Abstract
Urgent visits to the clinic and emergency department for acute severe asthma exacerbations are all too frequent. Existing national guidelines do not present consistent or specific recommendations for the evaluation and treatment of individual asthma patients in respiratory distress. In this vein, we propose the term “critical asthma syndrome” (CAS) to describe any child or adult who is at high risk for fatal asthma. Acute severe asthma, refractory asthma, status asthmaticus, and near-fatal asthma all describe CAS where physical exhaustion from the overwhelming work of breathing leads to respiratory arrest and death from hypoxia or related complications. The authors of this supplement seek to emphasize the importance of early recognition, prompt and coordinated evaluation, and treatment of CAS in the emergency department, hospital, and intensive care units by experienced healthcare provider teams. CAS is not severe persistent asthma where control of symptoms and prevention of exacerbations are targets of chronic disease management in the outpatient setting. The authors address the distinctions between the two entities throughout the supplement, and elaborate on the considerations important in the care of a critically ill patient, including the common errors to avoid. In addition, gaps in knowledge and clinical experience in regards to critical asthma are highlighted. Knowledge gaps include a lack of understanding of how to recognize CAS, how to coordinate and integrate hospital and outpatient resources, when to further phenotype patients with critical asthma in order to facilitate effective treatment, and how to prevent future acute exacerbations. Lastly, CAS is complicated by the fact that asthma care in diverse healthcare settings is haphazard. We recommend that primary care physicians refer patients promptly to an asthma specialist for consultation to reduce the frequency of acute exacerbations and prevent the development of CAS.
Keywords: Critical asthma, Fatal asthma, Near fatal asthma, Status asthmaticus, Severe persistent asthma
Introduction
Consider the patient with acute worsening asthma from the perspective of the physician. Her past medical history is punctuated by several emergency department (ED) admissions in the past year and a remote episode of near-fatal asthma requiring prolonged intubation and mechanical ventilation. She presents now with a 2-week history of progressive dyspnea, nocturnal awakenings, and rescue drug use every 3 h after an apparent upper respiratory tract infection. The physician or healthcare provider may be a hospital-based pulmonary and critical care specialist or an emergency room doctor, but just as likely may be a primary care physician or allergist in the clinic setting. Other key personnel must be involved —for example, a registered respiratory therapist and/or registered nurse. All recognize that the patient has a worrisome virus-associated asthma exacerbation with a deteriorating clinical course, but the next course of action is not always clear and difficult decisions must be made quickly to protect the patient (e.g., oxygen, pharmacotherapy, endotracheal intubation, mechanical ventilation).
Published guidelines including the National Asthma Education and Prevention Program (NAEPP) Expert Panel Report-3 (EPR-3) [1] and the World Health Organization (WHO) Global Initiative for Asthma (GINA) [2] present stepwise evaluation and treatment recommendations for chronic persistent asthma management, but do not emphasize as well a coherent plan for this urgent if not critical setting. While management strategies for asthma in the ED and intensive care unit (ICU) setting have been proposed, these statements lack the rigor of the NAEPP guidelines and fail to define the role of other providers caring for the patient in question.
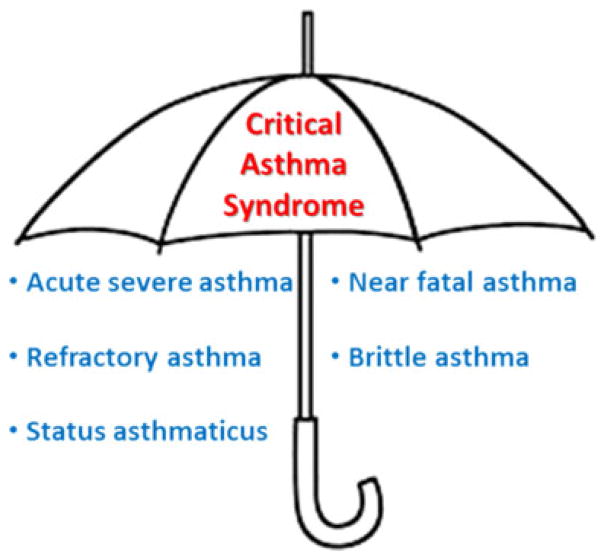
In this vein, we propose the umbrella term “critical asthma syndrome” (CAS) to define a severe and sudden respiratory condition that, although needing aggressive and urgent treatment, has not progressed to irreversible hypoxia and cardio-pulmonary arrest (Fig. 1). CAS includes all sub-acutely to acutely decompensating asthmatics where common but non-specific signs and symptoms predominate, primarily shortness of breath, progressive respiratory fatigue (paradoxical breathing), and lightheadedness. These CAS patients are very unstable and require close monitoring of vital signs and their response or lack thereof to treatments. In every case, CAS begins with what appears to be an ordinary asthma exacerbation. In this and succeeding manuscripts, the authors address many aspects of critical asthma situations, including the immediate treatment of CAS, and pitfalls in hospital management that must be avoided or acted upon quickly, and secondary prevention of future CAS.
Fig. 1.
Critical asthma syndrome (CAS) is an umbrella term that represents many other terms historically and currently used to describe acute and severe life-threatening exacerbations
The Impact of the Critical Asthma Syndrome
Asthma itself is a very common complex syndrome, rather than a single disease. Approximately 26 million people in the United States and a significant percentage are at risk for critical events, particularly those with poor access to care, poor self-management skills, and a personal history of past critical asthma episodes.
Approximately 2 million ED visits are attributed to acute asthma exacerbations annually in the United States. It is projected that 500,000 will be hospitalized (25 % of visits), 25,000 will be intubated (5 % of hospitalizations), and between 10 % and 25 % of patients will die primarily from consequences of anoxia and cardiopulmonary arrest [3]. Approximately 3,000 deaths occur annually, but the majority of these deaths occur outside the hospital. A recent study of the effect of age on asthma mortality showed that age >55 years conferred a 5-fold increased risk of death from asthma compared to younger adults and children [4]. Overall the risk of death from asthma in the ED or hospital in this large inpatient database study was 0.06 %.
Asthmatic patients gain a modicum of understanding of their disease from their doctors, but also from their family and friends, the Internet, and the lay press. Much of the information that patients procure informs them that asthma is a disease that requires regular attention and treatment, but also that it is intermittent and inherently controllable. Instead, we believe it is important to emphasize to patients, physicians, caregivers, and all healthcare providers that not all asthma is equal and that perception of acute dyspnea is highly variable among patients. Besides age, the highest rates of asthma death are in African Americans, Puerto Rican Americans, Cuban Americans and women over age 55 years. Approximately 1 % to 7 % of people with severe asthma will die of their disease each year, and perhaps 17 % of those who survive near-fatal attacks will eventually succumb to asthma [5]. Asthma deaths are very uncommon (approximately nine deaths occur daily in the United States), especially among children and young adults, but they remain a target of costly education and preventive efforts to avoid asthma-related deaths [6]. Early treatment of exacerbations, better control of asthma symptoms, and special attention to patients who are at high risk of asthma-related death are key clinical activities. Predictors of fatal asthma include three or more ED visits for asthma in the past year, an asthma hospitalization or ED visit in the past month, overuse of short-acting beta 2 agonist, a history of intubation or ICU stay for asthma, difficulty perceiving asthma symptoms, lack of a written asthma action plan, certain patient characteristics (e.g., low socioeconomic status, female, nonwhite, current smoker, or major psychosocial problems), and the presence of other medical conditions such as heart disease. Death from asthma or CAS continues to decline and is down between 25 % and 30 % since 1996. A total of 4,269 deaths from asthma were reported in 2001, whereas 3,388 deaths were recorded in 2009 [7].
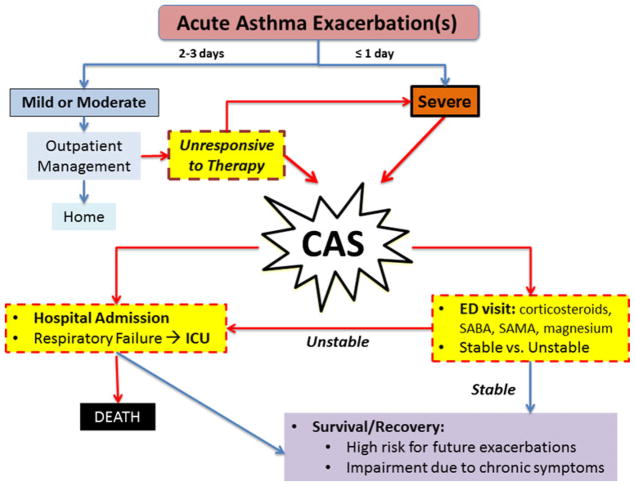
Many CAS cases occur because chronic asthma is not well controlled, raising the risk and frequency for acute exacerbations (Fig. 2), and there is plenty of evidence to support this. For example, in one study up to 77 % of patients in the United States have moderate to severe persistent disease [8]. The Real-world Evaluation of Asthma Control and Treatment (REACT) study found that 55 % of 1,812 patients assessed using an Internet-based survey had uncontrolled asthma using the Asthma Control Test (ACT)™ to stratify cohorts [9]. Such patients with “continuous asthma exacerbations” are at higher risk for CAS and therefore ED visits and hospitalization. They often have persistent expiratory airflow obstruction (FEV1 <68 % predicted) despite high medication use [10].
Fig. 2.
Progression and timeline of acute exacerbation of asthma to CAS
Severe Asthma and Critical Asthma
Critical asthma is not severe asthma. The former is an acute clinical syndrome conceptually similar to stroke or acute coronary syndrome, whereas the latter describes a specific chronic asthma phenotype notable for poor asthma control, despite the use of multiple controller medications, that is coincidentally at high risk of acute exacerbation. Critical asthma episodes will occur at times to patients who fit the severe asthma framework, but those with mild asthma may suffer such events also. Other historical terms have been used to frame the spectrum of critical asthma, which we will explore and compare, such as status asthmaticus, brittle asthma, refractory asthma, and near-fatal asthma.
The definition of severe asthma is probably most important to discuss as a comparator to our definition of CAS. Our understanding of severe asthma has improved considerably with the advent of consensus definitions from the American Thoracic Society (ATS) [11] and the WHO [12], and further updates on severe asthma management from the ATS/ European Respiratory Society (ERS) are expected in the next 1–2 years.
Severe asthma includes any or all of the following asthma characteristics: the failure to achieve asthma control despite confirmed adherence to treatment with inhaled corticosteroids (ICS), the repeated need for emergency health-care services for asthma exacerbations, the need for chronic daily oral corticosteroid therapy, and reduced lung function. The most commonly applied definition of severe asthma was developed as part of an ATS workshop and has been adopted by the 10-year-old Severe Asthma Research Program (SARP) [11] funded by the National Institutes of Health (NIH) [13]. Severe asthma is defined by at least one major criterion and two minor criteria. The major criteria are as follows: (1) requirement for treatment with high-dose ICS (>800 μg/d fluticasone or equivalent); and (2) treatment with oral corticosteroids for >50 % of the year. Minor criteria are as follows: (a) requirement for additional daily preferred controller treatments (long-acting beta 2 agonists [LABA], theophylline, omalizumab, leukotriene receptor antagonists [LTRA]); and (b) asthma symptoms requiring albuterol on a daily basis; (c) persistent airway obstruction (FEV1 <80 %, peak expiratory flow rate [PEFR] >20 %); (d) one or more urgent care visits per year; (e) three or more oral corticosteroid bursts per year; and (f) near-fatal asthma event in the past [11].
The NIH-funded SARP consortium investigators have invested heavily in phenotyping research with the hope of ultimately targeting potential treatments to certain subgroups of patients. An important study by Wenzel and colleagues [14] defined two populations of severe asthma based on the pattern of inflammatory cells found in endobronchial biopsy samples. Patients referred to the investigators’ clinic who required ≥ 10 mg of prednisone during >75 % of the year underwent evaluation with bronchoscopy. In 14 patients with severe asthma, biopsy samples yielded solely neutrophils, while 20 patients had both eosinophils and neutrophils. Members of the latter group had significantly more episodes of respiratory failure requiring intubation and ventilatory support and a lower ratio of FVC to slow vital capacity. More recently, Woodruff and colleagues outlined “Th2-high” and “Th2-low” groups. The T helper type 2 (Th2) lymphocytes are defined by the cytokines, namely IL-4, IL-5, and IL-13, all of which are important in the development and persistence of eosinophilic airway inflammation [15]. In this 8-week study in subjects with mild to moderate asthma, Th2-high subjects had an average increase of 300 ml in FEV1 with ICS treatment and this was significantly greater than the increase in either the Th2-low or the placebo-control group. This study was one of the first to show clear responses to therapy tailored to the specific molecular phenotype of asthma. Many more research studies outside of the US have promoted phenotyping efforts and directions, mostly in more symptomatic adult asthmatics [16, 17] with the eventual hope of developing a personalized-medicine treatment approach.
More broadly, the SARP investigators have proposed a “clustering” paradigm for severe asthma patients based on baseline FEV1, max FEV1 (the maximum FEV1 effort after serial albuterol doses of up to eight puffs), and age of onset of asthma. Patients in severe asthma clusters 4 and 5 who had a baseline FEV1 <68 % of predicted, with or without a max FEV1 >65 % of predicted, had a high rate of hospitalization per year (23 % and 28 %, respectively) and required oral corticosteroid bursts (≥3/year)frequently (46 % and 42 %, respectively) [10]. These clustering approaches have been validated in children [18] and in cohorts outside of this SARP cohort [19]. It is these clusters or groups of asthmatics that require the most attention in future clinical trials.
Brittle Asthma and Refractory Asthma
Brittle asthma, a term coined by Turner-Warwick [20] in the early 1970s may have been the first attempt to identify patients at risk for CAS. She described asthma patients with dramatic fluctuations in daily PEFR despite oral corticosteroids and she further divided them into two subtypes: Type I, with large variations in PEFR despite appropriate treatment, and Type II, with sudden, unexpected drops in PEFR during clinically stable period [21]. While both types of asthmatics are recognized as at high risk for CAS events, it is the Type II asthmatic that is particularly concerning because acute exacerbation does not necessarily follow worsening airway inflammation from a viral respiratory infection, increasing dyspnea, and more frequent rescue drug use. Of note, CAS can also develop following exposure to cleaning solutions, cigarette smoke, and chlorine all of which may cause sudden attacks increasing risk for rapid deterioration.
Type I brittle asthma is reminiscent of “refractory” asthma, a term adopted by the ATS in 2000 to describe a vexing outpatient asthma conundrum [11]. It was defined in adult patients as persistent impairment and poor response to otherwise appropriate and guideline-recommended drug therapy, for example, need for albuterol or an alternative short-acting bronchodilator, such as ipratropium bromide if albuterol is ineffective, for more than 2 days a week; an Asthma Control Test™ score less than 20 out of 25; FEV1 less than 80 % predicted; and increased risk from poorly controlled asthma despite 3 months of preferred treatment of asthma and/or two or more acute asthma exacerbations requiring rescue treatment, including prednisone, in the past year. The pathophysiology of refractory or Type I brittle asthma is not necessarily the same, but CAS events can occur with all of these patient groupings. Basic research on the pathophysiology of severe asthma or even fatal asthma will not necessarily pertain to the immediate management of all critical asthma patients but should have relevance to the secondary prevention of CAS.
Near-Fatal Asthma and Status Asthmaticus
While most asthma patients are at risk for fatal attacks, the majority of adult patients who have died actually had moderate or severe asthma [22]. Less than 1 % of asthmatics hospitalized in the ICU die from their disease, giving rise to the terms near-fatal asthma or status asthmaticus. Both status asthmaticus and near-fatal asthma are historical terms, akin to the term life-threatening asthma and all are still in use today by clinicians. Status asthmaticus is defined as an acute, severe asthma exacerbation that does not respond readily to initial intensive therapy (usually in the ED), while near-fatal or life-threatening asthma refer loosely to status asthmaticus that progresses to acute respiratory failure requiring non-invasive or invasive ventilatory support. While these descriptors were very useful at one time, their distinctions are now blurred. The increasing understanding of the spectrum and heterogeneity of asthma exacerbations warrants a more encompassing and simpler descriptor. CAS fits this need.
Recognizing and Evaluating Critical Asthma Syndrome
Every physician makes mistakes in the diagnosis and treatment of asthma exacerbation because of the prevalent pitfalls and mimics of asthma. The most common cause of “severe asthma” may be a misdiagnosis of asthma in lieu of other conditions (Table 1). No laboratory test or biomarker exists to readily distinguish the onset of CAS from less severe exacerbations that warrant a simple increase in controller therapy and can be managed easily at home, either by physicians or well-educated patients themselves. Lacking biomarkers, physician must be alert for clinical signals (Table 2); for example, the best predictor of adverse outcomes and excessive use of asthma control medications appears to be baseline FEV1. There are times, however, when CAS is an immediate concern; for example during the recent influenza H1N1 pandemic. The high prevalence rate of asthma (20–30 %) among all proven H1N1 cases that presented for medical attention immediately put physicians on alert for CAS [23, 24]. While most asthmatics had an uncomplicated course with this influenza strain, a few developed severe CAS, sometimes requiring hospital transfers to centers with capabilities for extracorporeal membrane oxygenation (ECMO) support.
Table 1.
Diseases and conditions that mimic critical asthma
|
Table 2.
Signs and symptoms of critical asthma syndrome
|
Knowledge Gaps in Critical Asthma Syndrome
Gaps in our knowledge and experience in critical asthma are many and obvious. They include an understanding of how to recognize CAS, how to coordinate and integrate hospital and outpatient resources including the sub-specialty expertise needed to properly care for severe asthmatics, how best to identify severe asthmatics promptly, when to further phenotype patients with critical asthma, in order to facilitate effective treatment and prevent future severe acute exacerbations.
The pathology of fatal asthma is defined from autopsy studies, and is understandably not defined during near-fatal, critical asthma events. Patients who die from asthma suffocate, usually from dense mucous impaction of the distal airways. While critical asthmatics may have extensive small airway mucous plugging, this may not be the defining characteristic of these patients pathologically. Rrepetitive epithelial injury, inflammation, and repair occur throughout the bronchial tree in asthma. There is increasing concern that the more distal airways (<5 mm) are untreated in this subset thereby affecting lung function, symptoms and work of breathing in 10 % or more of asthmatic individuals [25, 26]. Structural airway alterations occur with chronic inflammation leading to the phenomenon of adverse airway remodeling in asthma. Airway wall thickening, subepithelial collagen and matrix protein deposition, smooth muscle cell hypertrophy, vascular remodeling, and goblet cell metaplasia develop even in patients with mild asthma. In severe asthma, most or all of these changes are striking. Some studies show a correlation between airway wall thickness, a surrogate for remodeling as a whole, and lung function or asthma severity, but as with inflammatory mediators, remodeling changes should not be equated directly with severe asthma [27]. Improvements in imaging technology probably represent our best opportunity to begin to understand the degree to which structural airway changes occur in this group.
The use of beta-2 agonists, particularly LABAs, remains very controversial. The United States Food and Drug Administration (FDA) has ruled that LABAs cause asthma deaths. What happens to the asthmatic who has self-administered high dose beta agonists for several days at home? They are usually prescribed more beta-2 agonists. However, ultimately physicians hope to prescribe asthma medications based on pharmacogenomics, which may provide a clearer understanding of which patient may benefit the most from a particular drug.
Conclusion
How should CAS patients be treated? There is no consensus on corticosteroid type and dose, triage decisions, and follow up. Furthermore, asthma care in diverse healthcare settings is haphazard. The optimal therapy for asthma in adults should be determined by the patient’s favorable response to the drug. Even ICS are ineffective in controlling asthma symptoms in up to 46 % of asthma patients according to a NIH study [28]. There is no study that clearly shows that any drug therapy, including ICS, can alter the natural course of the disease in adults. The NAEPP recommendation to see asthma patients every 2 to 6 weeks for regular review of asthma control and drug side effects is pragmatic, allowing early detection of poor responses to treatments. If patients remain not well controlled or very poorly controlled after 3 months of treatment, we recommend that primary-care physicians refer patients promptly to an asthma specialist for consultation to reduce the frequency of acute exacerbations and prevent the development of CAS. The key in the treatment of CAS is prevention, recognition of CAS, and immediate admission to the acute setting for aggressive treatment.
Contributor Information
Nicholas Kenyon, Division of Pulmonary, Critical Care, Sleep Medicine, Department of Medicine, University of California, Davis, Davis, CA, USA.
Amir A. Zeki, Division of Pulmonary, Critical Care, Sleep Medicine, Department of Medicine, University of California, Davis, Davis, CA, USA
Timothy E. Albertson, Division of Pulmonary, Critical Care, Sleep Medicine, Department of Medicine, University of California, Davis, Davis, CA, USA. VA Northern California Healthcare System, VA Mather Hospital, Mather, CA, USA
Samuel Louie, Division of Pulmonary, Critical Care, Sleep Medicine, Department of Medicine, University of California, Davis, Davis, CA, USA. University of California, Davis, 4150 V Street, Suite 3400, Sacramento, CA 95817, USA.
References
- 1.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 2.Kroegel C. Global Initiative for Asthma (GINA) guidelines: 15 years of application. Expert Rev Clin Immunol. 2009;5:239–249. doi: 10.1586/eci.09.1. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro JM. Intensive care management of status asthmaticus. Chest. 2001;120:1439–1441. doi: 10.1378/chest.120.5.1439. [DOI] [PubMed] [Google Scholar]
- 4.Tsai CL, Lee WY, Hanania NA, Camargo CA. Age-related differences in clinical outcomes for acute asthma in the United States, 2006–2008. J Allergy Clin Immunol. 2012;129:1252–1258. doi: 10.1016/j.jaci.2012.01.061. [DOI] [PubMed] [Google Scholar]
- 5.Sly RM. Increases in deaths from asthma. Ann Allergy. 1984;53:20–25. [PubMed] [Google Scholar]
- 6.Greiling AK, Boss LP, Wheeler LS. A preliminary investigation of asthma mortality in schools. J Sch Health. 2005;75:286–290. doi: 10.1111/j.1746-1561.2005.00039.x. [DOI] [PubMed] [Google Scholar]
- 7.Moorman JE, Akinbami LJ, Bailey CM, et al. National surveillance of asthma: United States, 2001–2010. 2012;3:1–67. DHHS Publincation No. (PHS) 2013–1419. [PubMed] [Google Scholar]
- 8.Fuhlbrigge AL, Adams RJ, Guilbert TW, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the national asthma education and prevention program guidelines. Am J Respir Crit Care Med. 2002;166:1044–1049. doi: 10.1164/rccm.2107057. [DOI] [PubMed] [Google Scholar]
- 9.Peters SP, Jones CA, Haselkorn T, Mink DR, Valacer DJ, Weiss ST. Real-world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based survey. J Allergy Clin Immunol. 2007;119:1454–1461. doi: 10.1016/j.jaci.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119:405–413. doi: 10.1016/j.jaci.2006.11.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000;162:2341–2351. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 12.Bush A, Zar HJ. WHO universal definition of severe asthma. Curr Opin Allergy Clin Immunol. 2011;11:115–121. doi: 10.1097/ACI.0b013e32834487ae. [DOI] [PubMed] [Google Scholar]
- 13.Busse WW. Asthma diagnosis and treatment: filling in the information gaps. J Allergy Clin Immunol. 2011;128:740–750. doi: 10.1016/j.jaci.2011.08.014. [DOI] [PubMed] [Google Scholar]
- 14.Wenzel SE, Schwartz LB, Langmack EL, et al. Evidence that severe asthma can be divided pathologically into two inflammatory subtypes with distinct physiologic and clinical characteristics. Am J Respir Crit Care Med. 1999;160:1001–1008. doi: 10.1164/ajrccm.160.3.9812110. [DOI] [PubMed] [Google Scholar]
- 15.Woodruff PG, Modrek B, Choy DF, et al. T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med. 2009;180:388–395. doi: 10.1164/rccm.200903-0392OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amelink M, de Nijs SB, de Groot JC, van Tilburg PM, et al. Three phenotypes of adult-onset asthma. Allergy. 2013;68:674–680. doi: 10.1111/all.12136. [DOI] [PubMed] [Google Scholar]
- 17.Kim TB, Jang HS, Kwon JS, et al. Identification of asthma clusters in two independent Korean adult asthma cohorts. Eur Respir J. 2013;41(6):1308–1314. doi: 10.1183/09031936.00100811. [DOI] [PubMed] [Google Scholar]
- 18.Fitzpatrick AM, Teague WG, Meyers DA National Institutes of Health/National Heart, Lung, and Blood Institute Severe Asthma Research Program et al. Heterogeneity of severe asthma in childhood: confirmation by cluster analysis of children in the National Institutes of Health/National Heart, Lung, and Blood Institute Severe Asthma Research Program. J Allergy Clin Immunol. 2011;127(2):382–389. doi: 10.1016/j.jaci.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patrawalla PA, Kazeros L, Rogers Y, et al. Application of the asthma phenotype algorithm from the Severe Asthma Research Program to an urban population. PLoS One. 2012;7(9):e44540. doi: 10.1371/journal.pone.0044540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner-Warwick M. Provoking factors in asthma. British J Dis Chest. 1971;65:1–20. [PubMed] [Google Scholar]
- 21.Ayres JG, Miles JF, Barnes PJ. Brittle asthma. Thorax. 1998;53:315–321. doi: 10.1136/thx.53.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McFadden ER., Jr Fatal and near-fatal asthma. N Engl J Med. 1991;324:409–411. doi: 10.1056/NEJM199102073240609. [DOI] [PubMed] [Google Scholar]
- 23.McKenna JJ, Bramley AM, Skarbinski J, Fry AM, Finelle L, Jain S. Asthma in patients hospitalized with pandemic influenza A(H1N1)pdm09 virus infection-United States, 2009. BMC Infect Dis. 2009;13:57. doi: 10.1186/1471-2334-13-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mortensen E, Louie J, Pertowski C, et al. Epidemiology and outcomes of adults with asthma who were hospitalized or died with 2009 pandemic influenza A (H1N1) — California, 2009. Influenza Other Respir Viruses. 2013 doi: 10.1111/irv.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeffery PK. Remodeling in asthma and chronic obstructive lung disease. Am J Respir Crit Care Med. 2001;164:S28–S38. doi: 10.1164/ajrccm.164.supplement_2.2106061. [DOI] [PubMed] [Google Scholar]
- 26.Mauadk T, Bel EH, Sterk PJ. Asthma therapy and airway remodeling. J Allergy Clin Immunol. 2007;120:997–1009. doi: 10.1016/j.jaci.2007.06.031. [DOI] [PubMed] [Google Scholar]
- 27.Brewster CE, Howarth PH, Djukanovic R, Wilson J, Holgate ST, Roche RW. Myofibroblasts and subepithelial fibrosis in bronchial asthma. Am J Respir Cell Mol Biol. 1990;3:507–511. doi: 10.1165/ajrcmb/3.5.507. [DOI] [PubMed] [Google Scholar]
- 28.Martin RJ, Szefler SJ, King TS, et al. The Predicting Response to Inhaled Corticosteroid Efficacy (PRICE) trial. J Allergy Clin Immunol. 2007;119:73–80. doi: 10.1016/j.jaci.2006.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]