Abstract
Background
Sumo wrestling is a demanding sport. Although watching sumo wrestling may have cardiovascular effects, no studies of this relationship have been performed. Thus, we aimed to evaluate the association between sumo wrestling tournaments and the rate of out‐of‐hospital cardiac arrests.
Methods and Results
We counted the daily number of patients aged 18 to 110 years who had an out‐of‐hospital cardiac arrest of presumed‐cardiac origin in the Tokyo metropolis between 2005 and 2014. A Poisson regression was used to model out‐of‐hospital cardiac arrests of presumed‐cardiac origin per day. Exposure days were the days on which a sumo tournament was held and broadcast, whereas control days were all other days. Events that occurred on exposure days were compared with those that occurred on control days. Risk ratios for out‐of‐hospital cardiac arrests on Grand Sumo tournaments days compared with control days were estimated. In total, 71 882 out‐of‐hospital cardiac arrests met the inclusion criteria. We recorded a 9% increase in the occurrence of out‐of‐hospital cardiac arrests on the day of a sumo tournament compared with control days. In patients aged 75 to 110 years, we found a 13% increase in the occurrence of out‐of‐hospital cardiac arrests on the day of a sumo tournament compared with control days.
Conclusions
We found a significant increase in the occurrence of out‐of‐hospital cardiac arrests on the days of sumo tournaments compared with control days in the Tokyo metropolis between 2005 and 2014. Further studies are needed to verify these initial findings on sumo tournaments and cardiovascular events.
Keywords: cardiac arrest, Japan, sudden cardiac arrest, sumo tournament, sporting events
Subject Categories: Epidemiology
Clinical Perspective
What Is New?
We found a significant increase in the occurrence of out‐of‐hospital cardiac arrests on the days of sumo tournaments compared with control days in the Tokyo metropolitan area between 2005 and 2014.
What Are the Clinical Implications?
Additional studies are warranted to verify the relationship between sumo tournaments and cardiovascular events, with an eye towards mitigating the risk in vulnerable populations if proven true.
Introduction
The role of triggering factors in cardiovascular health has been evaluated in several previous studies. Sports events, earthquakes, and war can all induce environmental stress in a large number of people in defined areas.1 Objective evidence of triggering comes from earthquakes in Northridge in Southern California in 1994,2 in Hanshin‐Awaji in Japan in 1995,3 and in Great East Japan in 2011.4 Similar results have also been obtained for military conflicts.5, 6 Although the psychological upheaval caused by earthquakes and wars cannot be equated with the stress caused by sporting events, it is likely that sporting events increase the risk of cardiovascular events. Several studies have found that soccer matches are related to increased cardiac emergencies and myocardial infarction.7, 8 Conversely, mortality from myocardial infarction decreased in France after a World Cup final in 1998.9 In Italy, international soccer matches were not associated with rates of admissions for acute myocardial infarction.10 It is pointed out that the cardiovascular effects of watching soccer matches are likely to be small if they exist at all.10
Sumo is the national sport in Japan. It is a kind of martial art in where 2 sumo wrestlers, or rikishi, fight in a ring, or dohyo. Watching sumo is popular among elderly people.11 Acute mental stress increases the risk of a variety of cardiovascular events.7, 8, 12 Since sumo is fierce struggle which causes increased emotions in spectators, it is possible that watching sumo matches increases the risk of cardiovascular events, particularly among elderly people. To date, no studies have been undertaken to determine the relationship between sumo tournaments and cardiovascular events in Japan. Thus, we evaluated the association between sumo tournaments and rates of out‐of‐hospital cardiac arrests of presumed‐cardiac origin in the Tokyo metropolis between 2005 and 2014.
Methods
The authors declare that all supporting data are available within the article.
Sumo Tournaments
The Grand Sumo tournament runs for 15 days, from the second to fourth Sundays of odd‐numbered months. Thus, Grand Sumo tournaments are held 6 times a year. Three tournaments are held in Tokyo in January, May, and September, and another 3 tournaments are held in Osaka in March, Nagoya in July, and Fukuoka in November. The sumo wrestler with the highest winning percentage wins the championship. If there are multiple sumo wrestlers with the highest winning percentage on the 15th day, an additional championship match is held. Every sumo match of senior‐grade sumo wrestlers is broadcast on NHK (Japan Broadcasting Corporation) television.13 Exposure days were days on which a sumo match was held and broadcast, whereas control days were all other days. In the study setting, 3 sumo tournaments (in July 2010, March 2011, and May 2011) were suspended or not broadcast because of sumo wrestlers betting on professional baseball games or fixing the match. In total, there were 855 exposure and 2797 control days.
Study Settings and Data
The study site was the Tokyo metropolis, and the study ran from January 1, 2005, to December 31, 2014. As of January 1, 2014, the total population of the Tokyo metropolis was 13 294 039 in an area of 2190.75 km2. Emergency medical services are provided by about 80 fire stations and dispatch centers run by the Tokyo metropolitan government. Japanese guidelines do not allow emergency medical service personnel to terminate resuscitation in the field, except in cases of obvious death. Thus, all patients with out‐of‐hospital cardiac arrests who are treated by emergency medical services personnel are transported to medical institutions.14 The Fire and Disaster Management Agency maintains a prospective, nationwide population‐based registry of all out‐of‐hospital cardiac arrest cases in Japan using a standardized Utstein‐style template.14, 15, 16 We collected the following data from the national Utstein registry: date of the occurrence of out‐of‐hospital cardiac arrest, time of the emergency call, origin of the cardiac arrest, and patient age and sex. We also gathered data on weather factors in Tokyo metropolis from January 1, 2005, to December 31, 2014 (ie, daily mean ambient temperature and barometric pressure) from the Japan Meteorological Agency.17 We obtained data on the television (TV) ratings of sumo tournaments run between 2012 and 2014 in the Tokyo area from Video Research Ltd.
This study was approved by the ethics committee at Kyushu University Graduate School of Medicine. The committee waived the requirement for written informed consent.
Statistical Analysis
We calculated the daily number of patients aged 18 to 110 years who had an out‐of‐hospital cardiac arrest of presumed‐cardiac origin in the Tokyo metropolis from January 1, 2005 to December 31, 2014. We compared events that occurred on exposure days with those that occurred on control days. We used Poisson regression with a log link to model out‐of‐hospital cardiac arrests of presumed‐cardiac origin per day. According to International Organization for Standardization 8601, a day was defined as a 24‐hour period beginning at noon. To control for seasonality and long‐term trends, we included categorical variables for the day of the week and year, and the time elapsed since the start of the study in the model.18 To allow for auto‐correlations, an auto‐regressive term at order one was incorporated into the models.19 We also controlled the daily mean temperature and barometric pressure in the model and checked the linearity of these weather factors using quadratic and smooth functions.20 We used indicator variables and calculated risk ratios for the 855 sumo match days compared with the 2797 control days. Then we calculated risk ratios for subgroups according to sex and age of patients based on the assumption of asymptotic normality of parameter estimates and independence of events between subgroups. A scatter plot of deviance residuals against predicted values and fitted Poisson regression analyses involving an additional overdispersion scaling parameter supported the adequacy of our model.
We also calculated risk ratios for the 855 sumo match days compared with 2797 control days by the hour of the day. Most sumo stables (gyms) are in the Tokyo area, and half of the tournaments are held in Tokyo. The magnitude of the increase in out‐of‐hospital cardiac arrest was supposed to be larger when sumo tournaments were held in Tokyo than in other cities. Thus, we compared television (TV) sumo tournaments program ratings between 17:00 and 18:00 hours in the Tokyo area from 2012 to 2014 when sumo tournaments were held in Tokyo or other cities. Sumo matches featuring high‐ranking sumo wrestlers who were popular and potential championship contenders, and summaries of the matches were broadcast from 17:30 to 21:59 hours. It is probable that patient age, times, and sumo venue (cities) might relate to the event. Previous studies have shown that the effects of triggers on cardiac arrest do not last longer.21, 22 Thus, to determine whether the effects of patient age on the occurrence of out‐of‐hospital cardiac arrests are modified by hours when sumo matches and summaries are broadcast (ie, 17:30–21:59), we assessed the effect modifications of these 2 factors on additive (eg, relative excess risk due to interaction23, 24) and multiplicative scales (eg, ratio of odds ratios [ORs]23) by sumo venue. The significance level for all tests was P<0.05 (2‐sided). All statistical analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC).
Results
In the study setting, there were 71 882 out‐of‐hospital cardiac arrests that met the inclusion criteria in the Tokyo metropolis. Of the 71 882 cases of out‐of‐hospital cardiac arrest, 17 200 cases occurred on the 855 sumo tournament days, and 54 682 cases occurred on the 2797 control days. Table 1 shows the demographics of patients with events on control days, exposure days, and then exposure days broken down by Tokyo versus other cities. The number of cases in the 75 to 110 year‐old group, especially in the female subgroup, was larger. Table 2 shows the risk ratios for out‐of‐hospital cardiac arrest on the sumo tournament days compared with control days. After we adjusted for covariates, the risk ratio for out‐of‐hospital cardiac arrest on sumo match days was 1.09 (95% confidence interval [CI] [1.04–1.16]) times the risk on control days. Analysis of subgroups by sex indicated that compared with the control days, the number of out‐of‐hospital cardiac arrests increased for both males (risk ratio=1.09, 95% CI [1.03–1.20]) and females (risk ratio=1.11, 95% CI [1.03–1.20]) on sumo match days. Analysis of subgroups by age showed a significant increase in the number of events on days of sumo matches for people aged 75 to 110 years (risk ratio=1.13, 95% CI [1.06–1.21]) but no increases for other age groups.
Table 1.
The Demographics of Patients With Events on Control Days, Exposure Days, and Then Exposure Days Broken Down by Tokyo Versus Other Cities
| Control Days (n=54 682) | Exposure Days (n=17 200) | Exposure Days (n=17 200) | ||||||
|---|---|---|---|---|---|---|---|---|
| Tokyo (n=8736) | Other (n=8464) | |||||||
| Male | Female | Male | Female | Male | Female | Male | Female | |
| 18 to 64 y, n (%) | 9087 (16.62) | 2744 (5.02) | 2795 (16.25) | 847 (4.92) | 1421 (16.27) | 403 (4.61) | 1374 (16.23) | 444 (5.24) |
| 65 to 74 y, n (%) | 7354 (13.45) | 3237 (5.92) | 2290 (13.31) | 1009 (5.87) | 1210 (13.85) | 476 (5.45) | 1080 (12.76) | 533 (6.30) |
| 75 to 110 y, n (%) | 15 597 (28.52) | 16 663 (30.47) | 4974 (28.92) | 5285 (30.73) | 2551 (29.20) | 2675 (30.62) | 2423 (28.63) | 2610 (30.34) |
Table 2.
Risk Ratios for Out‐of‐Hospital Cardiac Arrests on Grand Sumo Tournaments Days Compared With Control Days in the Overall and Subgroups
| Group | Total No. of Events | Event on 855 Tournament Days (n=17 200) | Event on 2797 Control Days (n=54 682) |
|---|---|---|---|
| Overall | 71 882 | ||
| No. of events per day | 20.1 | 19.6 | |
| Risk ratio (95% CI) | 1.09 (1.04–1.16) | 1 | |
| P value | 0.001 | ||
| Males | 42 132 | ||
| No. of events per day | 11.8 | 11.5 | |
| Risk ratio (95% CI) | 1.09 (1.02–1.17) | 1 | |
| P value | 0.011 | ||
| Females | 29 750 | ||
| No. of events per day | 8.4 | 8.1 | |
| Risk ratio (95% CI) | 1.11 (1.03–1.20) | 1 | |
| P value | 0.008 | ||
| 18 to 64 years of age | 15 841 | ||
| No. of events per day | 4.4 | 4.3 | |
| Risk ratio (95% CI) | 1.08 (0.97–1.19) | 1 | |
| P value | 0.168 | ||
| 65 to 74 years of age | 13 710 | ||
| No. of events per day | 3.8 | 3.7 | |
| Risk ratio (95% CI) | 1.02 (0.91–1.14) | 1 | |
| P value | 0.726 | ||
| 75 to 110 years of age | 42 331 | ||
| No. of events per day | 12.0 | 11.5 | |
| Risk ratio (95% CI) | 1.13 (1.06–1.21) | 1 | |
| P value | <0.001 |
Risk ratio was adjusted for year, week, time elapsed since the start of the study, temperature, barometric pressure, site of sumo tournament, and match days. CI indicates confidence interval.
Table 3 shows the risk ratios for an out‐of‐hospital cardiac arrest on sumo tournament days compared with control days, by cardiac arrest onset time. In patients aged 75 to 110 years, after adjusting for covariates, we found a significant increase in the number of events on sumo tournament days compared with control days from 20:00 to 21:59 hours (OR=1.58). On the other hand, the risk of an event did not increase significantly on sumo tournament days in all patients and in those aged 18 to 74 years, respectively.
Table 3.
Risk Ratios for Out‐of‐Hospital Cardiac Arrests on Grand Sumo Tournaments Days Compared With Control Days by Cardiac Arrest Onset Time in the Various Age Groups
| Hours | Overall (N=71 882) | 18 to 74 y (n=29 551) | 75 to 110 y (n=42 331) |
|---|---|---|---|
| Risk Ratio (95% CI) P Value | Risk Ratio (95% CI) P Value | Risk Ratio (95% CI) P Value | |
| 0 to 1 | 0.89 (0.66–1.21) 0.46 | 0.79 (0.49–1.27) 0.33 | 1.02 (0.69–1.50) 0.93 |
| 2 to 3 | 0.89 (0.64–1.22) 0.46 | 0.66 (0.39–1.11) 0.12 | 1.10 (0.72–1.68) 0.65 |
| 4 to 5 | 1.08 (0.82–1.42) 0.60 | 1.06 (0.68–1.65) 0.80 | 1.03 (0.71–1.49) 0.87 |
| 6 to 7 | 1.08 (0.88–1.31) 0.48 | 0.98 (0.71–1.36) 0.92 | 1.17 (0.90–1.52) 0.24 |
| 8 to 9 | 1.12 (0.93–1.34) 0.24 | 1.13 (0.84–1.51) 0.41 | 1.15 (0.90–1.46) 0.26 |
| 10 to 11 | 0.90 (0.73–1.12) 0.35 | 0.94 (0.69–1.30) 0.72 | 0.90 (0.68–1.20) 0.48 |
| 12 to 13 | 1.18 (0.95–1.47) 0.14 | 1.02 (0.73–1.42) 0.91 | 1.34 (1.00–1.80) 0.05 |
| 14 to 15 | 1.02 (0.81–1.28) 0.87 | 0.97 (0.68–1.37) 0.85 | 1.10 (0.81–1.49) 0.55 |
| 16 to 17 | 0.96 (0.77–1.20) 0.72 | 0.93 (0.66–1.30) 0.66 | 1.01 (0.75–1.37) 0.92 |
| 18 to 19 | 1.08 (0.88–1.33) 0.45 | 1.05 (0.75–1.48) 0.78 | 1.18 (0.90–1.54) 0.22 |
| 20 to 21 | 1.18 (0.95–1.47) 0.14 | 0.78 (0.55–1.12) 0.18 | 1.58 (1.19–2.10) 0.00 |
| 22 to 23 | 0.85 (0.66–1.09) 0.20 | 0.84 (0.56–1.26) 0.41 | 0.89 (0.64–1.25) 0.51 |
Risk ratios were adjusted for year, week, time elapsed since the start of the study, temperature, barometric pressure, site of sumo tournament, and match days.
Figure shows TV sumo tournament program ratings during part of the study setting in the Tokyo area, from the first day to the 15 match days. Of the 57 sumo tournaments that run in the study setting, tournament champions were decided 7 times on day 13, 20 times on day 14, and 30 times on day 15 of the sumo matches. In addition, there were 12 championship matches on day 15. From match days 11 to 15, TV sumo tournaments program ratings in the Tokyo area were higher when sumo tournaments were held in Tokyo than in other cities.
Figure 1.
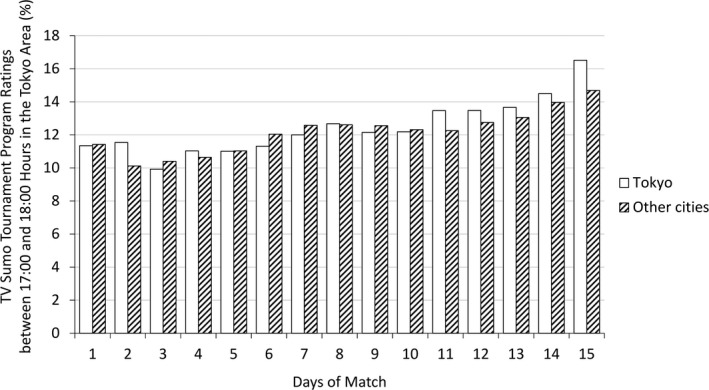
Television sumo tournament program ratings were collected between 17:00 and 18:00 hours, when matches featuring high‐ranking sumo wrestlers were broadcast, in the Tokyo area from 2012 to 2014 by the days of the matches. White and shaded bars show the mean television sumo tournament program ratings when sumo tournaments were held in Tokyo and other cities (Osaka, Nagoya, and Fukuoka), respectively. From match days 11 to 15, the ratings were higher when sumo tournaments were held in Tokyo rather than other cities. TV indicates television.
Table 4 shows how the effects of patient age on the occurrence of out‐of‐hospital cardiac arrest is modified by hours of the day. The table reports adjusted ORs for 4 groups categorized by patient age and hours of the day, with 22:00 to 17:29 hours and 18 to 74 years of age serving as references. In Tokyo, compared with the reference, 17:30 to 21:59 hours with 75 to 110 years of age was associated with a higher occurrence of out‐of‐hospital cardiac arrests (OR=1.13; 1.04–1.22). Between 17:30 and 21:59 hours, compared with 18 to 74 years of age, 75 to 110 years of age was associated with a higher occurrence of out‐of‐hospital cardiac arrests (OR=1.17; 1.05–1.31). The relative excess risk due to interaction was significant (0.14, 95% confidence interval [CI]: 0.02–0.26), and there was a positive effect modification of patient age by sumo broadcasting hours on an additive scale. The ratio of ORs was also significant (1.14, 95% CI: 1.00–1.28), and there was a positive effect modification of patient age by sumo broadcasting hours on a multiplicative scale. In other cities, we found no such effect modification between the 2 factors on the occurrence of out‐of‐hospital cardiac arrests.
Table 4.
Modification of the Effects of Patient Age on the Occurrence of Out‐of‐Hospital Cardiac Arrests of Presumed Cardiac Origin on Grand Sumo Tournaments Days (Versus on Control Days) by Hours when Sumo Tournaments and Summaries are Broadcast
| Patient Age | OR (95% CI) (P Value) for Patient Age Within Each Hours of the Day | ||||
|---|---|---|---|---|---|
| 18 to 74 y | 75 to 110 y | ||||
| n With/Without Events | OR (95% CI) (P Value) | n With/Without Events | OR (95% CI) (P Value) | ||
| Tokyo | |||||
| Hours of the day | |||||
| 22:00 to 17:29 | 2856/18 150 | 1.0 | 4127/25 995 | 1.03 (0.98–1.09) (P=0.29) | 1.03 (0.98–1.09) (P=0.29) |
| 17:30 to 21:59 | 614/3992 | 0.96 (0.87–1.06) (P=0.44) | 1078/6118 | 1.13 (1.04–1.22) (P<0.01) | 1.17 (1.05–1.31) (P<0.01) |
| RERI=0.14 (0.02–0.26), ratio of ORs=1.14 (1.00–1.28, P<0.05) | |||||
| Other cities | |||||
| Hours of the day | |||||
| 22:00 to 17:29 | 2781/18 150 | 1.0 | 4088/25 995 | 1.01 (0.96–1.07) (P=0.67) | 1.01 (0.96–1.07) (P=0.67) |
| 17:30 to 21:59 | 612/3992 | 0.98 (0.89–1.08) (P=0.72) | 925/6118 | 0.96 (0.89–1.05) (P=0.37) | 0.98 (0.88–1.10) (P=0.73) |
| RERI=−0.03 (−0.15 to 0.09), ratio of ORs=0.97 (0.86–1.10, P=0.61) | |||||
ORs were adjusted for year, month, week, temperature, barometric pressure, match days, and site of sumo tournament when sumo tournaments were held in other cities. CI indicates confidence interval; OR indicates odds ratio; other cities, Osaka, Nagoya and Fukuoka; ratio of ORs, ratio of ORs for the occurrence of out‐of‐hospital cardiac arrest on Grand Sumo days; RERI, relative excess risk due to interactions (95% CIs) for the occurrence of out‐of‐hospital cardiac arrest on Grand Sumo days.
Discussion
We first reported an association between sumo tournaments and the occurrence of out‐of‐hospital cardiac arrest in the Tokyo metropolis. In the study setting, we found a significant increase in cardiac events in elderly patients. Since most sumo fans are aged ≥60 years,11 we hypothesized that an increase in the occurrence of out‐of‐hospital cardiac arrests on sumo tournament days would be attributable to increased emotions in spectators of an advanced age. Additional analyses on modified effects of patient age on out‐of‐hospital cardiac arrest by hours of a day, and out‐of‐hospital cardiac arrest by onset hour supported the study hypothesis. In addition, although our TV ratings data cover only part of the study period, it is probable that the greater interest in sumo matches in their final stages in Tokyo may explain the greater increase in out‐of‐hospital cardiac arrest numbers when sumo tournaments were held in Tokyo.
While this is the first study to describe the impact of Sumo on spectators’ cardiovascular health, there are many studies that have looked at the impact of other spectator sports. However, there are many unique features of Sumo in Japan. First, broadcasting occurs during the daytime, it is difficult for employed people to watch the tournament. Second, sumo wrestlers compete for the championship during 15 days of the Grand Sumo tournament. Third, since a wrestler with the highest winning percentage wins the championship, the competition among sumo wrestlers becomes more intense as match days approach.15 Fourth, the Grand Sumo tournament schedule, including venue, time, and broadcasting time, is fixed in Japan.13 Fifth, high‐ranking wrestlers often win the championship, and their matches and summaries of the matches were broadcast from 17:30 to 21:59 hours. We modeled all data using a Poisson distribution. There are unique features with the analysis. The data include many events over many years, which increases the validity of our findings. The analysis has an ability to precisely analyze the times, controlling for weather and day of the week, etc. All of the results are new. However, since this is the first report on sumo tournaments and cardiovascular events, there are no previous studies to compare against. A review of studies on soccer games and cardiovascular events showed that risk ratio estimates for soccer matches and cardiovascular events were between 0.70 and 1.3.10 Although the type of sporting event is different, the effects of the sumo tournaments were also within this range. According to the trigger hypothesis, a stimulus that produces pathophysiological changes leads directly to disease, which in this case is out‐of‐hospital cardiac arrest.8 The mechanisms are not clear, but it is probable that emotional arousal caused by watching the sumo match leads to cardiac arrest through arrhythmias caused by multiple factors, such as acute myocardial infarction, alcohol, catecholamines, or decreased heart rate variability.12, 25
We would now consider the practical implications of the findings. Since the risk ratios were averaged over a 24‐hour period, the value is an average between a risk ratio of 1.00 during hours when sumo matches are not broadcast and a risk ratio >1 during hours when sumo matches are broadcast.10 Thus, risk ratios over a 24‐hour period in the study would correspond to larger acute risk ratios. We found the risk ratio between 20:00 and 21:00 hours was 1.58 in patients aged 75 to 110 years. Given the magnitude of the sumo tournament acute risk (ie, a 60% increase in the occurrence of out‐of‐hospital cardiac arrest in patients aged 75–110 years), it might be necessary to take measures to eliminate these negative effects. Effective countermeasures might include beta‐blocker therapy to reduce ischemic episodes and cardiovascular events; using aspirin to decrease the circadian patterns of acute myocardial infarction; controlling cardiovascular risk factors; and avoiding smoking, fatty foods, overeating, alcohol, and stress.12 While the relative risk increases, the absolute risk of cardiac arrest is likely extremely low. Thus, in our case, although avoiding sumo wrestling broadcasts in old people's homes might be recommendable, the study finding does not warrant avoiding broadcasts of this popular event in other places.
There are several limitations to this study. First, we used out‐of‐hospital cardiac arrest as an end point. To verify the validity of our findings, it is necessary to evaluate the association between sumo tournaments and other outcome measures, such as hospital admissions attributable to acute myocardial infarction, stroke, unstable angina, and symptomatic cardiac arrhythmia. Second, patients being reported were patients with out‐of‐hospital cardiac arrest of presumed‐cardiac origin. Although the origin of the cardiac arrest (ie, cardiac or non‐cardiac) was determined clinically by the physician in charge in cooperation with emergency medical services personnel, some misclassification may have occurred. However, misclassification will always bias an effect, if there is one, toward the null value.26 We believe that the effect of misclassification would not pose a serious problem. Third, there are a large number of confounding factors that we cannot account for in the analysis. Especially, we could not control the effects of other potential trigger factors, such as overeating, alcohol consumption, smoking, lack of sleep, and failure to comply with a medical regimen.
In summary, we found a significant increase in the occurrence of out‐of‐hospital cardiac arrests in the Tokyo metropolis in association with sumo tournaments between 2005 and 2014. We hypothesize that these additional cardiovascular events in patients of advanced age were triggered by emotional arousal in relation to the sumo matches when sumo tournaments were held in Tokyo. Additional studies are necessary to verify these findings on sumo tournaments and cardiovascular events.
Sources of Funding
This work was supported by Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Numbers 15K08714, 16H05247, and 18K11666. The funding source had no role in the study design, data collection, data analysis, data interpretation, or preparation of the article.
Disclosures
None.
Acknowledgments
The authors are grateful to Kyoko Ishikawa and Yuji Shiiba of Video Research Ltd. for allowing us to use data on TV sumo tournament program ratings in the Tokyo area between 2012 and 2014.
(J Am Heart Assoc. 2018;7:e009163 DOI: 10.1161/JAHA.118.009163.)
References
- 1. Schwartz BG, French WJ, Mayeda GS, Burstein S, Economides C, Bhandari AK, Cannom DS, Kloner RA. Emotional stressors trigger cardiovascular events. Int J Clin Pract. 2012;66:631–639. [DOI] [PubMed] [Google Scholar]
- 2. Leor J, Kloner RA. The Northridge earthquake as a trigger for acute myocardial infarction. Am J Cardiol. 1996;77:1230–1232. [DOI] [PubMed] [Google Scholar]
- 3. Suzuki S, Sakamoto S, Miki T, Matsuo T. Hanshin‐Awaji earthquake and acute myocardial infarction. Lancet. 1995;345:981. [DOI] [PubMed] [Google Scholar]
- 4. Kitamura T, Kiyohara K, Iwami T. The great east Japan earthquake and out‐of‐hospital cardiac arrest. N Engl J Med. 2013;369:2165–2167. [DOI] [PubMed] [Google Scholar]
- 5. Meisel SR, Kutz I, Dayan KI, Pauzner H, Chetboun I, Arbel Y, David D. Effect of Iraqi missile war on incidence of acute myocardial infarction and sudden death in Israeli civilians. Lancet. 1991;338:660–661. [DOI] [PubMed] [Google Scholar]
- 6. Bergovec M, Mihatov S, Prpic H, Rogan S, Batarelo V, Sjerobabski V. Acute myocardial infarction among civilians in Zagreb city area. Lancet. 1992;339:303. [DOI] [PubMed] [Google Scholar]
- 7. Wilbert‐Lampen U, Leistner D, Greven S, Pohl T, Sper S, Volker C, Guthlin D, Plasse A, Knez A, Kuchenhoff H, Steinbeck G. Cardiovascular events during World Cup soccer. N Engl J Med. 2008;358:475–483. [DOI] [PubMed] [Google Scholar]
- 8. Carroll D, Ebrahim S, Tilling K, Macleod J, Smith GD. Admissions for myocardial infarction and World Cup football: database survey. BMJ. 2002;325:1439–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berthier F, Boulay F. Lower myocardial infarction mortality in French men the day France won the 1998 World Cup of football. Heart. 2003;89:555–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barone‐Adesi F, Vizzini L, Merletti F, Richiardi L. It is just a game: lack of association between watching football matches and the risk of acute cardiovascular events. Int J Epidemiol. 2010;39:1006–1013. [DOI] [PubMed] [Google Scholar]
- 11. Yahoo! JAPAN big data report. 2017.
- 12. Leeka J, Schwartz BG, Kloner RA. Sporting events affect spectators’ cardiovascular mortality: it is not just a game. Am J Med. 2010;123:972–977. [DOI] [PubMed] [Google Scholar]
- 13. NHK sports online. 2017.
- 14. Japanese Guideline for Emergency Care and Cardiopulmonary Resuscitation. 3rd ed Tokyo: Health Shupansha; 2007. [Google Scholar]
- 15. Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, Bossaert L, Delooz HH, Dick WF, Eisenberg MS. Recommended guidelines for uniform reporting of data from out‐of‐hospital cardiac arrest: the Utstein Style. A statement for health professionals from a Task Force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–975. [DOI] [PubMed] [Google Scholar]
- 16. Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A, Cobbe S. Recommended guidelines for reviewing, reporting, and conducting research on in‐hospital resuscitation: the in‐hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–2239. [DOI] [PubMed] [Google Scholar]
- 17. Registry of past meteorological data. 2017.
- 18. Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42:1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brumback BA, Ryan LM, Schwartz JD, Neas LM, Stark PC, Burge HA. Transitional regression models, with application to environmental time series. J Am Stat Assoc. 2000;95:16–27. [Google Scholar]
- 20. Akaike H. Information theory and an extension of the maximum likelihood principle In: Petrov BN, Csaki F, eds. 2nd International Symposium on Information Theory. Budapest: Akademiai Kiado; 1973:267–281. [Google Scholar]
- 21. Strike PC, Perkins‐Porras L, Whitehead DL, McEwan J, Steptoe A. Triggering of acute coronary syndromes by physical exertion and anger: clinical and sociodemographic characteristics. Heart. 2006;92:1035–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tofler GH, Muller JE. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation. 2006;114:1863–1872. [DOI] [PubMed] [Google Scholar]
- 23. Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41:514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992;3:452–456. [DOI] [PubMed] [Google Scholar]
- 25. Hemingway H, Malik M, Marmot M. Social and psychosocial influences on sudden cardiac death, ventricular arrhythmia and cardiac autonomic function. Eur Heart J. 2001;22:1082–1101. [DOI] [PubMed] [Google Scholar]
- 26. Rothman KJ. Epidemiology: An Introduction. New York: Oxford University Press; 2012. [Google Scholar]


