
| Total | 45 | 1.75 ± 0.08 | 75.62 ± 12.65 | 21.1 ± 5.8 yrs | 7.6 ± 1.9 (4.7 – 12.0) | 22 Left, 23 Right |
Table 2.
Correlation values (r) between Y-Balance Test variables and isokinetic variables with the involved limb using the Spearman Rho
| Y-Balance Measures | |||||||
|---|---|---|---|---|---|---|---|
| Isokinetic Measures | Anterior Reach Distance | Posterior-medial Reach Distance | Posterior-lateral Reach Distance | Asymmetry Anterior Reach | Asymmetry Posteromedial Reach | Asymmetry Posterolateral Reach | Composite Scores |
| Extension Torque | .591** | .498** | .294* | .165 | -.136 | -.010 | .268 |
| Flexion Torque | .493** | .577** | .445** | .034 | -.015 | .032 | .362** |
| Extension Deficit | -.144 | -.135 | .037 | .264** | .303* | .117 | -.162 |
| Flexion Deficit | -.248 | -.280* | -.186 | .005 | .063 | -.152 | -.139 |
| HQ Ratio | -.037 | .106 | .216 | -.075 | .259 | .054 | .136 |
=significant at p<0.05
=significantn at p<0.01
Table 3.
Correlation values (r) between Y-Balance Test variables and isokinetic variables on Uninvolved limb using the Spearman Rho
| Y-Balance Measures | |||||||
|---|---|---|---|---|---|---|---|
| Isokinetic Measures | Anterior Reach Distance | Posterior-medial Reach Distance | Posterior-lateral Reach Distance | Asymmetry Anterior Reach | Asymmetry Posteromedial Reach | Asymmetry Posterolateral Reach | Composite Scores |
| Extension Torque | .269 | .302* | .223 | .157 | .033 | .132 | -.026 |
| Flexion Torque | .293* | .338* | .281* | .031 | .010 | .052 | .161 |
| Extension Deficit | -.026 | .068 | .058 | .264** | .303* | .117 | -.044 |
| Flexion Deficit | -.236 | -.160 | -.311 | .005 | .063 | -.152 | -.060 |
| HQ Ratio | .139 | .083 | .146 | -.079 | -.013 | .114 | .326* |
=significant at p<0.05
=significant at p<0.01
With regard to the YBT-LQ composite scores, the involved side was moderately correlated to the peak flexor torque production (r=0.362) (p<0.01). Peak flexor torque was also moderately correlated to both anterior (r=0.493), posteromedial (r=0.577), and posterolateral (r=0.445) reach distances on the involved side (p<0.01). On the uninvolved side, the relationship between peak flexor torque and reach distances were correlated, but, to a lesser extent (r=0.281-0.338). (Table 2) On the involved side, relationships also existed between peak extensor torque values and the anterior (r=0.591) (p<0.01), posteromedial (r=0.498) (p<0.01), and posterolateral (r=0.294) (p<0.05) reach distances. Again, relationships existed, to a lesser extent, between peak extensor torque and each reach distance on the uninvolved side, with only the posteromedial reach demonstrating a significant relationship (r=0.302) (p<.05).
With regard to asymmetries between limbs, the most significant, though weak, relationship existed between the anterior reach asymmetry and the extensor torque deficit (r=0.264) (p<0.01). Also, the posteromedial reach asymmetry significantly was correlated to extension deficit (r=0.303) (p<0.05).
Additionally, YBT-LQ subjects were dichotomized into subgroups of low performers and high performers for additional observation. Those who demonstrated greater than a 4 cm side to side deficit on the YBT-LQ anterior reach (n=14) were observed to show a side to side mean extensor deficit of27.36 ± 19.12% on isokinetic testing compared to those that demonstrated less than or equal to 1 cm anterior reach deficits (n=14) who had a mean extensor deficit of 12.43 ± 20.66%. However, there was only a minimal difference observed in side-to-side isokinetic flexor deficits (16.29 ± 20.40%; 17.07 ± 13.65%) for greater than 4cm or less than/equal to 1cm respectively.
DISCUSSION
The primary purpose of this retrospective investigation was to determine whether relationships exist between isokinetic extensor and flexor peak torque values and YBT-LQ performance in a group of patients who had undergone ACLR. As functional testing batteries are often included in examination for return to sport, it is important to understand how different tests are related so that the measures included in such a battery minimize redundancy and demonstrate ideal validity and predictive value. Both isokinetic testing and YBT-LQ have historically been used by clinicians as outcome measures and included in decision making for return to sport. The data presented in this study indicate that relations of varying degrees do exist between the two tests.
While limited studies examining the relationship between the YBT-LQ and isokinetic testing exist in a healthy population,18 Booysen et al compared eccentric knee extensor and flexor torque (as a measure of strength) to normalized YBT-LQ composite scores and found a significant relationship between knee extension torque and YBT-LQ scores in the non-dominant extremity of healthy soccer players.18 Their study did not include concentric strength measures and did not report relationships between strength and individual reach directions. In EMG studies performed on healthy, college-age subjects, vastus medialis contraction during the anterior and posteromedial directions of the star excursion balance test ranged from 66% to greater than 100% maximal voluntary isometric contraction (MVIC). This suggests a requirement for functional knee extensor strength during this task.19,20 Both YBT-LQ and isokinetic testing outcomes for the patients in the current study are similar to those reported in the literature. The results of the current study indicate that weak to moderate relationships exist between certain reach directions on the YBT-LQ and peak torques suggesting they measure similar constructs. This information is useful as it might allow one to use certain reach distances on the YBT-LQ to help make clinical judgments regarding the functional strength of the quadriceps and hamstrings. It also suggests that not all who perform poorly on the YBT-LQ will have poor torque output or that all who are weak, as measured using isokinetic testing, will fail the YBT-LQ. Those who do perform poorly on isokinetic testing and well on the YBT-LQ may have learned to adapt to strength deficits to better perform functionally. Conversely, those who perform well on isokinetic testing but poorly on functional testing may have other limitations that need to be addressed such as poor dorsiflexion range of motion or decreased balance and neuromuscular control.2,3,7,10,13,17
Reach Asymmetries
It is important to understand what role asymmetries in both functional movement and isolated strength play in injury risk and readiness to return to sport. Plisky et al. found that an anterior reach difference of 4 cm or more or a composite score less than or equal to 94% of leg length for women on the SEBT during a pre-participation athletic screening was a predictor of lower extremity injury.15 In a study examining risk factors for injuries in female soccer players, Soderman et al. found that of the five players who had sustained an ACL injury, all had a lower HQ ratio on the ACL-injured side than on their non-injured side.24 While the current study is retrospective in nature, and unable to provide predictive value regarding injury risk based on previously measured asymmetries, this data does demonstrate that asymmetries remain up to 12 months after ACL reconstruction. Secondary analysis examined a subset of athletes who demonstrated a meaningful clinical asymmetry identified by the current literature. Based on previous studies an asymmetry of more than 4 cm on the anterior reach component is considered “at risk” and for the purpose of this study served to define a low performer on YBT-LQ14,15. Conversely, a high performer was defined as no greater than 1 cm anterior reach asymmetry. Subgroups of high and low performers allowed further investigation into how quadriceps or hamstring strength may impact performance on the YBT-LQ. Analysis of these subgroups revealed a greater deficit in knee extensor torque in those who were low YBT-LQ performers. High performers had a lower knee extensor torque deficit suggesting that quadriceps strength may influence performance on this component of the YBT-LQ. However, this is only present in the subgroups and not the group as a whole. Additional factors beyond quadriceps and hamstring strength contribute to performance on the YBT-LQ which, as intended by its creators, incorporates range of motion, closed chain stabilization, and balance in addition to strength.
Limitations
As with any study, limitations exist in the current report. First, because this investigation was conducted as a retrospective review, there are inherent limitations in the study design. For one, retrospective reviews can only study associations and not causality. Second, the investigators must rely on others, in this case multiple clinicians and researchers, for accuracy of conduct and reportingat the time of documentation. An additional limitation of this study is a small sample size with more males (29) than females (16). Thus, care should be taken when applying the study results to a larger heterogeneous population. Lastly, while the YBT-LQ is a derivative of the SEBT and the two are closely related, they are not interchangeable.25 Therefore, care must be taken when applying the results of this study to performance on the SEBT which may be more clinically affordable than the YBT-LQ. Similarly, alternative methods of strength testing, such as hand held dynamometry or one repetition maximum, should be compared with caution as these methods were not included in the current study.
CONCLUSIONS
Both the YBT-LQ and isokinetic testing may be administered independently to examine for performance and torque deficits in the ACL reconstructed population. Based on the relationships reported in this study, anterior reach asymmetry and extension torque deficit in ACL reconstructed knees are related. Individual reach distances and peak knee extension and flexion torques demonstrate stronger relationships in the involved knee versus the uninvolved knee. This suggests that, in ACL reconstructed patients, knee extensor and flexor strength is related to Y-Balance performance but cannot fully explain observed deficits. Neither test, in isolation can stand-alone and the combination of both functional and strength testing should be included in return to sport examination and assessment.
REFERENCES
- 1.Mayer SW Queen RM Taylor D, et al. Functional testing differences in anterior cruciate ligament reconstruction patients released versus not released to return to sport. Am J Sports Med. 2015;43(7):1648-55. [DOI] [PubMed] [Google Scholar]
- 2.Barber-Westin SD Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697-1705. [DOI] [PubMed] [Google Scholar]
- 3.Di Stasi S Myer GD Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777-792, A1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright RW Preston E Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I: continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21(3):217-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen W Zantop T. Return to play following ACL reconstruction: survey among experienced arthroscopic surgeons (AGA instructors). Arch Orthop Trauma Surg. 2013;133(7):969-77. PubMed PMID: 23604790. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL Webster KE Taylor NF, et al. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2011;39(3):538-543. [DOI] [PubMed] [Google Scholar]
- 7.Thomeé R Kaplan Y Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798-1805. [DOI] [PubMed] [Google Scholar]
- 8.Wells L Dyke JA Albaugh J, et al. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. 2009;29(5):486-489. [DOI] [PubMed] [Google Scholar]
- 9.Andrade MDS De Lira CAB Koffes FDC, et al. Isokinetic hamstrings-to-quadriceps peak torque ratio: the influence of sport modality, gender, and angular velocity. J Sports Sci. 2012;30(6):547-553. [DOI] [PubMed] [Google Scholar]
- 10.Goradia VK Grana WA Pearson SE. Factors associated with decreased muscle strength after anterior cruciate ligament reconstruction with hamstring tendon grafts. Arthroscopy. 2006;22(1):80-88. [DOI] [PubMed] [Google Scholar]
- 11.Zwolski C Schmitt LC Quatman-Yates C, et al. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(9):2242-9. [DOI] [PubMed] [Google Scholar]
- 12.Gorman PP Butler RJ Rauh MJ, et al. Differences in dynamic balance scores in one sport versus multiple sport high school athletes. Int J Sports Phys Ther. 2012;7(2):148-53. [PMC free article] [PubMed] [Google Scholar]
- 13.Padua DA DiStefano LJ Beutler AI, et al. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589-95). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plisky PJ Gorman PP Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports PhysTher. 2009;4(2):92-99. [PMC free article] [PubMed] [Google Scholar]
- 15.Plisky PJ Rauh MJ Kaminski TW, et al. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911-919. [DOI] [PubMed] [Google Scholar]
- 16.Butler RJ Lehr ME Fink ML, et al. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 20135(5):417-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Noronha M França LC Haupenthal A, et al. Intrinsic predictive factors for ankle sprain in active university students: a prospective study. Scand J Med Sci Sports. 2013;23(5):541-7. [DOI] [PubMed] [Google Scholar]
- 18.Booysen MJ Gradidge PJ Watson E. The relationship of eccentric strength and power with dynamic balance in male footballers. J Sport Sci. 2015;33(20):2157-65. [DOI] [PubMed] [Google Scholar]
- 19.Earl JE Hertel J. Lower-extremity muscle activation during the star excursion balance test. J Sport Rehabil. 2001;10:93-104. [Google Scholar]
- 20.Norris B Trudelle-Jackson E. Hip- and thigh-muscle activation during the star excursion balance test. J Sport Rehabil. 2011;20:428-441. [DOI] [PubMed] [Google Scholar]
- 21.Cardone C Menegassi Z Emygdio R. Isokinetic assessment of muscle strength following anterior cruciate ligament reconstruction. Isokinet Exerc Sci. 2001;12(3): 173-177. [Google Scholar]
- 22.HUMAC/NORM Testing and Rehabilitation System: Operator's Manual. Stoughton, MA: Computer Sports Medicine Incorporated; 2005.
- 23.Cohen J. (1988), Statistical Power Analysis for the Behavioral Sciences, 2nd Edition Hillsdale, N.J.: Lawrence Erlbaum. [Google Scholar]
- 24.Söderman K Alfredson H Pietilä T, et al. Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):313-21. [DOI] [PubMed] [Google Scholar]
- 25.Coughlan GF Fullan K Delahunt E, et al. A comparison between performance on selected directions of the Star Excursion Balance Test and Y balance Test. J Athl Train. 2012;47(4):366-371. [DOI] [PMC free article] [PubMed] [Google Scholar]