Abstract
Context:
Health-related quality of life (HRQL) is an important outcome measure for various diseases, although there are sparse data regarding HRQL among Indian patients with hypothyroidism.
Aims:
This study aimed to assess HRQL among Indian patients with hypothyroidism using the SF-36 questionnaire.
Methods:
This cross-sectional study evaluated 244 consecutive patients with hypothyroidism who were treated at the Vydehi Institute of Medical Sciences and Research Centre in Bengaluru. All patients were >18 years old and visited the outpatient department for endocrine treatment. Perceived health status was evaluated using the SF-36 questionnaire. The patients' data were compared to data from 250 age-matched and sex-matched healthy controls.
Results:
Compared to the healthy controls, the patients with hypothyroidism had significantly lower scores for six of the eight SF-36 scales. No significant intergroup differences were observed in the “role emotional” and “social functioning” dimensions.
Interpretation and Conclusions:
Hypothyroidism was associated with reduced HRQL among Indian patients. These patients generally experienced greater reductions in physical dimensions, compared to social and emotional dimensions.
Keywords: Health-related quality of life, hypothyroidism, India, SF-36
INTRODUCTION
Health-related quality of life (HRQL) is a subjective assessment of the effects of disease and its treatment on the physical, social, psychological, and somatic dimensions of a patient's life. Thus, HRQL is considered an important supplementary outcome measure in the management of different conditions.[1] Increasing attention is being paid to assessing HRQL among patients with thyroid disorders, and previous studies have revealed that HRQL is frequently affected in patients with hypothyroidism.[2,3,4]
The Medical Outcomes Study Short-Form Health Survey (SF-36) is a widely used instrument for measuring HRQL, which consists of 36 questions regarding eight dimensions of health. This instrument has been validated in various disease states, including hypothyroidism.[5] Although the primary outcome measures for evaluating therapies are generally related to morbidity and mortality, patient-centered outcomes (e.g., HRQL) are also being considered in overall patient and therapy assessments.[6] Furthermore, HRQL is particularly important for individuals with chronic health conditions, who survive for many years after their diagnosis with significant disability and/or physical and mental limitations. In these patients, even modest changes in their disease and physical condition can have a profound effect on HRQL. Therefore, HRQL may be as important as survival for patients with many chronic health conditions.
Mood and emotional disturbances are common among patients with hypothyroidism, and these events can significantly affect HRQL. In addition, significant reductions in subjective health status are frequently reported by many patients with hypothyroidism, and these perceived reductions can persist after adequate replacement therapy. Patients with hypothyroidism can also experience reduced HRQL as a result of undue anxiety that is related to weight gain and awareness of their condition.[7] Moreover, neck enlargement and goiter development are associated with discomfort and cosmetic concerns, which can also affect HRQL. Finally, fatigue is commonly associated with hypothyroidism and is also associated with reduced HRQL. Nevertheless, there are sparse data regarding HRQL among Indian patients with hypothyroidism, and the present study aimed to evaluate these patients using the SF-36 questionnaire.
METHODS
This cross-sectional study evaluated consecutive patients with hypothyroidism who were treated at the Vydehi Institute of Medical Sciences and Research Centre in Bengaluru between October 2015 and October 2016. All patients were >18 years old and received treatment at the endocrine outpatient department. The exclusion criteria were patients with comorbid conditions, such as diabetes mellitus, ischemic heart disease, chronic renal impairment, cerebrovascular disease, and known psychological illnesses that could affect their perceived health status. The patients' data were compared to data from 250 age-matched and sex-matched healthy controls. All participants provided informed consent, and the study's protocol was approved by the Institutional Ethics Review Board.
Short-Form-36
Perceived health status was evaluated using the SF-36 questionnaire, which evaluates eight dimensions of health: disease-related limitations in physical activities, social function limitations that are caused by physical and/or emotional problems, emotional function limitations in performing work or other daily activities, physical function limitations, bodily pain, general mental health (e.g., feelings of well-being or depression), vitality (energy and fatigue), and general health perceptions. Item scores for each dimension were coded, summed, and transformed using a scale that ranged from 0 (worst possible perceived health status) to 100 (best possible perceived health status).
Data collection
All participants received a brief explanation of the study's objectives and then completed the SF-36 questionnaires. However, trained personnel were present to confirm that the questionnaires were completed and to prompt participants regarding missing data without biasing the participant's answers. Therefore, complete data were obtained for most questionnaires.
Statistical analysis
All data were recorded on a predesigned collection form and were managed using an Excel spreadsheet. Descriptive data were reported as a mean ± standard deviation. Student's unpaired t-test was used to compare mean values between the groups. Differences were considered statistically significant at values of P < 0.01.
RESULTS
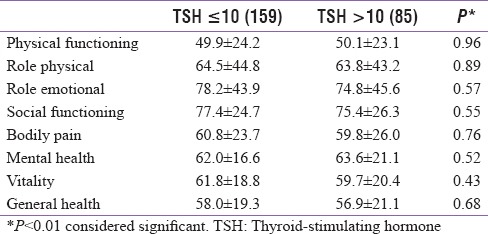
A total of 244 patients with hypothyroidism completed the questionnaire. These patients included 43 male patients (17.62%) and 201 female patients (82.37%), who had a mean age of 36.57 years. The participants' baseline demographic and clinical features are summarized in Table 1. Compared to the healthy controls, the patients with hypothyroidism had significantly lower scores for six of the eight HRQL scales [Table 2]. No significant intergroup differences were observed for the “role emotional” and “social functioning” dimensions. No significant differences in any of the eight scales were observed when we compared male and female patients [Table 3] or when we compared patients who were <40 years old and >40 years old (data not shown). Thyroid-stimulating hormone (TSH) levels were not significantly associated with the scores for any of the eight HRQL scales [Table 4].
Table 1.
Demographic and clinical characteristics of study subjects
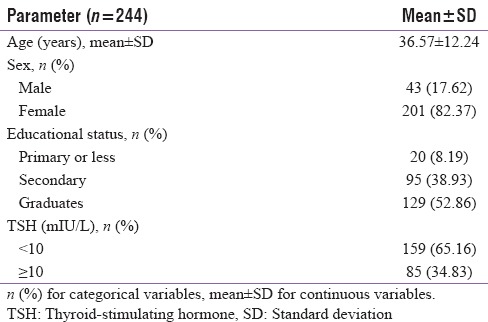
Table 2.
Comparison of health-related quality of life parameters between hypothyroid patients and healthy volunteers
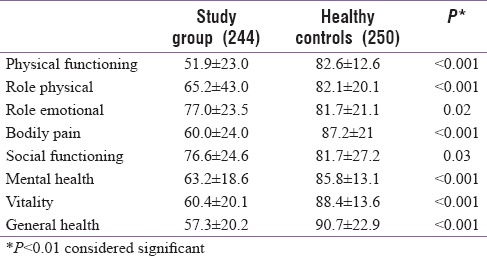
Table 3.
Comparison of health-related quality of life parameters between male and female hypothyroid patients
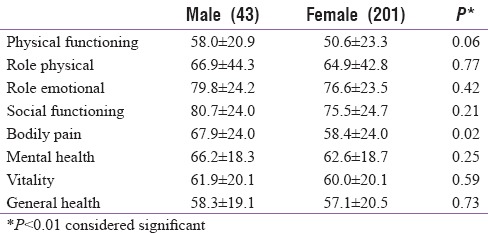
Table 4.
Comparison of health-related quality of life parameters between hypothyroid patients with thyroid-stimulating hormone less than and more than 10 mIU/L
DISCUSSION
The present study revealed that Indian patients with hypothyroidism experienced significant HRQL reductions in six of the eight SF-36 scales, compared to healthy controls. In this context, perceived health status is not merely the presence or the absence of a disease and/or its symptoms, as it incorporates broader aspects of social, physical, and emotional dimensions. Although clinicians do not commonly evaluate their patients' subjective perception of well-being, there is a growing realization that the patient's and clinician's perception of health status are equally valuable in a complete assessment of a medical condition and its outcomes.[6]
The findings of the present study agree with previous reports, as Bianchi et al. reported that 81 patients with hypothyroidism experienced significant reductions in seven of the eight SF-36 scales.[7] In addition, they observed that mood and behavioral disturbances were common among patients with hypothyroidism. Furthermore, a prospective cohort study by Winther et al. revealed that 78 patients with autoimmune hypothyroidism experienced significant reductions in seven of the eight SF-36 scales (apart from bodily pain).[8] That study also revealed that at 6 months after starting levothyroxine therapy, the patients experienced significant improvements in the SF-36 scales for role vitality, bodily pain, physical functioning, social functioning, and mental health. Another crossover trial revealed that SF-36 scores were significantly reduced at baseline and during the euthyroid and subclinical hypothyroid phases.[9] Moreover, a study of 100 patients with subclinical hypothyroidism revealed significant reductions in all eight SF-36 scales,[10] and similar findings of poor HRQL have been revealed in other studies of patients with hypothyroidism.[11,12]
Data from previous studies have revealed that the reduced HRQL of patients with hypothyroidism is often related to fatigue and mood/behavioral changes. In this context, fatigue is more commonly associated with poor physical domain scores, while behavior problems are more commonly associated with poor mental health. To a lesser extent, sleep disturbances, muscle cramps, and pruritus were found to be associated with poor HRQL among patients with hypothyroidism.[7] Tiredness is reportedly the most common symptom of hypothyroidism and is relatively severe in newly diagnosed patients.[8] Depression can also contribute to poor HRQL among patients with hypothyroidism,[8] and high TSH levels are frequently associated with depression.[13]
The present study revealed that the patients' poor HRQL persisted, even after adequate replacement therapy. Similarly, previous studies have revealed persistently poor HRQL that is related to altered energy, physical capabilities, motivation, physical appearance, and weight among patients with treated hypothyroidism.[14] The cause of this persistently poor HRQL remains unclear, although it may be partially explained by differences in levothyroxine sensitivity in the peripheral tissues and pituitary glands of patients with hypothyroidism.[15] Based on findings among patients with other conditions, poor HRQL might also be related to the patient's awareness of their disease state.[8] Alternatively, unaddressed persistent symptoms that are not attributable to hypothyroidism might contribute to the HRQL reduction. For example, obesity is frequently associated with hypothyroidism and may contribute to reduced HRQL.[11] Moreover, high titers of antibodies to thyroid peroxidase may affect psychological well-being in patients with hypothyroidism, which could lead to poor HRQL.[16,17]
Some researchers have speculated that HRQL is correlated with thyroid parameters, such as levels of TSH, free triiodothyronine, and free thyroxine. Thus, some studies have evaluated the effects of lowering serum TSH levels or a combination of liothyronine and levothyroxine in an attempt to improve HRQL among patients with hypothyroidism.[13,18,19,20,21,22,23] However, these attempts have not consistently provided improvements in measures of well-being.
Patients with a euthyroid goiter also experience reduced HRQL, which is frequently related to mood/behavior disorders, fatigue, and sleep problems.[7] In the present study, an interdomain comparison revealed that the patients had invariably lower scores for physical domains, compared to social domains. Similar results have been observed among patients with other chronic diseases.[24,25,26,27,28,29,30] It is possible that the strong family support system in India contributed to the relatively good scores in the social and environmental domains.
CONCLUSION
Indian patients with hypothyroidism had significantly poorer self-perceived health status, compared to healthy controls. Thus, it is imperative that physicians routinely assess the HRQL of patients with hypothyroidism, and target improvements in HRQL as an integral part of their hypothyroidism management strategy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.McNeil BJ, Weichselbaum R, Pauker SG. Speech and survival: Tradeoffs between quality and quantity of life in laryngeal cancer. N Engl J Med. 1981;305:982–7. doi: 10.1056/NEJM198110223051704. [DOI] [PubMed] [Google Scholar]
- 2.Aoki Y, Belin RM, Clickner R, Jeffries R, Phillips L, Mahaffey KR, et al. Serum TSH and total T4 in the United States population and their association with participant characteristics: National health and nutrition examination survey (NHANES 1999-2002) Thyroid. 2007;17:1211–23. doi: 10.1089/thy.2006.0235. [DOI] [PubMed] [Google Scholar]
- 3.Unnikrishnan AG, Kalra S, Sahay RK, Bantwal G, John M, Tewari N, et al. Prevalence of hypothyroidism in adults: An epidemiological study in eight cities of India. Indian J Endocrinol Metab. 2013;17:647–52. doi: 10.4103/2230-8210.113755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaeschke R, Guyatt G, Cook D, Harper S, Gerstein HC. Spectrum of quality of life impairment in hypothyroidism. Qual Life Res. 1994;3:323–7. doi: 10.1007/BF00451724. [DOI] [PubMed] [Google Scholar]
- 5.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) I Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 6.Leplège A, Hunt S. The problem of quality of life in medicine. JAMA. 1997;278:47–50. doi: 10.1001/jama.1997.03550010061041. [DOI] [PubMed] [Google Scholar]
- 7.Bianchi GP, Zaccheroni V, Solaroli E, Vescini F, Cerutti R, Zoli M, et al. Health-related quality of life in patients with thyroid disorders. Qual Life Res. 2004;13:45–54. doi: 10.1023/B:QURE.0000015315.35184.66. [DOI] [PubMed] [Google Scholar]
- 8.Winther KH, Cramon P, Watt T, Bjorner JB, Ekholm O, Feldt-Rasmussen U, et al. Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS One. 2016;11:e0156925. doi: 10.1371/journal.pone.0156925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samuels MH, Schuff KG, Carlson NE, Carello P, Janowsky JS. Health status, mood, and cognition in experimentally induced subclinical hypothyroidism. J Clin Endocrinol Metab. 2007;92:2545–51. doi: 10.1210/jc.2007-0011. [DOI] [PubMed] [Google Scholar]
- 10.Razvi S, Ingoe LE, McMillan CV, Weaver JU. Health status in patients with sub-clinical hypothyroidism. Eur J Endocrinol. 2005;152:713–7. doi: 10.1530/eje.1.01907. [DOI] [PubMed] [Google Scholar]
- 11.Kelderman-Bolk N, Visser TJ, Tijssen JP, Berghout A. Quality of life in patients with primary hypothyroidism related to BMI. Eur J Endocrinol. 2015;173:507–15. doi: 10.1530/EJE-15-0395. [DOI] [PubMed] [Google Scholar]
- 12.Watt T, Cramon P, Hegedüs L, Bjorner JB, Bonnema SJ, Rasmussen ŠK, et al. The thyroid-related quality of life measure thyPRO has good responsiveness and ability to detect relevant treatment effects. J Clin Endocrinol Metab. 2014;99:3708–17. doi: 10.1210/jc.2014-1322. [DOI] [PubMed] [Google Scholar]
- 13.Quinque EM, Villringer A, Kratzsch J, Karger S. Patient-reported outcomes in adequately treated hypothyroidism - insights from the German versions of thyDQoL, thySRQ and thyTSQ. Health Qual Life Outcomes. 2013;11:68. doi: 10.1186/1477-7525-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMillan CV, Bradley C, Woodcock A, Razvi S, Weaver JU. Design of new questionnaires to measure quality of life and treatment satisfaction in hypothyroidism. Thyroid. 2004;14:916–25. doi: 10.1089/thy.2004.14.916. [DOI] [PubMed] [Google Scholar]
- 15.Kalra S, Khandelwal SK. Why are our hypothyroid patients unhappy? Is tissue hypothyroidism the answer? Indian J Endocrinol Metab. 2011;15:S95–8. doi: 10.4103/2230-8210.83333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ott J, Promberger R, Kober F, Neuhold N, Tea M, Huber JC, et al. Hashimoto's thyroiditis affects symptom load and quality of life unrelated to hypothyroidism: A prospective case-control study in women undergoing thyroidectomy for benign goiter. Thyroid. 2011;21:161–7. doi: 10.1089/thy.2010.0191. [DOI] [PubMed] [Google Scholar]
- 17.Müssig K, Künle A, Säuberlich AL, Weinert C, Ethofer T, Saur R, et al. Thyroid peroxidase antibody positivity is associated with symptomatic distress in patients with hashimoto's thyroiditis. Brain Behav Immun. 2012;26:559–63. doi: 10.1016/j.bbi.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Hamilton TE, Davis S, Onstad L, Kopecky KJ. Thyrotropin levels in a population with no clinical, autoantibody, or ultrasonographic evidence of thyroid disease: Implications for the diagnosis of subclinical hypothyroidism. J Clin Endocrinol Metab. 2008;93:1224–30. doi: 10.1210/jc.2006-2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Appelhof BC, Fliers E, Wekking EM, Schene AH, Huyser J, Tijssen JG, et al. Combined therapy with levothyroxine and liothyronine in two ratios, compared with levothyroxine monotherapy in primary hypothyroidism: A double-blind, randomized, controlled clinical trial. J Clin Endocrinol Metab. 2005;90:2666–74. doi: 10.1210/jc.2004-2111. [DOI] [PubMed] [Google Scholar]
- 20.Grozinsky-Glasberg S, Fraser A, Nahshoni E, Weizman A, Leibovici L. Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: Meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2006;91:2592–9. doi: 10.1210/jc.2006-0448. [DOI] [PubMed] [Google Scholar]
- 21.Walsh JP, Ward LC, Burke V, Bhagat CI, Shiels L, Henley D, et al. Small changes in thyroxine dosage do not produce measurable changes in hypothyroid symptoms, well-being, or quality of life: Results of a double-blind, randomized clinical trial. J Clin Endocrinol Metab. 2006;91:2624–30. doi: 10.1210/jc.2006-0099. [DOI] [PubMed] [Google Scholar]
- 22.Gärtner R, Reincke M. Substitution of thyroid hormones. Internist (Berl) 2008;49(538):540–4. doi: 10.1007/s00108-008-2109-9. [DOI] [PubMed] [Google Scholar]
- 23.Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: Cosponsored by the American association of clinical endocrinologists and the American thyroid association. Endocr Pract. 2012;18:988–1028. doi: 10.4158/EP12280.GL. [DOI] [PubMed] [Google Scholar]
- 24.Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, et al. Functional status and well-being of patients with chronic conditions. Results from the medical outcomes study. JAMA. 1989;262:907–13. [PubMed] [Google Scholar]
- 25.Muniyandi M, Rajeswari R, Balasubramanian R, Nirupa C, Gopi PG, Jaggarajamma K, et al. Evaluation of post-treatment health-related quality of life (HRQoL) among tuberculosis patients. Int J Tuberc Lung Dis. 2007;11:887–92. [PubMed] [Google Scholar]
- 26.Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: A field report from south India. Soc Sci Med. 2005;60:1845–53. doi: 10.1016/j.socscimed.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Kohli RM, Sane S, Kumar K, Paranjape RS, Mehendale SM. Modification of medical outcome study (MOS) instrument for quality of life assessment & its validation in HIV infected individuals in India. Indian J Med Res. 2005;122:297–304. [PubMed] [Google Scholar]
- 28.Bedi GS, Gupta N, Handa R, Pal H, Pandey RM. Quality of life in Indian patients with rheumatoid arthritis. Qual Life Res. 2005;14:1953–8. doi: 10.1007/s11136-005-4540-x. [DOI] [PubMed] [Google Scholar]
- 29.Haroon N, Aggarwal A, Lawrence A, Agarwal V, Misra R. Impact of rheumatoid arthritis on quality of life. Mod Rheumatol. 2007;17:290–5. doi: 10.1007/s10165-007-0604-9. [DOI] [PubMed] [Google Scholar]
- 30.Ray J, Das SK, Gangopadhya PK, Roy T. Quality of life in Parkinson's disease-Indian scenario. J Assoc Physicians India. 2006;54:17–21. [PubMed] [Google Scholar]


