Abstract
Resolution of inflammation is a critical process that is facilitated by specialized proresolving mediators (SPMs). In this issue, Bang et al. show that the G protein–coupled receptor GPR37 is a receptor for one such SPM, neuroprotectin D1. They also show that GPR37 activation in macrophages enhances phagocytosis, shifts cytokine release toward an antiinflammatory profile, and thereby helps to reverse inflammatory pain.
Specialized proresolving mediators as active participants in resolution of inflammation
The earliest events following tissue infection or injury typically involve the sequential recruitment of neutrophils and macrophages, together with cardinal features of inflammation: tumor (edema), calor (warmth), dolor (pain), rubor (redness), and functio laesa (loss of function). Over time, however, antiinflammatory processes reduce immune cell infiltration by reciprocally suppressing the release of proinflammatory cytokines while enhancing the release of antiinflammatory cytokines. Meanwhile, proresolution processes limit further damage and enhance restoration of tissue homeostasis by promoting neutrophil apoptosis and the phagocytic removal of apoptotic neutrophils, cell debris, and residual pathogens by phagocytic macrophages (1). These events coincide with reversal of inflammation and pain. Yet, while mechanisms whereby proinflammatory mediators drive inflammatory pain have been well-studied, relatively less is known at the molecular level about how inflammatory pain is resolved.
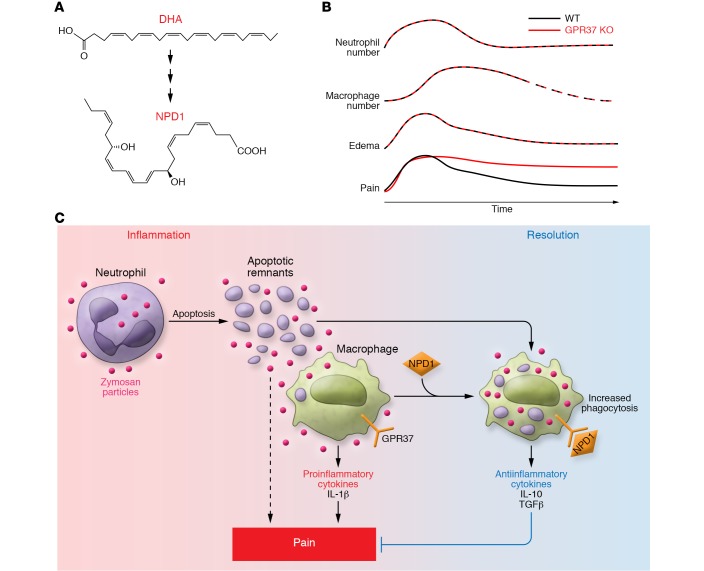
An array of specialized proresolving mediators (SPMs) (2, 3) generated endogenously during inflammation promotes the resolution of inflammation. Most SPMs are lipids derived enzymatically from essential fatty acids such as arachidonic acid (AA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) (4). Lipoxins (LXA4 and LXB4) are SPMs derived from AA (1, 5). Additional SPM families, including resolvins, protectins, and maresins, were first identified by Serhan (2). E-series resolvins (RvE1 and RvE2) are derived from EPA whereas D-series resolvins (RvD1-6), neuroprotectins/protectins (NPD1/PD1), and maresins are derived from DHA (refs. 6–8 and Figure 1A). As a class, SPMs share similar biological functions, including limiting neutrophil infiltration, shifting cytokine profiles from pro- to antiinflammatory, and promoting macrophage phagocytosis. However, SPMs display cell-type–specific actions owing to differential expression of their receptors. SPMs exert most of their effects via GPCRs such as those that bind LXA4 (ALXR/FPR2) (9), RvE1 (chemokine-like receptor 1/CHEMR23) (10), RvD1 (GPR32) (11), and RvD2 (GPR18) (12). Until now, however, the receptor that mediates the proresolving actions of NPD1 has remained undefined. In this issue, Bang et al. identify GPR37 (parkin-associated endothelin-like receptor/Pael-R) as a receptor for NPD1 and provide evidence implicating GPR37 as a new molecular participant in macrophage phagocytosis and the resolution of inflammatory pain (13).
Figure 1. NPD1-GPR37 signaling promotes resolution of inflammatory pain.
(A) Biosynthesis of neuroprotectin D1 (NPD1) from dietary docosahexaenoic acid (DHA). (B) Genetic knockout of the NPD1 receptor GPR37 prolongs pain evoked by zymosan injection without altering kinetics of immune cell trafficking or resolution of edema. (C) NPD1 and GPR37 signaling likely promotes resolution of inflammatory pain by both enhancing macrophage phagocytosis and shifting cytokine release toward an antiinflammatory profile. Onset of inflammation is at left; resolution phase is at right.
NPD1, GPR37, and the resolution of inflammatory pain
GPR37 is a GPCR most extensively studied in the brain that has been associated with Parkinson’s disease and autism spectrum disorder (14–16). Two known GPR37 ligands, prosaposin and prosaposin-derived 14-mer peptide (TX14), have been shown to exert neuroprotective and glioprotective effects via this receptor (17). Prosaposin and TX14 have also been shown to alleviate tactile allodynia in several models of neuropathic- and formalin-induced pain (17), although the relevant receptor for those actions was not identified. Moreover, the expression and function of GPR37 in immune cells has not been previously addressed. To explore potential roles for GPR37 in inflammatory pain, Bang et al. characterized the cellular distribution of GPR37 in mouse hind paw skin, dorsal root ganglia (DRG, which house sensory neuron cell bodies), the spinal cord, and the brain (13). They detected GPR37 expression in a subset of macrophages in skin, peritoneal fluid, and DRG. Interestingly, however, they observed no GPR37 in spinal or brain microglia, which share many features with macrophages, or in peripheral sensory neurons.
Bang et al. also provide several lines of evidence suggesting that GPR37 is a receptor for NPD1 (13). First, NPD1, like prosaposin and TX14, evoked Ca2+ responses in HEK293 cells transfected with GPR37 but not in those transfected with other SPM receptors. Second, among multiple SPMs screened, only NPD1 could activate Ca2+ responses in GPR37-transfected cells. Third, genetic knockout of GPR37 abolished NPD1-evoked Ca2+ responses in cultured primary peritoneal macrophages. And fourth, dot-blot assays supported the ability of NPD1 to bind GPR37.
Another important finding of Bang et al. was that NPD1 could enhance macrophage phagocytosis of yeast-derived zymosan particles, an effect that was absent in peritoneal macrophages isolated from GPR37-KO mice (13). Using pharmacological inhibitors, they further determined that the potentiation of macrophage phagocytosis by NPD1 and GPR37 depends on signaling through G protein subunit Gi/o, ERK, and PI3K/AKT. This differs from RvD2/DRV2 signaling, which has been shown to promote resolution via a pathway involving cAMP, pCREB, STAT3, and ERK (18).
Upon injection into rodent skin, zymosan particles evoke inflammation and associated mechanical and thermal hypersensitivity that peak within approximately 4 hours but then revert back to baseline within about one week. Bang and colleagues employed this model to determine the contributions of GPR37 and macrophages to the resolution of inflammatory pain (ref. 13 and Figure 1B). They observed that GPR37-KO impaired in vivo macrophage phagocytosis of zymosan and apoptotic neutrophils but had no effect on neutrophil recruitment or on the reduction in neutrophil numbers at later time points (presumably a consequence of neutrophil apoptosis). In addition, GPR37 deficiency augmented the expression of proinflammatory cytokines (e.g., IL-1β) and reciprocally suppressed the expression of antiinflammatory cytokines (e.g., IL-10 and TGF-β) in macrophages, suggesting that GPR37 activation favors an M2-like over an M1-like macrophage phenotype. In behavioral assays, naive GPR37-KO mice showed normal withdrawal responses to painful mechanical, thermal, and chemical stimuli. The onset and peak severity of mechanical and thermal hyperalgesia evoked by injection with zymosan were also normal in GPR37-KO mice. However, despite a normal resolution of edema, the resolution of inflammatory pain was much slower in mice lacking GPR37 compared with WT controls, with substantial residual hyperalgesia at 4 weeks. A similar pattern of normal onset of hyperalgesia but delayed resolution was observed in GPR37-KO mice injected with IL-1β. Thus, it appears that GPR37 plays a selective role in the resolution phase of inflammatory pain, potentially by facilitating macrophage participation in proresolution events (summarized in Figure 1C).
Bang et al. employed both gain- and loss-of-function approaches to further test this possibility (13). First, depletion of macrophages from WT mice using the chemical toxin clodronate phenocopied the prolonged zymosan-induced pain phenotype seen in GPR37-KO mice. Second, and even more strikingly, adoptive transfer of WT but not GPR37-deficient macrophages into GPR37-KO mice reversed their prolonged hyperalgesia phenotype. Moreover, the proresolving effect of adoptively transferred WT macrophages was attenuated by neutralizing antibodies against IL-10. Taken together, these findings suggest that GPR37 in macrophages promotes the resolution of inflammatory pain, at least in part by promoting the release of IL-10.
Implications and future directions
The findings of Bang et al. identify roles for a previously unappreciated ligand-receptor pair in the resolution of inflammatory pain. They also raise a number of important questions. First, what endogenous ligand(s) drive GPR37-mediated proresolution effects in the setting of zymosan-induced pain? Are these events mediated by NPD1, prosaposin, TX14, or other, unidentified GPR37 ligands? Time-resolved biochemical assays for SPMs during zymosan inflammation, coupled with selective blockade of their synthesis, could help to address this issue.
Second, what might be the utility of different SPMs engaging different signaling pathways (Gi/o/Ca2+/PI3K/ERK vs. cAMP/pCREB/STAT3/ERK) to promote phagocytosis by innate immune cells? Do these pathways act additively or synergistically, or function complementarily to target different cellular populations or preferentially enhance the phagocytosis of distinct substrates? Furthermore, do these events occur in parallel with the reported direct analgesic effects of SPMs on sensory neurons (19)?
Third, what is the relative importance of GPR37-augmented phagocytosis vs. cytokine profile shift to the resolution of inflammatory pain? A major role for GPR37-stimulated macrophage IL-10 secretion in pain resolution is well-supported by the study of Bang et al. (13). However, any benefits of this receptor’s prophagocytic effects, while conceptually reasonable, remain speculative. Although Bang et al. show that the proportion of macrophage-engulfed neutrophils during the resolution phase of zymosan inflammation is dependent on the presence of GPR37, knockout of this receptor apparently does not alter either the recruitment of neutrophils to zymosan-treated skin or the degree of neutrophil elimination by day 5. While the latter might be attributable, in part, to normal neutrophil apoptosis in the absence of GPR37, the specific respective contributions of neutrophil apoptosis and macrophage-mediated phagocytosis to pain resolution remain to be clarified. The precise interplay between phagocytosis, inflammation, nociceptive neurons, and pain is likely to be especially relevant in the setting of infection with living microorganisms. Recent studies have shown that certain pathological bacteria directly activate nociceptive neurons through the production of toxins such as Streptolysin S, and that the consequent release of neuropeptides from the nociceptive neurons suppresses recruitment of innate immune cells that would normally phagocytose the bacteria to clear or limit the infection (20). Presumably, mechanisms that augment phagocytosis, per se, would reduce bacterial growth and consequently pain in this setting. However, this idea remains to be directly tested.
Fourth, in the setting of peripheral nerve injury, do GPR37 or other SPMs facilitate macrophage phagocytosis of axonal and myelin debris and is this effect a contributing factor to effective nerve regeneration and subsequent reversal of neuropathic pain?
Collectively, the findings of Bang et al. (13) identify new molecular participants (and attractive candidate therapeutic targets) in the resolution of inflammatory pain, highlight the utility of the zymosan system for the analysis of “active” resolution of pain, and bring into focus new questions about the details of this multifaceted process.
Acknowledgments
Supported by the Neurosurgery Pain Research Institute at Johns Hopkins and by NIH R01AR072230 to LQ.
Version 1. 07/16/2018
Electronic publication
Version 2. 08/01/2018
Print issue publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Reference information: J Clin Invest. 2018;128(8):3246–3249. https://doi.org/10.1172/JCI122203.
See the related article at GPR37 regulates macrophage phagocytosis and resolution of inflammatory pain.
Contributor Information
Lintao Qu, Email: lqu4@jhmi.edu.
Michael J. Caterina, Email: caterina@jhmi.edu.
References
- 1.Serhan CN. Resolution phase of inflammation: novel endogenous anti-inflammatory and proresolving lipid mediators and pathways. Annu Rev Immunol. 2007;25:101–137. doi: 10.1146/annurev.immunol.25.022106.141647. [DOI] [PubMed] [Google Scholar]
- 2.Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014;510(7503):92–101. doi: 10.1038/nature13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serhan CN, Dalli J, Colas RA, Winkler JW, Chiang N. Protectins and maresins: new pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome. Biochim Biophys Acta. 2015;1851(4):397–413. doi: 10.1016/j.bbalip.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basil MC, Levy BD. Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nat Rev Immunol. 2016;16(1):51–67. doi: 10.1038/nri.2015.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petasis NA, et al. Design, synthesis and bioactions of novel stable mimetics of lipoxins and aspirin-triggered lipoxins. Prostaglandins Leukot Essent Fatty Acids. 2005;73(3-4):301–321. doi: 10.1016/j.plefa.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 6.Arita M, et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci U S A. 2005;102(21):7671–7676. doi: 10.1073/pnas.0409271102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serhan CN, et al. Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J Immunol. 2006;176(3):1848–1859. doi: 10.4049/jimmunol.176.3.1848. [DOI] [PubMed] [Google Scholar]
- 8.Sun YP, et al. Resolvin D1 and its aspirin-triggered 17R epimer. Stereochemical assignments, anti-inflammatory properties, and enzymatic inactivation. J Biol Chem. 2007;282(13):9323–9334. doi: 10.1074/jbc.M609212200. [DOI] [PubMed] [Google Scholar]
- 9.Dufton N, Perretti M. Therapeutic anti-inflammatory potential of formyl-peptide receptor agonists. Pharmacol Ther. 2010;127(2):175–188. doi: 10.1016/j.pharmthera.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Arita M, et al. Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J Exp Med. 2005;201(5):713–722. doi: 10.1084/jem.20042031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnamoorthy S, et al. Resolvin D1 binds human phagocytes with evidence for proresolving receptors. Proc Natl Acad Sci U S A. 2010;107(4):1660–1665. doi: 10.1073/pnas.0907342107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiang N, Dalli J, Colas RA, Serhan CN. Identification of resolvin D2 receptor mediating resolution of infections and organ protection. J Exp Med. 2015;212(8):1203–1217. doi: 10.1084/jem.20150225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bang S, Xie YK, Zhang ZJ, Wang Z, Xu ZZ, Ji RR. GPR37 regulates macrophage phagocytosis and resolution of inflammatory pain. J Clin Invest. 2018;128(8):3568–3582. doi: 10.1172/JCI99888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fujita-Jimbo E, et al. Mutation in Parkinson disease-associated, G-protein-coupled receptor 37 (GPR37/PaelR) is related to autism spectrum disorder. PLoS One. 2012;7(12):e51155. doi: 10.1371/journal.pone.0051155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marazziti D, Gallo A, Golini E, Matteoni R, Tocchini-Valentini GP. Molecular cloning and chromosomal localization of the mouse Gpr37 gene encoding an orphan G-protein-coupled peptide receptor expressed in brain and testis. Genomics. 1998;53(3):315–324. doi: 10.1006/geno.1998.5433. [DOI] [PubMed] [Google Scholar]
- 16.Murakami T, et al. Pael-R is accumulated in Lewy bodies of Parkinson’s disease. Ann Neurol. 2004;55(3):439–442. doi: 10.1002/ana.20064. [DOI] [PubMed] [Google Scholar]
- 17.Jolivalt CG, Ramos KM, Herbetsson K, Esch FS, Calcutt NA. Therapeutic efficacy of prosaposin-derived peptide on different models of allodynia. Pain. 2006;121(1–2):14–21. doi: 10.1016/j.pain.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Chiang N, de la Rosa X, Libreros S, Serhan CN. Novel resolvin D2 receptor axis in infectious inflammation. J Immunol. 2017;198(2):842–851. doi: 10.4049/jimmunol.1601650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park CK, Xu ZZ, Liu T, Lü N, Serhan CN, Ji RR. Resolvin D2 is a potent endogenous inhibitor for transient receptor potential subtype V1/A1, inflammatory pain, and spinal cord synaptic plasticity in mice: distinct roles of resolvin D1, D2, and E1. J Neurosci. 2011;31(50):18433–18438. doi: 10.1523/JNEUROSCI.4192-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinho-Ribeiro FA, et al. Blocking neuronal signaling to immune cells treats streptococcal invasive infection. Cell. 2018;173(5):1083–1097.e22. doi: 10.1016/j.cell.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]