Abstract
Objective
To assess the long-term efficacy and safety of infliximab (IFX) treatment for refractory uveitis associated with Behçet’s disease (BD) and to identify predictors of long-term IFX therapy outcomes.
Methods
We retrospectively studied 44 consecutive BD patients with uveitis who were started on IFX therapy and analyzed the efficacy and safety of IFX and the treatment continuation rate. To determine predictors of IFX responsiveness, we analyzed the clinical characteristics of the patients who received regular maintenance therapy and those who required treatment intensification. The serum cytokine levels prior to IFX were measured through the Bio-Plex human cytokine assays.
Results
IFX significantly reduced the frequency of ocular attacks and improved the visual acuity of patients with BD-related uveitis. However, approximately half of the patients required dose escalations, necessitating a shortening of the intervals between IFX infusions due to loss of efficacy during the 5-year treatment. The frequency of ocular attacks was significantly higher in patients with complete BD than in patients with incomplete BD. A multiplex cytokine analysis revealed that patients with BD-related uveitis exhibited increased serum IL-2, IL-6, IL-8, and MCP-1 levels. Moreover, among BD patients, the serum IL-2 and IL-6 levels were particularly high in those who maintained remission and received regular IFX treatments.
Conclusion
We confirmed the long-term efficacy and tolerability of IFX in patients with BD-related uveitis. Our results indicate that complete BD may be less responsive to IFX and that the pretreatment serum cytokine profiles may be useful for predicting the long-term IFX therapy outcomes.
Keywords: Behçet’s disease, infliximab, predictive factor, uveitis
Introduction
Behçet’s disease (BD) is a recurrent systemic inflammatory disorder of unknown origin characterized by oral and genital ulcers, skin lesions, and ocular involvement. Vascular, intestinal, and central nervous system involvement are also possible but rare (1). Ocular involvement may be the most problematic complication faced by BD patients due to its severity and frequency, which reportedly ranges from approximately 50% to 70% (2). BD-related ocular disease manifests mostly as panuveitis or posterior uveitis and is characterized by recurrent attacks of intraocular inflammation that may cause cumulative intraocular structural damage and eventually lead to blindness (2). Although corticosteroids and immunosuppressants have been used to treat refractory BD and uveitis and have substantially improved patient prognoses, these conventional therapies sometimes fail to control acute episodes of BD-related uveitis, resulting in rapid disease progression and visual impairment (2, 3).
The recent advent of biologic agents, especially monoclonal antibodies against tumor necrosis factor-a (TNF-a), has facilitated the use of cytokine-targeted therapies for immune-mediated inflammatory diseases. Infliximab (IFX) is a chimeric monoclonal antibody against TNF-a and is widely used in patients with rheumatoid arthritis (RA), Crohn’s disease, psoriasis, and ankylosing spondylitis. In Japan, IFX was approved for use in BD patients with refractory uveitis in January 2007, based on promising results from multicenter clinical trials. To date, several previous studies have demonstrated the efficacy of IFX in refractory BD-related uveitis, including multicenter studies in Japan (4–9).
Several studies have also demonstrated the long-term efficacy and safety of IFX therapy in BD uveitis (6, 7). However, not all patients have been shown to respond well to treatment, and loss of efficacy may appear over time in subsets of patients who were initially responsive to therapy (10, 11). The predictors of IFX responsiveness in patients with BD-related uveitis, as well as the prognostic factor(s) of IFX responsiveness, remain unclear, and it may be important to determine whether individual patients possess characteristics associated with primary or secondary failure of IFX therapy.
In the present study, we aimed to identify the predictors of IFX treatment responses in patients with BD-related uveitis by analyzing baseline patient demographics and clinical characteristics, including patient serum cytokine profiles.
Methods
Patients
We retrospectively studied 44 consecutive patients who were treated with scheduled IFX therapy for refractory uveitis associated with BD between October 2005 and December 2014 at Kyushu University Hospital. The diagnosis of BD was made on the basis of the criteria established by the Behçet’s Disease Research Committee of, in which BD is classified as “complete” or “incomplete” according to its manifestations (12). The “complete type” is diagnosed when all four major findings occur during the course of the disease. Each patient was followed for 2 years (up to 5 years) after initiation of IFX therapy.
The exclusion criteria were recent or chronic infections, including HBV, HCV, or fungal infections or tuberculosis and serious liver, renal, cardiac or pulmonary disease or malignancy.
BD patients received intravenous infusions of IFX (5 mg/kg) at weeks 0, 2, 6, and 14 and every 8 weeks thereafter, in accordance with the treatment protocol of the Japanese Ministry of Health, Labour and Welfare. The intervals between IFX treatments could be adapted after the fourth infusion. The decision of whether to shorten the intervals between IFX treatments (treatment intensification) was made by the ophthalmologists at Kyushu University Hospital based on a disease activity assessment. The assessment of the severities of ocular attacks was made by the ophthalmologists according to the recommendations of the Standardization of Uveitis Nomenclature Working Group (13).
Patient information, such as blood test results and clinical histories, was obtained from patient medical records. Written informed consent was obtained from all patients by their physicians according to the Declaration of Helsinki, and the study has been approved by the institutional ethics committee.
Cytokine analysis
To determine the predictors of IFX effectiveness, baseline patient characteristics, laboratory data, and serum cytokine levels were assessed and compared in patients treated with the either standard protocol or with shortened intervals (dose escalation). Serum samples were collected before IFX therapy initiation and stored at −80°C. Cytokine (including some chemokines) levels were measured in serum samples using the Bio-Plex Human Cytokine Assays (Bio-Rad Laboratories, Hercules, CA, USA). The levels of the following 27 cytokines were measured: basic fibroblast growth factor (FGF), eotaxin, granulocyte colony-stimulating factor (G-CSF), granulocyte-macrophage colony-stimulating factor (GM-CSF), interferon (IFN)-g, interleukin (IL)-10, IL-12 (p70), IL-13, IL-15, IL-17, IL-1b, IL-1 receptor antagonist (IL-1ra), IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IFN-g-inducible protein (IP)-10, monocyte chemoattractant protein (MCP)-1, macrophage inflammatory protein (MIP)-1a, MIP-1b, platelet-derived growth factor (PDGF), regulated on activation, normal T-cell expressed and secreted (RANTES), TNF-a, and vascular endothelial growth factor (VEGF).
Statistical analysis
Statistical analyses were performed using JMP version 9.0 (Business Unit of SAS Inc., Cary, NC, USA). Frequency data were compared using a chi-square test. Continuous data were compared using Wilcoxon’s signed-rank test. Changes in ocular attack frequency and improvements in visual acuity from baseline were analyzed using Wilcoxon’s matched pairs signed-rank test. Time to discontinuation of IFX therapy or time to IFX interval shortening was analyzed using the Kaplan-Meier method. p values less than 0.05 were considered statistically significant.
Results
Baseline patient characteristics
Baseline patient demographics and clinical characteristics are summarized in Table 1. Of the 44 patients with BD, 36 patients (81.8%) were men and the remaining 8 (18.2%) were women. The mean age at IFX initiation was 39.1 years (range, 23–66). The mean disease duration was 4.0 years (range, 0–21). Sixteen patients (36.4%) had “complete” BD, whereas 28 (63.6%) had “incomplete” BD. HLA-A*26 and HLA-B*51 were positive in 65.5% (19/29) and 46.4% (13/28) of the patients, respectively. Corticosteroids were administered to 31.8% of the patients, and higher doses (equivalent to ≥10 mg/day prednisone) were used in 18.2% of the patients. Fourteen patients (31.8%) received concomitant treatment with immunosuppressive drugs, mainly ciclosporin A (CsA).
Table 1.
The baseline demographic and clinical characteristics of the 44 BD patients
| Age, median (range) | 39.1 (23–66) |
|---|---|
| Male/Female, % | 36/8 (81.8/18.2) |
| Disease duration, year | 4.0 (0–21) |
| Observation period, year (range) | 4.2 (0.4–8.5) |
| Complete type/Incomplete type, % | 36.4/63.6 |
| Uveitis, % | 100 |
| Aphthous ulcers, % | 88.6 |
| Genital ulcers, % | 68.2 |
| Skin lesion, % | 40.9 |
| Neuro-BD, % | 9.1 |
| Entero-BD, % | 9.1 |
| Vascular-BD, % | 6.8 |
| HLA-A*26, % | 65.5 (19/29) |
| HLA-B*51, % | 46.4 (13/28) |
| Corticosteroids, % | 31.8 |
| Colchicine, % | 59.1 |
| Immunosuppressive drugs, % | 31.8 |
| CsA, % | 20.5 |
| MTX, % | 9.1 |
| AZA, % | 2.3 |
AZA: azathioprine; BD: Behçet’s disease; CsA: ciclosporin A; MTX: methotrexate
Long-term efficacy of IFX in BD-related uveitis
Of the 44 patients with BD originally enrolled in this study, 32 patients were thoroughly followed and assessed by the ophthalmologists about the frequencies of ocular attacks and changes in visual acuity (VA) before and after treatment of IFX. The frequencies of ocular attacks in the 32 BD patients 6 months before treatment and in subsequent 6-month intervals (0–6, 6–12, 12–18, and 18–24 months) are shown in Figure 1a. IFX treatment significantly reduced the number of acute uveitis attacks from 3.28±0.32 to 0.45±0.18 during the 6 months immediately after IFX initiation (p<0.0001). In addition, this improvement was maintained up to 2 years, as the mean numbers of attacks during subsequent 6-month intervals were as follows: 0.88±0.20 from 6–12 months, 1.03±0.21 from 12–18 months, and 0.88±0.24 from 18–24 months. Of the 32 patients treated with IFX, 12 (37.5%) and 7 patients (21.9%) experienced no episodes of acute uveitis at 1 and 2 years after IFX initiation, respectively.
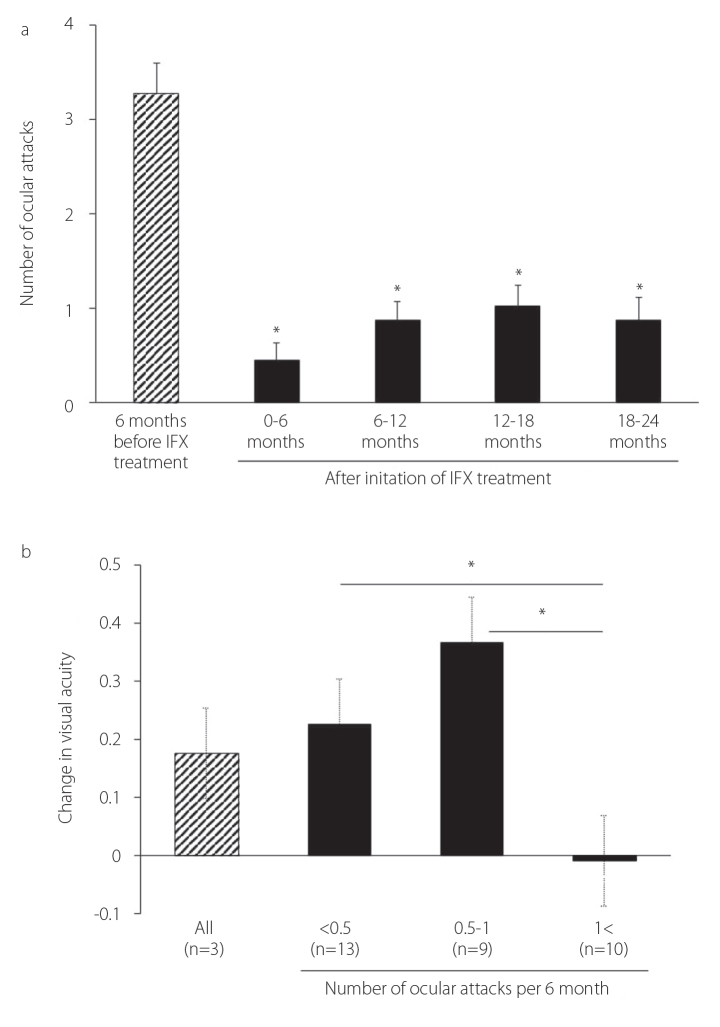
Figure 1. a, b.
IFX treatment significantly reduced the number of acute BD-related uveitis attacks bars show the mean±SEM
*p<0.0001 by Wilcoxon’s signed-rank test (a); Based on analyses of 2-year VA outcomes according to the frequencies of ocular attacks per 6 months, significant improvements in VA were noted in the groups with 1 ocular attack or less per 6 months. Bars show the mean±SEM. **p<0.01 by the Mann-Whitney U test (b)
Changes in VA after 2 years of IFX therapy are shown in Figure 1b. For analysis, the 32 patients were divided into the following three groups according to their frequencies of ocular attacks per 6 months: less than 0.5, 0.5–1, and more than 1. Significant improvements in VA were noted in the groups with less than 0.5 or 0.5–1 attacks, but not in the group with more than 1 attack per 6 months, demonstrating the existence of a strong correlation between ocular attack frequency and VA outcomes.
The continuation rate and safety of IFX therapy
The continuation rate of IFX treatment at 5 years, excluding removals, was 87.9%, as determined via the Kaplan-Meier method (data not shown). Of the 44 patients who were originally enrolled in this study, three discontinued IFX therapy because of general fatigue (n=1) and malignancies (n=2). Malignant lymphoma and thoracic carcinoma were noted in one patient each (aged 62 and 71 years, respectively) 4 years after IFX initiation. One patient developed an infusion reaction, which was mild and manageable; however, several patients developed serious infections requiring hospitalization. One patient developed bacterial colitis, whereas another patient developed pelvic inflammatory disease (PID) within 1 year after IFX therapy initiation. Interestingly, PID and bacterial enteritis developed in patients with genital ulcers and Behçet’s enteritis, respectively.
Loss of efficacy of IFX therapy and IFX infusion interval shortening
The severities and times of onset of all 87 ocular attacks in the 32 patients with BD that occurred during the 2-year follow-up period after IFX initiation are shown in Figure 2. Most ocular attacks (61/87) occurred between 6 and 8 weeks after the last IFX infusion and were more frequent during the second year following IFX initiation, suggesting that the efficacy of IFX therapy may have decreased.
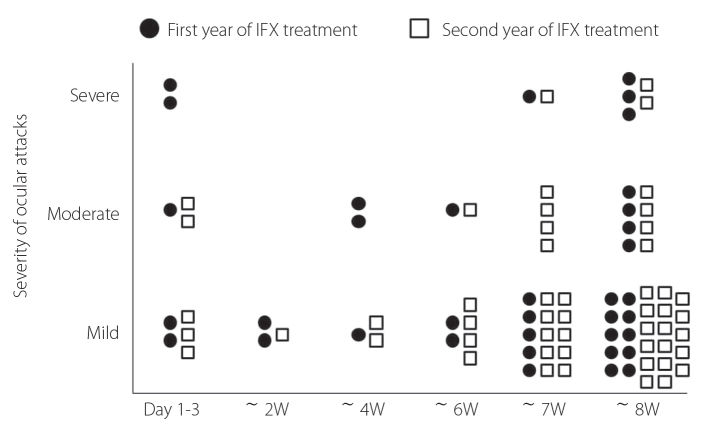
Figure 2.
Most ocular attacks occurred between the sixth and seventh weeks after the last IFX infusion and were more frequent during the second year; bars show the mean±SEM
To reduce the number of uveitis attacks in refractory patients who had experienced frequent and/or severe acute episodes, we intensified therapy by shortening the intervals between IFX treatments. An increasing number of patients was transitioned to shorter intervals between IFX treatments, i.e., treatments every 6–7 weeks, due to recurrent and refractory BD-related uveitis under standard IFX treatment (8-week intervals). The overall 1-, 3-, and 5-year continuation rates with IFX interval shortening were 9.7%, 29.6%, and 48.5%, respectively.
Prediction of responsiveness to IFX therapy
On the basis of the ophthalmologists’ judgment, we intensified therapy by shortening the intervals of IFX in refractory patients who had experienced more frequent and severe ocular attacks, which appeared to be the risk and poor prognostic factors for the outcome of VA in BD (14). Therefore, the 32 patients who continuously received IFX infusions for 2 years were divided into groups that received standard treatment at a dose of 5 mg/kg every 8 weeks (group I) and those that received treatment at a dose of 5 mg/kg every 6–7 weeks (group II). To determine the predictors of IFX responsiveness in patients with BD-related uveitis, baseline patient clinical characteristics, laboratory data, and serum cytokine levels were compared between the patients in group I (n=18) and those in group II (n=14). The disease characteristics of each group at baseline are summarized in Table 2. Comparisons between group I and group II indicate that group II had high percentages of younger patients and complete BD patients, a trend with borderline significance (p=0.07 and 0.09, respectively). There were no significant differences in disease characteristics, including HLA profiles, laboratory data, and medical treatments, between the two groups. The frequency of acute ocular attacks was significantly higher in the patients with complete BD than in the patients with incomplete BD throughout the duration of IFX treatment (12–24 months) (Figure 3), indicating that uveitis associated with complete BD is likely to be resistant to IFX treatment. There was no significant difference in HLA-B51 positivity between the patients in group I and group II.
Table 2.
Baseline disease characteristics of the groups receiving standard IFX therapy (Group I) or intensification therapy (Group II)
| Group I (n=18) | Group II (n=14) | p | |
|---|---|---|---|
| Age, median (range) | 40 (24–67) | 34 (23–50) | 0.07 |
| Disase duration, year | 5.5 (0–27) | 2.0 (0–17) | 0.25 |
| Male/Female, % | 72.2 | 85.7 | 0.75 |
| Complete type, % | 27.7 | 57.1 | 0.09 |
| Aphthous ulcers, % | 88.9 | 92.9 | 0.7 |
| Skin lesion, % | 61.1 | 71.4 | 0.54 |
| Genital ulcers, % | 38.9 | 64.3 | 0.15 |
| HLA-A*26, % | 57.1 | 72.7 | 0.41 |
| HLA-B*51, % | 46.2 | 45.5 | 0.97 |
| WBC | 8883±605 | 8420±685 | 0.88 |
| Neutrophil | 6095±670 | 5952±760 | 0.9 |
| CRP (mg/dL) | 0.37±0.15 | 0.41±0.17 | 0.27 |
| Corticosteroids (CSs), % | 22.2 | 28.6 | 0.68 |
| Average döşe of CSs (mg) | 13.1±14.6 | 16.3±9.7 | 0.73 |
| Colchicine, % | 44.4 | 64.3 | 0.54 |
| Immunosuppressive drugs, % | 16.7 | 35.7 | 0.22 |
CRP: C-reactive protein; CS: corticosteroid; WBC: white blood cell
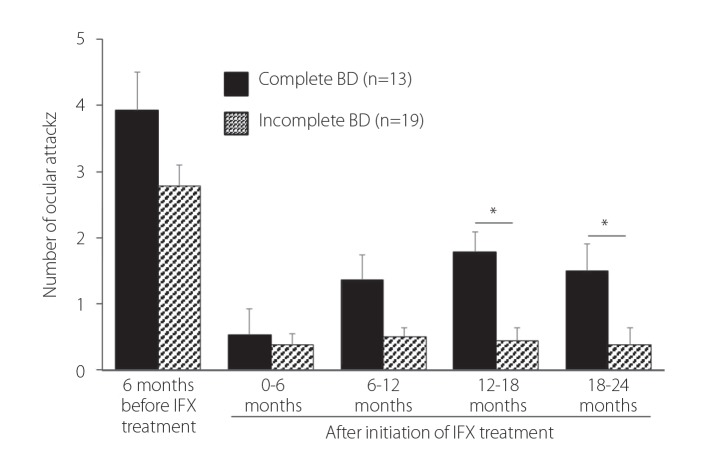
Figure 3.
The frequency of acute ocular attacks was significantly higher in patients with complete BD than in patients with incomplete BD during the second year of IFX treatment; bars show the mean±SEM
*p<0.05 by the Mann-Whitney U test
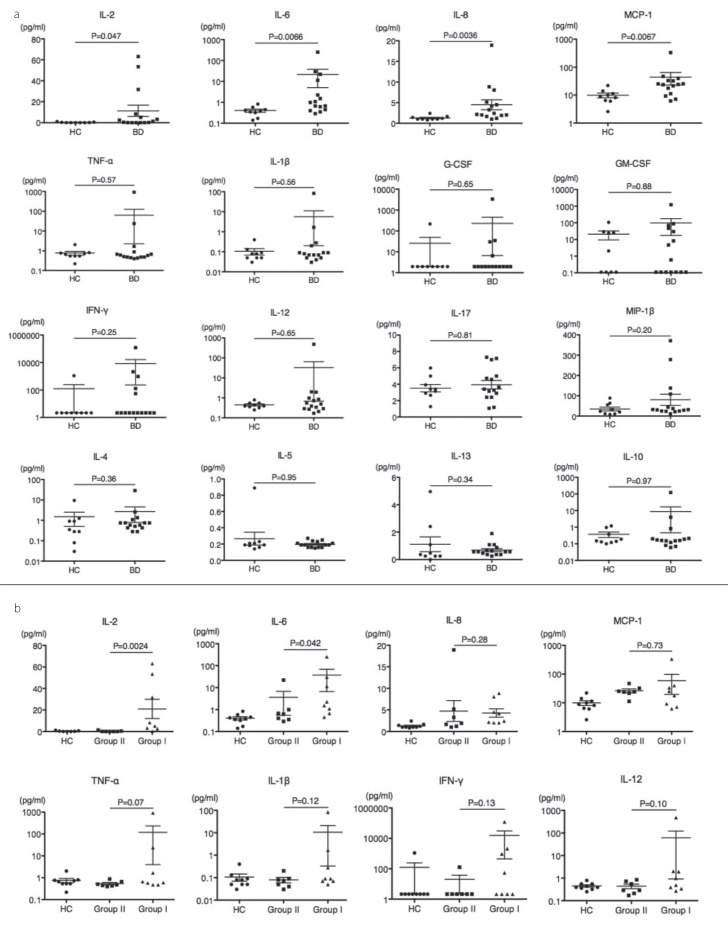
Using serum samples collected before IFX initiation, we measured the levels of 25 serum cytokines using the Bio-Plex human cytokine assays in nine healthy controls (HCs), eight BD patients from group I, and seven BD patients from group II. Compared with the HCs, the BD patients exhibited higher serum levels of most cytokines, including significantly higher serum levels of IL-2, IL-6, IL-8, and MCP-1 (Figure 4a). Intriguingly, the serum levels of IL-2 and IL-6 in group I were significantly higher than those in group II (Figure 4b).
Figure 4. a, b.
Using serum samples collected before initiation of IFX treatment, multiple serum cytokine levels were measured using Bio-Plex human cytokine assays in nine HCs, eight BD patients in group I, and seven BD patients in group II. Compared to the HC, the BD patients with uveitis exhibited significantly increased serum IL-2, IL-6, IL-8, and MCP-1 levels (a); Serum IL-2 and IL-6 levels were significantly higher in group I than in group II (b)
Discussion
In the present study, we demonstrated long-term efficacy of IFX therapy for BD-related uveitis up to 5 years and found complete-type BD as a refractory factor for IFX treatment. Moreover, cytokine analyses revealed that serum levels of IL-2, IL-6, IL-8, and MCP-1 in patients with BD uveitis were significant higher than those in healthy controls, of which the patients with high serum levels of IL-2 and IL-6 were more responsive to IFX therapy. To the best of our knowledge, this was the first study to investigate the predictors of IFX treatment responsiveness in patients with BD-related uveitis using analyses of pretreatment serum cytokine profiles.
Consistent with the previous reports, our study demonstrated that IFX treatment significantly reduced the frequency of ocular attacks and improved VA compared with baseline (4–9). Moreover, the frequency of ocular attacks was strongly associated with VA outcomes, that is, improved VA was seen only in the patients with one attack or less per 6 months. This information is clinically significant with respect to BD-related uveitis management.
In this study, approximately half of the patients received intensified treatments, in which the intervals between IFX infusions were shortened. This finding may be attributed to secondary IFX treatment failure due to the production of anti-drug antibodies, i.e., antibodies to IFX (ATI). The incidence of treatment failure due to ATI production appears to vary among different chronic inflammatory diseases, and patient genetics, drug doses, routes of administration, treatment schedules, and concomitant use of immunosuppressant use may also play a role in its occurrence (15, 16). However, the incidence of secondary failure due to ATI production in BD remains unknown. Moreover, there are no randomized studies comparing combined therapy with IFX and immunosuppressive agents, such as methotrexate (MTX), with anti-TNF-a monotherapy in patients with BD-related uveitis, although concomitant therapy may achieve better disease control and/or reductions in anti-TNF-a agent immunogenicity (7, 17). In this study, loss of IFX efficacy may not have been caused by a lack or shortage of concomitant medications because the group that underwent therapy intensification (group II) actually received a higher dose of corticosteroids and was also more likely to use additional medications, such as colchicine and CsA (Table 2). Because the efficacy of concurrent use of MTX or other immunosuppressants with IFX in BD patients has not been established, it may be important to determine whether combined therapy is more effective at treating BD in the future.
Regarding the predictors of IFX treatment responsiveness, patients who underwent IFX treatment intensification (group II) were younger and more likely to have complete BD than patients who received standard IFX treatment (group I). Moreover, acute ocular attacks occurred more frequently in patients with complete BD than in patients with incomplete BD between 12 and 24 months after IFX initiation, indicating that BD uveitis associated with complete BD may be more likely to be refractory to IFX treatment.
Among the various cytokines analyzed, the pretreatment serum levels of IL-2, IL-6, IL-8, and MCP-1 were significantly higher in the patients with BD uveitis than in the healthy controls. Previous studies have also noted increased expression of these cytokines in the peripheral blood of BD patients (18–20), and our results are consistent with these findings. Notably, IL-8, also known as neutrophil chemotactic factor, has been repeatedly implicated as a serological marker of disease activity in patients with BD (18, 19, 21–23). As the presence of activated neutrophils with high levels of chemotactic and phagocytic activity is a hallmark of BD, IL-8 is likely to play an important role in the pathogenesis of BD. Intraocular injections of IL-8 can induce neutrophil-mediated inflammatory reactions, and anti-IL-8 antibodies have been shown to partially block endotoxin-induced uveitis (EIU) in animal models (24). Several studies have reported higher concentrations of MCP-1, a potent monocyte chemotactic factor, in the sera and whole blood of BD patients than in normal controls (19, 25). Previous data indicate that MCP-1-deficient mice were resistant to EIU, whereas co-administration of recombinant MCP-1 induced EIU in these mice (26), suggesting that MCP-1 plays a pathologic role in inflammatory uveitis.
Moreover, increased levels of type 1 T helper (Th1)-related cytokines, as well as IL-2 and IL-6, have been reported in BD patients. For example, intracellular immunofluorescence staining analysis demonstrated increased percentages of CD3+/IL-2+ cells in patients with active BD compared with healthy subjects (27). In addition to the above Th1 polarization, recent data indicate that Th17-mediated responses and IL-23/IL-17 pathway upregulation may be associated with enhanced neutrophil recruitment and function in BD patients with active uveitis (28). IL-6 may play a role in BD pathogenesis by mediating Th17 differentiation and expansion along with transforming growth factor (TGF)-b and IL-23 upregulation, although IL-17 levels in the sera of the BD patients were not elevated and were similar to those of subjects in the control group in the present study.
Comparisons of cytokine levels between group I and group II indicated that BD patients with especially high serum IL-2 and IL-6 levels were more responsive to IFX therapy and had good clinical courses. Serum TNF-a levels were also higher in good responders (group I) than in poor responders (group II) prior to IFX therapy, a difference with borderline statistical significance (Figure 4b). Consistent with these results, previous studies have shown that high levels of circulating bioactive TNF-a were associated with a good response to IFX in RA patients (29, 30), suggesting that high systemic levels of pro-inflammatory cytokines may be associated with good clinical responses to TNF-a blockers, such as IFX, in BD uveitis. In such cases, induction of Foxp3+ regulatory T cells by IFX may play a role in suppressing refractory uveitis (31). Our results indicated for the first time that serum IL-2 and IL-6 levels may be useful as surrogate markers of responsiveness to IFX treatment in patients with BD uveitis.
The 5-year continuation rate of IFX treatment for BD patients was 87.9%, indicating that IFX therapy is well-tolerated in BD with refractory uveitis. Regarding adverse events, two patients with genital ulcers and entero-Behçet’s disease developed PID and bacterial enteritis, respectively, within 1 year of initiating therapy. Therefore, due to the possibility of microbe entry, it is important to observe patients closely for signs of infection after initiating IFX therapy. Two patients developed malignancies, namely, malignant lymphoma and thoracic carcinoma, 4 years after initiating IFX therapy. Given the advanced ages of these patients, the association between IFX treatment and malignancy is not clear. However, we cannot exclude the possibility that long-term administration of a TNF-a blocker, such as IFX, increases the risk of malignancy.
In summary, we confirmed the long-term efficacy and tolerability of IFX in patients with BD-related uveitis. Our findings indicate that complete BD may be more refractory to IFX than incomplete BD and that pretreatment serum IL-2 and IL-6 levels may be useful biomarkers for predicting long-term responsiveness to IFX therapy.
Acknowledgements
We are grateful to the patients and volunteers for their participation in this study.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Kyushu University Hospital.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.U., M. Akakoshi, A.T., Y.I., H.T., K.A.; Design - S.U., M. Akakoshi, A.T., Y.I., H.N., K.A.; Supervision - M. Akakoshi, H.T., T.H., T.I., K.S., K.A.; Resources - H.T., T.I., K.S., K.A.; Materials - A.O., A.T., S.H., T.F., T.I., K.S.; Data Collection and/or Processing - S.U., A.O., A.T., S.H., T.F., T.I., K.S.; Analysis and/or Interpretation - S.U., M. Akakoshi, A.T., M. Ayano, Y.K., H.M., Y.A., H.N., H.T., S.H., T.F.; Literature Search - M. Akakoshi, Y.I., M. Ayano, Y.K., H.M., Y.A., T.H.; Writing Manuscript - S.U., M. Akakoshi, H.T.; Critical Review - A.O., M. Ayano, Y.K., H.M., Y.A., H.N, H.T., T.H., K.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: This work was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology in Japan (Grants-in-Aid for Scientific Research 15K09527).
References
- 1.Sakane T, Takeno M, Suzuki N, Inaba G. Behçet’s disease. N Engl J Med. 1999;341:1284–91. doi: 10.1056/NEJM199910213411707. [DOI] [PubMed] [Google Scholar]
- 2.Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M. Uveitis in Behçet disease: an analysis of 880 patients. Am J Ophthalmol. 2004;138:373–80. doi: 10.1016/j.ajo.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Kitaichi N, Miyazaki A, Iwata D, Ohno S, Stanford MR, Chams H. Ocular features of Behçet’s disease: an international collaborative study. Br J Ophthalmol. 2007;91:1579–82. doi: 10.1136/bjo.2007.123554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tugal-Tutkun I, Mudun A, Urgancioglu M, Kamali S, Kasapoglu E, Inanc M, et al. Efficacy of infliximab in the treatment of uveitis that is resistant to treatment with the combination of azathioprine, cyclosporine, and corticosteroids in Behçet’s disease: an open-label trial. Arthritis Rheum. 2005;52:2478–84. doi: 10.1002/art.21231. [DOI] [PubMed] [Google Scholar]
- 5.Okada AA, Goto H, Ohno S, Mochizuki M. Multicenter study of infliximab for refractory uveoretinitis in Behçet disease. Arch Ophthalmol. 2012;130:592–8. doi: 10.1001/archophthalmol.2011.2698. [DOI] [PubMed] [Google Scholar]
- 6.Al Rashidi S, Al Fawaz A, Kangave D, Abu El-Asrar AM. Long-term clinical outcomes in patients with refractory uveitis associated with Behçet disease treated with infliximab. Ocul Immunol Inflamm. 2013;21:468–74. doi: 10.3109/09273948.2013.779727. [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi M, Kezuka T, Sugita S, Keino H, Namba K, Kaburaki T, et al. Evaluation of the long-term efficacy and safety of infliximab treatment for uveitis in Behçet’s disease: a multicenter study. Ophthalmology. 2014;121:1877–84. doi: 10.1016/j.ophtha.2014.04.042. [DOI] [PubMed] [Google Scholar]
- 8.Calvo-Rio V, Blanco R, Beltran E, Sanchez-Burson J, Mesquida M, Adan A, et al. Anti-TNF-a therapy in patients with refractory uveitis due to Behçet’s disease: a 1-year follow-up study of 124 patients. Rheumatology (Oxford) 2014;53:2223–31. doi: 10.1093/rheumatology/keu266. [DOI] [PubMed] [Google Scholar]
- 9.Cordero-Coma M, Sobrin L. Anti-tumor necrosis factor-a therapy in uveitis. Surv Ophthalmol. 2015;60:575–89. doi: 10.1016/j.survophthal.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Hyrich KL, Lunt M, Watson KD, Symmons DP, Silman AJ. Outcomes after switching from one anti-tumor necrosis factor a agent to a second anti-tumor necrosis factor a agent in patients with rheumatoid arthritis: results from a large UK national cohort study. Arthritis Rheum. 2007;56:13–20. doi: 10.1002/art.22331. [DOI] [PubMed] [Google Scholar]
- 11.Hetland ML, Christensen IJ, Tarp U, Dreyer L, Hansen A, Hansen IT, et al. Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum. 2010;62:22–32. doi: 10.1002/art.27227. [DOI] [PubMed] [Google Scholar]
- 12.Suzuki Kurokawa M, Suzuki N. Behçet’s disease. Clinical and experimental medicine. 2004;4:10–20. doi: 10.1007/s10238-004-0033-4. [DOI] [PubMed] [Google Scholar]
- 13.Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takeuchi M, Hokama H, Tsukahara R, Kezuka T, Goto H, Sakai J, et al. Risk and prognostic factors of poor visual outcome in Behçet’s disease with ocular involvement. Graefes Arch Clin Exp Ophthalmol. 2005;243:1147–52. doi: 10.1007/s00417-005-0005-8. [DOI] [PubMed] [Google Scholar]
- 15.van Schouwenburg PA, Rispens T, Wolbink GJ. Immunogenicity of anti-TNF biologic therapies for rheumatoid arthritis. Nat Rev Rheumatol. 2013;9:164–72. doi: 10.1038/nrrheum.2013.4. [DOI] [PubMed] [Google Scholar]
- 16.Felis-Giemza A, Moots RJ. Measurement of anti-drug antibodies to biologic drugs. Rheumatology (Oxford) 2015;54:1941–3. doi: 10.1093/rheumatology/kev279. [DOI] [PubMed] [Google Scholar]
- 17.Ito T, Sonoda KH, Hijioka K, Fujimoto T, Ishibashi T. Acquired resistance to infliximab against uveitis due to Behçet’s disease after one year of administration. Jpn J Ophthalmol. 2010;54:502–4. doi: 10.1007/s10384-010-0859-0. [DOI] [PubMed] [Google Scholar]
- 18.Evereklioglu C, Er H, Turkoz Y, Cekmen M. Serum levels of TNF-a, sIL-2R, IL-6, and IL-8 are increased and associated with elevated lipid peroxidation in patients with Behçet’s disease. Mediators Inflamm. 2002;11:87–93. doi: 10.1080/09629350220131935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaburaki T, Fujino Y, Kawashima H, Merino G, Numaga J, Chen J, et al. Plasma and whole-blood chemokine levels in patients with Behçet’s disease. Graefes Arch Clin Exp Ophthalmol. 2003;241:353–8. doi: 10.1007/s00417-003-0668-y. [DOI] [PubMed] [Google Scholar]
- 20.Akdeniz N, Esrefoglu M, Keles MS, Karakuzu A, Atasoy M. Serum interleukin-2, interleukin-6, tumour necrosis factor-a and nitric oxide levels in patients with Behçet’s disease. Ann Acad Med Singapore. 2004;33:596–9. [PubMed] [Google Scholar]
- 21.Itoh R, Takenaka T, Okitsu-Negishi S, Matsushima K, Mizoguchi M. Interleukin 8 in Behçet’s disease. J Dermatol. 1994;21:397–404. doi: 10.1111/j.1346-8138.1994.tb01762.x. [DOI] [PubMed] [Google Scholar]
- 22.Ozoran K, Aydintug O, Tokgoz G, Duzgun N, Tutkak H, Gurler A. Serum levels of interleukin-8 in patients with Behçet’s disease. Ann Rheum Dis. 1995;54:610. doi: 10.1136/ard.54.7.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gur-Toy G, Lenk N, Yalcin B, Aksaray S, Alli N. Serum interleukin-8 as a serologic marker of activity in Behçet’s disease. Int J Dermatol. 2005;44:657–60. doi: 10.1111/j.1365-4632.2004.02184.x. [DOI] [PubMed] [Google Scholar]
- 24.Verma MJ, Mukaida N, Vollmer-Conna U, Matsushima K, Lloyd A, Wakefield D. Endotoxin-induced uveitis is partially inhibited by anti-IL-8 antibody treatment. Invest Ophthalmol Vis Sci. 1999;40:2465–70. [PubMed] [Google Scholar]
- 25.Cho ML, Kim JY, Ko HJ, Kim YH, Kim WU, Cho CS, et al. The MCP-1 promoter -2518 polymorphism in Behçet’s disease: correlation between allele types, MCP-1 production and clinical symptoms among Korean patients. Autoimmunity. 2004;37:77–80. doi: 10.1080/08916930310001609446. [DOI] [PubMed] [Google Scholar]
- 26.Tuaillon N, Shen DF, Berger RB, Lu B, Rollins BJ, Chan CC. MCP-1 expression in endotoxin-induced uveitis. Invest Ophthalmol Vis Sci. 2002;43:1493–8. [PubMed] [Google Scholar]
- 27.Frassanito MA, Dammacco R, Cafforio P, Dammacco F. Th1 polarization of the immune response in Behçet’s disease: a putative pathogenetic role of interleukin-12. Arthritis Rheum. 1999;42:1967–74. doi: 10.1002/1529-0131(199909)42:9<1967::AID-ANR24>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 28.Chi W, Zhu X, Yang P, Liu X, Lin X, Zhou H, et al. Upregulated IL-23 and IL-17 in Behçet patients with active uveitis. Invest Ophthalmol Vis Sci. 2008;49:3058–64. doi: 10.1167/iovs.07-1390. [DOI] [PubMed] [Google Scholar]
- 29.Marotte H, Maslinski W, Miossec P. Circulating tumour necrosis factor-a bioactivity in rheumatoid arthritis patients treated with infliximab: link to clinical response. Arthritis Res Ther. 2005;7:R149–55. doi: 10.1186/ar1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marotte H, Arnaud B, Diasparra J, Zrioual S, Miossec P. Association between the level of circulating bioactive tumor necrosis factor a and the tumor necrosis factor a gene polymorphism at -308 in patients with rheumatoid arthritis treated with a tumor necrosis factor a inhibitor. Arthritis Rheum. 2008;58:1258–63. doi: 10.1002/art.23430. [DOI] [PubMed] [Google Scholar]
- 31.Sugita S, Yamada Y, Kaneko S, Horie S, Mochizuki M. Induction of regulatory T cells by infliximab in Behçet’s disease. Invest Ophthalmol Vis Sci. 2011;52:476–84. doi: 10.1167/iovs.10-5916. [DOI] [PubMed] [Google Scholar]