Abstract
Background
Return to activity decisions after anterior cruciate ligament reconstruction (ACL-R) are limited by functional performance tests often performed in a non-fatigued state. Fatigue can improve test sensitivity, but current methods to induce fatigue are typically bilateral tasks or focus on the quadriceps muscle in isolation.
Hypothesis/Purpose
To determine the effects of a two-minute lateral step-down fatigue test compared to a 30-second side-hop test on single-leg forward hop distance in healthy individuals. It was hypothesized that participants would demonstrate decreased hop distance with both tests, but the two-minute lateral step-down fatigue test would result in greater deficits in single-leg forward hop distance.
Study Design
Randomized crossover
Methods
Twenty healthy participants (16 females, 4 males; age = 23.7±3.0 years, height = 153.8±36.2 cm; mass = 64.4±12.8 kg; Tegner = 6.8±1.2) were asked to perform single-leg forward hop for distance pre- and post-fatigue. Participants were randomly assigned to one of the two fatigue tests, 30-second side-hop or 2-minute lateral step-down test, during the first visit. They returned within a week and performed the same sequence of tests but underwent whichever fatigue test was not assigned at the prior visit.
Results
There was a significant decrease (p < 0.001) in single-leg forward hop distance following the 30-second side-hop test (pre = 134.1±23.7 cm, post = 126.2±24.4 cm) and the two-minute lateral step-down test (pre = 135.0±26.1 cm, post = 122.7±27.4 cm). The decrease in hop distance was significantly greater (p < 0.001) for the two-minute lateral step-down test compared to the 30-second side-hop test.
Conclusion
The two-minute lateral step-down test resulted in a greater decrease in hop performance compared to the 30-second side-hop test. The results establish a threshold for expected changes that occur in a healthy population and that can then be compared with an injured athlete population. The two-minute lateral step-down exercise may be an effective method of inducing fatigue to better mimic performance in a sports environment to inform return-to-sport decisions.
Level of Evidence
Level 1b- Therapy
Keywords: Anterior cruciate ligament reconstruction, fatigue, knee, rehabilitation, return to sport
INTRODUCTION
The knee is the most commonly injured joint by adolescents, with about 2.5 million injuries per year in the United States.1 Estimates for anterior cruciate ligament (ACL) tears can range anywhere from 100,000 to up to 250,000 injuries per year; approximately 75% of those injuries result in ACL reconstruction (ACL-R).2 Decisions regarding return to activity following ACL-R are partially informed by a battery of functional performance tests, consisting of a range of jumping tasks and strength measurements.3,4 These functional performance tests typically include, but are not limited to, vertical jump, triple hop, and single-leg forward hop.5,6 The single-leg forward hop test is one of the most commonly used functional performance tests to measure the abilities of an individual in the later phases of rehabilitation post-injury.4,7 Despite wide use, the single-leg forward hop test has relatively poor psychometric properties (sensitivity = 52%, specificity = 97%, +LR = 17.33, -LR = 0.49), reducing the ability to identify abnormal symmetry (LSI <85%) between limbs after ACL injury.5
Fatigue may play a role in ACL injury risk, as rates tend to be higher toward the end of competition (e.g., second half, last quarter).8,9 A limitation of current functional performance test batteries is that they are often performed under non-fatigued conditions and may not be of sufficient demand to identify limb asymmetries.7 Although athletes following ACL-R are thought to be resistant to quadriceps fatigue in isometric conditions,10,11 they demonstrate deficits in explosive strength12 and endurance with dynamic contractions.13 While the role of fatigue is not fully understood, it has been shown to have mixed effects on coordination and motor control14 and single-leg forward hop distance.6 These mixed effects seen with the incorporation of fatigue may be due to lack of uniformity in fatigue protocols,14 which may not facilitate enough fatigue to produce the biomechanical changes associated with increased risk for non-contact ACL injuries. Fatigue protocols often involve both limbs at the same time (e.g., agility drills, repeated squats or jumping, running),14 limiting between-side comparisons. An alternative is to induce unilateral fatigue. In two previous studies, participants completed a single-leg extension task until failure at 50% or 80% of a one repetition maximum (1RM).6,15 This test has been shown to be reliable15 and results in decreased single-leg forward hop distance in both healthy15 and ACL-R populations.6 The addition of fatigue also improves the psychometric properties of the single-left forward hop test. Prior to fatigue, all individuals with a history of ACL-R demonstrated normal single-leg forward hop symmetry values (LSI ≥90%), but following fatigue, 68% of the participants demonstrated relevant impairments in hop symmetry (LSI <90%).6 This suggests that test sensitivity can be improved with the addition of a fatigue protocol. However, this approach has limitations: a leg extension machine may not be available in all clinical settings and the task only focuses on a single muscle, which is not reflective of sport demands. Although it is known that quadriceps muscle strength is an important outcome measure following ACL-R, it is not the only muscle group fatigued during physical activity; thus, a more global approach to fatigue may better simulate sports-related fatigue.
Several single-leg tasks have been used to provide insights into movement impairments following knee injury, including the side hop and lateral step-down.16,17 While these tests have not been used to specifically induce fatigue, both provide an anaerobic challenge and utilize minimal equipment. It is necessary to develop methods to effectively fatigue individuals in a manner that is more clinically pragmatic but still relevant (i.e., without the use of equipment), and can provide greater insight into rehabilitation progress and return-to-sport decision making. It is necessary to first determine whether either of these tests will impact single-leg hop performance, prior to introducing in a clinical population. Therefore, the purpose of this study was to determine the effects of a two-minute lateral step-down fatigue test compared to a 30-second side-hop test on single-leg forward hop distance in healthy individuals. It was hypothesized that participants would demonstrate decreased hop distance with both tests, but the two-minute lateral step-down fatigue test would result in greater deficits in single-leg forward hop distance due to the longer duration of the test and greater demands on lower extremity musculature.
METHODS
A randomized crossover design was used. Each participant performed one of two fatigue interventions, determined by a randomized table, during the first session and performed the other fatigue intervention during the second session, with three to seven days between testing sessions. The same investigator obtained measures during each session. The study was reviewed for ethical considerations and approved by the Institutional Review Board at Creighton University (IRB 959318). All participants completed an approved informed consent form, compliant with the Declaration of Helsinki, prior to study enrollment.
Twenty healthy participants (16 females, 4 males; age = 23.7±3.0 years, height = 153.8±36.2 cm; mass = 64.4±12.8 kg; Tegner = 6.8±1.2) volunteered for this study. Inclusion criteria included age 19-40 years, no history of knee surgery, and a Tegner Activity Scale score >5 (heavy labor, competitive endurance sports, recreational sports- jogging on uneven ground at least twice weekly). Exclusion criteria included traumatic spine or lower extremity injury within the prior six months and inability to give consent or understand the experimental procedures. All participants completed a standardized health history form and the Tegner Activity Scale. Each session started with a five-minute warm up consisting of jogging on a treadmill at a self-selected speed and three single-leg vertical jumps with the dominant limb, defined as the preferred jumping limb (e.g., basketball layup), followed by the non-dominant limb. The single-leg vertical jump was performed as part of a separate reliability study.
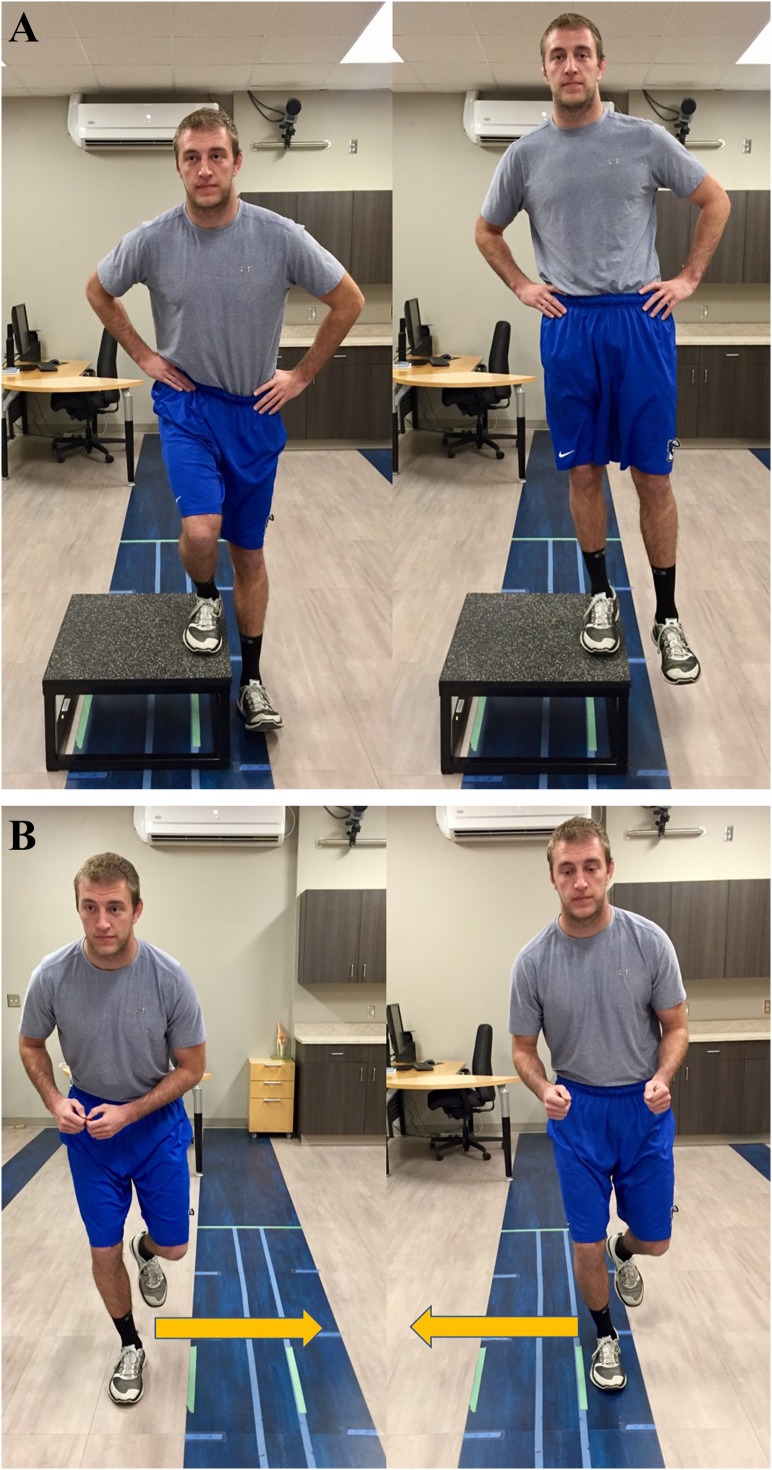
The study protocol consisted of three parts: pre-fatigue evaluation, fatigue intervention, and post-fatigue evaluation. First, participants performed the single-leg hop for distance (Figure 1).5,17 They were instructed to hop as far forward as possible with a controlled single-limb landing, defined as maintaining position on a single leg for two to three seconds. A loss of balance or placing the contralateral limb on the ground to maintain support was determined to be a failed trial and the trial was repeated. The first trial was used as a warm-up and the maximum single-leg hop distance (cm) of trials two and three was used for data analysis. The dominant limb was tested prior to the non-dominant limb. Single-leg hop for distance has good within-session reliability (ICC = 0.98),15 good between-session reliability (ICC = 0.92 to .95),18,19 and an established minimal detectable change of 8.1% for the limb symmetry index19 and 13-14 cm for absolute single-leg hop distance.18
Figure 1.
Single-leg forward hop test starting and finish position. The orange arrow indicates hop direction.
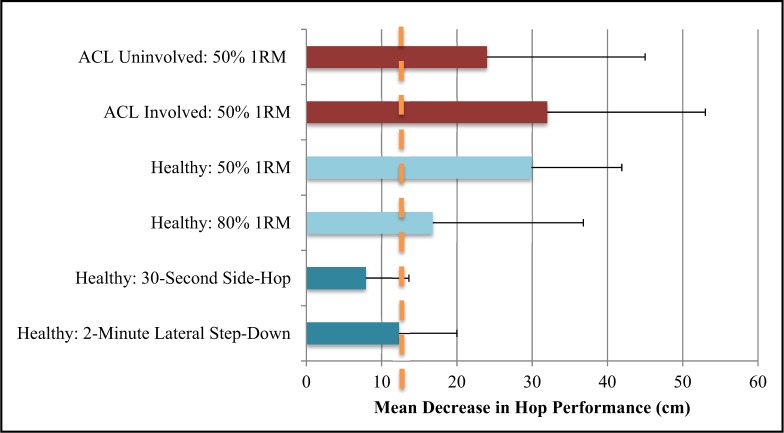
Next, participants were randomized to either a 30-second side-hop (Figure 2A) test or two-minute lateral step-down test (Figure 2B). The 30-second side-hop test required participants to jump as many times as possible over two parallel strips of tape placed 40 cm apart on the floor.17 An unsuccessful jump was defined as touching the tape or the area inside the tape. The two-minute lateral step-down test required participants to perform a unilateral step-down from a 30.5 cm box (12-inches), tapping their heel to the floor each time, and completing this as many times as possible for two minutes. The number of step downs and side hops performed was recorded for descriptive purposes. Immediately following the fatiguing intervention, participants performed the single-leg hop for distance three more times, using the same protocol as the pre-fatigue measures. Following a three to five minute rest, participants repeated the same protocol (pre-fatigue, fatigue exercise, and post-fatigue) on the opposite limb. Participants returned three to seven days later and performed the same sequence of tests, but performed the fatigue test, which was not performed at the prior visit.
Figure 2.
A) 30-second side-hop, B) 2-minute lateral step-down test starting and finish position. The orange arrow indicates hop direction.
Sample size was based on a previous study15 utilizing an isolated quadriceps fatigue exercise to decrease single-leg forward hop distance (mean change = 10 cm, SD = 15) in healthy individuals. It was determined that at least 16 participants were necessary in order to detect a significant (α = .05, 1-β = .80) change in single-leg forward hop distance following the fatigue protocol. The independent variables included the fatigue test (30-second side hop, two-minute lateral step-down), time (pre-test, post-test), and side (dominant, non-dominant). The dependent variable was single-leg forward hop distance (cm). Descriptive statistics, including frequency counts, were calculated for the outcome variables. A mixed model ANOVA was used to determine differences between sides and pre- and post-test measures for each fatigue test. A separate paired t-test was used to determine differences in hop test performance between tests using the average of the dominant and non-dominant limbs. Statistical significance was set a priori at p <0.05. Effect sizes (Cohen’s d) were calculated for outcome variables using the mean difference between pre- and post-test trials and the pooled standard deviation. Effect sizes were interpreted as follows: small (.20), moderate (.50), and large (.80).20
RESULTS
There was not a significant interaction (side x time) for the 30-second side-hop test (p = 0.86) or the two-minute lateral step-down test (p = 0.33). The dominant limb demonstrated significantly greater (p< 0.05) single-leg forward hop distance compared to the non-dominant limb for both tests. Both fatigue tests significantly decreased (p <0.001) single-leg forward hop distance (Table 1), but the magnitude of this decrease was significantly greater (p <0.001) with the two-minute lateral step-down test compared to the 30-second side-hop test (Table 1). The frequency of observed changes in single-leg forward hop distance following fatiguing exercise is provided in Figure 3. Effect sizes were considered small to moderate for changes in single-leg forward hop distance following the 30-second side-hop test (d = -0.33) and the two-minute lateral step-down test (d = -0.46). The 30-second side-hop test resulted in decreased single-leg hop distance exceeding the 13 cm minimal detectable change in 15% of the trials, compared to 40% of the trials after the two-minute lateral step-down test.
Table 1.
Single-limb forward hop distance (cm) mean values (SD) before and after fatigue intervention.
| Pre-Fatigue | Post-Fatigue | Change in Hop Distance | |||||
|---|---|---|---|---|---|---|---|
| Dominant | Non-Dominant* | Average | Dominant | Non-Dominant | Average | ||
| 30-Second Side Hop | 137.0 (25.0) | 131.3 (22.9) | 134.1 (23.7) | 128.9 (25.5) | 123.5 (24.3) | 126.2 (24.4)† | 8.0 (3.4)‡ |
| 2-Minute Lateral Step-Down | 137.9 (26.4) | 132.0 (27.3) | 135.0 (26.1) | 124.1 (23.7) | 120.7 (28.7) | 122.7 (27.4)† | 12.3 (6.5)‡ |
significant difference (p< .05) in single-limb forward hop distance between dominant and non-dominant limbs
significant decrease in single-limb forward hop distance post-fatigue compared to pre-fatigue (p <0.001)
significant difference between fatigue tests (p <0.004)
Figure 3.
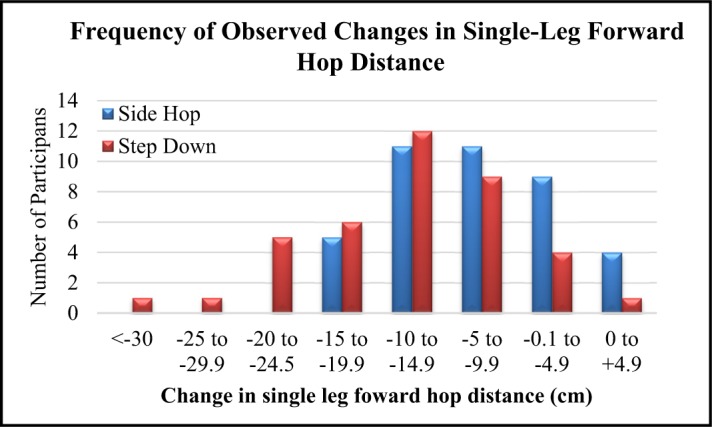
Frequency of observed changes in single-leg forward hop distance following fatiguing exercise.
DISCUSSION
The purpose of this study was to determine the effects of a two-minute lateral step-down fatigue test compared to a 30-second side-hop test on single-leg forward hop distance in healthy individuals. The results confirmed our hypothesis that both fatigue tests would decrease single-leg forward hop performance, and that the two-minute lateral step-down test resulted in a significantly greater decrease in single-leg hop performance compared to the 30-second side-hop test. The two-minute lateral step-down test resulted in not only a greater average change from pre- to post-testing relative to the 30-second side-hop test (12.3 cm versus 8.0 cm), but also a larger effect size (-0.46 versus -0.33), allowing interpretation of the magnitude of this change. Thus, the current study provides evidence that single-leg forward hop distance is negatively impacted by the fatigue tests.
Currently, return-to-sport protocols include functional hop tests, as well as objective quadriceps strength measures, in the clinical decision-making tree of returning athletes to sport after ACL-R. An LSI of >85-90% has been established as sufficient criteria to begin a return-to-sport progression.21 Limb dominance may impact LSI as the dominant limb demonstrated significantly greater single-leg forward hop performance compared to the non-dominant limb (Table 1). This finding is supported by previous work22 and suggests that LSI values after knee injury may be influenced by limb dominance. Although athletes may reach a single-limb forward hop LSI >85-90%, it is possible this threshold may not be sufficient, as deficits in quadriceps strength and altered landing biomechanics may still be present at return to sport.6,23,24 These deficits may persist for years, leading to increased risk of re-injury23,25,26 and an earlier onset of knee osteoarthritis.27 The addition of testing single-leg forward hop performance in a fatigued state has been shown to improve the sensitivity of single-leg forward hop LSI,6 allowing a more accurate representation of the presence of asymmetry. Previous research demonstrated that, prior to fatigue, all individuals with a history of ACL-R demonstrated normal single-leg forward hop symmetry values (LSI >90%), but following fatigue, 68% of the participants demonstrated relevant impairments in hop symmetry (LSI <90%).6 This indicates that a non-fatigued single-leg forward hop LSI greater than 90% may not be a sufficient cut-off to allow athletes to return to sport.6,28 Adding a unilateral fatigue test may improve our ability to detect clinically meaningful differences between limbs for single-leg forward hop performance that may not be expressed in non-fatigued hop testing conditions.6
There are two potential advantages of using the 30-second side-hop or the two-minute lateral step-down fatigue tests as opposed to previous fatigue protocols (i.e. leg extensor machine testing). The first is that there is strong potential of more effectively detecting strength and functional deficits post-ACL-R.6 A second benefit is that both fatigue tests may also provide insights into anaerobic performance differences between limbs or in comparison to healthy controls.17,29,30 The side-hop test has been utilized as an endurance task and used to differentiate between performance of the involved and uninvolved limb following ACL injury and reconstruction.17 As the quadriceps and other lower extremity muscles fatigue, this test can provide critical insights into what the knee can potentially withstand during sport. The lateral step-down test has been used clinically to examine performance as well as movement quality.16,31 The authors’ application of the lateral step-down test included two minutes per limb versus five repetitions16 or three minutes31 which have been used in previous studies. The decreases in single-leg forward hop distance after fatigue demonstrate potential for the fatigue test to decrease jumping performance. Although the number of repetitions performed for each of the tests was monitored, other measures were not captured to better quantify fatigue (e.g., rating of perceived exertion, electromyography). Previous studies6,15 have performed a unilateral leg-extension task at 50% or 80% of 1RM until failure to fatigue the quadriceps muscle.6,15 This resulted in a 17 cm decrease in hop performance for healthy individuals (Figure 4). Greater deficits following fatigue are seen in individuals with a history ACL-R on both the involved (30 cm) and uninvolved limb (25 cm).6,15 The minimal detectable change of the single-leg forward hop test is 13-14 cm,18 which indicates that changes less than 13-14 cm cannot be differentiated from measurement error and should be viewed with caution. While the 12 cm decrease in forward hop distance was close to the minimal detectable change, there is a compelling potential that when applied in a population with ACL-R, results would yield those that would be comparable to that of the leg-extensor fatigue test (Figure 4) at 80% of a 1RM which resulted in approximately 17 cm decrease in forward hop distance.6,15 As seen in Figure 4, healthy participants (blue bars) had decreases in forward hop performance that were lower in magnitude compared to participants with a history of ACL reconstruction (red bars). Future studies should determine changes in single-leg forward hop distance following the fatigue protocols, outlined in the current study, for individuals with a history of ACL-R. The two-minute lateral step-down test and 30-second side-hop test offer a more pragmatic solution, as compared to current fatigue methods, to implementing fatigue testing in the clinic. Both require minimal time and equipment (30.5 cm step, stopwatch) and are relatively inexpensive compared to a leg-extension machine. Not only are these tests clinically useful, but also are more functional evaluative tests. During sporting activity quadriceps fatigue does not occur in isolation, but involves both central and peripheral mechanisms.32 It is also possible that avoidance patterns or compensatory strategies may be utilized to allow task completion and preserve quadriceps function. Individuals with a history of ACL reconstruction have been shown to rely more heavily on contributions from the hip and ankle to offset decreased contributions from the knee when performing a vertical jump33 or single-leg forward hop.34 Although the side-hop or lateral step down may be considered more functional-type tasks, compensatory strategies to preserve quadriceps function would not be able available during a strictly knee extensor fatigue protocol. Future research should focus on the use of fatigue tests in athletes following ACL-R, as well as the use of 3-D motion capture and/or electromyographic (EMG) data to investigate the compensatory strategies individuals with a history of ACL-R use when fatigued.15,33,35 This information may better determine which type of fatigue protocol provides to most relevant information to inform return to sport decisions.
Figure 4.
Results of mean decrease in hop performance of our study and adapted data from Augustsson et al. Shades of blue indicate healthy subject values, shades of red indicate non-healthy values. Values shown are in centimeters of change in hop distance between pre-and post-fatigue of fatigue protocols. The vertical line indicates the minimal detectable change 13-14 cm.18
A limitation of this study was that only young, healthy individuals were included, consisting of a greater number of female participants. It is known that females may demonstrate a different fatigue profile than males.36,37 Future studies should employ a more balanced recruitment of female and male participants and of sufficient sample size to allow between sex comparisons. A second limitation was that the order of limb testing was not randomized. Instead, the authors elected to test the dominant limb prior the non-dominant limb, a method used in previous studies.38,39 There is little consensus regarding an appropriate testing sequence for injured (involved then uninvolved; randomized) or healthy participants (right then left, dominant then non-dominant, randomized). A third limitation was that time-anchored tests (30 seconds, 2 minutes) were used that did not include a subjective or objective measure of fatigue such as rating of perceived exertion40,41 or changes in quadriceps EMG profile.37 It could be possible for a participant to not provide full effort during the fatigue test, which would then underestimate likely changes in single-leg forward hop performance. The data provided by this study and future studies can give clinicians greater insight into the challenges associated with athletes post-ACL-R, as well as provide a more thorough return to pre-injury levels of performance in order to reduce the likelihood of re-injury and promote a safe and smooth return to sport.
CONCLUSION
Return-to-sport/activity decisions are informed by a battery of functional and strength tests that are typically performed in a non-fatigued state, which may inaccurately determine whether an athlete is fully ready to return to sport. Fatiguing exercise is thought to better identify asymmetries in single-limb forward hop performance, as demonstrated previously with a leg-extensor fatigue test. This results of the current study indicate that the two-minute lateral step-down test has the ability to significantly decrease hop performance in a healthy population, and that these decreases are comparable to changes observed in a healthy population with the leg-extensor fatigue test (Figure 4). Even more so, the two-minute lateral step-down test is a more pragmatic solution to testing athletes in a fatigued state as compared to a leg-extension machine because it is inexpensive and targets the muscles of the entire lower extremity. Future research should evaluate the use of the two-minute lateral step-down test as a fatiguing protocol for persons following ACL-R to make appropriate determinations for return-to-sport readiness.
REFERENCES
- 1.Simon TD Bublitz C Hambidge SJ. Emergency department visits among pediatric patients for sports-related injury: Basic epidemiology and impact of race/ethnicity and insurance status. Pediatr Emerg Care. 2006;22(5):309-315. [DOI] [PubMed] [Google Scholar]
- 2.Sanders TL Maradit Kremers H Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. 2016;44(6):1502-1507. [DOI] [PubMed] [Google Scholar]
- 3.Barber-Westin SD Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697-1705. [DOI] [PubMed] [Google Scholar]
- 4.Engelen-van Melick N van Cingel REH Tijssen MPW Nijhuis-van der Sanden MWG. Assessment of functional performance after anterior cruciate ligament reconstruction: A systematic review of measurement procedures. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):869-879. [DOI] [PubMed] [Google Scholar]
- 5.Noyes FR Barber SD Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513-518. [DOI] [PubMed] [Google Scholar]
- 6.Augustsson J Thomeé R Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004/09/01 2004;12(5):350-356. [DOI] [PubMed] [Google Scholar]
- 7.Abrams GD Harris JD Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: A systematic review. Orthop J Sports Med. 2014;2(1) 2325967113518305. 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris JD Erickson BJ Bach BR, et al. Return-to-sport and performance after anterior cruciate ligament reconstruction in National Basketball Association players. Sports Health. 2013;5(6):562-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montgomery C Blackburn J Withers D Tierney G Moran C Simms C. Mechanisms of ACL injury in professional rugby union: A systematic video analysis of 36 cases. Br J Sports Med. 2016; pii bjsports-2016-096425. 10.1136/bjsports-2016-096425. [DOI] [PubMed] [Google Scholar]
- 10.Snyder-Mackler L Binder-Macleod SA Williams PR. Fatigability of human quadriceps femoris muscle following anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 1993;25(7):783-789. [DOI] [PubMed] [Google Scholar]
- 11.McHugh MP Tyler TF Nicholas SJ Browne MG Gleim GW. Electromyographic analysis of quadriceps fatigue after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31(1):25-32. [DOI] [PubMed] [Google Scholar]
- 12.Knezevic OM Mirkov DM Kadija M Nedeljkovic A Jaric S. Asymmetries in explosive strength following anterior cruciate ligament reconstruction. Knee. 2014;21(6):1039-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laudner K Evans D Wong R, et al. Relationship between isokinetic knee strength and jump characteristics following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2015;10(3):272-280. [PMC free article] [PubMed] [Google Scholar]
- 14.Barber-Westin SD Noyes FR. Effect of fatigue protocols on lower limb neuromuscular function and implications for anterior cruciate ligament injury prevention training. Am J Sports Med. 2017; 363546517693846. 10.1177/0363546517693846. [DOI] [PubMed] [Google Scholar]
- 15.Augustsson J Thomeé R Lindén C Folkesson M Tranberg R Karlsson J. Single-leg hop testing following fatiguing exercise: Reliability and biomechanical analysis. Scand J Med Sci Sports. 2006;16(2):111-120. [DOI] [PubMed] [Google Scholar]
- 16.Piva SR Fitzgerald K Irrgang JJ, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gustavsson A Neeter C Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778-788. [DOI] [PubMed] [Google Scholar]
- 18.Thomas C Dos’Santos T Comfort P Jones P. Between-session reliability of common strength- and power-related measures in adolescent athletes. Sports. 2017;5(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reid A Birmingham TB Stratford PW Alcock GK Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337-349. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 21.Wright RW Haas AK Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7(3):239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers BA Jenkins WL Killian C Rundquist P. Normative data for hop tests in high school and collegiate basketball and soccer players. Int J Sports Phys Ther. 2014;9(5):596-603. [PMC free article] [PubMed] [Google Scholar]
- 23.Capin JJ Khandha A Zarzycki R Manal K Buchanan TS Snyder-Mackler L. Gait mechanics and second ACL rupture: Implications for delaying return-to-sport. J Orthop Res. 2017;35(9):1894-1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmitt LC Paterno MV Ford KR Myer GD Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kyritsis P Bahr R Landreau P Miladi R Witvrouw E. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-51. [DOI] [PubMed] [Google Scholar]
- 26.Grindem H Snyder-Mackler L Moksnes H Engebretsen L Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Claes S Hermie L Verdonk R Bellemans J Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967-1976. [DOI] [PubMed] [Google Scholar]
- 28.Zwolski C Schmitt LC Thomas S Hewett TE Paterno MV. The utility of limb symmetry indices in return-to-sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(8):230-238. [DOI] [PubMed] [Google Scholar]
- 29.Fältström A Hägglund M Kvist J. Functional performance among active female soccer players after unilateral primary anterior cruciate ligament reconstruction compared with knee-healthy controls. Am J Sports Med. 2017;45(2):377-385. [DOI] [PubMed] [Google Scholar]
- 30.Gokeler A Welling W Zaffagnini S Seil R Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haitz K Shultz R Hodgins M Matheson GO. Test-retest and interrater reliability of the functional lower extremity evaluation. J Orthop Sports Phys Ther. 2014;44(12):947-954. [DOI] [PubMed] [Google Scholar]
- 32.Borotikar BS Newcomer R Koppes R McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: Central and peripheral contributions to ACL injury risk. Clin Biomech. 2008;23(1):81-92. [DOI] [PubMed] [Google Scholar]
- 33.Ernst GP Saliba E Diduch DR Hurwitz SR Ball DW. Lower-extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000;80(3):251-260. [PubMed] [Google Scholar]
- 34.Orishimo KF Kremenic IJ Mullaney MJ McHugh MP Nicholas SJ. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1587-1593. [DOI] [PubMed] [Google Scholar]
- 35.Orishimo KF Kremenic IJ. Effect of fatigue on single-leg hop landing biomechanics. J Appl Biomech. 2006;22(4):245-254. [DOI] [PubMed] [Google Scholar]
- 36.Hunter SK. Sex differences and mechanisms of task-specific muscle fatigue. Exerc Sport Sci Rev. 2009;37(3):113-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fujisawa C Tamaki A Yamada E Matsuoka H. Influence of gender on muscle fatigue during dynamic knee contractions. Phys Ther Res. 2017;20(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xergia SA Pappas E Georgoulis AD. Association of the single-limb hop test with isokinetic, kinematic, and kinetic asymmetries in patients after anterior cruciate ligament reconstruction. Sports Health. 2015;7(3):217-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krishnan C. Are practice trials required for hop tests? Gait Posture. 2015;41(4):960-963. [DOI] [PubMed] [Google Scholar]
- 40.Benjaminse A Habu A Sell TC, et al. Fatigue alters lower extremity kinematics during a single-leg stop-jump task. Knee Surg Sports Traumatol Arthrosc. 2008;16(4):400-407. [DOI] [PubMed] [Google Scholar]
- 41.Coventry E O’Connor KM Hart BA Earl JE Ebersole KT. The effect of lower extremity fatigue on shock attenuation during single-leg landing. Clin Biomech. 2006;21(10):1090-1097. [DOI] [PubMed] [Google Scholar]