Abstract
Background
This systematic review aims to assess the effect of silver diamine fluoride (SDF) in preventing and arresting dental caries in exposed root surfaces of adults (PROSPERO registration: CRD42016036963).
Types of studies reviewed
Two reviewers independently searched for controlled clinical trials with at least 12 months of follow-up, without language or date of publication restraints, in eight electronic databases, five registries of ongoing trials and reference lists of narrative reviews.
Results
2,356 unique records were found and three trials that randomized 895 elders were included. All compared SDF to placebo; one also compared SDF to chlorhexidine (CHX) and sodium fluoride varnishes (FV). The primary effect measures were the pooled mean differences (WMD) in decayed or filled root surfaces (DFRS) and the mean differences in arrested caries lesions between SDF and control groups. The studies had low risk of bias in most domains. SDF applications had a significantly better preventive effect in comparison to placebo, (WMD, DFRS: 24 months: -0.56; 95% CI: -0.77, -0.36 and 30 months or more: -0.80; 95% CI:-1.19, -0.42) and they were as effective as either CHX or FV in preventing new root caries lesions. SDF also provided a significantly higher caries arrest effect in comparison to placebo (pooled results not calculated). Complaints about black staining of the carious lesions by SDF were rare among elders.
Practical implications
Yearly 38% SDF applications to exposed root surfaces of elderly people are a simple, inexpensive and effective way of preventing dental caries initiation and progression.
Keywords: Root caries, Preventive dentistry, Cariostatic agents, Fluoride, Dental care for Aged, Systematic review
Introduction
The cumulative incidence of root caries in people aged 60 years or above ranges from 12% to 77%; relevant risk factors being age, poor oral health and periodontal disease. 1 The widespread occurrence of root caries in elderly people translates into a peak of untreated dental caries in the world adult population at around 70 years of age. 2 Besides placing a huge financial burden on society 2, untreated caries negatively impacts on the elderly's quality of life, especially because of pain experience, which can lead to psychological and physical discomfort, social disability and even handicap. 3
The development of root caries is a result of repeated cycles of de- and remineralization coupled with the degradation of the organic matrix of dentin and cementum; demineralization initiates the caries process, but protein degradation plays a key role on its progression. Thus, topical applications of substances containing protease inhibitors could be an effective means of controlling root caries. 4
Silver diamine fluoride (SDF) is an alkaline topical solution containing fluoride and silver that has been used mainly for dental caries treatment in young children.5 Besides reducing the growth of cariogenic bacteria and promoting remineralisation of the inorganic content of enamel and dentin, silver diamine fluoride (SDF) prevents collagen degradation in dentin by inhibiting the activity of collagenases and cysteine-cathepsins.6 SDF is also known for its ability to desensitize teeth with hypersensitivity. 5
SDF has been used for decades in some countries, such as Australia, Brazil, China and Japan.5 Recently, it was approved in the US as a dentin desensitizing agent but it is also being applied off-label for dental caries treatment.7 The application of SDF is simple, painless, non-invasive and inexpensive 8, 9. Therefore, it may be considered a very attractive approach for the prevention and treatment of dental caries in elderly, especially in those with limited locomotion and impaired self-care ability.
Previous reviews on the effects of SDF in preventing and arresting root caries in adults conducted systematic searches of the evidence, but lacked methodological sophistication 10, 11. They did not follow the most current guidelines for conducting and reporting systematic reviews 12, 13 and only the most recently published one 11 provided some critical appraisal of the design and reporting of the included studies. More importantly, meta-analyses were not conducted; i.e. the results of individual studies were not statistically combined to provide a more precise estimate of the degree to which SDF prevents new root caries lesions from occurring or arrests the progression of existing lesions. Moreover, reviews of head-to-head comparisons between SDF and other interventions (e.g., fluoride or chlorhexidine varnishes) have not been published.
The objective of this systematic review is to perform a qualitative and quantitative synthesis of the scientific evidence on the effect of SDF for preventing and arresting dental caries on exposed root surfaces of adults.
Subjects and Methods
This is a systematic review of randomized controlled clinical trials. It was registered at PROSPERO (CRD42016036963) and is reported according to the recommendations of the PRISMA statement 13. To be eligible for inclusion in the present review studies needed to meet the following criteria:
- Participants: adults of any age with exposed root surfaces at the beginning of the study;
- Intervention: topical SDF solution (any concentration or frequency) applied by any health care worker at any setting;
- Comparisons: no intervention, placebo, and any cariostatic agent or dental restorative material;
- Outcomes: primary outcomes were the development of new dental caries lesions and the arrest of existing carious lesions in exposed root surfaces of permanent teeth within at least 12 months after product application (e.g., 12, 24 or 30 months of follow-up or more). The secondary outcome measures were any self/ caregiver-reported or professionally diagnosed adverse events.
A highly sensitive search strategy was developed for MEDLINE and later adapted for other databases and online repositories of trials with the help of a librarian (Appendix). The databases - Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, MEDLINE via PubMed, SCOPUS, Web of Science, LILACS, BBO, SciELO - were searched on April 2016 without language or date of publication restrictions. Five registries of ongoing trials (i.e., ClinicalTrials.gov, Brazilian Register of Clinical Trials, EU Clinical Trials Register, ISRCTN registry and Current Controlled Trials and Australian New Zealand Clinical Trials Register) and the Brazilian database of thesis and dissertations were also searched. All searches were updated on July 2017. Cross-referencing from narrative reviews on the subject of SDF for caries prevention or arrest was used to identify additional articles.
The records downloaded from each database were organized into one core database using EndNote X7 (Thomson Reuters, San Francisco, USA). After training, two review authors independently examined the title and abstracts of all records that remained after removal of duplicates and decided which articles should be read in full. When a study apparently met the inclusion criteria but no abstract was available or there was not enough information in the title or abstract, the article was obtained and read. Studies in Japanese and Chinese were examined regarding inclusion with the help of individuals knowledgeable in those languages.
An extraction data form was prepared and pilot tested. Two review authors independently read all the studies selected for inclusion and extracted the data. They also independently assessed the risk of bias for all included trials by using the Cochrane risk of bias tool. 12 Disagreements between the reviewers over the inclusion of studies and the risk of bias in particular studies were resolved with the involvement of a third researcher. Study authors were contacted to obtain missing or unclear information.
For caries prevention, the primary outcome measure of treatment effect was the difference in mean caries increment (i.e., follow-up mean number of decayed or filled root surfaces minus baseline mean number of decayed or filled root surfaces - DFRS) between the SDF and control groups (i.e., water, tonic water or another active treatment). We also calculated prevented fractions (PF; mean caries increment in control minus mean caries increment in intervention groups divided by mean caries increment in control) for the comparison between SDF and placebo. Confidence intervals of PFs were estimated by using Fieller's method. 14
For caries arrest, the primary outcome measure of treatment effect was the difference in mean number of arrested lesions (i.e., mean number of active root lesions at baseline that became arrested at follow-up) between the SDF and control groups (i.e., water, tonic water or another active treatment).
Since the estimate of between-studies variance under the random-effects model has poor precision when the number of studies is very small 15, we used the fixed-effect model to obtain pooled estimates of caries increment as weighted mean differences (WMD) or PF when combining the studies. Heterogeneity of studies was assessed by the Chi-square (χ2) test for heterogeneity and Higgins index (I2). The studies in our meta-analyses were grouped according to the duration of their follow-up in: 12 months, 24 months and 30 months or more. The difference in caries increments regarding the comparisons between SDF and other active treatments (i.e., chlorhexidine varnish (CHX) and sodium fluoride varnish (FV)) could not be pooled because there was only one study for each comparison. When there was more than one SDF intervention group per study 16, 17 they were combined into a single group. All analyses were carried out in Stata® 14 (StataCorp LP, College Station, USA) and followed the procedures described in the Cochrane Handbook for Systematic Reviews of Interventions. 12
Results
The searches yielded 2,356 unique records; 22 publications were assessed for eligibility. Eventually, we included four reports from three trials 16-19 that randomized 895 elderly people and analysed 544, 712 and 460 subjects at 12, 24 and 30 or more months of follow-up, respectively. (Figure 1 and Table 1) These subjects had similar mean age (i.e., from 72.1 years to 78.8 years), low caries experience (i.e., mean baseline decayed and filled root surfaces ranged from 1.1 to 2.1) and consumed fluoridated water (0.5 ppm). In all studies both the test and control groups received individualized oral hygiene instruction (OHI). All included trials were conducted in Hong Kong, used SDF at a 38% concentration and compared it to a placebo (i.e., water 17, 18 or tonic water 16). Two trials had two intervention groups: one 17 compared yearly SDF applications with or without participation on a biannually oral health education program (OHE) to a placebo; another 16 compared yearly SDF applications followed or not by a potassium iodide (KI) application to a placebo. One trial 18 also compared yearly SDF applications to quarterly applications of 1% chlorhexidine varnish (CHX) and 5% sodium fluoride varnish (FV). (Table 1) Three studies 16-18 provided data on caries prevention and two studies provided data on caries arrest 17, 19. Active root caries was recorded when a shape sickle-shaped probe 18 or a Community Periodontal Index (CPI) probe 17, 19 could easily penetrate a lesion when applied with a light force. Inactive caries was recorded when no soft dentine was detected 17, 19 and root surface was smooth and dark brown or black in colour. 17
Figure 1.
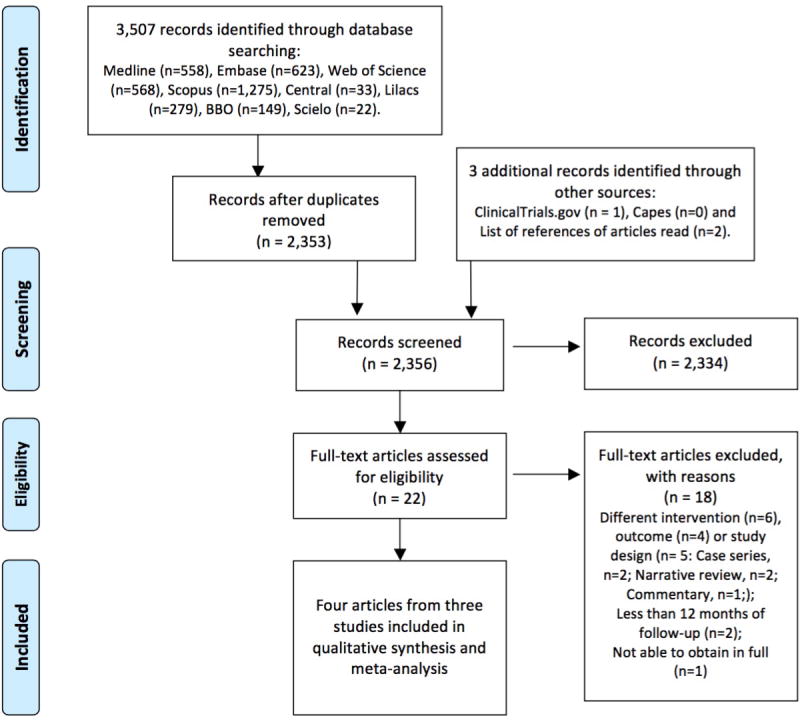
Flow diagram showing the process of identifying, screening, assessing for eligibility, excluding and including studies.
Table 1. Characteristics of the included studies.
| Study, Country | Total duration of follow-up in months | Number of participants randomized (Ni) and analysed regarding caries incidence (Nf) | Mean age of participants in years (SD) and caries experience at baseline (DFRS) | Intervention | Comparison |
|---|---|---|---|---|---|
| China Li 2017, China | 30 | Ni=323 Nf= 297 (12 mos), 258 (24 mos) and 257 (30 mos) |
Mean age=72.1 (6.3) DFRS= 1.1 |
OHI+38% SDF applications or OHI+38% SDF applications + KI applications, every 12 months, onto all exposed root surfaces | OHI+tonic water applications, every 12 months, onto all exposed root surfaces |
| Tan 2010, China | 36 | Ni=306 Nf= 247 (12 mos), 227 (24 mos) and 203 (36 mos) |
Mean age=78.8 (6.2) DFRS= 2.1 |
OHI+38% SDF applications (every 12 months) or OHI+ CHXV (every 3 months) or OHI+FV (every 3 months), onto all exposed root surfaces | OHI+water applications, every 12 months, onto all exposed root surfaces |
| Zhang 2013, China | 24 | Ni=266 Nf= 227 |
Mean age: 72.5 (5.7) DFRS= 1.9 |
OHI+38% SDF applications (every 12 months) or OHI+38% SDF applications (every 12 months)+OHE (every 6 months), onto all exposed root surfaces | OHI+water applications, every 12 months, onto all exposed root surfaces |
SD= standard deviation, DFRS =mean number of decayed or filled root surfaces, OHI= individualized oral hygiene instruction, OHE= oral health education programme, SDF= silver diamine fluoride, KI= potassium iodide, CHXV= chlorhexidine varnish, FV= sodium fluoride varnish
The three trials were soundly designed, conducted and reported. One 17 had all domains, except for allocation concealment, with low risk of bias. The other two trials 16, 18 had six domains with low risk and two domains with unclear risk of bias. (Figure 2)
Figure 2.
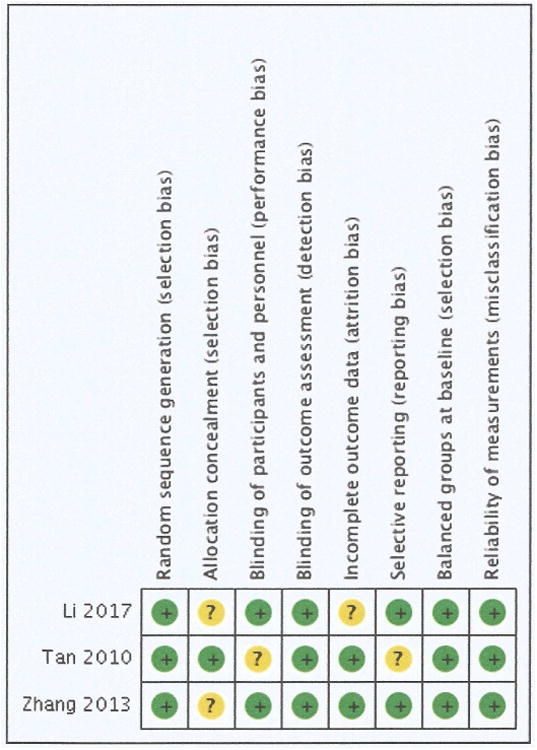
Ascertainment of the risk of bias in the included studies (+ Low risk, - High risk,? Unclear risk).
Caries Prevention
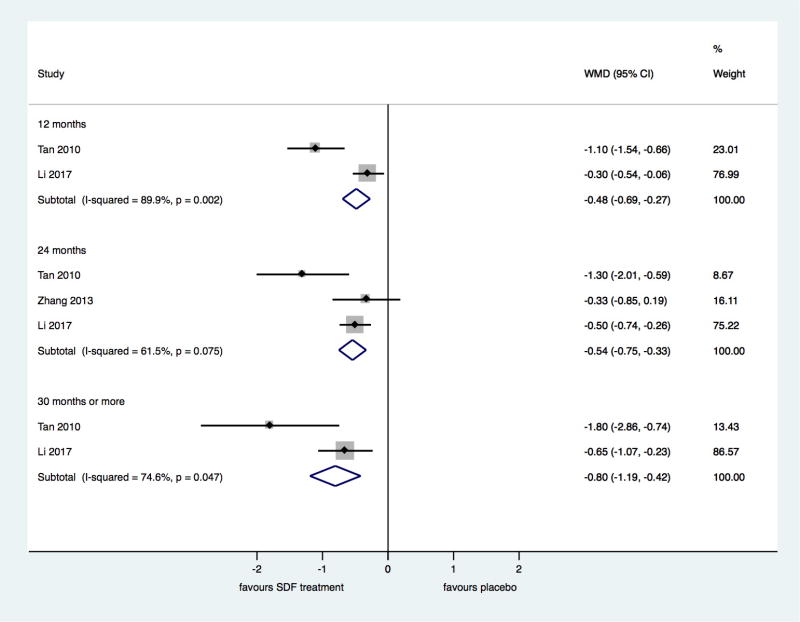
The meta-analysis of three studies with 24 months of follow-up comparing SDF to placebo showed that SDF applications significantly decrease the number of new root caries lesions (WMD DFRS: -0.56; 95% CI: -0.77, -0.36). (Figure 3) The prevented fraction (PF) for root caries prevention ranged from 50.30% to 68.35% depending on duration of follow-up. (Figure 4) When SDF was compared to SDF followed by KI no significant difference was observed in caries increment after 30 months of follow-up. 16 Since in Zhang study 17 only the test group that received a co-intervention (OHE) had a significantly lower new caries increment in comparison to the placebo group, we performed a sensitivity analysis excluding this group from the comparison between SDF and placebo. The pooled WMD and PF changed from -0.56 to -0.54 (95% CI -0.75, -0.33) and from 50.30% to 52.05% (95% CI 38.55, 65.55), respectively.
Figure 3.
Comparisons of the mean increment in the number of decayed or filled root surfaces (DFRS) of permanent teeth, in silver diamine fluoride and placebo groups, by duration of follow-up (12 months, 24 months or 30 months or more).
Figure 4.
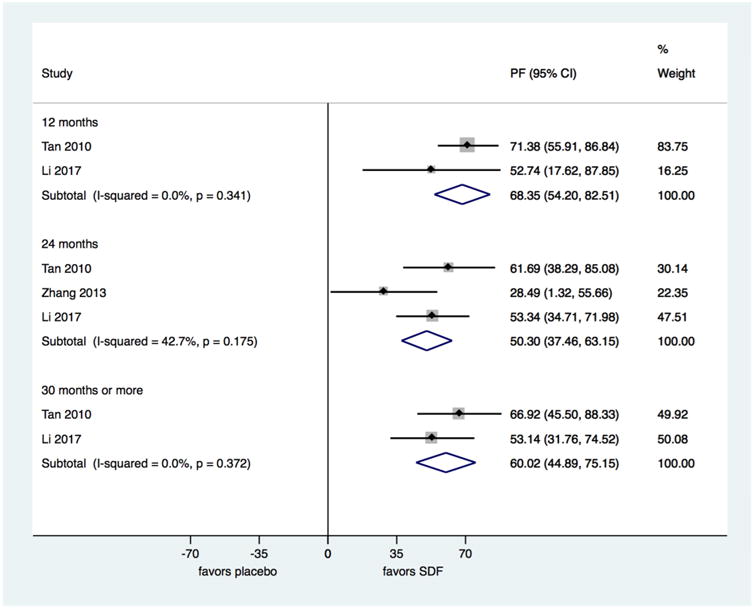
Comparisons of the prevented fractions in root surfaces of permanent teeth, in silver diamine fluoride and placebo groups, by duration of follow-up (12 months, 24 months or 30 months or more).
The comparisons between SDF and FV or CHX varnish were based on one study. 18 CHX had a significantly higher preventive effect than SDF at 12 months of follow-up but there were no significant differences between SDF and FV at any of the follow-up periods analysed (i.e., 12, 24 or 36 months) or between SDF and CHX varnish at 24 months of follow-up or more. (Figure 5)
Figure 5.
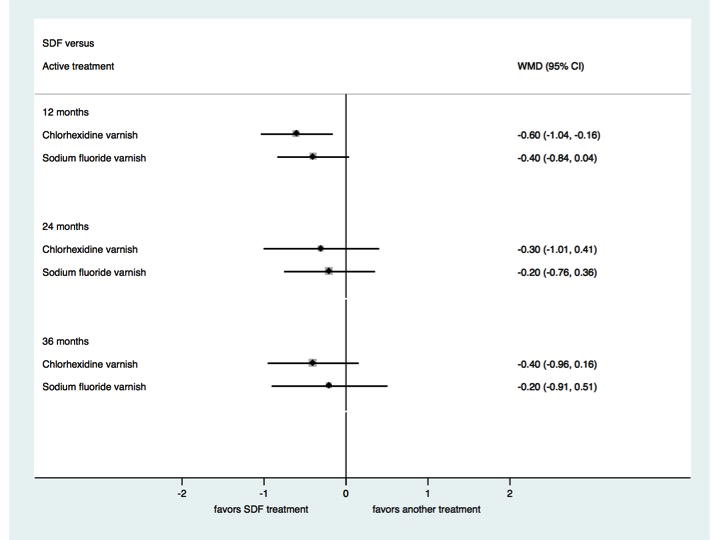
Comparisons of the mean increment in the number of decayed or filled root surfaces (DFRS) of permanent teeth, in silver diamine fluoride and active treatment groups, by duration of follow-up (12 months, 24 months or 30 months or more).
Caries arrest
Significantly higher mean numbers of arrested lesions were observed in the test groups than in the placebo group after 24 months of follow-up in one study 17. In the other study 16 results were provided as percentage of caries arrest and the test groups presented significantly higher percentages of caries lesions arrested than the placebo group at 12, 24 and 30 months of follow-up. In this study 323 subjects were randomized to the test and control groups but only 83 were included and 67 analysed in the authors' reporting on caries arrest. (Table 2)
Table 2. Results of the individual studies regarding caries arrest by duration of follow-up.
| Study, Year Outcome | Number of participants at baseline (Ni) and number of participants analysed (Nf) by duration of follow-up | Results
|
|
|---|---|---|---|
| Intervention Group | Comparison Group | ||
| Zhang, 2013 | Ni=266 | ||
| Mean number of arrested root caries surfaces (SD) | 24 months Nf =227 |
OHI + SDF (n=83) = 0.28 (0.02) OHI + SDF + OHE (n=69) = 0.33 (0.10) |
OHI + water (n=75) = 0.04 (0.02) |
| Li, 2017 Percentage of arrested root caries surfaces |
Ni=323 (randomized) and 83 with active root caries lesions | ||
| 12 months (Nf =75) |
OHI + SDF (n=27) = 61.0% OHI + SDF + KI (n=29) = 75.9% |
OHI + tonic water (n=19) = 32.1% | |
| 24 months (Nf =65) |
OHI + SDF (n=26) = 82.1% OHI + SDF + KI (n=23) = 85.4% |
OHI + tonic water (n=16) = 28.6% | |
| 30 months (Nf =67) |
OHI + SDF (n=27) = 90.0% OHI + SDF + KI (n=24) = 92.5% |
OHI + tonic water (n=16) = 45.0% | |
SD=standard deviation, SDF= silver diamine fluoride, OHI= individualized oral hygiene instruction, OHE= oral health education programme, KI= potassium iodide.
Two studies 16, 18 reported that the interventions were well accepted by the elders. In one trial, 3.5% of all participants complained about the black staining of their treated root surfaces.16 In another, only two elders, both in the SDF group, raised the same complaint (additional information provided by one of the authors). 18
Discussion
Our findings show that annual applications of 38% SDF in elderly people decrease the incidence of new caries lesions in exposed root surfaces by at least 50%; the longer the duration of the intervention, the greater the effect. Limited evidence with low risk of bias indicates that SDF is significantly more effective in preventing the development of new carious lesions when compared to placebo and similar or better than FV and CHX varnishes.
In our meta-analyses for caries prevention, two SDF test groups were combined into one SDF group in two of the included trials. One of them 17 tested whether the benefits of SDF applications would be increased by participation in a bi-annual OHE programme conducted by trained dental hygienists that emphasized the prevention of snacking habits, correct toothbrushing practices and adoption of additional tooth cleaning aids. This programme was costly and time-consuming but only the SDF plus OHE group had a significantly lower new caries increment in comparison to the placebo group. Considering that toothbrushing behavior improvement did not significantly differ between the SDF only and SDF plus OHE groups and that sugar snacking plays a major role in caries development, it is likely that an unmeasured modification of the participants' dietary habits might have contributed to the lower caries incidence in the SDF plus OHE group. However, a sensitivity analysis excluding the SDF plus OHE group from the comparison between SDF and placebo showed that the impact of this co-intervention on the pooled effect was only negligible. The other trial compared the use of SDF alone with the use of SDF plus KI solution 16, 19. The KI application immediately after the SDF application did not interfere with SDF's effectiveness in preventing 16 root caries.
Despite reaching a conclusion similar to that of a previous meta-analysis that combined the results of two trials with different follow-up periods 20 regarding the efficacy of SDF for root caries prevention, we obtained a more conservative estimate of effect. Since our meta-analysis pooled the results of three trials, our estimate of effect is probably more precise. Moreover, because we grouped the studies in our meta-analyses according to the duration of their follow-up, we were able to show that the preventive effect of SDF in root surfaces seems to increase with increasing duration of therapy. This has not been shown before and needs to be more thoroughly investigated.
When comparing SDF with other active treatments for root caries prevention, evidence from only one study indicated no difference between the yearly SDF and quarterly FV or CHX varnish applications, except for the comparison between SDF and CHX varnish at 12 months of follow-up, which favored CHX. A recent meta-analysis 20 has estimated a reduction of 0.67 mean DFRS in subjects treated with CHX varnish in comparison to placebo. Taken together, these findings suggest that SDF and CHX varnish may have a similar effect on the prevention of root caries. Nevertheless, an analysis of cost-effectiveness in the context of the German health care system showed that quarterly applications of CHX varnish were not cost-effective whereas SDF was more cost-effective than no treatment, specially in populations with high caries risk.21 The lack of difference between the root caries preventive effect of SDF and FV contrasts with what has been observed in primary teeth, where yearly 38% SDF applications performed significantly better than quarterly 5% sodium FV applications. 22 Clearly, more well-designed clinical trials comparing different frequency and interval between applications of SDF, CHX and F varnishes and other cariostatic agents are needed.
The assessment of the effect size of SDF on the arrest of root caries was hindered by the difference in outcome measures used in the studies and results could not be pooled. However, there is good quality evidence accrued from one trial 17 that annually 38% SDF applications effectively arrest root caries. Moreover, KI application immediately after SDF or participation on a bi-annual OHE programme together with yearly SDF applications do not seem to interfere with SDF's caries arresting effect.19
Esthetics of the arrested lesions was not a concern among the elderly that participated in the studies included in our review. However, adults of different cultural backgrounds or presenting a higher number of root caries surfaces or lesions in front teeth may consider the darkening effect of SDF unacceptable.23 One trial tested whether the use of a KI solution immediately after SDF application would reduce the black staining produced by silver ions present in SDF. Interestingly, the study failed to show a significant reduction of the black staining with the use of the KI solution. 16, 19 Thus, there is still a need to investigate whether this change in color in SDF treated caries lesions can be minimized.
The results of this systematic review are limited by the low number of clinical trials addressing our research question and the lack of information from the included trials on the potential side effects of the intervention other than the darkening of caries lesions. In addition, all the included trials were from the same group of investigators and enrolled Chinese elders with low risk of dental caries. The extent to which the findings can be generalized to other populations (e.g., elders with higher caries risk, not exposed to fluoridated water, not submitted to individual oral hygiene instruction regularly or having different dietary habits) and reproduced by other investigators needs to be investigated further. Additionally, moderate to considerable statistical heterogeneity was encountered when WMD were pooled. This is hard to explain since relevant clinical and methodological variations among the studies are not apparent and there are not enough studies to allow a reliable statistical investigation of the reasons for heterogeneity. The change of the effect measure has been suggested as an alternative to deal with heterogeneity. 12 When pooled PF were estimated no heterogeneity was observed and results were consistent with those obtained through meta-analyses of WMD confirming the effectiveness of SDF for the prevention of root caries.
In conclusion, yearly 38% SDF applications to exposed root surfaces of elderly people are effective against dental caries initiation and progression. The preventive effect of SDF for root caries is similar to that of 5% sodium fluoride and 1% chlorhexidine varnishes. Further research is needed to replicate these findings and to determine the best frequency and interval of SDF applications. Given the potential of SDF for both prevention and arrest of dental caries, its low cost and simplicity of application, future studies in elderly populations should consider the impact of SDF on satisfaction with dental care, quality of life and the cost benefit of using SDF in lieu of more complex treatments at this stage of life.
Practical Implications.
Besides placing a huge financial burden on society, untreated root caries negatively impacts on the elderly's quality of life, especially because of pain experience, which can lead to psychological and physical discomfort, social disability and even handicap. The application of silver diamine fluoride (SDF) is simple, painless, non-invasive and inexpensive. Therefore, it may be considered a very attractive approach for the prevention and treatment of dental caries in elderly, especially in those with limited locomotion and impaired self-care ability. Knowing that it works for both caries prevention and arrest and is well accepted by patients may be of great interest to clinicians.
Acknowledgments
We thank Mr. Richard McGowan, MLS, Research Librarian at New York University College of Dentistry, for his help with searching the literature and Ms. Xiaoxi Gu and Dr. Mikako Deguchi, MBA, for their help with translating into English the articles written in Chinese and Japanese, respectively. We also thank Dr. Edward Lo, PhD, who provided additional information about Tan and Colleagues, 2010 trial.
Research reported in this publication was partially supported by the National Institute On Minority Health and Health Disparities of the National Institutes of Health under Award Numbers R01MD011526 and U24MD006964, and partially funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (PCS-1609-36824). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee. The Teacher Training Program of the University of the State of Rio de Janeiro (Programa de Capacitação Docente da Universidade do Estado do Rio de Janeiro) also supported this work. The authors declare no potential conflicts of interest with respect to the authorship or publication of this article.
Footnotes
Disclosure. None of the authors reported any disclosures.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lopez R, Smith PC, Gostemeyer G, Schwendicke F. Ageing, dental caries and periodontal diseases. J Clin Periodontol. 2017;44(Suppl 18):S145–s52. doi: 10.1111/jcpe.12683. [DOI] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Bernabe E, Dahiya M, et al. Global Burden of Untreated Caries: A Systematic Review and Metaregression. J Dent Res. 2015;94(5):650–8. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 3.Masood M, Newton T, Bakri NN, Khalid T, Masood Y. The relationship between oral health and oral health related quality of life among elderly people in United Kingdom. J Dent. 2017;56(1):78–83. doi: 10.1016/j.jdent.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi N, Nyvad B. Ecological Hypothesis of Dentin and Root Caries. Caries Res. 2016;50(4):422–31. doi: 10.1159/000447309. [DOI] [PubMed] [Google Scholar]
- 5.Mei ML, Chin-Man Lo E, Chu CH. Clinical Use of Silver Diamine Fluoride in Dental Treatment. Compend Contin Educ Dent. 2016;37(2):93–98. [PubMed] [Google Scholar]
- 6.Zhao IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2017 doi: 10.1111/idj.12320. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horst JA, Ellenikiotis H, Milgrom PL. UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale, Indications and Consent. J Calif Dent Assoc. 2016;44(1):16–28. [PMC free article] [PubMed] [Google Scholar]
- 8.Crystal Y, Niederman R. Silver Diamine Fluoride Treatment Considerations in Children's Caries Management. Pediatr Dent. 2016;38(7):466–71. [PMC free article] [PubMed] [Google Scholar]
- 9.Chhokar SK, Laughter L, Rowe DJ. Perceptions of Registered Dental Hygienists in Alternative Practice Regarding Silver Diamine Fluoride. J Dent Hyg. 2017;91(4):53–60. [PubMed] [Google Scholar]
- 10.Gluzman R, K RV, Frey BJ, McGowan R. Prevention of root caries: a literature review of primary and secondary preventive agents. Spec Care Dentist. 2013;33(3):133–40. doi: 10.1111/j.1754-4505.2012.00318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hendre AD, Taylor GW, Chavez EM, Hyde S. A systematic review of silver diamine fluoride: Effectiveness and application in older adults. Gerodontology. 2017;34(4):411–19. doi: 10.1111/ger.12294. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J, Green S. Version 5.10. London: John Wiley & Sons; 2011. Cochrane Handbook for Systematic Reviews of Interventions. [updated March 2011] ed. [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abrams AM, McClendon BJ, Horowitz HS. Confidence intervals for percentage reductions. J Dent Res. 1972;51(2):492–7. doi: 10.1177/00220345720510024101. [DOI] [PubMed] [Google Scholar]
- 15.Borenstein M, Hedges L, Higgins J, Rothstein HR. Introduction to Meta-Analysis. New York: John Wiley & Sons; 2009. [Google Scholar]
- 16.Li R, Lo ECM, Liu BY, Wong MCM, Chu CH. Randomized Clinical Trial on Preventing Root Caries among Community-Dwelling Elders. JDR Clinical & Translational Research. 2017;2(1):66–72. doi: 10.1177/2380084416668491. [DOI] [PubMed] [Google Scholar]
- 17.Zhang W, McGrath C, Lo EC, Li JY. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47(4):284–90. doi: 10.1159/000346620. [DOI] [PubMed] [Google Scholar]
- 18.Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89(10):1086–90. doi: 10.1177/0022034510375825. [DOI] [PubMed] [Google Scholar]
- 19.Li R, Lo EC, Liu BY, Wong MC, Chu CH. Randomized clinical trial on arresting dental root caries through silver diammine fluoride applications in community-dwelling elders. J Dent. 2016;51(8):15–20. doi: 10.1016/j.jdent.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Wierichs RJ, ML H. Systematic review on noninvasive treatment of root caries lesions. J Dent Res. 2015;94(2):261–71. doi: 10.1177/0022034514557330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwendicke F, Göstemeyer G. Cost-effectiveness of root caries preventive treatments. J Dent. 2017;56(1):58–64. doi: 10.1016/j.jdent.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81(11):767–70. doi: 10.1177/0810767. [DOI] [PubMed] [Google Scholar]
- 23.Crystal YO, Janal MN, Hamilton DS, Niederman R. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc. 2017;148(7):510–18.e4. doi: 10.1016/j.adaj.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]