Abstract
Background
Current preoperative models use clinical risk factors alone in estimating risk of in‐hospital mortality following cardiac surgery. However, novel biomarkers now exist to potentially improve preoperative prediction models. An assessment of Galectin‐3, N‐terminal pro b‐type natriuretic peptide (NT‐ProBNP), and soluble ST2 to improve the predictive ability of an existing prediction model of in‐hospital mortality may improve our capacity to risk‐stratify patients before surgery.
Methods and Results
We measured preoperative biomarkers in the NNECDSG (Northern New England Cardiovascular Disease Study Group), a prospective cohort of 1554 patients undergoing coronary artery bypass graft surgery. Exposures of interest were preoperative levels of galectin‐3, NT‐ProBNP, and ST2. In‐hospital mortality and adverse events occurring after coronary artery bypass graft were the outcomes. After adjustment, NT‐ProBNP and ST2 showed a statistically significant association with both their median and third tercile categories with NT‐ProBNP odds ratios of 2.89 (95% confidence interval [CI]: 1.04–8.05) and 5.43 (95% CI: 1.21–24.44) and ST2 odds ratios of 3.96 (95% CI: 1.60–9.82) and 3.21 (95% CI: 1.17–8.80), respectively. The model receiver operating characteristic score of the base prediction model (0.80 [95% CI: 0.72–0.89]) varied significantly from the new multi‐marker model (0.85 [95% CI: 0.79–0.91]). Compared with the Northern New England (NNE) model alone, the full prediction model with biomarkers NT‐proBNP and ST2 shows significant improvement in model classification of in‐hospital mortality.
Conclusions
This study demonstrates a significant improvement of preoperative prediction of in‐hospital mortality in patients undergoing coronary artery bypass graft and suggests that biomarkers can be used to identify patients at higher risk.
Keywords: cardiac biomarkers, cardiac surgery, mortality, outcomes research
Subject Categories: Mortality/Survival, Cardiovascular Surgery, Biomarkers, Quality and Outcomes
Clinical Perspective
What Is New?
Current preoperative models use clinical risk factors alone in estimating risk of in‐hospital mortality following cardiac surgery.
What Are the Clinical Implications?
The application of novel cardiac biomarkers ST2, N‐terminal pro‐brain natriuretic peptide, and Galectin‐3 may improve the predictive ability of an existing prediction model of in‐hospital mortality may improve our capacity to risk‐stratify patients before surgery.
Introduction
Measures to reduce in‐hospital mortality after coronary artery bypass graft (CABG) surgery have involved the development of risk prediction models.1, 2, 3, 4, 5, 6, 7, 8 The ability of current models to improve the predictive ability of in‐hospital mortality has not been improved by the addition of additional patient and disease characteristics.9, 10 In recent years, new biomarkers with the ability to measure subtle tissue‐level injuries have become available. While an effort to improve the predictive ability of an existing model through the addition of 4 preoperative biomarkers [cardiac troponin T, N‐terminal pro‐brain natriuretic peptide (NT‐proBNP), high‐sensitivity C‐reactive protein, and blood glucose], did not significantly improve the model's ability to predict in‐hospital mortality, the consideration of certain other biomarkers may result in a statistically significant improvement in predictive ability.11, 12
With the use of a base prediction model of mortality, we can assess the ability of certain biomarkers to improve preoperative prediction of in‐hospital mortality in patients with CABG. Given NT‐proBNP's strong associations with heart failure, mortality attributable to cardiovascular events, and mortality after cardiac surgery, its inclusion in a prediction model of in‐hospital mortality may serve to improve the model's predictive ability.13, 14, 15, 16 Galectin‐3, a member of the lectin family of proteins, and ST2, a biomarker for cardiac stress, have also been found to be strongly associated with heart failure.17, 18, 19, 20, 21, 22 Additionally, Galectin‐3 has been found to be associated with increased risk for all‐cause mortality in the Framingham Offspring Cohort.23 ST2 has been shown to be a sensitive biomarker of cardiac stress with statistically significant differences in concentration when stratified by age or sex.24, 25 We hypothesized that the use of these 3 biomarkers will improve the current risk prediction model used by the American College of Cardiology/American Heart Association CABG guidelines.26, 27, 28
Methods
To ensure the entire research community can benefit from the data generated by our study group, pending third parties rights, our institution will share the data with the outside researchers upon request. We will ensure the protection of patient privacy associated with clinical data through appropriate de‐identification and security measures.
Study Design and Setting
This study used data and blood specimens stored from the Northern New England (NNE) Biomarker Study, a regional consortium in Northern New England with experience in risk prediction in CABG surgery, to conduct a prospective cohort analysis.7, 29, 30 This study uses a harmonized data set from 8 medical centers in Vermont, New Hampshire, and Maine in the NNECDSG (NNE Cardiovascular Disease Study Group). The NNECDSG is a voluntary, regional collaborative of clinicians, research scientists and hospital administrators dedicated to improving the quality, safety, and effectiveness of care delivered to patients undergoing cardiac surgery. The NNECDSG registry contains data on patient characteristics, procedural indications, clinical variables, and in‐hospital outcomes. Data are periodically validated to ensure that all procedures and end points included in the registry have been accurately assessed. The Committee for the Protection of Human Subjects at Dartmouth College (IRB) approved this study for both the prospective cohort with patient consent and the linkage of readmission and mortality events.
Patient, procedural and outcome data were collected from patients undergoing CABG surgery and/or valve surgery at any of the participating hospitals were prospectively enrolled into the NNE Biomarker Study from 2004 to 2007 (N=1690). Those undergoing isolated CABG (n=1421) and CABG incidental to heart valve repair or replacement were included in the analyses (n=133). Finally, only patients who had all biomarker levels collected were retained in the final analyses (n=1554) (Figure 1). For the present study, the sample included patients undergoing emergent, urgent, and non‐urgent CABG surgeries. Collected characteristic and risk factor variables included: patient sex and age, ejection fraction, percentage stenosis of the left main coronary artery, white blood cell count, priority of surgery, prior occurrence of CABG, diabetes mellitus, 3‐vessel disease, preoperative renal failure, serum creatinine >2 mg/dL, chronic obstructive pulmonary disease, and vascular disease. Priority of surgery was assessed by cardiothoracic surgeons using previously published definitions.29
Figure 1.
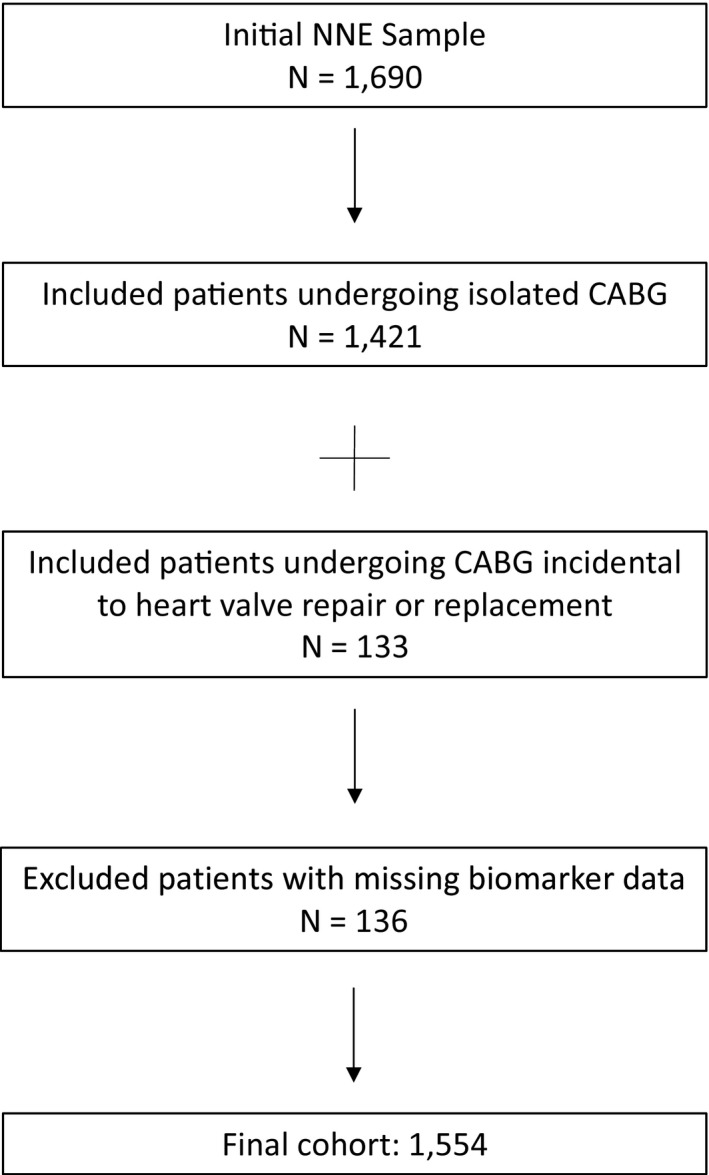
NNE patient cohort flow diagram. Patient, procedural and outcome data were collected from patients undergoing CABG surgery and/or valve surgery at any of the participating hospitals were prospectively enrolled into the NNE Biomarker Study from 2004 to 2007 (N=1690). Those undergoing isolated CABG (n=1421) and CABG incidental to heart valve repair or replacement were included in the analyses (n=133). We excluded patients with missing biomarker data (n=136). The final cohort included 1554 patients. (CABG indicates coronary artery bypass grafting; NNE, Northern New England).
Sample Collection
Methods for blood sample collection, storage, and analysis have been noted in a prior publication.11 Blood was collected immediately before induction of isolated CABG at each participating site of the NNECDSG from 2003 to 2007. Blood was allowed to clot at room temperature for 20 minutes to separate out red blood cells before being centrifuged at 1855 g for 20 minutes. The samples were stored at the respective medical centers until transportation to, and analysis at, a central laboratory for preoperative levels of Galectin‐3, NT‐ProBNP, and ST2.
Primary and Secondary Outcomes
The primary outcome of this study was all‐cause in‐hospital mortality from the index admission. In‐hospital mortality was determined at the time of discharge. Secondary outcomes were new atrial fibrillation, new dialysis, mediastinitis, transient ischemic attack, stroke, low cardiac output, pneumonia, bleeding complications, and leg infection collected prospectively from each medical center.
Statistical Analysis
Differences in risk factors were compared using Pearson's chi‐square tests; continuous variables were compared with 2‐sample t test or Wilcoxon rank‐sum tests. Patients were categorized into 2 groups for each biomarker based on the median value of that biomarker. Similarly, patients were equally distributed into terciles for each of the biomarkers. Dummy variables were created for each of the terciles and median values. Logistic regression analysis was used to perform univariate and multivariate analyses assessing the association between these median and tercile categories and the primary and secondary outcomes. The covariate in the multivariate regression models was the predicted score described below. We also conducted multivariate fractional polynomial modeling to further examine associations with biomarker categories and the primary and secondary outcomes. All statistical analyses were performed using the Stata 14.1 statistical program (Stata Corp., College Station, TX).
NNE Base Risk Prediction Model
The NNE base preoperative prediction model of in‐hospital mortality in this study was built using preoperative risk scores of risk factors for mortality designated by the American College of Cardiology and American Heart Association.7, 26, 31 The in‐hospital mortality model corrects for age, sex, ejection fraction <40%, number of diseased vessels, left main disease >50%, white blood cell count, prior myocardial infarction, prior CABG surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease and urgent and emergent priority. The risk scores were used to create a predicted score that served as the one covariate in the logistic models with and without biomarkers to limit over‐fitting of the logistic model. New prediction models were built by adding the tercile and median values of Galectin‐3, NT‐ProBNP, and ST2 to the base model, first by the addition of each individual biomarker and then by adding the panel of 2 biomarkers. The discriminating ability of the regression model was assessed by the c‐statistic, which is the area under the receiver operating characteristic (ROC) curve.32 The cut point for net reclassification improvement (NRI) and integrated discrimination improvement (IDI) calculations is 0.92% for preoperative in‐hospital mortality.
Secondary Analyses
As a secondary analyses we applied the well documented 2008 Society of Thoracic Surgeons (STS) CABG risk model to our cohort.33 We sought to compare risk stratification methods across the models to assess outcomes in the higher risk sub‐cohort. The STS CABG risk model includes 35 predictor variables that have been endorsed by an expert panel of cardiothoracic surgeons and biostatisticians.
External Validation Cohort
The TRIBE‐AKI (Translational Research Investigating Biomarker End Points for Acute Kidney Injury) study is a prospective cohort of 1417 adults with high risk of acute kidney injury who underwent cardiac surgery (CABG or valve surgery). Participants were prospectively enrolled at 6 academic centers in North America from 2007 through 2010.34 For Canadian participants, mortality was determined using the Registered Persons Database. These datasets were linked using unique encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES). Full study details were previously described.34, 35, 36
Short‐and Mid‐Term Mortality Model Analyses
In addition to postoperative in‐hospital mortality, we were interested to evaluate the predictive ability of the NNE and STS models on short‐and mid‐term mortality with our cohort. We applied the same model parameters already established in the NNE and STS risk models, but focused on 1‐ and 5‐year outcomes.
Results
Descriptive Data
Demographic differences in risk factors and preoperative biomarker levels, after stratification by status at discharge, are presented in Table 1. Of those in our cohort, 32 (2.1%) experienced in‐hospital death after surgery. The population of patients who were dead at discharge had a higher proportion of patients who were older (P=0.006), were female (P=0.002), had preoperative intra‐aortic balloon pump (P=0.001), had prior CABG (P<0.001), had unstable angina (P=0.005), received blood transfusion (P≤0.001) and COPD (P=0.010). For all 3 biomarkers, the patients who were dead at discharge had much higher, statistically significant, preoperative levels than the patients who were alive.
Table 1.
Preoperative Patient Characteristics by Status at Discharge
| Status at Discharge | P Value | ||
|---|---|---|---|
| Alive (n=1522) | Deceased (n=32) | ||
| Risk factors | |||
| Age | 65.2±10.1 | 70.2±10.7 | 0.006 |
| Female | 351 (23.1%) | 15 (46.9%) | 0.002 |
| BMI | 29.7±5.5 | 29.0±6.2 | 0.484 |
| BSA | 2.0±0.2 | 1.9±0.3 | 0.011 |
| Smoker | 345 (22.7%) | 7 (21.9%) | 0.912 |
| Atrial fibrillation | 101 (6.6%) | 4 (12.5%) | 0.191 |
| CHF | 159 (10.5%) | 6 (18.8%) | 0.132 |
| Preoperative creatinine | 1.2±1.0 | 1.48±1.05 | 0.066 |
| Diabetes mellitus | 570 (37.5%) | 11 (34.4%) | 0.722 |
| EF <40 | 159 (11.0%) | 6 (11.1%) | 0.981 |
| Hypertension | 1228 (80.8%) | 24 (75.0%) | 0.412 |
| Preoperative IABP | 58 (3.8%) | 5 (15.6%) | 0.001 |
| Prior MI | 0.819 | ||
| None | 856 (56.2%) | 16 (50.0%) | |
| <24 h preoperative | 26 (1.7%) | 0 (0.0%) | |
| >24 h and <7 d | 286 (18.8%) | 8 (25.0%) | |
| >7 and <365 d | 152 (10.0%) | 3 (9.4%) | |
| >365 d | 202 (13.3%) | 5 (15.6%) | |
| VAD | 408 (26.8%) | 14 (43.8%) | 0.033 |
| Unstable angina | 829 (55.0%) | 25 (80.6%) | 0.005 |
| COPD | 192 (12.6%) | 9 (28.1%) | 0.010 |
| Left main stenosis | 511 (33.6%) | 14 (43.8%) | 0.228 |
| Prior CABG | 31 (2.1%) | 4 (13.3%) | 0.000 |
| Prior PCI | 300 (19.7%) | 7 (21.9%) | 0.761 |
| Priority | 0.082 | ||
| Emergency or emergent salvage | 29 (1.9%) | 1 (3.1%) | |
| Urgent | 1026 (67.4%) | 27 (84.4%) | |
| Non‐urgent | 467 (30.7%) | 4 (12.5%) | |
| Received transfused blood | 565 (37.1%) | 27 (84.4%) | 0.000 |
| RBCs transfused preoperatively | 0.881 | ||
| 0 | 1489 (98.0%) | 32 (100.0%) | |
| 1 | 9 (0.6%) | 0 (0.0%) | |
| 2 | 15 (1.0%) | 0 (0.0%) | |
| 3 | 7 (0.5%) | 0 (0.0%) | |
BMI indicates body mass index; BSA, body surface area; CABG; coronary artery bypass graft; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; EF, ejection fraction; IABP, intra‐aortic balloon pump; MI, myocardial infarction; PCI, percutaneous coronary intervention; RBC, red blood cell count; VAD, ventricular assist device.
Univariate Analyses
We found a positive association with elevated preoperative novel cardiac biomarkers and in‐hospital mortality after CABG surgery. There was a significant association of in‐hospital mortality for elevated preoperative ST2 and NT‐proBNP tercile levels (P=0.006 and P<0.001, respectively). Preoperative Galectin‐3 terciles yielded a non‐significant difference (P=0.250) (Figure 2).
Figure 2.
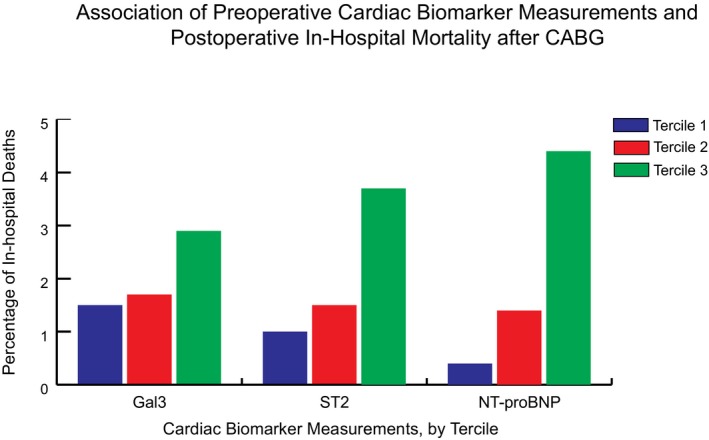
Association of preoperative cardiac biomarker measurements and postoperative in‐hospital mortality after CABG. We found a positive association with elevated preoperative novel cardiac biomarkers and in‐hospital mortality after CABG surgery. There is a statistically significant association of in‐hospital mortality for elevated preoperative ST2 and NT‐proBNP tercile levels (P=0.006 and P<0.001, respectively). Preoperative Gal3 terciles yielded a non‐significant difference (P=0.250). The addition of ST2 and NT‐proBNP to the NNE base risk prediction model significantly improved the preoperative prediction of in‐hospital mortality over patient characteristics and risk factors alone. (CABG indicates coronary artery bypass grafting; Gal3, Galectin‐3; NNE, Northern New England; NT‐proBNP, N‐terminal pro b‐type natriuretic peptide).
Odds ratios resulting from the univariate analysis assessing the relationship between preoperative biomarker are displayed in Tables 2 and 3. The unadjusted univariate analyses found that preoperative NT‐ProBNP and ST2 categories were significantly associated with in‐hospital mortality. Galectin‐3 was associated with new atrial fibrillation, low cardiac output, and leg wound infection morbidities. NT‐ProBNP was associated with new atrial fibrillation, new dialysis, stroke, low cardiac output, and pneumonia while ST2 was associated with mediastinitis, new dialysis, stroke, low cardiac output, and pneumonia.
Table 2.
Unadjusted Univariate Associations of Preoperative Biomarker Measurements and Postoperative In‐Hospital Outcomes
| Outcomes (OR [95% CI]) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| In‐Hospital Mortality | New AFib | New Dialysis | Mediastinitis | Transient Ischemic Attack | Low Cardiac Output | Stroke | Pneumonia | Bleeding Complications | Leg Infection | |
| Gal3 | ||||||||||
| Median 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Median 2 | 1.68 (0.82–3.47) | 1.44 (1.13–1.84) | 1.25 (0.38–4.13) | 0.57 (0.19–1.71) | 1.77 (0.29–10.64) | 1.69 (1.11–2.57) | 1.75 (0.83–3.70) | 1.59 (0.81–3.13) | 1.30 (0.57–2.99) | 3.97 (1.10–14.29) |
| Tercile 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Tercile 2 | 1.13 (0.43–2.95) | 1.35 (0.99–1.84) | 0.50 (0.09–2.74) | 0.67 (0.19–2.40) | 1.11 (0.16–7.94) | 1.55 (0.89–2.71) | 2.04 (0.82–5.10) | 0.58 (0.23–1.48) | 0.62 (0.20–1.91) | 1.60 (0.27–9.63) |
| Tercile 3 | 1.91 (0.80–4.54) | 1.54 (1.14–2.09) | 1.35 (0.36–5.04) | 0.70 (0.20–2.49) | 0.65 (0.06–7.17) | 2.04 (1.20–3.47) | 1.29 (0.48–3.49) | 1.44 (0.68–3.04) | 1.24 (0.49–3.18) | 5.21 (1.12–24.27) |
| NT‐proBNP | ||||||||||
| Median 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Median 2 | 5.53 (2.12–14.44) | 1.41 (1.10–1.80) | 11.19 (1.43–87.74) | 2.83 (0.88–9.07) | 0.48 (0.05–4.32) | 3.11 (1.95–4.96) | 2.84 (1.25–6.41) | 1.78 (0.90–3.55) | 1.36 (0.59–3.12) | 0.84 (0.29–2.42) |
| Tercile 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Tercile 2 | 3.52 (0.73–17.04) | 1.48 (1.08–2.02) | 0.20 (0.04–0.91) | 2.08 (0.38–11.41) | 0.44 (0.05–4.26) | 3.11 (1.45–6.69) | 0.57 (0.17–1.96) | 1.00 (0.37–2.68) | 1.44 (0.54–3.83) | 1.07 (0.31–3.74) |
| Tercile 3 | 11.89 (2.79–50.73) | 1.60 (1.18–2.18) | 1 (REF) | 4.74 (1.00–22.48) | 0.84 (0.09–8.16) | 7.66 (3.76–15.59) | 2.79 (1.16–6.70) | 2.54 (1.11–5.82) | 0.91 (0.30–2.72) | 0.93 (0.25–3.50) |
| ST‐2 | ||||||||||
| Median 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Median 2 | 4.43 (1.81–10.82) | 1.12 (0.87–1.42) | 2.82 (0.74–10.68) | 6.37 (1.42–28.60) | 0.84 (0.14–5.09) | 1.64 (1.07–2.49) | 3.34 (1.43–7.84) | 2.30 (1.12–4.71) | 0.94 (0.41–2.13) | 2.60 (0.81–8.35) |
| Tercile 1 | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) | 1 (REF) |
| Tercile 2 | 1.60 (0.52–4.93) | 1.28 (0.94–1.73) | 2.09 (0.19–23.14) | 0.71 (0.25–2.08) | 0.34 (0.04–3.31) | 1.66 (0.95–2.90) | 6.58 (1.48–29.32) | 2.63 (0.93–7.42) | 0.44 (0.13–1.42) | 6.09 (0.73–50.83) |
| Tercile 3 | 3.88 (1.44–10.48) | 1.32 (0.98–1.79) | 8.83 (1.10–70.92) | 1 (REF) | 0.45 (0.05–4.36) | 2.14 (1.25–3.66) | 7.58 (1.43–7.84) | 3.67 (1.35–9.97) | 1.15 (0.46–2.85) | 7.49 (0.92–61.20) |
Model adjusts for age, sex, ejection fraction <40%, presence of any disease, left main stenosis >50%, white blood cell count, prior myocardial infarction, prior coronary artery bypass graft surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease, and urgent and emergent priority. CI indicates confidence interval; Median 1, below median values; Median 2, above median values; New AFib, new atrial fibrillation; OR, odds ratio.
Table 3.
Unadjusted Fractional Polynomials With Preoperative Biomarker Measurements and Postoperative In‐Hospital Outcomes
| Biomarker Categories | Outcomes (OR [95% CI]) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| In‐Hospital Mortality | New AFib | New Dialysis | Mediastinitis | Transient Ischemic Attack | Stroke | Low Cardiac Output | Pneumonia | Bleeding Complications | Leg Infection | |
| Gal3 | ||||||||||
| Preoperative Gal30.5 | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) |
| Preoperative Gal33 | 1.37 (1.02–1.85) | 1.16 (1.03–1.30) | 1.20 (0.67–2.15) | 0.67 (0.19–2.40) | 0.83 (0.42–1.66) | 1.34 (0.95–1.90) | 1.26 (1.05–1.51) | 1.27 (0.96–1.69) | 1.00 (0.65–1.55) | 1.47 (1.10–1.95) |
| NT‐proBNP | ||||||||||
| Preoperative BNP−2 | 0.05 (0.00–0.98) | 0.90 (0.83–0.98) | 0.00 (0.00–20.59) | 0.26 (0.05–1.26) | 0.96 (0.84–1.09) | 0.83 (0.58–1.18) | 0.90 (0.68–1.20) | 0.64 (0.35–1.15) | 0.93 (0.78–1.10) | 0.72 (0.50–1.03) |
| Preoperative BNP0.5 | 1.24 (1.15–1.35) | 1.08 (1.02–1.13) | 1.42 (1.24–1.63) | 1.23 (1.05–1.44) | 1.14 (0.61–2.12) | 1.20 (1.11–1.30) | 1.22 (1.14–1.31) | 1.16 (1.07–1.25) | 0.90 (0.74–1.10) | 1.09 (0.90–1.33) |
| ST‐2 | ||||||||||
| Preoperative ST2−1 | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 0.98 (0.02–46.42) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (0.99–1.00) | 1.00 (1.00–1.00) |
| Preoperative ST22 | 0.01 (0.00–0.40) | 0.38 (0.16–0.92) | 0.00 (0.00–0.30) | 0.00 (0.00–0.02) | 0.98 (0.94–1.03) | 0.01 (0.00–0.11) | 0.07 (0.01–0.40) | 0.00 (0.00–0.11) | 1.79 (0.15–21.65) | 0.00 (0.00–0.28) |
Model adjusts for age, sex, ejection fraction <40%, presence of any disease, left main stenosis >50%, white blood cell count, prior myocardial infarction, prior coronary artery bypass graft surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease and urgent and emergent priority. CI indicates confidence interval; Gal3, Galectin‐3; Median 1, below median values; Median 2, above median values; New AFib, new atrial fibrillation; OR, odds ratio. Superscript values represent fractional powers.
Multivariate Analyses
After adjustment using the predicted score calculated from the risk factors, multivariate regression models using the median and tercile categories of each biomarker are described in Table 4. We found a non‐significant association between preoperative Galectin‐3 and mortality status at discharge. ST2 and NT‐ProBNP median and third tercile measurements had significant associations with in‐hospital death, after adjustment for risk factors using the predicted score.
Table 4.
NNE Adjusted Multivariate Associations With In‐Hospital Mortality
| Preoperative Biomarker Category | OR (95% CI) | P Value |
|---|---|---|
| Galectin‐3 | ||
| Median 1 | 1 [REF] | |
| Median 2 | 1.08 (0.51–2.29) | 0.835 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 0.98 (0.36–2.68) | 0.971 |
| Tercile 3 | 1.10 (0.45–2.67) | 0.832 |
| NT‐ProBNP | ||
| Median 1 | 1 [REF] | |
| Median 2 | 2.89 (1.04–8.05) | 0.043 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 2.53 (0.51–12.61) | 0.258 |
| Tercile 3 | 5.43 (1.21–24.44) | 0.027 |
| ST‐2 | ||
| Median 1 | 1 [REF] | |
| Median 2 | 3.96 (1.60–9.82) | 0.003 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 1.81 (0.58–5.65) | 0.310 |
| Tercile 3 | 3.21 (1.17–8.80) | 0.023 |
CI indicates confidence interval; OR, odds ratio.
Model adjusts for age, sex, ejection fraction <40%, presence of any disease, left main stenosis >50%, white blood cell count, prior myocardial infarction, prior coronary artery bypass graft surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease, and urgent and emergent priority.
NNE Preoperative Mortality Model
The model ROC score of the base prediction model was 0.80 (95% CI: 0.72–0.89) and is noted in Table 5. The individual addition of each unique biomarker's median and tercile categories to the base model resulted in non‐significant improvement in predictive ability of mortality. Applying a fully adjusted model containing median and tercile categories of NT‐ProBNP and ST2 biomarkers resulted in an ROC score of 0.85 (95% CI: 0.79–0.91; P=0.048) for the significant difference in the predictive ability for mortality of this model to the base. With the addition of Galectin‐3, a fully adjusted model that contained median categories of all biomarkers (NT‐ProBNP, ST2, and Galectin‐3) resulted in a shared ROC score of 0.85 (95% CI: 0.79–0.91) and a non‐significant P‐value of 0.058. Compared with the base NNE model alone, the full multi‐marker prediction model shows significant improvement in model classification of in hospital mortality. NRI and IDI calculated indices are listed in Table 6.
Table 5.
Risk Prediction NNE Models With Added Biomarkers
| Biomarker Categories | Prediction Modelsb (Model ROC [95% CI]) | ||||||
|---|---|---|---|---|---|---|---|
| NNE Model | NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.80 (0.72–0.89) | 0.82 (0.76–0.89) | 0.84 (0.76–0.91) | 0.80 (0.72–0.89) | 0.82 (0.76–0.89) | 0.85 (0.79–0.91) | 0.85 (0.79–0.91) |
| P valuea | ··· | 0.275 | 0.128 | 0.698 | 0.279 | 0.048 | 0.058 |
| Tercile | 0.80 (0.72–0.89) | 0.83 (0.77–0.90 | 0.82 (0.74–0.90) | 0.80 (0.71–0.89) | 0.83 (0.77–0.90) | 0.84 (0.78–0.91) | 0.84 (0.78–0.91) |
| P valuea | ··· | 0.198 | 0.352 | 0.425 | 0.210 | 0.072 | 0.090 |
CI indicates confidence interval; Gal3, Galectin‐3; NNE, Northern New England; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide.
P values compare the area under the ROC curve from the adjusted model to the area under the ROC curve from the base NNE Model.
Model adjusts for age, sex, ejection fraction <40%, presence of any disease, left main stenosis >50%, white blood cell count, prior myocardial infarction, prior coronary artery bypass graft surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease, and urgent and emergent priority.
Table 6.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the NNE Base Model, at Median and Tercile Cut Points
| Biomarker Categories | Prediction Modelsb | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.06 | 0.01 | 0.02 | 0.02 | 0.00 | 0.00 | 0.06 | 0.01 | 0.13 | 0.02 | 0.13 | 0.02 |
| P valuea | 0.278 | 0.001 | 0.773 | 0.032 | 0.398 | 0.494 | 0.073 | 0.001 | 0.044 | 0.017 | 0.045 | 0.014 |
| Tercile | 0.11 | 0.01 | 0.03 | 0.01 | 0.00 | 0.00 | 0.12 | 0.01 | 0.10 | 0.01 | 0.13 | 0.02 |
| P valuea | 0.075 | 0.022 | 0.460 | 0.080 | 0.505 | 0.161 | 0.323 | 0.023 | 0.064 | 0.020 | 0.039 | 0.016 |
IDI indicates integrated discrimination improvement; NNE, Northern New England; NRI, net reclassification improvement.
The predicted risk threshold based on preoperative biomarkers is 0.92% for NDI and IDI calcuations.
Model adjusts for age, sex, ejection fraction <40%, presence of any disease, left main stenosis >50%, white blood cell count, prior myocardial infarction, prior coronary artery bypass graft surgery, presence of any vascular disease, presence of diabetes mellitus, history of renal failure, chronic obstructive pulmonary disease and urgent and emergent priority.
External Validation Model Performance
We externally validated our results using coefficients from the NNE preoperatively mortality model. The ROC score for the in‐hospital clinical model with the TRIBE cohort is 0.67 (95% CI: 0.56–0.78). When we applied the 1‐year model using the tercile cut points, the ROC resulted in 0.66 (95% CI: 0.60–0.73). Similarly with the 5‐year model the ROC resulted in 0.66 (95% CI: 0.62–0.71).
STS Preoperative Mortality Prediction Model
The model ROC score of the base STS CABG mortality risk prediction was 0.81. STS preoperative adjusted multivariate associations with in‐hospital death are described in Table 7. We found few appreciable differences between the predicted risk between the NNE and STS models. Adjusting for the STS model, the NT‐proBNP median cut point resulted in less risk and was non‐significant (OR 2.36; 95% CI: 0.82–6.87; P=0.117) compared with the NNE model (OR: 2.89; 95% CI: 1.04–8.05; P=0.043). Similarly, after adjustment, the highest NT‐proBNP tercile is associated with 4.37‐fold odds of in‐hospital death after CABG, but this association is not significant. Risk of in‐hospital death, adjusted with the STS model, was significantly higher for preoperative ST2 median and highest tercile cut points; adjustment using the NNE model resulted in similar findings. None of the Galectin‐3 results changed meaningfully after adjustment with the STS model.
Table 7.
STS Preoperative Adjusted Multivariate Associations With In‐Hospital Mortality
| Preoperative Biomarker Category | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Galectin‐3 | ||
| Median 1 | 1 [REF] | |
| Median 2 | 1.18 (0.55–2.54) | 0.675 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 1.06 (0.39–2.91) | 0.909 |
| Tercile 3 | 1.18 (0.47–2.94) | 0.728 |
| NT‐ProBNP | ||
| Median 1 | 1 [REF] | |
| Median 2 | 2.36 (0.81–6.87) | 0.117 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 2.23 (0.45–11.12) | 0.328 |
| Tercile 3 | 4.37 (0.93–20.49) | 0.061 |
| ST‐2 | ||
| Median 1 | 1 [REF] | |
| Median 2 | 3.62 (1.43–9.15) | 0.007 |
| Tercile 1 | 1 [REF] | |
| Tercile 2 | 1.96 (0.59–6.45) | 0.269 |
| Tercile 3 | 2.96 (1.04–8.41) | 0.042 |
CI indicates confidence interval; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide.
*Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
C‐statistics obtained from models adjusting for the variables in the 2008 STS CABG mortality risk model were higher across the board than those obtained adjusting for the variables in the NNE mortality risk model. The base STS mortality model c‐statistic was 0.86 (0.80–0.92) compared with 0.80 (0.72–0.89) for the NNE mortality model alone (Table 8). Adding medians (0.88, CI: 0.83–0.94) and terciles (0.88, CI: 0.83–0.93) of all 3 biomarkers increased the c‐statistic relative to the base STS mortality model, and both ROC comparison tests were statistically significant. NRI and IDI calculated indices are listed in Table 9.
Table 8.
Risk Prediction STS Models With Added Biomarkers
| Prediction Modelsb (Model ROC [95% CI]) | |||||||
|---|---|---|---|---|---|---|---|
| STS Model | STS+NT‐Pro BNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.86 (0.80–0.92) | 0.87 (0.82–0.92) | 0.87 (0.81–0.94) | 0.86 (0.80–0.92) | 0.87 (0.82–0.92) | 0.88 (0.83–0.94) | 0.88 (0.83–0.94) |
| P valuea | ··· | 0.176 | 0.301 | 0.409 | 0.158 | 0.048 | 0.041 |
| Tercile | 0.86 (0.80–0.92) | 0.88 (0.83–0.93) | 0.86 (0.80–0.93) | 0.86 (0.80–0.92) | 0.88 (0.83–0.93) | 0.88 (0.83–0.93) | 0.88 (0.83–0.93) |
| P valuea | ··· | 0.136 | 0.580 | 0.740 | 0.135 | 0.039 | 0.042 |
CI indicates confidence interval; Gal3, Galectin‐3; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; STS, Society of Thoracic Surgeons.
P values compare the area under the ROC (receiver operator curve) from the adjusted model to the area under the ROC from the base STS Model.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Table 9.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the STS Base Model, at Median and Tercile Cut Points
| Biomarker Categories | Prediction Modelsa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STS+NT‐Pro BNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.12 | 0.00 | 0.05 | 0.02 | −0.03 | 0.00 | 0.12 | 0.00 | 0.09 | 0.02 | 0.09 | 0.02 |
| P valuea | 0.034 | 0.112 | 0.276 | 0.030 | 0.356 | 0.574 | 0.029 | 0.165 | 0.008 | 0.026 | 0.006 | 0.031 |
| Tercile | 0.10 | 0.01 | 0.04 | 0.01 | 0.00 | 0.01 | 0.10 | 0.01 | 0.07 | 0.02 | 0.07 | 0.02 |
| P Valuea | 0.021 | 0.098 | 0.000 | 0.080 | 0.590 | 0.410 | 0.022 | 0.094 | 0.000 | 0.042 | 0.000 | 0.041 |
CI indicates confidence interval; Gal3, Galectin‐3; IDI, integrated discrimination improvement; NRI, net reclassification improvement; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; STS, Society of Thoracic Surgeons.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Mid‐Term Mortality Models
The NNE mortality model had a lower c‐statistic when evaluated against 1‐year mortality (c‐statistic: 0.70, 95% CI: 0.64–0.77), compared with NNE risk prediction of in‐hospital mortality at discharge. With the addition of tercile values of ST2 and NT‐proBNP, the c‐statistic significantly improved to 0.76 (95% CI: 0.70–0.81; P=0.031). None of the median cut point values for any of the 3 biomarkers yielded a significant improvement at 1‐year mortality after CABG. Table 10 describes these results and Table 11 lists NRI and IDI calculations. When we applied the STS preoperative risk model at 1‐year mortality to our NNE cohort, the prediction model yielded a higher c‐statistic compared with the NNE mortality model (c‐statistic: 0.76 [95% CI: 0.70–0.82]). The addition of ST2 and NT‐proBNP tercile values resulted in a statistically significant improvement from the base model to a c‐statistic of 0.79 (95% CI: 0.74–0.85; P=0.033). When the Galectin‐3 tercile values were added to the model, the discriminatory power did not appreciably change (c statistic: 0.80 [95% CI: 0.74–0.85]; P=0.032). The STS risk prediction model at 1‐year mortality results are listed in Tables 12 and 13.
Table 10.
Risk Prediction Models With Added Biomarkers, Adjusting for the NNE Model, at 1‐Year Mortality
| Prediction Models (Model ROC [95% CI]) | |||||||
|---|---|---|---|---|---|---|---|
| NNE Model | NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.70 (0.64–0.77) | 0.73 (0.67–0.78) | 0.72 (0.66–0.78) | 0.71 (0.64–0.77) | 0.73 (0.67–0.79) | 0.74 (0.69–0.80) | 0.74 (0.69–0.80) |
| P valuea | ··· | 0.183 | 0.261 | 0.692 | 0.159 | 0.078 | 0.056 |
| Tercile | 0.70 (0.64–0.77) | 0.75 (0.70–0.81) | 0.71 (0.65–0.78) | 0.71 (0.64–0.77) | 0.75 (0.70–0.81) | 0.76 (0.70–0.81) | 0.76 (0.70–0.81) |
| P Valuea | ··· | 0.034 | 0.444 | 0.618 | 0.032 | 0.031 | 0.030 |
CI indicates confidence interval; NNE, Northern New England.
P values compare the area under the ROC (receiver operator characteristic) curve from the adjusted model to the area under the ROC curve from the base NNE Model.
Table 11.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the NNE Base Model, at Median and Tercile Cut Points—at 1‐Year Mortality
| Biomarker Categories | Prediction Models (Model ROC [95% CI]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.03 | 0.01 | −0.02 | 0.01 | 0.06 | 0.00 | 0.02 | 0.01 | 0.07 | 0.01 | 0.04 | 0.01 |
| P valuea | 0.543 | 0.002 | 0.597 | 0.005 | 0.084 | 0.165 | 0.750 | 0.002 | 0.204 | 0.000 | 0.474 | 0.000 |
| Tercile | 0.11 | 0.01 | 0.02 | 0.01 | 0.00 | 0.01 | 0.05 | 0.02 | 0.08 | 0.02 | 0.09 | 0.02 |
| P valuea | 0.047 | 0.000 | 0.640 | 0.012 | 0.953 | 0.012 | 0.338 | 0.000 | 0.178 | 0.000 | 0.130 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; IDI, integrated discrimination improvement; NRI, net reclassification improvement NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC, receiver operator characteristic.
P values compare the area under the ROC (receiver operator characteristic) curve from the adjusted model to the area under the ROC curve from the base NNE Model.
Table 12.
Risk Prediction Models With Added Biomarkers, Adjusting for the STS Model, at 1‐Year Mortality
| Prediction Modelsb (Model ROC [95% CI]) | |||||||
|---|---|---|---|---|---|---|---|
| STS Model | STS+NT‐Pro BNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.76 (0.70–0.82) | 0.78 (0.72–0.83) | 0.76 (0.70–0.83) | 0.77 (0.71–0.83) | 0.78 (0.73–0.84) | 0.78 (0.72–0.84) | 0.78 (0.73–0.84) |
| P valuea | ··· | 0.026 | 0.583 | 0.246 | 0.027 | 0.127 | 0.078 |
| Tercile | 0.76 (0.70–0.82) | 0.80 (0.75–0.85) | 0.76 (0.70–0.82) | 0.76 (0.71–0.83) | 0.80 (0.74–0.85) | 0.79 (0.74–0.85) | 0.80 (0.74–0.85) |
| P Valuea | ··· | 0.124 | 0.891 | 0.567 | 0.100 | 0.033 | 0.032 |
CI indicates confidence interval; Gal3, Galectin‐3; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; STS, Society of Thoracic Surgeons.
P values compare the area under the ROC (receiver operator characteristic) curve from the adjusted model to the area under the ROC curve from the base STS Model.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Table 13.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the STS Base Model, at Median and Tercile Cut Points—at 1‐Year Mortality
| Biomarker Categories | Prediction Modelsa (Model ROC [95% CI]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STS+NT‐ProBNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.09 | 0.00 | 0.03 | 0.01 | 0.02 | 0.00 | 0.12 | 0.04 | 0.12 | 0.03 | 0.12 | 0.04 |
| P valuea | 0.053 | 0.037 | 0.218 | 0.011 | 0.573 | 0.437 | 0.000 | 0.000 | 0.001 | 0.000 | 0.001 | 0.000 |
| Tercile | 0.11 | 0.01 | 0.02 | 0.01 | 0.01 | 0.00 | 0.11 | 0.04 | 0.11 | 0.04 | 0.13 | 0.05 |
| P valuea | 0.027 | 0.010 | 0.418 | 0.015 | 0.724 | 0.063 | 0.003 | 0.000 | 0.001 | 0.000 | 0.000 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; IDI, integrated discrimination improvement; NRI, net reclassification improvement; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC; receiver operator characteristic; STS, Society of Thoracic Surgeons.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Tables 14 through describe 5‐year mortality prediction from the NNE and STS models. The findings from the NNE clinical mortality model to predict 5‐year death was similar to those for 1‐year death. The c‐statistic from the model alone (0.67; 95% CI: 0.63–0.71) was lower than for one‐death or in‐hospital death. The additions of preoperative NT‐proBNP median (0.72, CI: 0.69–0.75) and tercile values (0.72, CI: 0.69–0.76) produced the highest c‐statistics of any individual biomarker on this sample; both increases were significant at 95% according to the ROC comparison test. The inclusion of preoperative NT‐proBNP and ST2 medians (0.73, CI: 0.70–0.76) and terciles (0.74, CI: 0.70–0.77) together both yielded higher c‐statistics than from the base NNE clinical model alone (Tables 14 and 15). The results obtained from using the 2008 STS mortality model to predict 5‐year death were similar in all cases to the results obtained using the NNE mortality model (Tables 16 and 17).
Table 14.
Risk Prediction Models With Added Biomarkers, Adjusting for the NNE Model, at 5‐Year Mortality
| Prediction Models (Model ROC [95% CI]) | |||||||
|---|---|---|---|---|---|---|---|
| NNE Model | NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.67 (0.63–0.71) | 0.72 (0.69–0.75) | 0.70 (0.66–0.74) | 0.69 (0.65–0.73) | 0.73 (0.69–0.76) | 0.73 (0.70–0.76) | 0.74 (0.71–0.77) |
| P valuea | ··· | 0.000 | 0.014 | 0.063 | 0.000 | 0.000 | 0.000 |
| Tercile | 0.67 (0.63–0.71) | 0.73 (0.69–0.76) | 0.70 (0.67–0.74) | 0.70 (0.66–0.73) | 0.74 (0.70–0.77) | 0.74 (0.70–0.77) | 0.74 (0.71–0.78) |
| P valuea | ··· | 0.001 | 0.013 | 0.034 | 0.000 | 0.000 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC; receiver operator characteristic.
P values compare the area under the ROC (receiver operator characteristic) curve from the adjusted model to the area under the ROC curve from the base NNE (Northern New England) model.
Table 15.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the NNE Base Model, at Median and Tercile Cut Points—at 5‐Year Mortality
| Biomarker Categories | Prediction Models (Model ROC [95% CI]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NNE+NT‐Pro BNP | NNE+ST2 | NNE+Gal3 | NNE+Gal3+NT‐ProBNP | NNE+ST2+NT‐ProBNP | NNE+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.08 | 0.03 | 0.06 | 0.02 | 0.05 | 0.01 | 0.12 | 0.04 | 0.12 | 0.03 | 0.12 | 0.04 |
| P valuea | 0.042 | 0.000 | 0.050 | 0.000 | 0.138 | 0.000 | 0.000 | 0.000 | 0.001 | 0.000 | 0.001 | 0.000 |
| Tercile | 0.08 | 0.03 | 0.06 | 0.01 | 0.07 | 0.02 | 0.11 | 0.04 | 0.11 | 0.04 | 0.13 | 0.05 |
| P valuea | 0.021 | 0.000 | 0.055 | 0.000 | 0.022 | 0.000 | 0.003 | 0.000 | 0.001 | 0.000 | 0.000 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; IDI, integrated discrimination improvement; NNE; Northern New England; NRI, net reclassification improvement; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC; receiver operator characteristic.
P values compare the area under the ROC (receiver operator characteristic) curve from the adjusted model to the area under the ROC curve from the base NNE (Northern New England) model.
Table 16.
Risk Prediction Models With Added Biomarkers, Adjusting for the STS Model, at 5‐Year Mortality
| Prediction Models (Model ROC [95% CI]) | |||||||
|---|---|---|---|---|---|---|---|
| STS Model | STS+NT‐Pro BNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |
| Median | 0.69 (0.65–0.73) | 0.73 (0.70–0.77) | 0.71 (0.67–0.75) | 0.71 (0.67–0.75) | 0.74 (0.71–0.78) | 0.74 (0.70–0.78) | 0.75 (0.72–0.79) |
| P valuea | ··· | 0.001 | 0.021 | 0.045 | 0.000 | 0.000 | 0.000 |
| Tercile | 0.69 (0.65–0.73) | 0.74 (0.70–0.77) | 0.72 (0.68–0.75) | 0.71 (0.68–0.75) | 0.75 (0.72–0.78) | 0.75 (0.71–0.78) | 0.76 (0.72–0.79) |
| P valuea | ··· | 0.001 | 0.025 | 0.019 | 0.000 | 0.000 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC; receiver operator characteristic; STS, Society of Thoracic Surgeons.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Table 17.
NRI and IDI Indices for Risk Prediction Biomarker Models Compared With the STS Base Model, at Median and Tercile Cut Points—at 5‐Year Mortality
| Biomarker Categories | Prediction Models (Model ROC [95% CI]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STS+NT‐Pro BNP | STS+ST2 | STS+Gal3 | STS+Gal3+NT‐ProBNP | STS+ST2+NT‐ProBNP | STS+ST2+NT‐ProBNP+Gal3 | |||||||
| NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | NRI | IDI | |
| Median | 0.06 | 0.02 | 0.04 | 0.01 | 0.03 | 0.01 | 0.11 | 0.03 | 0.10 | 0.03 | 0.11 | 0.04 |
| P valuea | 0.142 | 0.000 | 0.159 | 0.000 | 0.224 | 0.000 | 0.001 | 0.000 | 0.005 | 0.000 | 0.002 | 0.000 |
| Tercile | 0.08 | 0.03 | 0.03 | 0.02 | 0.03 | 0.02 | 0.10 | 0.04 | 0.07 | 0.04 | 0.12 | 0.05 |
| P valuea | 0.011 | 0.000 | 0.337 | 0.000 | 0.291 | 0.000 | 0.002 | 0.000 | 0.039 | 0.000 | 0.001 | 0.000 |
CI indicates confidence interval; Gal3, Galectin‐3; IDI, integrated discrimination improvement; NRI, net reclassification improvement; NT‐ProBNP, N terminal Pro b‐type natriuretic peptide; ROC; receiver operator characteristic; STS, Society of Thoracic Surgeons.
Model corrects for age, sex, body surface area, atrial fibrillation, last preoperative serum creatinine, presence of diabetes mellitus, ejection fraction <40%, hypertension, preoperative intra‐aortic balloon pump use, prior myocardial infarction, presence of any vascular disease, unstable angina, renal failure, chronic obstructive pulmonary disease, left main stenosis >50%, prior coronary artery bypass graft, prior percutaneous coronary intervention, date of operation, and urgent and emergent priority.
Discussion
In this observational study of regional data, we used a prospective cohort to assess the ability of 3 biomarkers (Galectin‐3, NT‐ProBNP, and ST2) to improve a pre‐existing multivariate prediction model of mortality in CABG patients. We discovered that the addition of the 2 biomarkers resulted in a statistically significant improvement in the predictive ability of the model. Simultaneous addition of NT‐ProBNP and ST2 into the base prediction model of mortality resulted in a greater ROC score when compared with the base, 0.80 versus 0.85, with a significant P‐value of 0.048.
Multi‐marker risk prediction has been sparsely evaluated for preoperative risk prediction in CABG surgery. Prior work aimed at improving the predictive ability of models of risk of in‐hospital mortality after CABG surgery through the addition of 4 biomarkers (cardiac troponin T, NT‐ProBNP, high‐sensitivity C‐reactive protein, and glucose and hemoglobin) to the existing model had found no statistically significant improvement in the model's ability to predict mortality.11 NT‐ProBNP has been shown to predict postoperative survival in patients with aortic stenosis, in‐hospital mortality in patients with heart failure, all‐cause mortality within 30 days of discharge after non‐cardiac surgery, and all‐cause mortality in adults with congenital heart disease.37, 38, 39, 40 Preoperative levels of its sister compound, brain natriuretic peptide (BNP), have been used to predict postoperative mortality in patients undergoing cardiac surgery procedures, including CABG.41, 42 Additionally, studies on patients undergoing isolated CABG found associations between preoperative levels of NT‐ProBNP and postoperative mortality, prompting inclusion of preoperative levels of the biomarker into our models.16, 43, 44
In regards to the other biomarkers in our multi‐marker model, the inclusion of preoperative levels of Galectin‐3 in the model was supported given this biomarkers association with health complications and mortality in patients with heart failure.45, 46 Much work has also been conducted to establish associations between ST2 levels and clinical outcomes before and after cardiovascular procedures in specific populations.47, 48, 49, 50 The individual and combined predictive power of these 3 biomarkers, in addition to boost in predictive ability they have provided to existing preoperative models of mortality and risk in many cardiovascular conditions and procedures, merited their congruent consideration in a multi‐marker model aimed at preoperatively predicting in‐hospital mortality in patients after CABG.51, 52, 53
Though the sole inclusion of any of the 3 biomarkers into our model individually did not show statistically significant improvement in predictive ability, there was a noticeable increase in the ROC score after the inclusion of ST2 and NT‐ProBNP simultaneously. However, though studies that investigated individual biomarkers in our multi‐marker model have found Galectin‐3 to be significantly associated with heart failure and other cardiovascular outcomes, the results of our univariate and multivariate logistic regression analyses suggest that this association does not extend to in‐hospital mortality.
When we compared our model and cohort to the well documented risk prediction methods developed by STS, we observed statistically significant improvement in the discriminating ability with the inclusion of 2 biomarkers compared with the STS clinical base model alone. The addition of median and tercile cut points for NT‐proBNP and ST2 yielded a c‐statistic of 0.88 versus base model of 0.86. The predictive ability did not change with the addition of Galectin‐3. Similar to the NNE risk prediction model findings, the individual inclusion of any of the 3 biomarkers into the STS model did not yield a statistically significant improvement the model.
We were interested to evaluate the predictive ability of our NNE risk models with short and mid‐term mortality after CABG. After applying the NNE preoperative clinical model and STS model to our cohort, we found similar results to the in‐hospital mortality model. We observed significant improvement to the prediction models with the inclusion of median and tercile preoperative values from biomarkers ST2 and NT‐proBNP. The addition of median and tercile Galectin‐3 values, to either the NNE or STS model, did not result in any appreciable difference.
There are limitations to consider. We externally validated our model using a multicenter, mixed cardiovascular disease cohort that includes those undergoing CABG, valve, or CABG and valve surgery who are at high risk of acute kidney injury. The lower validation performance may possibly be attributable to the complexity of the TRIBE‐AKI cohort. An improvement to external validation would be to identify a biorepository with a large sample size of isolated CABG patients.
Our NNE cohort includes the limited number of deaths at discharge and potential risk of over‐fitting. The cohort under study also consisted of a homogeneous population with race not being considered in the prediction score. Future research should conduct similar analyses using a larger sample size. However, our work suggests that current risk prediction models may be improved by inclusion of biomarkers. Future work should aim to investigate the existence and impact of other biomarkers on mortality after CABG.
CABG is the most common open‐heart surgery performed to treat heart disease.54 Our data are from 2004–2007, when the prevalence of heart disease was slightly higher compared with current data (221.6 versus 168.5 age‐adjusted deaths per 100 000 people). While age‐adjusted mortality rates have declined in recent years, heart disease remains the leading cause of death in the United States.54
Conclusion
In summary, the addition of NT‐ProBNP and ST2 to the risk prediction model significantly improved the preoperative prediction of in‐hospital mortality over patient characteristics and risk factors alone. The use of preoperative biomarkers may have clinical utility in identifying patients at greater risk of mortality after cardiac surgery.
Sources of Funding
This research is supported by the National Heart, Lung, and Blood Institute R01HL119664 (PI: Brown). All authors are research staff or investigators on the grant. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long‐Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Disclosures
None.
(J Am Heart Assoc. 2018;7:e008371 DOI: 10.1161/JAHA.117.008371.)
References
- 1. Califf RM, Phillips HR III, Hindman MC, Mark DB, Lee KL, Behar VS, Johnson RA, Pryor DB, Rosati RA, Wagner GS, Harrell FE Jr. Prognostic value of a coronary artery jeopardy score. J Am Coll Cardiol. 1985;5:1055–1063. [DOI] [PubMed] [Google Scholar]
- 2. Clark RE, Edwards FH, Schwartz M. Profile of preoperative characteristics of patients having CABG over the past decade. Ann Thorac Surg. 1994;58:1863–1865. [DOI] [PubMed] [Google Scholar]
- 3. Doliszny KM, Luepker RV, Burke GL, Pryor DB, Blackburn H. Estimated contribution of coronary artery bypass graft surgery to the decline in coronary heart disease mortality: the Minnesota Heart Survey. J Am Coll Cardiol. 1994;24:95–103. [DOI] [PubMed] [Google Scholar]
- 4. Grover FL, Johnson RR, Marshall G, Hammermeister KE. Factors predictive of operative mortality among coronary artery bypass subsets. Ann Thorac Surg. 1993;56:1296–1306; discussion 1306‐1297. [DOI] [PubMed] [Google Scholar]
- 5. Hannan EL, Kilburn H Jr, O'Donnell JF, Lukacik G, Shields EP. Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA. 1990;264:2768–2774. [PubMed] [Google Scholar]
- 6. Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992;267:2344–2348. [PubMed] [Google Scholar]
- 7. O'Connor GT, Plume SK, Olmstead EM, Coffin LH, Morton JR, Maloney CT, Nowicki ER, Levy DG, Tryzelaar JF, Hernandez F. Multivariate prediction of in‐hospital mortality associated with coronary artery bypass graft surgery. Northern New England Cardiovascular Disease Study Group. Circulation. 1992;85:2110–2118. [DOI] [PubMed] [Google Scholar]
- 8. Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79:I3–I12. [PubMed] [Google Scholar]
- 9. Jones RH, Hannan EL, Hammermeister KE, Delong ER, O'Connor GT, Luepker RV, Parsonnet V, Pryor DB. Identification of preoperative variables needed for risk adjustment of short‐term mortality after coronary artery bypass graft surgery. The Working Group Panel on the Cooperative CABG Database Project. J Am Coll Cardiol. 1996;28:1478–1487. [DOI] [PubMed] [Google Scholar]
- 10. Peterson ED, DeLong ER, Muhlbaier LH, Rosen AB, Buell HE, Kiefe CI, Kresowik TF. Challenges in comparing risk‐adjusted bypass surgery mortality results: results from the Cooperative Cardiovascular Project. J Am Coll Cardiol. 2000;36:2174–2184. [DOI] [PubMed] [Google Scholar]
- 11. Brown JR, MacKenzie TA, Dacey LJ, Leavitt BJ, Braxton JH, Westbrook BM, Helm RE, Klemperer JD, Frumiento C, Sardella GL, Ross CS, O'Connor GT. Using biomarkers to improve the preoperative prediction of death in coronary artery bypass graft patients. J Extra Corpor Technol. 2010;42:293–300. [PMC free article] [PubMed] [Google Scholar]
- 12. Parolari A, Poggio P, Myasoedova V, Songia P, Bonalumi G, Pilozzi A, Pacini D, Alamanni F, Tremoli E. Biomarkers in coronary artery bypass surgery: ready for prime time and outcome prediction? Front Cardiovasc Med. 2015;2:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhalla V, Willis S, Maisel AS. B‐type natriuretic peptide: the level and the drug—partners in the diagnosis of congestive heart failure. Congest Heart Fail. 2004;10:3–27. [DOI] [PubMed] [Google Scholar]
- 14. May HT, Horne BD, Levy WC, Kfoury AG, Rasmusson KD, Linker DT, Mozaffarian D, Anderson JL, Renlund DG. Validation of the Seattle Heart Failure Model in a community‐based heart failure population and enhancement by adding B‐type natriuretic peptide. Am J Cardiol. 2007;100:697–700. [DOI] [PubMed] [Google Scholar]
- 15. Pedrazzini GB, Masson S, Latini R, Klersy C, Rossi MG, Pasotti E, Faletra FF, Siclari F, Minervini F, Moccetti T, Auricchio A. Comparison of brain natriuretic peptide plasma levels versus logistic EuroSCORE in predicting in‐hospital and late postoperative mortality in patients undergoing aortic valve replacement for symptomatic aortic stenosis. Am J Cardiol. 2008;102:749–754. [DOI] [PubMed] [Google Scholar]
- 16. Schachner T, Wiedemann D, Fetz H, Laufer G, Kocher A, Bonaros N. Influence of preoperative serum N‐terminal pro‐brain type natriuretic peptide on the postoperative outcome and survival rates of coronary artery bypass patients. Clinics (Sao Paulo). 2010;65:1239–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bayes‐Genis A, Pascual‐Figal D, Januzzi JL, Maisel A, Casas T, Valdes Chavarri M, Ordonez‐Llanos J. Soluble ST2 monitoring provides additional risk stratification for outpatients with decompensated heart failure. Rev Esp Cardiol. 2010;63:1171–1178. [DOI] [PubMed] [Google Scholar]
- 18. Dumic J, Dabelic S, Flogel M. Galectin‐3: an open‐ended story. Biochem Biophys Acta. 2006;1760:616–635. [DOI] [PubMed] [Google Scholar]
- 19. Ky B, French B, McCloskey K, Rame JE, McIntosh E, Shahi P, Dries DL, Tang WH, Wu AH, Fang JC, Boxer R, Sweitzer NK, Levy WC, Goldberg LR, Jessup M, Cappola TP. High‐sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail. 2011;4:180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lok DJA, Van Der Meer P, de la Porte P, Lipsic E, Van Wijngaarden J, Hillege HL, van Veldhuisen DJ. Prognostic value of galectin‐3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL‐HF study. Clin Res Cardiol. 2010;99:323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rehman SU, Mueller T, Januzzi JL Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol. 2008;52:1458–1465. [DOI] [PubMed] [Google Scholar]
- 22. van Kimmenade RR, Januzzi JL Jr, Ellinor PT, Sharma UC, Bakker JA, Low AF, Martinez A, Crijns HJ, MacRae CA, Menheere PP, Pinto YM. Utility of amino‐terminal pro‐brain natriuretic peptide, galectin‐3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol. 2006;48:1217–1224. [DOI] [PubMed] [Google Scholar]
- 23. Ho JE, Liu C, Lyass A, Courchesne P, Pencina MJ, Vasan RS, Larson MG, Levy D. Galectin‐3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J Am Coll Cardiol. 2012;60:1249–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Andersson C, Enserro D, Sullivan L, Wang TJ, Januzzi JL Jr, Benjamin EJ, Vita JA, Hamburg NM, Larson MG, Mitchell GF, Vasan RS. Relations of circulating GDF‐15, soluble ST2, and troponin‐I concentrations with vascular function in the community: the Framingham Heart Study. Atherosclerosis. 2016;248:245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang TJ, Wollert KC, Larson MG, Coglianese E, McCabe EL, Cheng S, Ho JE, Fradley MG, Ghorbani A, Xanthakis V, Kempf T, Benjamin EJ, Levy D, Vasan RS, Januzzi JL. Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham Heart Study. Circulation. 2012;126:1596–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, Lytle BW, Marlow RA, Nugent WC, Orszulak TA, Antman EM, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, Ornato JP. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation. 2004;110:1168–1176. [DOI] [PubMed] [Google Scholar]
- 27. Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, Gott JP, Herrmann HC, Marlow RA, Nugent W, O'Connor GT, Orszulak TA, Rieselbach RE, Winters WL, Yusuf S, Gibbons RJ, Alpert JS, Garson A Jr, Gregoratos G, Russell RO, Ryan TJ, Smith SC Jr. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1991 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation. 1999;100:1464–1480. [DOI] [PubMed] [Google Scholar]
- 28. Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, Gott JP, Herrmann HC, Marlow RA, Nugent WC, O'Connor GT, Orszulak TA, Rieselbach RE, Winters WL, Yusuf S, Gibbons RJ, Alpert JS, Eagle KA, Garson A Jr, Gregoratos G, Russell RO, Smith SC Jr. ACC/AHA guidelines for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1991 Guidelines for Coronary Artery Bypass Graft Surgery). American College of Cardiology/American Heart Association. J Am Coll Cardiol. 1999;34:1262–1347. [DOI] [PubMed] [Google Scholar]
- 29. O'Connor GT, Plume SK, Olmstead EM, Coffin LH, Morton JR, Maloney CT, Nowicki ER, Tryzelaar JF, Hernandez F, Adrian L, Casey KJ, Soule DN, Marrin CA, Nugent WC, Charlesworth DC, Clough RA, Katz S, Leavitt BJ, Wennberg JE. A regional prospective study of in‐hospital mortality associated with coronary artery bypass grafting. The Northern New England Cardiovascular Disease Study Group. JAMA. 1991;266:803–809. [PubMed] [Google Scholar]
- 30. Surgenor SD, O'Connor GT, Lahey SJ, Quinn R, Charlesworth DC, Dacey LJ, Clough RA, Leavitt BJ, Defoe GR, Fillinger M, Nugent WC. Predicting the risk of death from heart failure after coronary artery bypass graft surgery. Anesth Analg. 2001;92:596–601. [DOI] [PubMed] [Google Scholar]
- 31. Dacey LJ, DeSimone J, Braxton JH, Leavitt BJ, Lahey SJ, Klemperer JD, Westbrook BM, Olmstead EM, O'Connor GT. Preoperative white blood cell count and mortality and morbidity after coronary artery bypass grafting. Ann Thorac Surg. 2003;76:760–764. [DOI] [PubMed] [Google Scholar]
- 32. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. [DOI] [PubMed] [Google Scholar]
- 33. Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP; Society of Thoracic Surgeons Quality Measurement Task F . The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1—coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:S2–S22. [DOI] [PubMed] [Google Scholar]
- 34. Parikh CR, Coca SG, Thiessen‐Philbrook H, Shlipak MG, Koyner JL, Wang Z, Edelstein CL, Devarajan P, Patel UD, Zappitelli M, Krawczeski CD, Passik CS, Swaminathan M, Garg AX. Postoperative biomarkers predict acute kidney injury and poor outcomes after adult cardiac surgery. J Am Soc Nephrol. 2011;22:1748–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Coca SG, Garg AX, Thiessen‐Philbrook H, Koyner JL, Patel UD, Krumholz HM, Shlipak MG, Parikh CR. Urinary biomarkers of AKI and mortality 3 years after cardiac surgery. J Am Soc Nephrol. 2014;25:1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Parikh CR, Puthumana J, Shlipak MG, Koyner JL, Thiessen‐Philbrook H, McArthur E, Kerr K, Kavsak P, Whitlock RP, Garg AX, Coca SG. Relationship of kidney injury biomarkers with long‐term cardiovascular outcomes after cardiac surgery. J Am Soc Nephrol. 2017;28:3699–3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bergler‐Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G, Gabriel H, Binder T, Pacher R, Maurer G, Baumgartner H. Natriuretic peptides predict symptom‐free survival and postoperative outcome in severe aortic stenosis. Circulation. 2004;109:2302–2308. [DOI] [PubMed] [Google Scholar]
- 38. Huang YT, Tseng YT, Chu TW, Chen J, Lai MY, Tang WR, Shiao CC. Corrigendum: N‐terminal pro B‐type natriuretic peptide (NT‐pro‐BNP) ‐based score can predict in‐hospital mortality in patients with heart failure. Sci Rep. 2017;7:46866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Popelova JR, Kotaska K, Tomkova M, Tomek J. Usefulness of N‐terminal pro‐brain natriuretic peptide to predict mortality in adults with congenital heart disease. Am J Cardiol. 2015;116:1425–1430. [DOI] [PubMed] [Google Scholar]
- 40. Alvarez Zurro C, Planas Roca A, Alday Munoz E, Vega Piris L, Ramasco Rueda F, Mendez Hernandez R. High levels of preoperative and postoperative N terminal B‐type natriuretic propeptide influence mortality and cardiovascular complications after noncardiac surgery: a prospective cohort study. Eur J Anaesthesiol. 2016;33:444–449. [DOI] [PubMed] [Google Scholar]
- 41. Berendes E, Schmidt C, Van Aken H, Hartlage MG, Rothenburger M, Wirtz S, Scheld HH, Brodner G, Walter M. A‐type and B‐type natriuretic peptides in cardiac surgical procedures. Anesth Analg. 2004;98:11–19, table of contents. [DOI] [PubMed] [Google Scholar]
- 42. Murad Junior JA, Nakazone MA, Machado Mde N, Godoy MF. Predictors of mortality in cardiac surgery: brain natriuretic peptide type B. Rev Bras Cir Cardiovasc. 2015;30:182–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Holm J, Vidlund M, Vanky F, Friberg O, Hakanson E, Svedjeholm R. Preoperative NT‐proBNP independently predicts outcome in patients with acute coronary syndrome undergoing CABG. Scand Cardiovasc J Suppl. 2013;47:28–35. [DOI] [PubMed] [Google Scholar]
- 44. Rothenburger M, Stypmann J, Bruch C, Wichter T, Hoppe M, Drees G, Berendes E, Huelsken G, Loeher A, Welp H, Rottger C, Schmid C, Scheld HH, Tjan TD. Aminoterminal B‐type pro‐natriuretic peptide as a marker of recovery after high‐risk coronary artery bypass grafting in patients with ischemic heart disease and severe impaired left ventricular function. J Heart Lung Transplant. 2006;25:596–602. [DOI] [PubMed] [Google Scholar]
- 45. Meijers WC, van der Velde AR, de Boer RA. ST2 and galectin‐3: ready for prime time? EJIFCC. 2016;27:238–252. [PMC free article] [PubMed] [Google Scholar]
- 46. Sygitowicz G, Tomaniak M, Filipiak KJ, Koltowski L, Sitkiewicz D. Galectin‐3 in patients with acute heart failure: preliminary report on first polish experience. Adv Clin Exp Med. 2016;25:617–623. [DOI] [PubMed] [Google Scholar]
- 47. Dupuy AM, Curinier C, Kuster N, Huet F, Leclercq F, Davy JM, Cristol JP, Roubille F. Multi‐marker strategy in heart failure: combination of ST2 and CRP predicts poor outcome. PLoS One. 2016;11:e0157159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parikh RH, Seliger SL, Christenson R, Gottdiener JS, Psaty BM, deFilippi CR. Soluble ST2 for prediction of heart failure and cardiovascular death in an elderly, community‐dwelling population. J Am Heart Assoc. 2016;5:e003188 DOI: 10.1161/JAHA.115.003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Szerafin T, Brunner M, Horvath A, Szentgyorgyi L, Moser B, Boltz‐Nitulescu G, Peterffy A, Hoetzenecker K, Steinlechner B, Wolner E, Ankersmit HJ. Soluble ST2 protein in cardiac surgery: a possible negative feedback loop to prevent uncontrolled inflammatory reactions. Clin Lab. 2005;51:657–663. [PubMed] [Google Scholar]
- 50. Willems S, Sels JW, Flier S, Versteeg D, Buhre WF, de Kleijn DP, Hoefer IE, Pasterkamp G. Temporal changes of soluble ST2 after cardiovascular interventions. Eur J Clin Invest. 2013;43:113–120. [DOI] [PubMed] [Google Scholar]
- 51. Meijers WC, de Boer RA, van Veldhuisen DJ, Jaarsma T, Hillege HL, Maisel AS, Di Somma S, Voors AA, Peacock WF. Biomarkers and low risk in heart failure. Data from COACH and TRIUMPH. Eur J Heart Fail. 2015;17:1271–1282. [DOI] [PubMed] [Google Scholar]
- 52. Richards AM, Di Somma S, Mueller T. ST2 in stable and unstable ischemic heart diseases. Am J Cardiol. 2015;115:48b–58b. [DOI] [PubMed] [Google Scholar]
- 53. Wang CH, Yang NI, Liu MH, Hsu KH, Kuo LT. Estimating systemic fibrosis by combining galectin‐3 and ST2 provides powerful risk stratification value for patients after acute decompensated heart failure. Cardiol J. 2016;23:563–572. [DOI] [PubMed] [Google Scholar]
- 54. Health, United States, 2016: With Chartbook on Long‐Term Trends in Health. Hyattsville, MD: Center for Health Statistics; 2017. [PubMed] [Google Scholar]


