Abstract
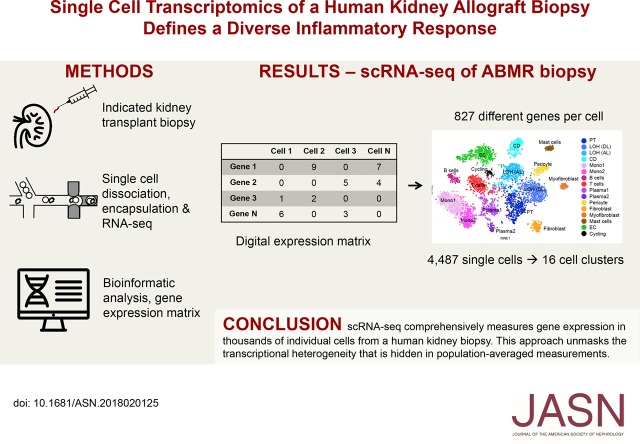
Background Single-cell genomics techniques are revolutionizing our ability to characterize complex tissues. By contrast, the techniques used to analyze renal biopsy specimens have changed little over several decades. We tested the hypothesis that single-cell RNA-sequencing can comprehensively describe cell types and states in a human kidney biopsy specimen.
Methods We generated 8746 single-cell transcriptomes from a healthy adult kidney and a single kidney transplant biopsy core by single-cell RNA-sequencing. Unsupervised clustering analysis of the biopsy specimen was performed to identify 16 distinct cell types, including all of the major immune cell types and most native kidney cell types, in this biopsy specimen, for which the histologic read was mixed rejection.
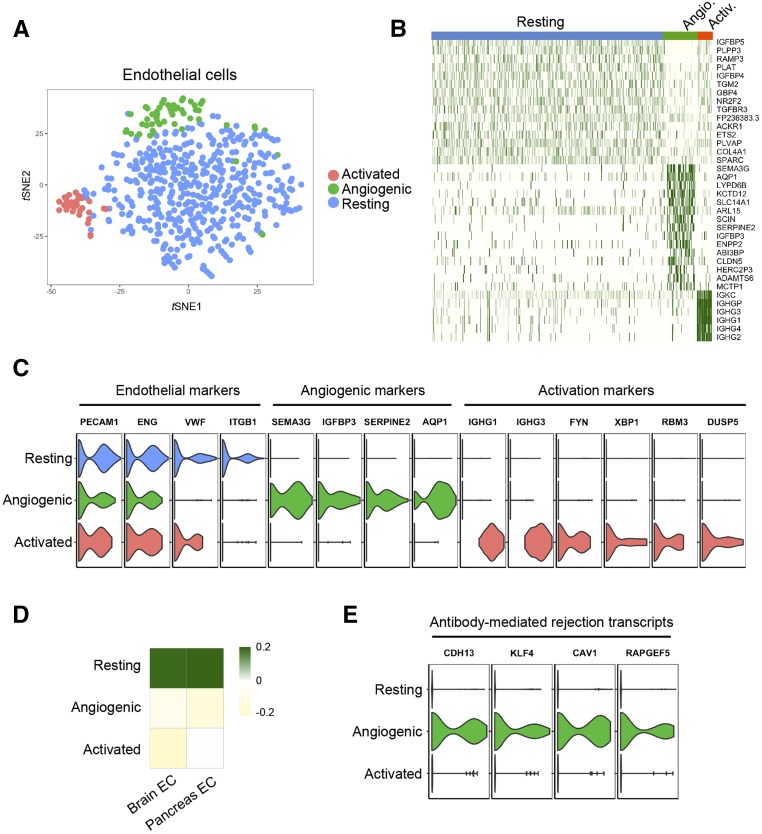
Results Monocytes formed two subclusters representing a nonclassical CD16+ group and a classic CD16− group expressing dendritic cell maturation markers. The presence of both monocyte cell subtypes was validated by staining of independent transplant biopsy specimens. Comparison of healthy kidney epithelial transcriptomes with biopsy specimen counterparts identified novel segment-specific proinflammatory responses in rejection. Endothelial cells formed three distinct subclusters: resting cells and two activated endothelial cell groups. One activated endothelial cell group expressed Fc receptor pathway activation and Ig internalization genes, consistent with the pathologic diagnosis of antibody-mediated rejection. We mapped previously defined genes that associate with rejection outcomes to single cell types and generated a searchable online gene expression database.
Conclusions We present the first step toward incorporation of single-cell transcriptomics into kidney biopsy specimen interpretation, describe a heterogeneous immune response in mixed rejection, and provide a searchable resource for the scientific community.
Keywords: kidney biopsy, rejection, transcriptional profiling
The renal biopsy provides critical diagnostic and prognostic information, but interpretation rests on a limited number of techniques perfected decades ago. With few exceptions, there have been no substantive changes in the way that biopsies are read in 25 years. Recent techniques for massively parallel single-cell RNA-sequencing (scRNA-seq) have been developed, in which the expression of thousands of genes in thousands of individual cells can be measured rapidly, simultaneously, and quantitatively. These approaches offer an unprecedented opportunity to define cell types and states comprehensively with molecular precision. Several international efforts, including the Kidney Precision Medicine Project, are underway using these strategies and other tissue interrogation strategies to generate kidney cellular expression atlases in health and disease. Recently, the first comprehensive mouse scRNA-seq dataset was published.1
Hurdles limit application of scRNA-seq to human kidney biopsies.2 Tissue availability is unpredictable, requiring access to equipment, such as fluorescence-activated sorting machines, with little notice. Additionally, the kidney biopsy consists of a very small sample of about 10×2 mm, but low-input samples pose challenges in scRNA-seq, which relies on double-Poisson loading of cells and oligobearing beads, leading to loss of 95% of cellular input, for example, with the DropSeq approach. Despite these limitations, we hypothesized that scRNA-seq can be successfully applied to a single human kidney biopsy and that doing so would reveal novel insights about disease pathogenesis. Successful application of scRNA-seq to human biopsies will enable evaluation of this powerful tool as an adjunct to traditional renal biopsy interpretation.
We chose to focus on renal allograft biopsies, because a substantial body of data has already established bulk transcriptional profiling to be predictive of outcomes in transplantation. These analyses, however, are limited, because population-averaged measurements mask single-cell transcriptomic heterogeneity, particularly with rare cell types. Moreover, rejection in all of its forms involves the complex interaction of many different immune and parenchymal cells. scRNA-seq is uniquely well suited to dissecting a complex tissue into multiple cellular subpopulations, because it can be easily scaled to tens of thousands of cells. Longitudinal clinicopathologic studies, such as the DeKAF Study, and bulk transcriptional analysis using microarrays suggest that antibody-mediated immune injury is the most common driver of late allograft loss.3–5 Our understanding of the molecular and cellular mechanisms of rejection, in particular, antibody-mediated rejection (ABMR), is poor. Analyses of allograft biopsy transcriptional profiles by microarray have classified patterns of gene expression that can define the different clinical phenotypes of allograft rejection6,7 or predict the development of IFTA using biopsy tissue.8,9 From these studies, a large number of genes have been described that play a role in allograft rejection and failure. Whether resolution of these bulk transcriptional profiles to individual cell types might improve our understanding of rejection or provide for better disease subclassification is unknown.
In this study, we present the first scRNA-seq analysis of a single human kidney allograft biopsy. We used unsupervised computational approaches to identify 16 different cell types and novel cell states within endothelium. We compared tubular cell transcriptomes with healthy adult kidney and thereby, identified proinflammatory parenchymal responses in the rejecting kidney. We mapped genes with expression that is known to associate with allograft pathologies to specific kidney cell types, in many cases finding expression in unexpected cells. Our data prove the feasibility of applying comprehensive scRNA-seq to human kidney biopsies and identify complex immune cell infiltrates and proinflammatory parenchymal responses.
Methods
Clinical Sample
The patient described in this study consented under the Washington University Kidney Translational Research Core (WUKTRC) Institutional Review Board protocol (identification 201102312). The donor and recipient HLA haplotypes, the clinical biopsy Banff scores, and follow-up clinical outcome data were received in a deidentified manner through the WUKTRC. The healthy kidney tissue was from a discarded human donor kidney where donor anonymity was preserved. The donor was a 70-year-old white man with a serum creatinine of 1.1 mg/dl.
Tissue Processing and Single-Cell Dissociation
The renal biopsy was minced into small pieces with a razor blade and incubated at 37°C in freshly prepared dissociation buffer containing 0.25% trypsin and 40 U/ml DNase I. Dissociated cells were harvested every 10 minutes by filtering the cell suspension through a 70-μm cell strainer (pluriSelect) into 10% FBS buffer on ice. The residual biopsy tissue trapped on the cell strainer was dissociated once again with 1 ml dissociation buffer for 10 minutes and passed through the cell strainer into the same FBS buffer from the first collection. We repeated this dissociation procedure three times until most of the tissue had been dissociated into single cells (total dissociation time was 30 minutes). Finally, cells were collected by centrifugation at 400×g for 5 minutes, resuspended in inDrops cell suspension buffer (9% Optiprep), and strained through a 40-μm cell mesh (pluriSelect) to further remove cell clumps and large fragments. Cell viability was approximately 90% for the biopsy used in this study as assessed by Trypan Blue staining.
Single-Cell and Single-Nucleus InDrops and Bioinformatic Analysis
Information is in Supplemental Material.
Data Availability
All relevant data have been deposited in the Gene Expression Omnibus under accession numbers GSE109564 and GSE114156.
Results
A clinically indicated kidney allograft biopsy was performed on a 21-year-old white man with ESRD secondary to hemolytic uremic syndrome. He received a deceased donor kidney transplant 2 years prior (HLA mismatch 1A, 2B, 1DR) with thymoglobulin induction (Supplemental Table 1). At the time of the biopsy, his creatinine was 6.1 mg/dl, and it had increased from a baseline of 1.2 mg/dl 4 months prior. Maintenance immunosuppression was tacrolimus (trough levels 4–8 ng/ml), mycophenolic acid, and prednisone. He failed to get laboratory testing in the 4 months before biopsy, raising suspicion of medication noncompliance.
The histologic diagnosis was acute T cell–mediated rejection with plasma cells graded Banff 1B and acute C4d-negative ABMR (Figure 1A, Supplemental Table 2). Donor-specific antibodies (DSAs) were positive at the time of biopsy (Supplemental Table 3). Treatment consisted of high-dose corticosteroids (750 mg methylprednisone), thymoglobulin (3.5 mg/kg), IVIG (1 g/kg), and rituximab (200 mg). Allograft function did not improve, and he returned to dialysis 2 months later.
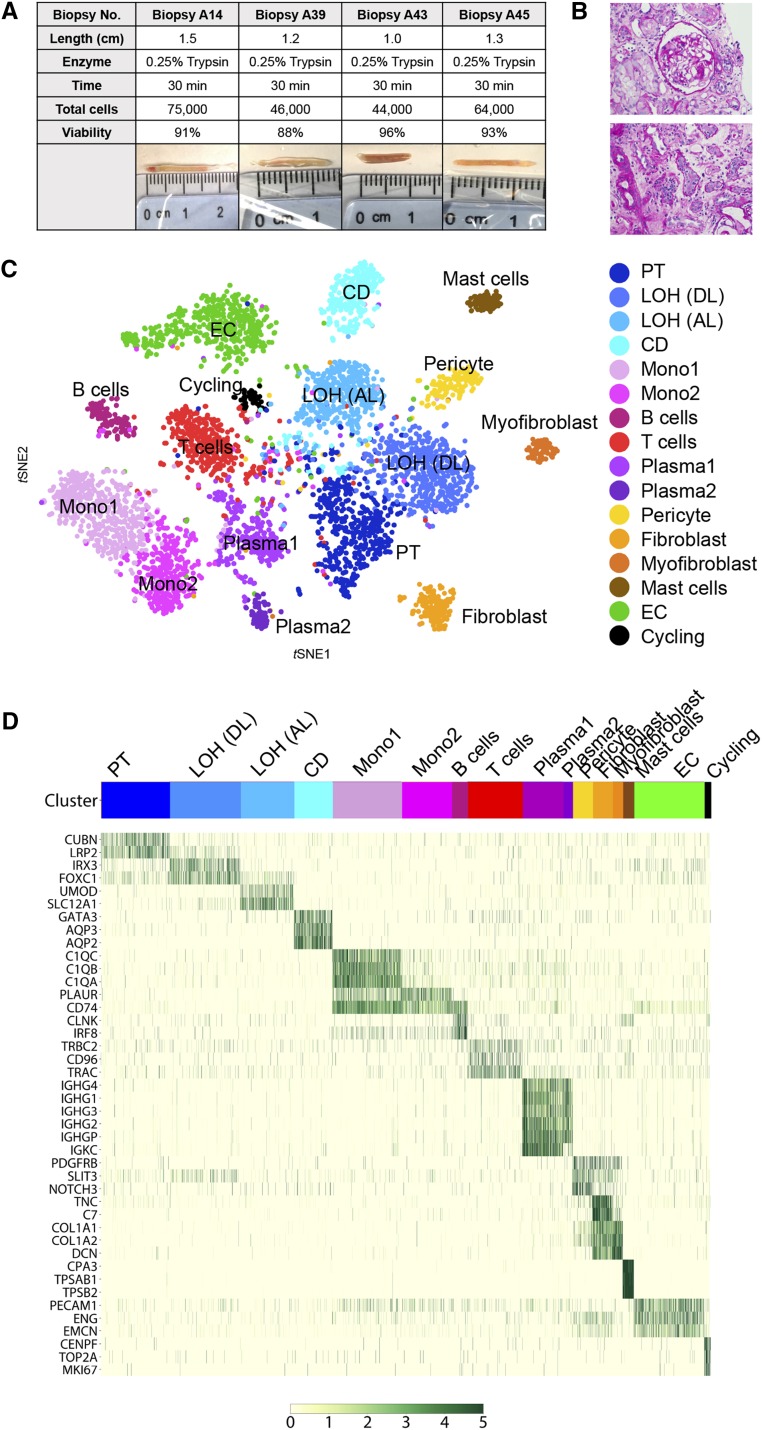
Figure 1.
Comprehensive single-cell RNA-sequencing of an allograft biopsy reveals diverse kidney and immune cell types. (A) Four 16-mm biopsy cores were subjected to cell dissociation. Cell yield varied between 44,000 and 75,000 cells, and viability was 88%–96%. (B) Biopsy A14 was used for single-cell RNA-sequencing, and periodic acid–Schiff staining revealed diffuse inflammatory infiltrates. (C) tSNE plot of cell clusters identified on the basis of the expression of highly variable genes. (D) Heat map of all cells clustered by recursive hierarchical clustering and Louvain–Jaccard clustering (Seurat) showing selected marker genes for each population. CD, collecting duct; EC, endothelial cell; LOH (AL), loop of Henle, ascending limb; LOH (DL), loop of Henle, distal limb; Mono, monocyte; PT, proximal tubule; tSNE, t-Distributed Stochastic Neighbor Embedding.
scRNA-seq Identifies Kidney Allograft Biopsy Cell Types
In preliminary experiments, we used a 30-minute 0.25% trypsin cell dissociation procedure to compare the cell yield and viability from four human kidney biopsies. Biopsy length ranged from 10 to 15 mm, cell yield ranged from 44,000 to 75,000 cells, and viability was between 88% and 96% (Figure 1A). We next assessed the ability of two common droplet-based techniques, DropSeq10 and inDrops,11 to generate single-cell transcriptomes from human kidney (Supplemental Figure 1). We consistently failed to generate libraries using DropSeq lysis buffer and beads, but we were successful using inDrops reagents (Supplemental Figure 1B). Of note, the DropSeq lysis buffer includes the detergent sarcosyl, whereas the inDrops lysis buffer includes NP40, suggesting the possibility that incomplete cell lysis might explain our failure to generate libraries using DropSeq.
We enzymatically dissociated one 16G biopsy core (Figure 1B) into a single-cell suspension, performed droplet-based microfluidic cell separation using InDrops, generated libraries, and sequenced the cells to a read depth of approximately 50,000 reads per cell. A total of 4487 cells passed our quality filters. We detected, on average, 1481 transcripts from 827 different genes per cell. Unsupervised clustering analysis using Seurat identified 16 distinct cell clusters (Figure 1C). A similar number of unique clusters were identified using an independent clustering approach12 (Supplemental Figure 2). We confirmed that there was no batch effect by projecting the cells from different tubes onto the same tSNE (Supplemental Figure 3).
We annotated clusters on the basis of anchor gene expression and the literature. We independently validated the clusters by computing Pearson correlation on averaged expression profiles derived from a recently generated mouse P1 kidney scRNA-seq dataset and a PBMC dataset from a healthy donor (http://support.10xgenomics.com/single-cell/datasets) (Figure 2A, Supplemental Figure 4A).13 We could, therefore, confidently annotate four tubular cell types (38.0%), three leukocyte populations (21.4%), four types of lymphocytes (19.8%), three stromal cell types (8.2%), endothelial cells (ECs; 11.5%), and an actively proliferating cell population (1.1%) (Supplemental Figure 4B). The expression of unique marker genes in each cell population confirmed the robustness of our cell type classification approach (Figure 1D). Full lists of differentially expressed genes in each cluster are provided in Supplemental Table 4. A searchable database for this dataset, including gene expression projected onto the tSNE diagram, is available at http://humphreyslab.com/SingleCell/.
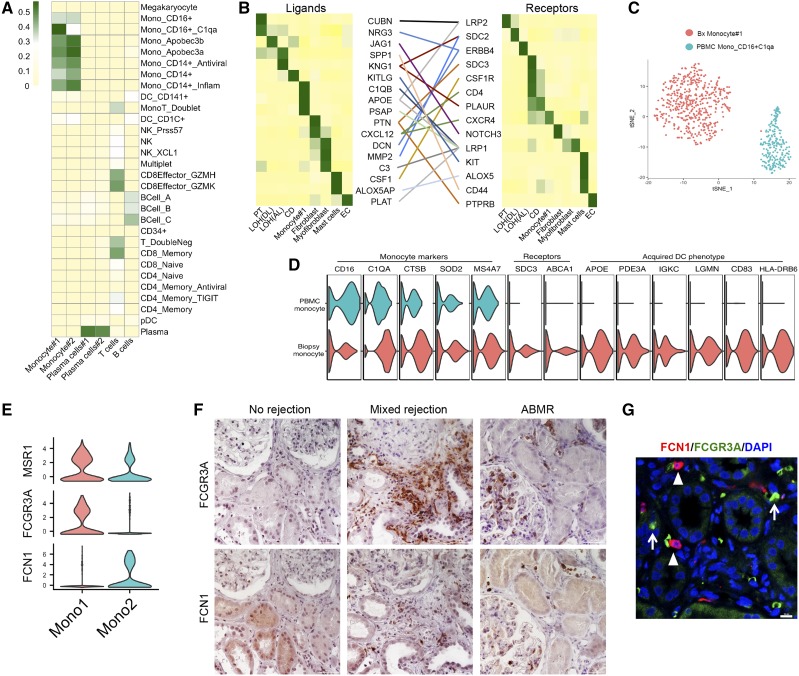
Figure 2.
Annotation of leukocyte subsets. (A) Heat map indicating Pearson correlations of the averaged transcriptional profiles between human PBMCs and leukocyte clusters from the kidney biopsy. (B) Ligand-receptor pair expression according to cell type. Ligands are indicated in the left panel, and receptors are indicated in the right panel. Straight lines indicate ligand-receptor pairs. (C) The biopsy monocyte 1 cluster is most similar to CD16+ peripheral blood monocytes on the basis of average expression; however, these cells form different clusters on the basis of tSNE, indicating that they are different cell types. (D) The monocyte 1 cluster is differentiating toward an acquired dendritic cell phenotype on the basis of expression of marker genes. (E) Violin plot showing that FCGR3A (CD16) distinguishes monocyte 1 from monocyte 2, whereas FCN1 is expressed in monocyte 2 but not monocyte 1. MSR1 is expressed in both clusters. (F) Immunohistochemistry for FCGR3A or FCN1 on normal, mixed rejected, or pure antibody-mediated rejection (ABMR) transplant kidney biopsies. Distinct monocyte 1 and 2 cell types can be seen. Upper and lower panels are serial sections. Scale bar, 50 μm. (G) Immunofluorescence analysis of mixed rejection. FCN1+ cells (arrowheads) and FCGR3A+ cells (arrows) are separate cell types. CD, collecting duct; DAPI, 4′,6-diamidino-2-phenylindole; EC, endothelial cell; LOH (AL), loop of Henle, ascending limb; LOH (DL), loop of Henle, distal limb; Mono, monocyte; PT, proximal tubule. Scale bar, 10 μm.
Comparative Analysis Reveals Monocyte Cell-State Transition and Cell-Cell Interactions between Many Cell Types
Monocyte infiltration is quantitatively associated with kidney dysfunction during allograft rejection.14,15 By mapping our dataset to a published single-cell PBMC dataset,16 we identified two distinct monocyte clusters (Figure 2A). Monocyte 1 strongly expressed FCGR3A (CD16) and was most similar to CD16-positive, proinflammatory, nonclassic monocytes.17 Of note, CD16++ cells are strongly associated with allograft rejection.18,19
Monocyte 2 seems to be a classic or intermediate monocyte population (Figure 2A, Supplemental Table 4). Interestingly, ABCA1, which mediates sterol efflux in activated dendritic cells (DCs),20,21 was uniquely detected in monocyte 1 (Figure 2D), likely indicating a phenotypic transition toward a DC fate by monocytes in allograft rejection. In support of this interpretation, direct comparison of monocyte 1 with the mono_CD16+_C1qa cluster from the PBMC dataset revealed a clear separation of monocyte 1 and the PBMC monocytes, although they were highly correlated on the basis of averaged expression (Figure 2C). Although both cells clusters expressed typical monocyte markers (Figure 2D), monocyte 1 from the biopsy dataset highly expressed two receptors (SDC3 and ABCA1) (Figure 2D) and a panel of DC maturation markers, including APOE,22 PDE3A, IGKC,23 LGMN, and iCD83,24 suggesting differentiation into DC in situ (Figure 2D).
We identified unique marker genes for each monocyte cluster (Figure 2E) and performed immunohistochemistry on independent transplant biopsies, with histologic diagnoses of no disease, mixed rejection, or ABMR. There was sparse interstitial staining for both the monocyte 1 marker (FCGR3A or CD16) and the monocyte 2 marker (FCN1) in biopsies with no disease. By contrast, there was strong staining for both monocyte subsets in mixed rejection, with lesser infiltration in pure ABMR (Figure 2F, Supplemental Figure 5). Costaining by immunofluorescence analysis confirmed that the monocyte subtypes are separate populations (Figure 2G). The presence of these monocyte subsets in all six independent biopsies with mixed rejection or ABMR validates the use of scRNA-seq to identify novel cell types associated with kidney rejection.
Ligand-receptor analysis revealed expression of 14 receptors (excluding collagens) for which we could detect expression of their cognate ligands (Figure 2B). These ligands were detected in all cell types, emphasizing the integration of signals between multiple kidney and leukocyte cell types. Pericytes, fibroblasts, and myofibroblasts expressed the chemoki CXCL12, which promotes lymphocyte and monocyte chemotaxis through its cognate receptor CXCR4, which itself is expressed in T cells, monocytes, and mast cells in our dataset. Further evidence for parenchymal cell regulation of the inflammatory response comes from the observation that collecting duct epithelia express KITLG, also known as stem cell factor, which binds the transmembrane receptor encoded by KIT and is expressed on mast cells in the biopsy (Figure 2B).25 Stem cell factor promotes mast cell migration, adhesion, proliferation, and survival. Mast cells transcripts correlate strongly with allograft biopsy fibrosis.26 These results suggest the unexpected hypothesis that collecting duct epithelia actively coordinate mast cell infiltration during rejection. Consistent with an important role for mast cells in kidney injury, a recent study showed that mast cell ablation in the early phases of renal injury is sufficient to reduce subsequent fibrosis by decreasing the inflammatory response.27,28
Activation of Epithelial, Endothelial, and Stromal Cells in Allograft Rejection
We next compared epithelial transcriptomes from the biopsy with their healthy counterparts. Multiple attempts at scRNA-seq of healthy nephrectomy tissue failed to generate libraries; however, we were successful in generating adult human kidney single-nucleus RNA-sequencing (RNA-seq) data. We sequenced 4259 nuclei to a similar depth as the biopsy and identified six distinct epithelial cell clusters, including podocytes, proximal tubule, loop of Henle, distal tubule, principal cells, and intercalated cells (Figure 3, A–C). The absence of stromal or leukocyte populations presumably reflects either dissociation bias and/or a cell frequency below our limit of detection.
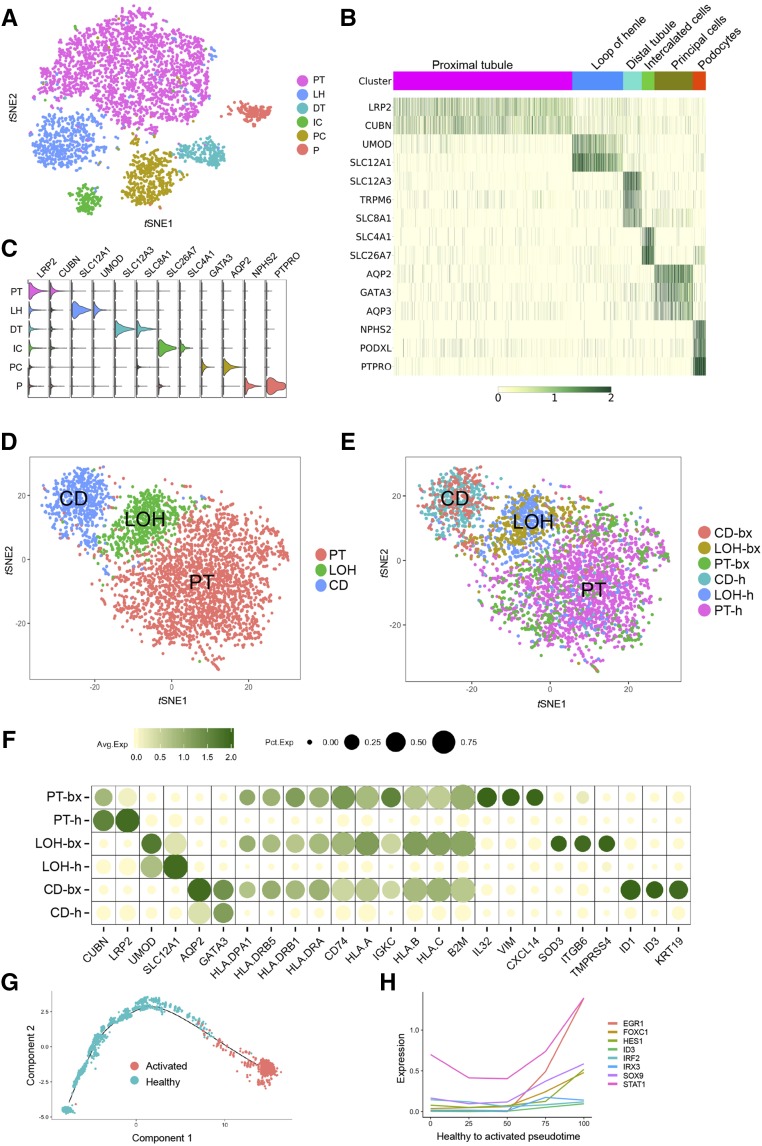
Figure 3.
Comparison of epithelia from single-cell RNA-sequencing of healthy adult kidney with transplant biopsy reveals activated and proinflammatory cell states. (A) Unsupervised clustering identified six distinct cell types in human adult kidney. These types include three tubular cell types (proximal tubule [PT], loop of Henle (LH), and distal tubule (DT), two collecting duct (CD) cell populations principal cells (PC) and intercalated cells (IC), and one podocyte population (P). (B) The heat map showed that putative molecular signature marks the identity of each cluster. (C) The violin plot further confirmed the clean expression of well known cell type–specific markers in each cell population, which makes it suitable for use in benchmarked comparison analysis. (D) tSNE analysis of PT, loop of Henle (LOH), and CD cells from the allograft biopsy and healthy adult human kidney cluster together indicating that cell identity is maintained despite allograft inflammation. (E) Collecting duct cells from the biopsy (CD-bx) coproject by tSNE onto the collecting duct cluster from healthy kidney (CD-h). The same is true of PT and LOH. (F) A dot plot comparing expression of terminal differentiation or inflammatory genes in epithelial cells from the biopsy or healthy kidney. (G) Ordering of healthy and activated PT cells along pseudotime using Monocle. (H) Selected transcription factors that are upregulated during PT activation. LOH-bx, loop of Henle from the biopsy; LOH-h, loop of Henle from healthy kidney; PT-bx, proximal tubule from the biopsy; PT-h, proximal tubule from healthy kidney.
Comparison of scRNA-seq and single-nucleus RNA-seq datasets has been shown to be valid after normalizing to reduce method-specific differences.29 Using a computational approach allowing for integrated analysis of multiple datasets across techniques,30 we compared proximal tubule, loop of Henle, and collecting duct cells from our biopsy dataset with the same cell types from our healthy adult kidney single-nucleus RNA-seq dataset. Unsupervised analysis of combined cells from all six clusters (three healthy and three rejection) by tSNE resulted in the expected three cell types, indicating that rejection did not fundamentally alter tubular cell identity (Figure 3D, Supplemental Figure 6). Consistent with this interpretation, projecting the source of cells onto this tSNE confirmed that healthy proximal tubule was overlaid with rejecting proximal tubule as was loop of Henle and collecting duct (Figure 3E).
Despite the overall similarity between healthy and rejecting proximal tubule, loop of Henle, and collecting duct, differential gene analysis revealed downregulation of terminal differentiation markers and upregulation of proinflammatory genes in biopsy epithelia (Figure 3F). The proximal tubule in particular expressed proinflammatory cytokine genes, such as CXCL14, which induces monocyte chemotaxis, and IL32, which induces expression of TNFα by macrophages (Figure 3F). ITGB6, a gene previously shown to be expressed in distal tubule of the diseased kidney transplant,31 was specifically induced in the loop of Henle in our biopsy dataset. Within collecting duct epithelia, the top statistically significant canonical signature by GSEA that distinguished the biopsy collecting duct from the healthy collecting duct was the TGF-β/BMP signaling signature (Supplemental Figure 7). Collectively, these results highlight the degree to which epithelial damage during rejection amplifies proinflammatory and profibrotic responses.
To further investigate proximal tubule injury responses, we performed cell trajectory analysis by reconstituting the healthy and biopsy proximal tubule clusters by pseudotime analysis. We found a smooth transition between healthy and activated proximal tubule cells (Figure 3G and F). We next asked what genes might be regulating proximal tubule activation by plotting differentially expressed transcription factors across pseudotime. Among others, we observed strong upregulation of Sox9, which has recently been identified as a master regulator of proximal tubule repair after injury, validating our approach.32
Donor ECs are the primary targets of the recipients’ humoral immune response in ABMR. Reclustering of the ECs revealed three separate cell states in rejection (Figure 4, A and B). Differential gene expression analysis suggested that the predominant EC cluster was in the resting state, because it expressed EC markers (PECAM1, VWF, and ENG) but no transcripts previously associated with ABMR or angiogenesis (Figure 4C). We compared average gene expression of the three clusters with healthy human brain and pancreas ECs, and the resting cluster correlated best (Figure 4D). A smaller subcluster expressed the angiogenic program,33 with several of these genes previously described in association with ABMR (Figure 4, C and E)34,35 A third EC cluster expressed markers of endoplasmic stress (XBP1) and the cold shock gene RBM3, suggesting cell stress and activation. This cluster was also actively transcribing Ig, such as has been observed in vitro (Figure 4C).36 The src family kinases have been shown to be activated on ingestion of IgG. Consistent with this, FYN is highly expressed in this EC subcluster.37 Thus, these ECs maybe internalizing bound IgG, consistent with DSA-EC binding in ABMR. Studies have shown that this process occurs in EC via Fc receptor–mediated phagocytosis.38 In line with this notion, our GO analysis data showed that the top GO terms for this cluster were all related to phagocytosis (Supplemental Figure 8).
Figure 4.
Analysis of endothelial cell (EC) subsets. (A) tSNE plot of endothelial subclusters from the kidney biopsy. (B) Heat map showing selected marker genes for the three EC subclusters. (C) Violin plots showing conserved expression of endothelial markers across all three subclusters. The genes SEMA3G, IGFBP3, SERPINE2, and AQP1 indicate activation of an angiogenic program. A separate EC subcluster expresses Igs as well as markers of endoplasmic reticulum stress (XBP1) and cold shock (RBM3). (D) Pearson correlation of all three EC subsets shows best correlation between the resting EC cluster and healthy brain or pancreas ECs. (E) Markers of antibody-mediated rejection are detected in the angiogenic cluster.
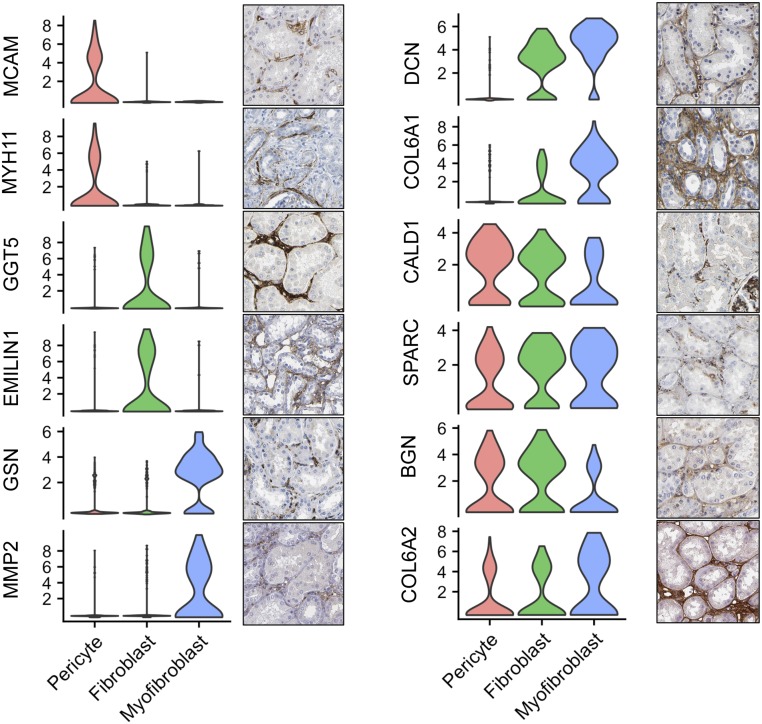
We identified three separate stromal clusters (Supplemental Table 4). Cluster 1 highly expresses RSG5, a pericyte marker,39 as well as CACNA1C, which is expressed in a pericyte pattern. Stromal cluster 2 expresses MoxD1, a gene upregulated in early kidney transplant biopsies and associated with subsequent fibrosis.40 This cluster likely represents a fibroblast cell type. The third stromal cluster uniquely expressed COL8A1 and COL12A1, two genes that we have previously shown to be strongly upregulated in kidney myofibroblasts during fibrotic injury, suggesting a myofibroblast identity for this cluster.41 The interstitial expression patterns for marker genes from each stromal cluster are shown in Figure 5.
Figure 5.
Marker gene localization to independent stromal cell types. The expression of known and new cell type discriminating genes. Violin plots are shown adjacent to immunohistochemistry, which is from the Human Protein Atlas (https://www.proteinatlas.org/). Examples of pericyte-, fibroblast-, and myofibroblast-specific marker genes are shown. In addition, DCN and COL6A1 are expressed in both fibroblast and myofibroblast populations, whereas SPARC, BGN, and COL6A2 are expressed in all three stromal cell types.
Antigen Expression and Antibody Production
Because alloantigens play a central role in ABMR, we profiled the expression of HLA transcripts. Appropriately, class 2HLA transcripts were predominantly expressed in the antigen-presenting cell clusters (Supplemental Figure 9A). Seurat analysis of our biopsy revealed two plasma cell clusters and one B cell cluster. The B cell cluster expressed few Ig genes but did express genes involved in antigen presentation (CD86) and T cell regulation (indoleamine 2,3-dioxygenase, IDO1), thus behaving like a naïve B cell. Plasma cell clusters highly express Ig genes; however, cluster 1 was κ-chain restricted, suggesting that these cells are monoclonal. Plasma cell cluster 2 was not light-chain restricted, and it highly expressed both κ- and λ-gene types (Supplemental Figure 9B). These clusters were labeled plasma cells on the basis of the correlation with a PBMC reference dataset; however, these cells could also represent mature B cells.
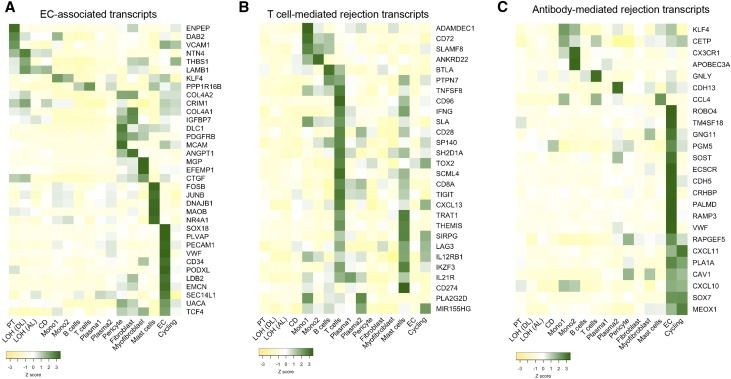
Reassessing the Molecular Signature for Disease Classification at the Single-Cell Level
We next assigned expression of genes previously associated with allograft pathologies to single-cell types.42 When we mapped putative EC-associated transcripts, we found that most of these genes were actually not specifically expressed in ECs. Some of them were even uniquely expressed in non-EC types, such as ENPEP (PT), ANGPT1 (fibroblast), MGP (myofibroblast), and FOSB (mast cells) (Figure 6A). Over one half of the transcripts were expressed in multiple cell types. Whether disease outcome correlates best with expression of these genes in one cell type and not others will require further investigation. By contrast, the 30 genes with expression that is associated with T cell–mediated rejection are predominantly expressed in immune cell types, with the majority expressed in T cells and almost no expression in kidney parenchyma (Figure 6B).43 Finally, most of the transcripts reported to be enriched in ABMR biopsies35 were mainly detected in the EC cluster in our biopsy dataset (Figure 6C), substantiating the critical role of endothelium in the pathogenesis of ABMR.44
Figure 6.
Mapping cell type expression of genes previously associated with kidney allograft pathology. (A) Expression of 35 endothelial cell (EC)–associated genes identified in bulk transcriptional profiling assigned to individual biopsy cell types (likelihood ratio test). A heat map was used to visualize the z score–normalized average gene expression of the candidate genes for each cell cluster identified from the biopsy dataset. A majority of EC-associated transcripts are not expressed in ECs. (B) A similar analysis performed on transcripts associated with T cell–mediated rejection reveals that nearly all of them are expressed in leukocytes and that the majority are expressed in T cells. (C) A similar analysis on transcripts associated with antibody-mediated rejection reveals that most of the genes were expressed in EC clusters. CD, collecting duct; LOH (AL), loop of Henle, ascending limb; LOH (DL), loop of Henle, distal limb; Mono, monocyte; PT, proximal tubule.
Discussion
This study establishes the feasibility of using scRNA-seq to comprehensively measure gene expression from thousands of cells from a single human kidney biopsy. We were able to identify 16 separate cell types from just under 5000 single-cell libraries. We are confident that future improvements of our basic workflow will enable the generation of ten times as many single-cell libraries from a single human biopsy, which should allow for much finer cell type separation and deeper transcript detection. Our experience suggests that standard DropSeq approaches are poorly suited for this application, however, potentially due to incomplete cell lysis as well as inefficient cell capture rates. By contrast, InDrops, as we used here, or the 10× Chromium system are much better suited to analyze single human kidney biopsy.
Our study is limited to a single biopsy, and therefore, results cannot be generalized. However, our findings do reveal several novel insights into human allograft rejection. Anti-HLA antibodies are known to play important roles in rejection, with much attention focused on EC responses to antibody binding. Previous studies suggest that antibody binding causes a number of EC responses, including cell proliferation,45–48 induction of secondary factors (FGFR and VEGF),49,50 and leukocyte recruitment (including vWF and P-selectin expression),51–53 as well as cell survival responses. Our data show two distinct pathologic EC responses in mixed rejection: a resting state and two ABMR response states consisting of an angiogenic state or an Ig phagocytosis state. The resting-state cells probably elicit the initial humoral response, because they express donor-specific HLA and leukocyte adhesion molecules (PECAM1). Evaluating the EC responses to different antibodies in the setting of ABMR will help us better understand why DSAs confer variable degrees of pathogenicity. Therapeutically, the B cell-plasma cell lineage is an attractive target for therapy, because inhibition of alloantibody production will likely improve outcomes in ABMR. To this end, we identified B cells that are likely naïve, polyclonal plasma cells (or mature B cells), and a monoclonal plasma cell cluster representing the spectrum of antibody-producing cells.
We have additionally provided the first single-nucleus RNA-seq dataset from healthy adult human kidney. The reasons for our failure to generate scRNA-seq libraries from healthy adult kidney compared with our success with a diseased transplant biopsy are unclear. We speculate that the robust inflammation present in the transplant biopsy made the tissue more amenable to dissociation. However, this points to a major current challenge and limitation in the application of single-cell technologies to human kidney—the difficulty of successful dissociation without RNA degradation and the associated problem of dissociation bias. For example, we could not identify podocytes in the transplant biopsy, whereas they were present in the healthy kidney single-nucleus dataset, although similar numbers of cells/nuclei were analyzed. However, the healthy human kidney dataset contained only epithelial cell types without stroma, endothelium, or leukocytes. These striking differences indicate that dissociation methods selectively enrich for certain cell types, while losing others—either because they die during dissociation or because they remain in clumps. Clearly, future work is needed to define the optimal cell/nucleus dissociation approach for human kidney. It is worth considering that nuclear dissociation can be carried out entirely on ice—which eliminates the artefactual transcriptional stress responses that are known to arise on incubation of kidney tissue with proteases at 37°C.13
An additional important consideration is that information concerning cell positioning is lost with scRNA-seq. Such information may be critical to properly interpret results. For example, a ligand-receptor analysis between podocytes and intercalated cells does not make sense biologically, because they are positioned so far apart, whereas the same comparison between principle cells and intercalated cells is biologically meaningful. New experimental and computational tools are in development to address the loss of spatial context with scRNA-seq. One approach, fluorescent in situ sequencing,54 allows for genome-wide expression profiling in fixed tissues—preserving tissue architecture for RNA localization studies. In addition, computational approaches can integrate scRNA-seq data with in situ hybridization RNA expression patterns, allowing inference of spatial expression patterns by virtual in situ hybridization.55
Despite current challenges, we envision a time in the future when kidney biopsies are routinely sent for scRNA-seq as part of a molecular diagnostic workup. scRNA-seq can unmask the transcriptional heterogeneity that is hidden in population-averaged measurements. We illustrate the power of this approach by analyzing paracrine signaling pathways between infiltrating leukocytes and kidney parenchyma and by mapping predictive gene expression to single-cell types. We expect that application of scRNA-seq technologies to human native and allograft biopsies will ultimately generate clinically useful datasets to improve diagnostic and prognostic accuracy, enable disease subphenotyping, and accelerate adoption of molecular biopsy interpretation.
Disclosures
None.
Supplementary Material
Acknowledgments
This work was supported by National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant DK107374 (to B.D.H.), grant 173970 (to B.D.H.) from the Chan Zuckerberg Initiative, NIDDK Diabetic Complications Consortium (www.diacomp.org) grants DK076169 (to B.D.H.) and DK115255 (to B.D.H.), and The Keller Family Fund at the Foundation for Barnes-Jewish Hospital (B.D.H.).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related perspective, “Single-Cell Sequencing the Glomerulus, Unraveling the Molecular Programs of Glomerular Filtration, One Cell at a Time,” on pages 2036–2038.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2018020125/-/DCSupplemental.
References
- 1.Park J, Shrestha R, Qiu C, Kondo A, Huang S, Werth M, et al.: Single-cell transcriptomics of the mouse kidney reveals potential cellular targets of kidney disease [published online ahead of print April 5, 2018]. Science doi: 10.1126/science.aar2131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malone AF, Wu H, Humphreys BD: Bringing renal biopsy interpretation into the molecular age with single-cell RNA sequencing. Semin Nephrol 38: 31–39, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sellarés J, de Freitas DG, Mengel M, Reeve J, Einecke G, Sis B, et al.: Understanding the causes of kidney transplant failure: The dominant role of antibody-mediated rejection and nonadherence. Am J Transplant 12: 388–399, 2012 [DOI] [PubMed] [Google Scholar]
- 4.El-Zoghby ZM, Stegall MD, Lager DJ, Kremers WK, Amer H, Gloor JM, et al.: Identifying specific causes of kidney allograft loss. Am J Transplant 9: 527–535, 2009 [DOI] [PubMed] [Google Scholar]
- 5.Gaston RS, Cecka JM, Kasiske BL, Fieberg AM, Leduc R, Cosio FC, et al.: Evidence for antibody-mediated injury as a major determinant of late kidney allograft failure. Transplantation 90: 68–74, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Halloran PF, Pereira AB, Chang J, Matas A, Picton M, De Freitas D, et al.: Potential impact of microarray diagnosis of T cell-mediated rejection in kidney transplants: The INTERCOM study. Am J Transplant 13: 2352–2363, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Halloran PF, Pereira AB, Chang J, Matas A, Picton M, De Freitas D, et al.: Microarray diagnosis of antibody-mediated rejection in kidney transplant biopsies: An international prospective study (INTERCOM). Am J Transplant 13: 2865–2874, 2013 [DOI] [PubMed] [Google Scholar]
- 8.O’Connell PJ, Zhang W, Menon MC, Yi Z, Schröppel B, Gallon L, et al.: Biopsy transcriptome expression profiling to identify kidney transplants at risk of chronic injury: A multicentre, prospective study. Lancet 388: 983–993, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Modena BD, Kurian SM, Gaber LW, Waalen J, Su AI, Gelbart T, et al.: Gene expression in biopsies of acute rejection and interstitial fibrosis/tubular atrophy reveals highly shared mechanisms that correlate with worse long-term outcomes. Am J Transplant 16: 1982–1998, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macosko EZ, Basu A, Satija R, Nemesh J, Shekhar K, Goldman M, et al.: Highly parallel genome-wide expression profiling of individual cells using nanoliter droplets. Cell 161: 1202–1214, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein AM, Mazutis L, Akartuna I, Tallapragada N, Veres A, Li V, et al.: Droplet barcoding for single-cell transcriptomics applied to embryonic stem cells. Cell 161: 1187–1201, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiselev VY, Kirschner K, Schaub MT, Andrews T, Yiu A, Chandra T, et al.: SC3: Consensus clustering of single-cell RNA-seq data. Nat Methods 14: 483–486, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adam M, Potter AS, Potter SS: Psychrophilic proteases dramatically reduce single-cell RNA-seq artifacts: A molecular atlas of kidney development. Development 144: 3625–3632, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mannon RB: Macrophages: Contributors to allograft dysfunction, repair, or innocent bystanders? Curr Opin Organ Transplant 17: 20–25, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Girlanda R, Kleiner DE, Duan Z, Ford EA, Wright EC, Mannon RB, et al.: Monocyte infiltration and kidney allograft dysfunction during acute rejection. Am J Transplant 8: 600–607, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng GX, Terry JM, Belgrader P, Ryvkin P, Bent ZW, Wilson R, et al.: Massively parallel digital transcriptional profiling of single cells. Nat Commun 8: 14049, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ziegler-Heitbrock L, Ancuta P, Crowe S, Dalod M, Grau V, Hart DN, et al.: Nomenclature of monocytes and dendritic cells in blood. Blood 116: e74–e80, 2010 [DOI] [PubMed] [Google Scholar]
- 18.van den Bosch TPP, Hilbrands LB, Kraaijeveld R, Litjens NHR, Rezaee F, Nieboer D, et al.: Pretransplant numbers of CD16+ monocytes as a novel biomarker to predict acute rejection after kidney transplantation: A pilot study. Am J Transplant 17: 2659–2667, 2017 [DOI] [PubMed] [Google Scholar]
- 19.Vereyken EJ, Kraaij MD, Baan CC, Rezaee F, Weimar W, Wood KJ, et al.: A shift towards pro-inflammatory CD16+ monocyte subsets with preserved cytokine production potential after kidney transplantation. PLoS One 8: e70152, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Westerterp M, Gautier EL, Ganda A, Molusky MM, Wang W, Fotakis P, et al. : Cholesterol accumulation in dendritic cells links the inflammasome to acquired immunity. Cell Metab 25: 1294–1304.e6, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castella B, Kopecka J, Sciancalepore P, Mandili G, Foglietta M, Mitro N, et al.: The ATP-binding cassette transporter A1 regulates phosphoantigen release and Vγ9Vδ2 T cell activation by dendritic cells. Nat Commun 8: 15663, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephens TA, Nikoopour E, Rider BJ, Leon-Ponte M, Chau TA, Mikolajczak S, et al.: Dendritic cell differentiation induced by a self-peptide derived from apolipoprotein E. J Immunol 181: 6859–6871, 2008 [DOI] [PubMed] [Google Scholar]
- 23.Worah K, Mathan TSM, Vu Manh TP, Keerthikumar S, Schreibelt G, Tel J, et al.: Proteomics of human dendritic cell subsets reveals subset-specific surface markers and differential inflammasome function. Cell Rep 16: 2953–2966, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lechmann M, Berchtold S, Hauber J, Steinkasserer A: CD83 on dendritic cells: More than just a marker for maturation. Trends Immunol 23: 273–275, 2002 [DOI] [PubMed] [Google Scholar]
- 25.Okayama Y, Kawakami T: Development, migration, and survival of mast cells. Immunol Res 34: 97–115, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mengel M, Reeve J, Bunnag S, Einecke G, Sis B, Mueller T, et al.: Molecular correlates of scarring in kidney transplants: The emergence of mast cell transcripts. Am J Transplant 9: 169–178, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Danelli L, Madjene LC, Madera-Salcedo I, Gautier G, Pacreau E, Ben Mkaddem S, et al. : Early phase mast cell activation determines the chronic outcome of renal ischemia-reperfusion injury. J Immunol 198: 2374–2382, 2017 [DOI] [PubMed] [Google Scholar]
- 28.Holdsworth SR, Summers SA: Role of mast cells in progressive renal diseases. J Am Soc Nephrol 19: 2254–2261, 2008 [DOI] [PubMed] [Google Scholar]
- 29.Lake BB, Codeluppi S, Yung YC, Gao D, Chun J, Kharchenko PV, et al.: A comparative strategy for single-nucleus and single-cell transcriptomes confirms accuracy in predicted cell-type expression from nuclear RNA. Sci Rep 7: 6031, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butler A, Hoffman P, Smibert P, Papalexi E, Satija R: Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol 36: 411–420, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trevillian P, Paul H, Millar E, Hibberd A, Agrez MV: Alpha(v)beta(6) integrin expression in diseased and transplanted kidneys. Kidney Int 66: 1423–1433, 2004 [DOI] [PubMed] [Google Scholar]
- 32.Kumar S, Liu J, Pang P, Krautzberger AM, Reginensi A, Akiyama H, et al.: Sox9 activation highlights a cellular pathway of renal repair in the acutely injured mammalian kidney. Cell Rep 12: 1325–1338, 2015 [DOI] [PubMed] [Google Scholar]
- 33.Reinders ME, Rabelink TJ, Briscoe DM: Angiogenesis and endothelial cell repair in renal disease and allograft rejection. J Am Soc Nephrol 17: 932–942, 2006 [DOI] [PubMed] [Google Scholar]
- 34.Sis B, Jhangri GS, Bunnag S, Allanach K, Kaplan B, Halloran PF: Endothelial gene expression in kidney transplants with alloantibody indicates antibody-mediated damage despite lack of C4d staining. Am J Transplant 9: 2312–2323, 2009 [DOI] [PubMed] [Google Scholar]
- 35.Sellarés J, Reeve J, Loupy A, Mengel M, Sis B, Skene A, et al.: Molecular diagnosis of antibody-mediated rejection in human kidney transplants. Am J Transplant 13: 971–983, 2013 [DOI] [PubMed] [Google Scholar]
- 36.Zhao Y, Liu Y, Chen Z, Korteweg C, Gu J: Immunoglobulin g (IgG) expression in human umbilical cord endothelial cells. J Histochem Cytochem 59: 474–488, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Majeed M, Caveggion E, Lowell CA, Berton G: Role of Src kinases and Syk in Fcgamma receptor-mediated phagocytosis and phagosome-lysosome fusion. J Leukoc Biol 70: 801–811, 2001 [PubMed] [Google Scholar]
- 38.Goebl NA, Babbey CM, Datta-Mannan A, Witcher DR, Wroblewski VJ, Dunn KW: Neonatal Fc receptor mediates internalization of Fc in transfected human endothelial cells. Mol Biol Cell 19: 5490–5505, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.He L, Vanlandewijck M, Raschperger E, Andaloussi Mäe M, Jung B, Lebouvier T, et al.: Analysis of the brain mural cell transcriptome. Sci Rep 6: 35108, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wei C, Menon M, Zhang W, Woytovich C, Philippe N, He J, Murphy B, Wei C: Genomic Analysis of Gene Expression in Human Kidney Transplants Identifies Moxd1 as a Key Driver for Renal Fibrosis [abstract]. Am J Transplant 2017. 17(suppl 3). Available at: http://atcmeetingabstracts.com/abstract/genomic-analysis-of-gene-expression-in-human-kidney-transplants-identifies-moxd1-as-a-key-driver-for-renal-fibrosis/. Accessed May 21, 2018 [Google Scholar]
- 41.Grgic I, Krautzberger AM, Hofmeister A, Lalli M, DiRocco DP, Fleig SV, et al.: Translational profiles of medullary myofibroblasts during kidney fibrosis. J Am Soc Nephrol 25: 1979–1990, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Einecke G, Sis B, Reeve J, Mengel M, Campbell PM, Hidalgo LG, et al.: Antibody-mediated microcirculation injury is the major cause of late kidney transplant failure. Am J Transplant 9: 2520–2531, 2009 [DOI] [PubMed] [Google Scholar]
- 43.Venner JM, Famulski KS, Badr D, Hidalgo LG, Chang J, Halloran PF: Molecular landscape of T cell-mediated rejection in human kidney transplants: Prominence of CTLA4 and PD ligands. Am J Transplant 14: 2565–2576, 2014 [DOI] [PubMed] [Google Scholar]
- 44.Wang S, Zhang C, Wang J, Yang C, Xu M, Rong R, et al.: Endothelial cells in antibody-mediated rejection of kidney transplantation: Pathogenesis mechanisms and therapeutic implications. J Immunol Res 2017: 8746303, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coupel S, Leboeuf F, Boulday G, Soulillou JP, Charreau B: RhoA activation mediates phosphatidylinositol 3-kinase-dependent proliferation of human vascular endothelial cells: An alloimmune mechanism of chronic allograft nephropathy. J Am Soc Nephrol 15: 2429–2439, 2004 [DOI] [PubMed] [Google Scholar]
- 46.Jin YP, Korin Y, Zhang X, Jindra PT, Rozengurt E, Reed EF: RNA interference elucidates the role of focal adhesion kinase in HLA class I-mediated focal adhesion complex formation and proliferation in human endothelial cells. J Immunol 178: 7911–7922, 2007 [DOI] [PubMed] [Google Scholar]
- 47.Jin YP, Jindra PT, Gong KW, Lepin EJ, Reed EF: Anti-HLA class I antibodies activate endothelial cells and promote chronic rejection. Transplantation 79[Suppl]: S19–S21, 2005 [DOI] [PubMed] [Google Scholar]
- 48.Jindra PT, Jin YP, Rozengurt E, Reed EF: HLA class I antibody-mediated endothelial cell proliferation via the mTOR pathway. J Immunol 180: 2357–2366, 2008 [DOI] [PubMed] [Google Scholar]
- 49.Bieri M, Oroszlan M, Farkas A, Ligeti N, Bieri J, Mohacsi P: Anti-HLA I antibodies induce VEGF production by endothelial cells, which increases proliferation and paracellular permeability. Int J Biochem Cell Biol 41: 2422–2430, 2009 [DOI] [PubMed] [Google Scholar]
- 50.Bian H, Harris PE, Reed EF: Ligation of HLA class I molecules on smooth muscle cells with anti-HLA antibodies induces tyrosine phosphorylation, fibroblast growth factor receptor expression and cell proliferation. Int Immunol 10: 1315–1323, 1998 [DOI] [PubMed] [Google Scholar]
- 51.Lowenstein CJ, Morrell CN, Yamakuchi M: Regulation of Weibel-Palade body exocytosis. Trends Cardiovasc Med 15: 302–308, 2005 [DOI] [PubMed] [Google Scholar]
- 52.Yamakuchi M, Kirkiles-Smith NC, Ferlito M, Cameron SJ, Bao C, Fox-Talbot K, et al.: Antibody to human leukocyte antigen triggers endothelial exocytosis. Proc Natl Acad Sci U S A 104: 1301–1306, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fishbein MC, Kobashigawa J: Biopsy-negative cardiac transplant rejection: Etiology, diagnosis, and therapy. Curr Opin Cardiol 19: 166–169, 2004 [DOI] [PubMed] [Google Scholar]
- 54.Lee JH, Daugharthy ER, Scheiman J, Kalhor R, Ferrante TC, Terry R, et al.: Fluorescent in situ sequencing (FISSEQ) of RNA for gene expression profiling in intact cells and tissues. Nat Protoc 10: 442–458, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karaiskos N, Wahle P, Alles J, Boltengagen A, Ayoub S, Kipar C, et al.: The Drosophila embryo at single-cell transcriptome resolution. Science 358: 194–199, 2017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data have been deposited in the Gene Expression Omnibus under accession numbers GSE109564 and GSE114156.