Abstract
Purpose
Oocyte vitrification is currently used for human fertility preservation. However, vitrification damage is a problem caused by decreasing ooplasmic levels of glutathione (GSH). The GSH donor glutathione ethyl ester (GSH-OEt) can significantly increase the GSH content in oocytes. However, it is difficult to obtain oocyte from woman. To overcome this, we used mouse oocytes to replace human oocytes as a model of study.
Methods
Oocytes from B6D2F1 mice were preincubated for 30 min with 2.5 mmol/L GSH-OEt (GSH-OEt group), without GSH-OEt preincubation before vitrification (control vitrification group) or in nonvitrified oocytes (fresh group). After thawing, oocytes were fertilized for evaluating the developmental competence of embryos in vitro and in vivo. Immunofluorescence, Polscope equipment and quantitative reverse transcription polymerase chain reaction (RT–qPCR) were used to analyze damage, including mitochondrial distribution, reactive oxygen species (ROS) levels, spindle morphology, and gene expression levels (Bcl-2, BAX, and MnSOD).
Results
The rates of fertilization, 3–4 cell, blastocyst formation and expanded blastocysts were significantly higher (p < 0.05) in the GSH-OEt group (90.4%; 91.1%; 88.9% and 63.0%) than in the control (80.0%; 81.4%; 77.7% and 50.5%). Provided embryos overcame the 2-cell block and developed to the blastocyst stage, birth rates of all groups were similar. Vitrification altered mitochondrial distribution, increased ROS levels, and caused abnormal spindle morphology; GSH-OEt preincubation could improve such damage. RT–qPCR showed that the expression of Bcl-2 was lower in the control group compared with the GSH-OEt group; BAX and MnSoD expression levels were higher in the control group than in the GSH-OEt group (p < 0.05).
Conclusions
The beneficial effect of GSH-OEt preincubation occurred before the 2-cell stage.
Keywords: Oocytes, Vitrification, Glutathione ethyl ester, Cryodamage, Embryo quality
Introduction
Oocyte vitrification is a promising new technique in human-assisted reproductive technology (ART), especially for establishing egg banks and female fertility preservation [1, 2]. This technique has been improved and innovated, including enhanced vitrification methods and cryoprotectants [3, 4], but it still has some problems and challenges. After oocyte vitrification, there are some problems compared with the use of fresh oocytes, such as low embryo development competence and implantation capacity in humans [5, 6] and mice [7, 8]. It has been confirmed that oocyte vitrification causes mitochondrial dysfunction [9]. Increased levels of reactive oxygen species (ROS) are characteristic of mitochondrial dysfunction [10]. Normally, ROS in mitochondria are catalyzed by manganese superoxide dismutase (MnSOD) [11]. If the accumulation of ROS cannot be eliminated in time, ROS induce apoptosis [12] via Bcl-2 family leading to low developmental competence [13], including downregulation of the anti-apoptotic gene Bcl-2 and upregulation of the apoptotic gene BAX [14]. On the other hand, high oxidative stress in vitro and cryopreservation can cause spindle damage [15, 16]. The current solution for these adverse effects is to prolong incubation time to enable microtubule reassembly in forming a spindle. However, the temporal fertilization window of metaphase II stage oocytes might be rather short [17].
As an antioxidant that can reduce the effect of ROS, glutathione (GSH) is a major nonenzymatic antioxidant in oocytes [18]. It ensures the correct assembly of microtubules, prevents ROS from attacking tubulin assembly, and maintains normal spindle function during meiosis [19, 20]. In addition, embryo development can be delayed and apoptosis increased as a result of decreased intracellular levels of GSH [21]. Oocytes and early embryos have a limited capability to synthesize GSH until they develop to the blastocyst stage. Before this stage, extracellular GSH cannot penetrate the cell membrane or enter the oocytes/embryos, which must rely on the γ-glutamyl cycle from surrounding cumulus cells for absorbing thiols such as β-mercaptoethanol and cysteine, which are then synthesized to GSH for early embryo metabolism [22, 23]. Therefore, denuded oocytes contain less GSH than intact cumulus–oocyte complexes (COCs) [24]. However, we often remove cumulus cells from around oocytes before vitrification, which itself is an unfavorable factor. Somfai et al. [10] reported that the concentration of GSH in oocytes decreased after vitrification, leading to a low fertilization rate and poor developmental competence. From this perspective, Gupta et al. [25] reported that adding β-mercaptoethanol could reduce the ROS levels significantly and improve the cleavage rate in vitrified–thawed oocytes, and compared with fresh oocytes, the developmental competence was still poor. Therefore, it was suggested that merely adding these small thiols into the cryopreservation solution cannot produce enough GSH because of cryodamage to the oocyte’s metabolism.
In 2008, Curnow et al. [26] found that the GSH donor glutathione ethyl ester (GSH-OEt) significantly increased the GSH content of primate oocytes subjected to in vitro maturation (IVM). This is a fat-soluble small molecule, which penetrates cell membranes efficiently without relying on the γ-glutamyl cycle. Subsequently, they confirmed [27] that 5 mmol/L GSH-OEt could enhance the efficient GSH concentration in IVM oocytes, and significantly improved the oocyte maturation rate, fertilization rate, and spindle morphology. IVM oocytes were similar to vitrified oocytes, with high ROS and low GSH levels. Therefore, here, we focused on the effectiveness of adding GSH-OEt during cryopreservation and evaluated whether it could reduce oxidative stress and improve the developmental competence of fertilized vitrified oocytes. Considering the difficulty and ethical problems of obtaining human oocytes for ART research, we used mouse oocytes as a model.
Methods
Oocyte retrieval and procedure
Oocytes were collected from 5 to 6-week-old B6D2F1 (BDF1) female mice, which were superovulated by injecting 10 IU pregnant mare serum gonadotropin (Shusheng Hormone Factory, People’s Republic of China), followed by injecting 10 IU human chorionic gonadotropin (hCG, Lizhu, Zhuhai People’s Republic of China) 48 h later. Mice were euthanized 14 h post-hCG injection, and the oviducts were removed and dissected out. COCs were obtained under stereoscopic microscopy and then denuded of cumulus cells in 80 IU/mL hyaluronidase (Sage IVF, Trunbull, CT, USA). We retained MII oocytes for use in experiments, discarding germinal vesicle and MI stage oocytes.
Grouping and vitrification
Oocytes were divided randomly into three groups: (1) fresh untreated control group, (2) control vitrified oocytes without GSH-OEt, and (3) GSH-OEt preincubated group (GSH-OEt group). For this treatment, 2.5 mmol/L GSH-OEt was added into Human Tubal Fluid culture medium (HTF, Irvine Scientific, Santa Ana, CA, USA) with 10% Serum Substitute Supplement (SSS, Irvine Scientific, Santa Ana, CA, USA) and preincubated for 30 min before vitrification. Kitazato Vitrification Kits (Kitazato BioPharmaceuticals, Shizuoka, Japan) were used for cryopreservation. Oocytes were vitrified by a two-step procedure in equilibration solution (ES) for 5 min, followed by vitrification solution (VS) for 1 min. Then, oocytes were placed in a Cryotop and plunged directly into liquid nitrogen. In our preliminary experiments, we set up three different concentrations of 0.5, 2.5, and 5 mmol/L of GSH-OEt adding to HTF to determine the best concentration. We found that the effects between 2.5 and 5 mmol/L were similar, and 0.5 mmol/L was not ideal. Therefore, we believe that at least 2.5 mmol/L GSH-OEt is optimal. At the same time, we performed oocytes for GSH analysis, as described by Curnow et al. [27].
Thawing
Thawing was done in four steps: First, thawing solution (TS) was pre-warmed at 37 °C for 20 min; then the Cryotop was placed into thawing solution (TS) for 1 min, immediately after collecting oocytes, and then moved into diluent solution (DS) and washing solutions (WS1 and WS2) for 3 min each. Finally, any surviving oocytes were moved into HTF medium and maintained in a 5% CO2 incubator for 2 h waiting for fertilization or analysis.
In vitro fertilization, culture, and blastocyst transfer
On the day of fertilization, 10–12-week-old B6D2F1 (BDF1) adult male mice were euthanized. The tail of the epididymis was punctured to obtain sperm suspensions, which were transferred into the center of 200 μL HTF droplets and maintained in a 5% CO2 incubator for 1 h for capacitation. The sperm suspension from the HTF droplets was used for fertilization in vitro at a final concentration of 4 × 106/mL. The fresh control group had 261 oocytes; the vitrified control group had 280 oocytes and the GSH-OEt group had 180 oocytes. We observed fertilization 6 h later and transferred zygote into Continuous Single Culture (CSC, Irvine Scientific, Santa Ana, CA, USA) with 10% SSS, for culturing. We recorded the numbers of 2-cell cleaved embryos at 1 day post-fertilization, of 3–4-cell at 2 days post-fertilization, and the numbers of blastocysts and expanded blastocysts 4 days post-fertilization. Expanded blastocyst is a blastocyst with grade 4 (an expanded blastocyst with a blastocoel volume larger than that of the early embryo, with a thinning zona) or higher, as described by Gardner. [28].
We used 8–10-week-old ICR female mice as recipients. These had been mated with vasectomized male mice to induce pseudopregnancy. We observed vaginal plugs the next day and selected eight to ten blastocysts to be transferred into each oviduct. Each group had six recipients. In the fresh group, we transferred 108 blastocysts to recipients; in the control vitrification group, we transferred 116 blastocysts; and in the GSH-OEt group, we transferred 105 blastocysts. Finally, we performed cesarean operations on the recipients 18 days later and recorded the birth rate, birth weights, and placental weights.
Distribution of mitochondria and ROS levels
Twenty oocytes in each group were studied for the distribution of mitochondria. Mitochondria and nuclei were stained with 50 nM Mitotracker Red CMXRos (Invitrogen, Carlsbad, CA, USA) and 4′,6-diamidino-2-phenylindole (DAPI) in four-well dishes for 20 min, and then washed three times with culture medium to remove the dyes. A laser scanning confocal microscope (Leica, Wetzlar, Germany) was used for examination at an excitation wavelength for Mitotracker Red CMXRos of 579 nm, and an emission wavelength of 599 nm. The excitation wavelength for DAPI staining was 358 nm, and the emission wavelength was 461 nm.
Oocytes were incubated in 10 μmol/L 2′,7′-dichlorofluorescin diacetate (DCFH-DA; Sigma-Aldrich, St Louis, MO, USA) at 37 °C for 20 min and then washed in phosphate-buffered saline (PBS) three times to remove the dye. In the fresh control group, we used 31 oocytes; in the control vitrification group, there were 30 oocytes; and in the GSH-OEt group, there were 32 oocytes. Laser scanning confocal microscopy (Leica, Wetzlar, Germany) was used to detect the ROS fluorescence intensity. The excitation emission wavelength was 488 nm and that for emitted wavelength was 550 nm. Fluorescence intensities were quantified using ImageJ software (https://imagej.nih.gov/ij/; National Institutes of Health, Bethesda, MD, USA).
Spindle morphology analysis
Oocytes were placed in glass-bottomed culture dishes and observed using a Polscope system (Oosight Imaging System, Woburn, MA, USA). There were 55 oocytes in the fresh control group, 54 in the control vitrified group, and 59 in the GSH-OEt group. Spindles with a fusiform or barrel shape were considered as normal morphology. Then, previously observed oocytes from the three groups were fixed in 4% paraformaldehyde at 37 °C and permeabilized using 0.5% Triton X-100 in PBS for 30 min. Then, the oocytes were transferred into a solution of monoclonal anti-α-tubulin antibody (Sigma-Aldrich) at dilution of 1:2000, washed three times in PBS before being transferred into fluorescein isothiocyanate (FITC)-conjugated anti-mouse IgG (Sigma-Aldrich) with 0.5% BSA, and incubated for 2 h in the dark. Propidium iodide (PI) staining was carried out for observation of nuclei. Laser scanning confocal microscopy (Leica, Wetzlar, Germany) was used to detect staining. The excitation wavelength for FITC was 495 nm, and the emitted wavelength was 521 nm. The excitation wavelength for PI was 540 nm and the emitted wavelength was 608 nm.
Quantitative reverse transcription polymerase chain reaction (RT–qPCR) amplification for the Bcl-2, BAX, and manganese superoxide dismutase (MnSOD) genes
Fifty oocytes in each group were transferred into 2 μL 0.5% NP 40 lysis buffer (Beyotime, People’s Republic of China) with a small amount of culture medium and quickly transferred into PCR tubes at − 80 °C. RT–qPCR kits (Takara, Otsu, Japan) were used for carrying out reverse transcription into cDNA. The primers were designed as follows: Bcl-2 sense (5′-3′), CTGCACCTGACGCCCTTCACC and anti-sense (5′-3′), CACATGACCCCACCGAACTCAAAGA (119 bp product); BAX sense (5′-3′), TGGAGCTGCAGAGGATGATT and anti-sense (5′-3′), GATCAGCTCGGGCACTTTAG (180 bp); MnSOD sense (5′-3′), TGTTACAACTCAGGTCGCTCTTCA and anti-sense (5′-3′), GAACCTTGGACTCCCACAGACA (204 bp); and GAPDH sense (5′-3′), CCTCGTCCCGTAGACAAAATGGT and anti-sense (5′-3′), TTGAGGTCAATGAAGGGGTCGT (140 bp). Finally, 5-μL aliquots of the reaction solution were separated by electrophoresis in a 2% agarose gel. The bands were visualized and quantified using GAPDH as an internal control.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics Software (v. 20; IBM Corp., Armonk, NY, USA). Chi-squared tests or analysis of variance (ANOVA) were applied as appropriate. Data were tested for normality before applying ANOVA, and results are presented as the mean ± standard error of the mean. Comparisons between pairs of groups were done using the Student–Newman–Keuls test. Differences at p < 0.05 were considered significant.
Results
GSH-OEt preincubation improved the developmental potential of vitrified oocytes
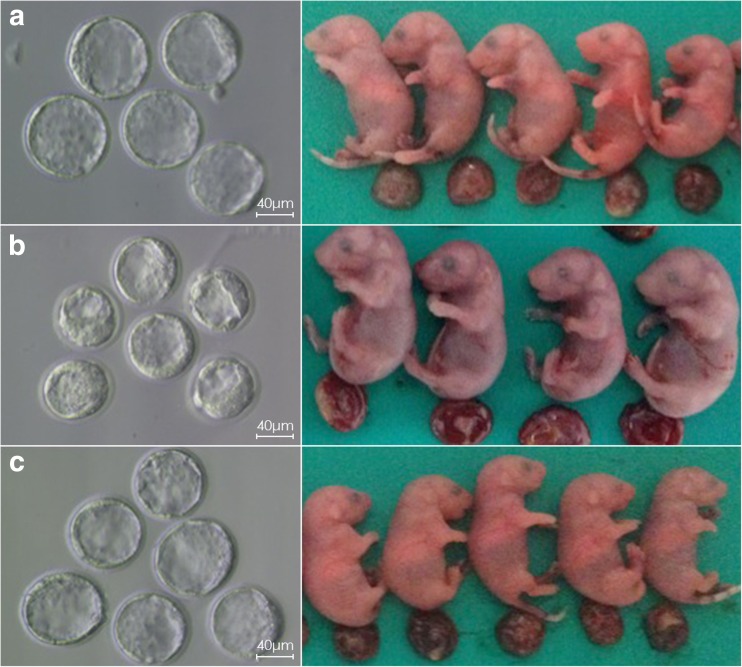
Vitrification led to poor developmental competence, including the rates of fertilization and growth to 3–4-cell embryos, blastocysts, and expanded blastocysts, compared with fresh oocytes (p < 0.05, Table 1). However, among the vitrified oocytes, GSH-OEt preincubation could improve outcomes, including fertilization rates (90.4 vs. 80.0%; p < 0.05), 3–4-cell formation (91.1 vs. 81.4%; p < 0.05), blastocyst formation (88.9 vs. 77.7%; p < 0.05), and expanded blastocyst (63.0 vs. 50.5%; p < 0.05). The cleavage and birth rates, and birth and placental weights showed no significant differences among the three groups. Under stereoscopic microscopy on day 4, the blastocoels from fresh oocytes were completely expanded, with a thinning zona, and hatching/hatched blastocysts were observed (Fig. 1a). 77.9% of blastocysts were expanded. The expanded blastocysts for the vitrification control group were low (50.5%), and no hatching blastocysts were found (Fig. 1b). In GSH-OEt group, some hatching/hatched blastocysts were seen, and 63.0% of blastocysts were expanded (Fig. 1c).
Table 1.
Developmental competence and results of blastocyst transfer from three groups
| Group oocytes | Survived oocytes | Fertilization | Cleavage | 3–4-cell | Blastocyst | Expanded blastocyst | Number of birth/transfer | Birth weight | Placental weight |
|---|---|---|---|---|---|---|---|---|---|
| Fresh 261 | 245 (93.9%)a | 222 (90.6%) | 218 (98.2%)ac | 209 (94.1%)a | 173 (77.9%)ac | 56/108 (51.9%) | 1.27 ± 0.20 | 0.14 ± 0.03 | |
| Control 280 | 265 (94.6%) | 212 (80.0%)ab | 188 (88.7%) | 153 (81.4%)ab | 146 (77.7%)ab | 95 (50.5%)ab | 53/116 (45.8%) | 1.34 ± 0.21 | 0.12 ± 0.04 |
| GSH-OEt 180 | 167 (92.8%) | 151 (90.4%)b | 135 (89.4%) | 123 (91.1%)bc | 120 (88.9%)b | 85 (63.0%)bc | 50/105 (47.6%) | 1.21 ± 0.11 | 0.12 ± 0.02 |
Differences in the fertilization rate, 3–4-cell, blastocyst rates, and expanded blastocysts among the three groups were significant (p < 0.05). Values with different superscripts within a column are significantly different (p < 0.05)
Fig. 1.
Blastocysts at the same time point, newborn mice, and the placental morphology of three groups are shown. a Fresh oocytes; the blastocoels were completely expanded, with a thinning zona pellucida and hatching/hatched blastocysts present. b The blastocoels in the control vitrification group were less than or equal to the volume of the embryo; there were no hatching/hatched blastocysts. c Blastocoel expansion in the GSH-OEt group was larger with some hatching/hatched blastocysts
GSH-OEt preincubation before vitrification improved mitochondrial distribution and reduced the levels of ROS
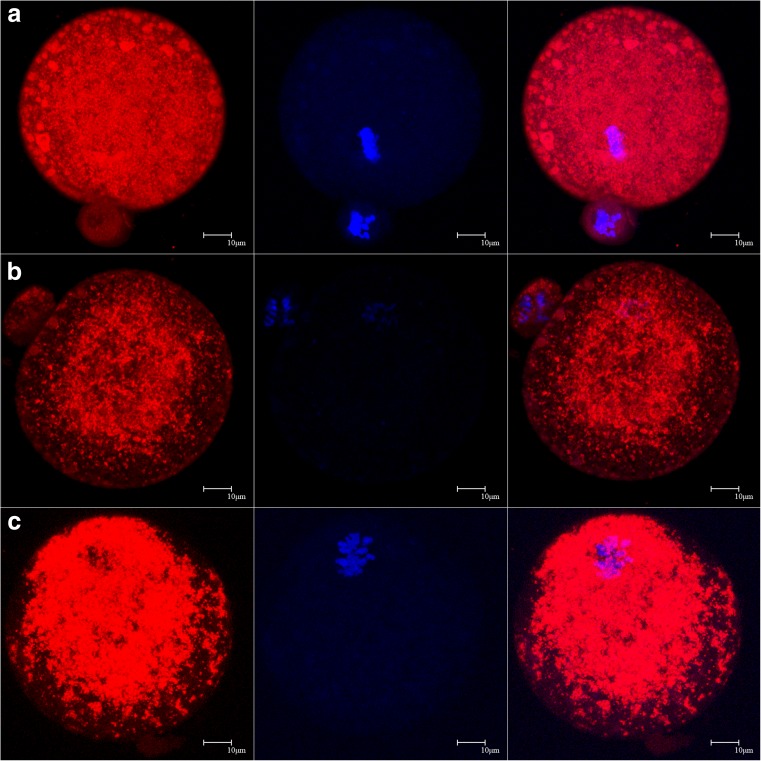
The mitochondria were evenly distributed in the cytoplasm of fresh oocytes (Fig. 2a), but this feature was largely absent in the control vitrification group and mitochondria were only distributed as clumps in the central region rather than the periphery (Fig. 2b). However, mitochondria in the GSH-OEt group also gathered as clumps around nuclei, and there was less loss of mitochondria (Fig. 2c).
Fig. 2.
Mitochondrial distributions of the three groups are shown. a Fresh group showing evenly distributed mitochondria. b Control vitrification group showing absence of mitochondria, distributed as clumps in the central region rather than the periphery. c GSH-OEt group showing fewer mitochondria also clumped around the nuclei
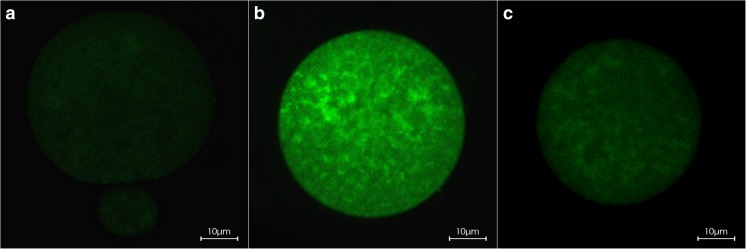
ROS staining in fresh oocytes had low fluorescence intensity (n = 31, 25.17 ± 5.88) (Fig. 3a). Fluorescence intensity became significantly enhanced in the control vitrification group (n = 30, 70.72 ± 28.04) (Fig. 3b), in which many high-intensity streaks were seen (Fig. 3b). However, the fluorescence intensity of GSH-OEt group was lower than in the control group, and some streaks were also found (n = 32, 35.52 ± 8.24) (Fig. 3c). There were significant differences between the three groups (p < 0.05).
Fig. 3.
ROS staining patterns of the three groups are shown. a Fresh group showing the lowest fluorescence intensity, evenly distributed (n = 31, 25.17 ± 5.88). b Control vitrification group showing markedly enhanced fluorescence intensity with many high-intensity streaks (n = 30, 70.72 ± 28.04). c GSH-OEt group showing low fluorescence intensity with some intense streaks (n = 32, 35.52 ± 8.24). There were significant differences between the three groups (p < 0.05)
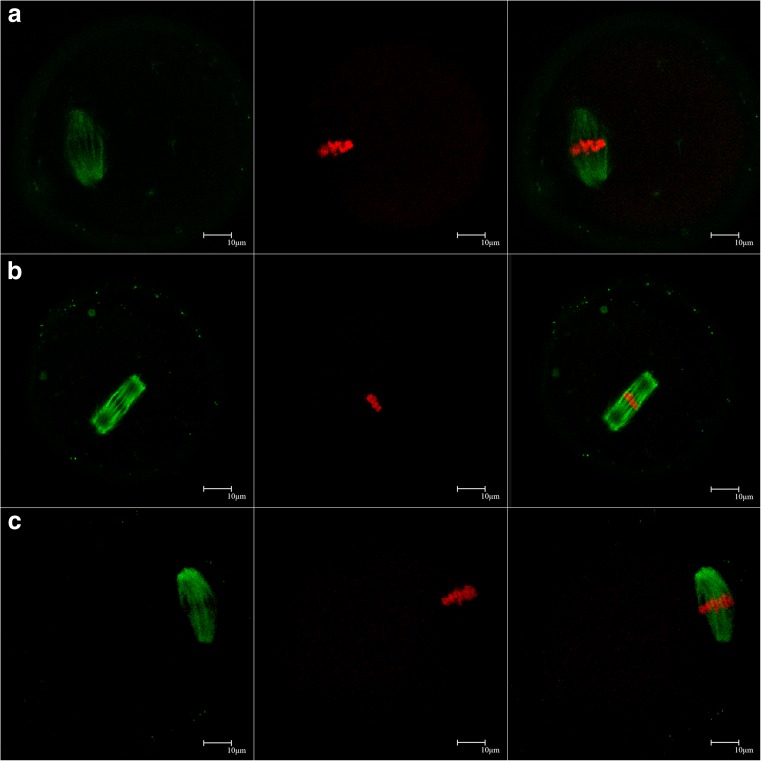
GSH-OEt preincubation before vitrification maintained the normal structure of the spindle
Under the Polscope, the proportions of oocytes with normal spindles in the fresh, control vitrification group, and GSH-OEt group were 81.8, 53.7, and 72.9% after warming for 2 h with significant differences between the groups (p < 0.05, Table 2). Normal spindles appeared as fusiform or barrel shapes (Fig. 4a). Spindles in the control group were elongated, fusiform, or absent (Fig. 4b). The spindles in the GSH-OEt group had barrel shapes (Fig. 4c). Under laser scanning confocal microscope, the fresh group spindles were fusiform (Fig. 5a). However, they appeared as rectangles and larger in the control vitrification group compared with the fresh group (Fig. 5b). Spindles in the GSH-OEt group were fusiform and elongated, as with fresh oocytes (Fig. 5).
Table 2.
Rates of normal spindle formation in the three groups
| Group | Oocytes | Normal spindle | Abnormal spindle or absent |
|---|---|---|---|
| Fresh | 55 | 45 (81.8%)b | 10 (18.2%) |
| Control | 54 | 29 (53.7%)ab | 25 (46.3%) |
| GSH-OEt | 59 | 43 (72.9%)a | 16 (27.1%) |
Values with different superscripts within a column are significantly different (p < 0.05)
Fig. 4.
Polscope images of spindles of the three groups are shown. a In the fresh group, spindles appeared as fusiform or barrel shaped. b In the control vitrification group, spindles were elongated like “earthworms” or absent. c In the GSH-OEt group, spindles were barrel shaped
Fig. 5.
The patterns of spindles and chromosomes of three groups are shown. a Fresh group showing small fusiform spindles. b Control vitrification group showing the spindles presenting as large rectangular profiles. c GSH-OEt group showing the spindles to be enlarged and fusiform
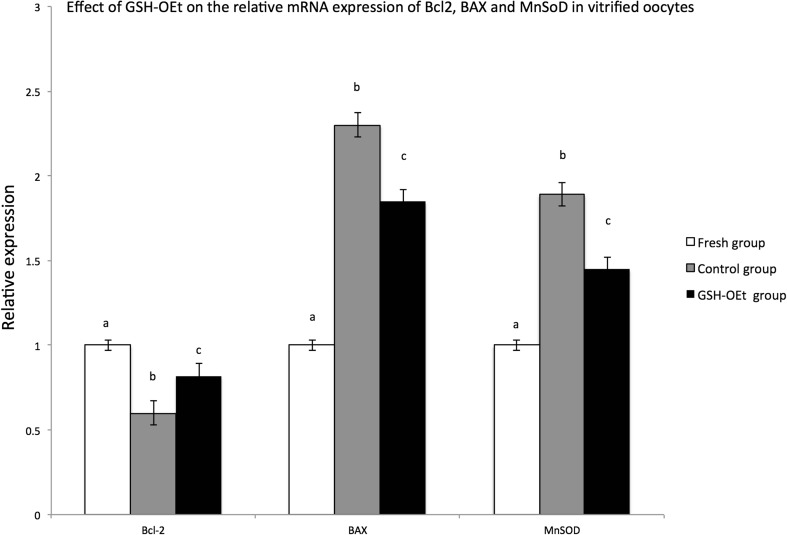
RT–qPCR for Bcl-2, BAX, MnSOD
Bcl-2 expression was lower in the control group compared with the GSH-OEt group (Fig. 6, p < 0.05). BAX and MnSoD expression levels were both increased in the GSH-OEt group and were highest in the control vitrification group (p < 0.05).
Fig. 6.
Effect of GSH-OEt on the mRNA expression levels relative to GAPDH of Bcl2, BAX, and MnSoD in vitrified oocytes. Values with different superscripts are significantly different (p < 0.05)
Discussion
In 2012, the American Society for Reproductive Medicine decided that oocyte vitrification would no longer be seen as an experimental technology, but as part of routine ART [29]. Because of the urgent need to develop this technology for oocyte donation and egg banking, the targets of reducing cryopreservation damage and improving developmental competence have been of high priority. We noted study of Curnow et al. [27] on primate oocytes, only 5 mmol/L GSH-OEt significantly increased the oocyte GSH content. However, GSH contents between the 2.5 mmol/L and 5 mmol/L levels were no different in mouse oocytes. Species specificity might explain this difference. Primate oocytes are larger than mouse oocytes, so must require greater GSH-OEt concentrations.
Vitrification leads to zona pellucida (ZP) hardening by premature cortical granule exocytosis [30]. ZP hardens owing to the polymerization of disulfide bonds and modification of the ZP glycoproteins [31, 32]. GSH promotes fertilization by reducing the number of disulfide bonds [32, 33]. Moreover, disrupted mitochondrial function and ATP depletion by ROS, damage to the cytoskeleton and altered meiotic spindle assembly are also responsible for low fertilization rates [34–37]. On the one hand, polymerization of spindle tubulin may itself depend on sulfhydryl (–SH) groups [38]. On the other hand, increased ROS from vitrification can attack microtubules and interfere with spindle formation [16, 39]. Furthermore, vitrified oocytes with enlarged spindles whose microtubules polymerized excessively are likely to yield abnormalities in chromosomal segregation, fertilization failure, and abnormal fertilization [40]. We surmise that GSH-OEt plays an important role as a provider of –SH groups. In addition, it also reduced ROS levels and kept tubulin from being attacked. Combining these two aspects of the role, GSH-OEt eventually promoted formation of normal spindles and increased the fertilization rate.
We defined three regions of MII oocytes: namely the periphery, intermediate region, and central perinuclear region. In our study, fresh oocytes showed evenly distributed mitochondria. However, it has been reported previously that mitochondrial distribution in fresh oocytes was throughout the periphery and intermediate cytoplasm [41], peripherally or evenly distributed [42], or in the perinuclear region [43]. We suspect that this difference might arise from studying different mouse strains. Our results for vitrified oocytes were similar to previous reports of altered mitochondrial distribution being clumped and decreased in the periphery [41, 43]. Mitochondrial distribution in oocytes is dependent on microtubules, which are damaged by vitrification leading to mitochondrial redistribution and low developmental competence or development block [43–45]. GSH-OEt treatment as antioxidant had obvious effects on protecting mitochondria from such damage, but it is unclear whether it can play a protective role in cytoplasmic microtubules because of the persistence of abnormal distributions in our GSH-OEt group. Furthermore, vitrification damages mitochondrial function, including to a decline in mitochondrial membrane potential and ATP depletion [9, 46]. Thus, it resulted in a decline in developmental competence [47]. Normally, The expression levels of the MnSOD gene increases with increasing levels of ROS, which is consistent with the results of ROS staining in our study. High level of ROS will continue to produce toxic effects on mitochondria, causing swelling. Then, the series of biochemical changes to apoptotic signals such as Bcl-2 family would be activated inside and outside the mitochondrial membrane [48]. Thus, the expression of Bcl-2 and BAX in the GSH-OEt group has helped avoid apoptosis, compared with the control group.
In our study, we found that the developmental competence improved by GSH-OEt did not include the initial cleavage rate. In other words, developmental competence after the 2-cell stage differed between the control vitrification and GSH-OEt groups. In mouse embryogenesis, many strains cease development at the 2-cell stage, known as the “2-cell block” [49], which is suggested to be caused by the accumulation of ROS, the inactivation of maturation-promoting factor (MPF) dephosphorylation and delay of zygotic gene activation (ZGA) [13, 50, 51]. In addition to ROS, vitrification cause “2-cell block,” which may also be related to MPF and ZGA [52, 53]. However, we found that once embryos overcame this block, they could develop to the blastocyst stage and produce birth rates that were no different from fresh controls. These promising results were similar to some previous reports [6, 54, 55]. Therefore, the protective effect of GSH-OEt was mainly reflected before the 2-cell stage. How GSH-OEt counteracted the development block remains unclear, besides the degradation of ROS. Furthermore, poor developmental competence also represents developmental delay. We observed the morphology of blastocysts among the three groups at the same time point. According to Gardner’s blastocyst grading scheme [28] with a higher stage being more mature, blastocysts from the control vitrification group were only at the early stages 3–4. This phenomenon might be related to the following three factors: (1) the time of overcoming the 2-cell block differed between groups, so the subsequent development speed also differed; (2) this explained the degree of damage as extra time is needed to repair the damage in order that embryos can reach next growth and development cycle [56]; and (3) ROS accumulation caused oocytes or embryos to undergo developmental arrest [13]. Obviously, the speed of development in three groups was negatively correlated with ROS levels.
Our study had many limitations. How GSH-OEt acts on microtubule assembly is still unclear, and more research is needed to focus on it. Moreover, the GSH metabolic pathways in human oocytes are poorly known and can only be tested indirectly in cumulus cells or follicular fluid [57, 58]. Mouse oocytes are similar to those of humans including their structure and metabolism. Even though the study had a good outcome for mouse oocytes, whether it can be applied to human oocytes is still unknown. We plan to understand the GSH synthesis mechanism of human oocytes by cumulus cells and pre-incubate IVM oocytes with GSH-OEt in future research. However, such studies first need to be approved by patients and our Ethics Committee.
Conclusions
Oocyte vitrification could cause damage and poor developmental competence. GSH-OEt preincubation could improve it before the developmental block at the 2-cell stage. Provided embryos can overcome this block, even though they slowly developed to the blastocyst, the birth rates were not affected. Our study casts new light on the roles of GSH-OEt in oocyte vitrification, but many mechanisms of how it acts are still unclear. Further studies are needed to understand GSH mechanisms and improve vitrification damage.
Funding
Natural Science Foundation of China (No. 81601342) from Dr Yijuan Sun
Compliance with ethical standards
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Footnotes
Zhichao Li and Ruihuan Gu contributed equally to this work.
Contributor Information
Yun Feng, Phone: 86 21 6437 4262, Email: artruijin1@163.com.
Yijuan Sun, Phone: +86 21 6345 5468, Email: sunyijuansub@126.com.
References
- 1.Stoop D, Nekkebroeck J, Devroey P. A survey on the intentions and attitudes towards oocyte cryopreservation for non-medical reasons among women of reproductive age. Hum Reprod. 2011;26(3):655–661. doi: 10.1093/humrep/deq367. [DOI] [PubMed] [Google Scholar]
- 2.Noyes N, Labella PA, Grifo J, Knopman JM. Oocyte cryopreservation: a feasible fertility preservation option for reproductive age cancer survivors. J Assist Reprod Genet. 2010;27(8):495–499. doi: 10.1007/s10815-010-9434-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seet VY, Al-Samerria S, Wong J, Stanger J, Yovich JL, Almahbobi G. Optimising vitrification of human oocytes using multiple cryoprotectants and morphological and functional assessment. Reprod Fertil Dev. 2013;25(6):918–926. doi: 10.1071/RD12136. [DOI] [PubMed] [Google Scholar]
- 4.Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod BioMed Online. 2005;11(3):300–308. doi: 10.1016/S1472-6483(10)60837-1. [DOI] [PubMed] [Google Scholar]
- 5.Siano L, Engmann L, Nulsen J, Benadiva C. A prospective pilot study comparing fertilization and embryo development between fresh and vitrified sibling oocytes. Conn Med. 2013;77(4):211–217. [PubMed] [Google Scholar]
- 6.Potdar N, Gelbaya TA, Nardo LG. Oocyte vitrification in the 21st century and post-warming fertility outcomes: a systematic review and meta-analysis. Reprod BioMed Online. 2014;29(2):159–176. doi: 10.1016/j.rbmo.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Abedpour N, Rajaei F. Vitrification by Cryotop and the maturation, fertilization, and developmental rates of mouse oocytes. Iran Red Crescent Med J. 2015;17(10):e18172. doi: 10.5812/ircmj.18172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kohaya N, Fujiwara K, Ito J, Kashiwazaki N. Generation of live offspring from vitrified mouse oocytes of C57BL/6J strain. PLoS One. 2013;8(3):e58063. doi: 10.1371/journal.pone.0058063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manipalviratn S, Tong ZB, Stegmann B, Widra E, Carter J, DeCherney A. Effect of vitrification and thawing on human oocyte ATP concentration. Fertil Steril. 2011;95(5):1839–1841. doi: 10.1016/j.fertnstert.2010.10.040. [DOI] [PubMed] [Google Scholar]
- 10.Somfai T, Ozawa M, Noguchi J, Kaneko H, Kuriani Karja NW, Farhudin M, Dinnyés A, Nagai T, Kikuchi K. Developmental competence of in vitro-fertilized porcine oocytes after in vitro maturation and solid surface vitrification: effect of cryopreservation on oocyte antioxidative system and cell cycle stage. Cryobiology. 2007;55(2):115–126. doi: 10.1016/j.cryobiol.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Sun J, Chen Y, Li M, Ge Z. Role of antioxidant enzymes on ionizing radiation resistance. Free Radic Biol Med. 1998;24(4):586–593. doi: 10.1016/S0891-5849(97)00291-8. [DOI] [PubMed] [Google Scholar]
- 12.Simon HU, Haj-Yehia A, Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5(5):415–418. doi: 10.1023/A:1009616228304. [DOI] [PubMed] [Google Scholar]
- 13.Favetta LA, St John EJ, King WA, Betts DH. High levels of p66shc and intracellular ROS in permanently arrested early embryos. Free Radic Biol Med. 2007;42(8):1201–1210. doi: 10.1016/j.freeradbiomed.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Taghavi SA, Valojerdi MR, Moghadam MF, Ebrahimi B. Vitrification of mouse preantral follicles versus slow freezing: morphological and apoptosis evaluation. Anim Sci J. 2015;86(1):37–44. doi: 10.1111/asj.12244. [DOI] [PubMed] [Google Scholar]
- 15.Chen SU, Lien YR, Chen HF, Chao KH, Ho HN, Yang YS. Open pulled straws for vitrification of mature mouse oocytes preserve patterns of meiotic spindles and chromosomes better than conventional straws. Hum Reprod. 2000;15(12):2598–2603. doi: 10.1093/humrep/15.12.2598. [DOI] [PubMed] [Google Scholar]
- 16.Choi WJ, Banerjee J, Falcone T, Bena J, Agarwal A, Sharma RK. Oxidative stress and tumor necrosis factor-alpha-induced alterations in metaphase II mouse oocyte spindle structure. Fertil Steril. 2007;88(4 Suppl):1220–1231. doi: 10.1016/j.fertnstert.2007.02.067. [DOI] [PubMed] [Google Scholar]
- 17.Somfai T, Kikuchi K, Nagai T. Factors affecting cryopreservation of porcine oocytes. J Reprod Dev. 2012;58(1):17–24. doi: 10.1262/jrd.11-140N. [DOI] [PubMed] [Google Scholar]
- 18.Day BJ. Catalase and glutathione peroxidase mimics. Biochem Pharmacol. 2009;77(3):285–296. doi: 10.1016/j.bcp.2008.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oliver JM, Albertini DF, Berlin RD. Effects of glutathione-oxidizing agents on microtubule assembly and microtubule-dependent surface properties of human neutrophils. J Cell Biol. 1976;71(3):921–932. doi: 10.1083/jcb.71.3.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zuelke KA, Jones DP, Perreault SD. Glutathione oxidation is associated with altered microtubule function and disrupted fertilization in mature hamster oocytes. Biol Reprod. 1997;57(6):1413–1419. doi: 10.1095/biolreprod57.6.1413. [DOI] [PubMed] [Google Scholar]
- 21.Lee CS, Koo DB, Fang N, Lee Y, Shin ST, Park CS, Lee KK. Potent and stage-specific action of glutathione on the development of goat early embryos in vitro. Mol Reprod Dev. 2000;57(1):48–54. doi: 10.1002/1098-2795(200009)57:1<48::AID-MRD7>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 22.Zuelke KA, Jeffay SC, Zucker RM, Perreault SD. Glutathione (GSH) concentrations vary with the cell cycle in maturing hamster oocytes, zygotes, and pre-implantation stage embryos. Mol Reprod Dev. 2003;64(1):106–112. doi: 10.1002/mrd.10214. [DOI] [PubMed] [Google Scholar]
- 23.Luberda Z. The role of glutathione in mammalian gametes. Reprod Biol. 2005;5(1):5–17. [PubMed] [Google Scholar]
- 24.de Matos DG, Furnus CC, Moses DF. Glutathione synthesis during in vitro maturation of bovine oocytes: role of cumulus cells. Biol Reprod. 1997;57(6):1420–1425. doi: 10.1095/biolreprod57.6.1420. [DOI] [PubMed] [Google Scholar]
- 25.Gupta MK, Uhm SJ, Lee HT. Effect of vitrification and beta-mercaptoethanol on reactive oxygen species activity and in vitro development of oocytes vitrified before or after in vitro fertilization. Fertil Steril. 2010;93(8):2602–2607. doi: 10.1016/j.fertnstert.2010.01.043. [DOI] [PubMed] [Google Scholar]
- 26.Curnow EC, Ryan J, Saunders D, Hayes ES. Bovine in vitro oocyte maturation as a model for manipulation of the gamma-glutamyl cycle and intraoocyte glutathione. Reprod Fertil Dev. 2008;20(5):579–588. doi: 10.1071/RD08041. [DOI] [PubMed] [Google Scholar]
- 27.Curnow EC, Ryan JP, Saunders DM, Hayes ES. In vitro developmental potential of macaque oocytes, derived from unstimulated ovaries, following maturation in the presence of glutathione ethyl ester. Hum Reprod. 2010;25(10):2465–2474. doi: 10.1093/humrep/deq225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. 2000;73(6):1155–1158. doi: 10.1016/S0015-0282(00)00518-5. [DOI] [PubMed] [Google Scholar]
- 29.Mature oocyte cryopreservation: a guideline. Fertility and sterility. 2013;99(1):37–43. doi:10.1016/j.fertnstert.2012.09.028. [DOI] [PubMed]
- 30.Larman MG, Sheehan CB, Gardner DK. Calcium-free vitrification reduces cryoprotectant-induced zona pellucida hardening and increases fertilization rates in mouse oocytes. Reproduction. 2006;131(1):53–61. doi: 10.1530/rep.1.00878. [DOI] [PubMed] [Google Scholar]
- 31.Bogliolo L, Ledda S, Innocenzi P, Ariu F, Bebbere D, Rosati I, Leoni GG, Piccinini M. Raman microspectroscopy as a non-invasive tool to assess the vitrification-induced changes of ovine oocyte zona pellucida. Cryobiology. 2012;64(3):267–272. doi: 10.1016/j.cryobiol.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 32.Takeo T, Nakagata N. Reduced glutathione enhances fertility of frozen/thawed C57BL/6 mouse sperm after exposure to methyl-beta-cyclodextrin. Biol Reprod. 2011;85(5):1066–1072. doi: 10.1095/biolreprod.111.092536. [DOI] [PubMed] [Google Scholar]
- 33.Ishizuka Y, Nishimura M, Matsumoto K, Miyashita M, Takeo T, Nakagata N, Hosoi Y, Anzai M. The influence of reduced glutathione in fertilization medium on the fertility of in vitro-matured C57BL/6 mouse oocytes. Theriogenology. 2013;80(5):421–426. doi: 10.1016/j.theriogenology.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 34.Zhao XM, Du WH, Wang D, Hao HS, Liu Y, Qin T, et al. Recovery of mitochondrial function and endogenous antioxidant systems in vitrified bovine oocytes during extended in vitro culture. Mol Reprod Dev. 2011;78(12):942–950. doi: 10.1002/mrd.21389. [DOI] [PubMed] [Google Scholar]
- 35.Ou XH, Li S, Wang ZB, Li M, Quan S, Xing F, Guo L, Chao SB, Chen Z, Liang XW, Hou Y, Schatten H, Sun QY. Maternal insulin resistance causes oxidative stress and mitochondrial dysfunction in mouse oocytes. Hum Reprod. 2012;27(7):2130–2145. doi: 10.1093/humrep/des137. [DOI] [PubMed] [Google Scholar]
- 36.Wu C, Rui R, Dai J, Zhang C, Ju S, Xie B, Lu X, Zheng X. Effects of cryopreservation on the developmental competence, ultrastructure and cytoskeletal structure of porcine oocytes. Mol Reprod Dev. 2006;73(11):1454–1462. doi: 10.1002/mrd.20579. [DOI] [PubMed] [Google Scholar]
- 37.Rojas C, Palomo MJ, Albarracin JL, Mogas T. Vitrification of immature and in vitro matured pig oocytes: study of distribution of chromosomes, microtubules, and actin microfilaments. Cryobiology. 2004;49(3):211–220. doi: 10.1016/j.cryobiol.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 38.Mellon MG, Rebhun LI. Sulfhydryls and the in vitro polymerization of tubulin. J Cell Biol. 1976;70(1):226–238. doi: 10.1083/jcb.70.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tarin JJ, Vendrell FJ, Ten J, Blanes R, van Blerkom J, Cano A. The oxidizing agent tertiary butyl hydroperoxide induces disturbances in spindle organization, c-meiosis, and aneuploidy in mouse oocytes. Mol Hum Reprod. 1996;2(12):895–901. doi: 10.1093/molehr/2.12.895. [DOI] [PubMed] [Google Scholar]
- 40.Tamura AN, Huang TT, Marikawa Y. Impact of vitrification on the meiotic spindle and components of the microtubule-organizing center in mouse mature oocytes. Biol Reprod. 2013;89(5):112. doi: 10.1095/biolreprod.113.108167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zander-Fox D, Cashman KS, Lane M. The presence of 1 mM glycine in vitrification solutions protects oocyte mitochondrial homeostasis and improves blastocyst development. J Assist Reprod Genet. 2013;30(1):107–116. doi: 10.1007/s10815-012-9898-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moawad AR, Xu B, Tan SL, Taketo T. l-Carnitine supplementation during vitrification of mouse germinal vesicle stage-oocytes and their subsequent in vitro maturation improves meiotic spindle configuration and mitochondrial distribution in metaphase II oocytes. Hum Reprod. 2014;29(10):2256–2268. doi: 10.1093/humrep/deu201. [DOI] [PubMed] [Google Scholar]
- 43.Nagai S, Mabuchi T, Hirata S, Shoda T, Kasai T, Yokota S, Shitara H, Yonekawa H, Hoshi K. Correlation of abnormal mitochondrial distribution in mouse oocytes with reduced developmental competence. Tohoku J Exp Med. 2006;210(2):137–144. doi: 10.1620/tjem.210.137. [DOI] [PubMed] [Google Scholar]
- 44.Brevini TA, Vassena R, Francisci C, Gandolfi F. Role of adenosine triphosphate, active mitochondria, and microtubules in the acquisition of developmental competence of parthenogenetically activated pig oocytes. Biol Reprod. 2005;72(5):1218–1223. doi: 10.1095/biolreprod.104.038141. [DOI] [PubMed] [Google Scholar]
- 45.Rho GJ, Kim S, Yoo JG, Balasubramanian S, Lee HJ, Choe SY. Microtubulin configuration and mitochondrial distribution after ultra-rapid cooling of bovine oocytes. Mol Reprod Dev. 2002;63(4):464–470. doi: 10.1002/mrd.10196. [DOI] [PubMed] [Google Scholar]
- 46.Chen C, Han S, Liu W, Wang Y, Huang G. Effect of vitrification on mitochondrial membrane potential in human metaphase II oocytes. J Assist Reprod Genet. 2012;29(10):1045–1050. doi: 10.1007/s10815-012-9848-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jo JW, Lee JR, Jee BC, Suh CS, Kim SH. Exposing mouse oocytes to necrostatin 1 during in vitro maturation improves maturation, survival after vitrification, mitochondrial preservation, and developmental competence. Reprod Sci. 2015;22(5):615–625. doi: 10.1177/1933719114556482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinou JC, Youle RJ. Mitochondria in apoptosis: Bcl-2 family members and mitochondrial dynamics. Dev Cell. 2011;21(1):92–101. doi: 10.1016/j.devcel.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goddard MJ, Pratt HP. Control of events during early cleavage of the mouse embryo: an analysis of the ‘2-cell block’. J Embryol Exp Morpholog. 1983;73:111–133. [PubMed] [Google Scholar]
- 50.Qiu JJ, Zhang WW, Wu ZL, Wang YH, Qian M, Li YP. Delay of ZGA initiation occurred in 2-cell blocked mouse embryos. Cell Res. 2003;13(3):179–185. doi: 10.1038/sj.cr.7290162. [DOI] [PubMed] [Google Scholar]
- 51.Nakano H, Kubo H. Rescue of mouse embryos from 2-cell blocks by microinjection of maturation promoting factor. Fertil Steril. 2001;75(6):1194–1197. doi: 10.1016/S0015-0282(01)01778-2. [DOI] [PubMed] [Google Scholar]
- 52.Chamayou S, Bonaventura G, Alecci C, Tibullo D, Di Raimondo F, Guglielmino A, et al. Consequences of metaphase II oocyte cryopreservation on mRNA content. Cryobiology. 2011;62(2):130–134. doi: 10.1016/j.cryobiol.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 53.Ariu F, Bogliolo L, Leoni G, Falchi L, Bebbere D, Nieddu SM, Zedda MT, Pau S, Ledda S. Effect of caffeine treatment before vitrification on MPF and MAPK activity and spontaneous parthenogenetic activation of in vitro matured ovine oocytes. Cryo Letters. 2014;35(6):530–536. [PubMed] [Google Scholar]
- 54.Grifo JA, Noyes N. Delivery rate using cryopreserved oocytes is comparable to conventional in vitro fertilization using fresh oocytes: potential fertility preservation for female cancer patients. Fertil Steril. 2010;93(2):391–396. doi: 10.1016/j.fertnstert.2009.02.067. [DOI] [PubMed] [Google Scholar]
- 55.Cobo A, Meseguer M, Remohi J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod. 2010;25(9):2239–2246. doi: 10.1093/humrep/deq146. [DOI] [PubMed] [Google Scholar]
- 56.Gartner A, Milstein S, Ahmed S, Hodgkin J, Hengartner MO. A conserved checkpoint pathway mediates DNA damage—induced apoptosis and cell cycle arrest in C. elegans. Mol Cell. 2000;5(3):435–443. doi: 10.1016/S1097-2765(00)80438-4. [DOI] [PubMed] [Google Scholar]
- 57.Nunez-Calonge R, Cortes S, Gutierrez Gonzalez LM, Kireev R, Vara E, Ortega L, et al. Oxidative stress in follicular fluid of young women with low response compared with fertile oocyte donors. Reprod BioMed Online. 2016;32(4):446–456. doi: 10.1016/j.rbmo.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 58.Donabela FC, Meola J, Padovan CC, de Paz CC, Navarro PA. Higher SOD1 gene expression in cumulus cells from infertile women with moderate and severe endometriosis. Reprod Sci. 2015;22(11):1452–1460. doi: 10.1177/1933719115585146. [DOI] [PubMed] [Google Scholar]