Abstract
Introduction:
Antepartum anxiety and depression are two of the most common risk factors for the development of postpartum depression. Women are at a higher risk of developing depression and suffering from mental disorders during pregnancy and the postnatal period. Psychopathological symptoms during pregnancy have physiological consequences for the fetus, such as impaired blood flow leading to low birth weight, as well as cognitive delay and behavioral problems.
Objectives:
To screen antenatal women for common mental health disorders and to determine the factors associated with mental health disorders during pregnancy.
Methods:
A cross-sectional study among 208 pregnant mothers in the third trimester attending the antenatal clinic at a Government Maternity Home in a low-income urban area of Bengaluru was conducted using clinical interview schedule-revised (CIS-R) questionnaire as a screening tool for detecting the presence of mental morbidity. Data collected were analyzed using SPSS version 16.
Results:
In the study population, 12 (5.8%) screened positive for antepartum mental morbidities, of which depression was the most common. 3.8% of all women screened positive for depression, with 15.4% demonstrating depressive symptoms. Overall, 82 (39.4%) had the presence of one or more psychological symptoms, including fatigue, irritability, anxiety, and problems with sleep and concentration but scored less than the CIS-R cutoff score of 12. Factors associated with the presence of antepartum mental morbidities included poor relationships with their spouse, poor/satisfactory relationship with siblings or in-laws, as well as the desire to have a male child.
Conclusion:
In the study population, 12 (5.8%) screened positive for antepartum mental morbidities. Considering the effects on quality of life for these women as well as poor fetal outcomes associated with maternal mental morbidity, it is important to include screening and treatment of mental morbidity as a part of routine antenatal care.
Keywords: Antepartum mental morbidities, mental health disorders, pregnant women
INTRODUCTION
Pregnancy is a particularly vulnerable time during a woman's life. In addition to common health problems during pregnancy, including gestational diabetes, hypertension, and anemia, mental health issues also pose a large problem. Depression is the leading cause of disability for women worldwide,[1] and pregnancy has been associated with an increased risk of depressive episodes.[2,3]
Postpartum depression is a relatively well-known phenomenon, but studies have shown that depression is also often present in pregnancy, with as many as 12.7% of pregnant women having an episode of major depression.[4] It has been found that 23% of women with postpartum depression started experiencing symptoms of depression during pregnancy.[5] Having an antenatal anxiety disorder has also been found to be a strong risk factor.[6,7] Studies on antenatal anxiety have indicated that generalized anxiety disorder is the most common, with a prevalence of about 8.5%–10.5%, followed by panic disorder (1.4%–5.2%) and obsessive–compulsive disorder (1.2%–5.2%).[8,9,10,11,12] Stressful life events during pregnancy, a lack of social support, and a previous history of depression have been identified as important risk factors for mental morbidities during pregnancy as well. Childcare stresses, pregnancy and obstetric complications, poor relationship with their partner, and lower socioeconomic status have also been identified as moderate-risk factors for depression in pregnancy.[6,7]
Antepartum mental health issues are of public health concern because of the implications for the health of both the mother and child. Depression during pregnancy has been associated with poor attendance at antenatal clinics, substance abuse, and low birth weight, all of which can lead to neonatal morbidity and mortality.[13,14] Anxiety disorders are associated with elevated maternal cortisol, which is a predictor of negative neonatal outcomes, impaired cognitive development, and future behavioral problems.[15]
Mental health issues during pregnancy must, therefore, be diagnosed and addressed. It is clear that interventions to improve maternal mental health during pregnancy are important preventive strategies against negative health and developmental outcomes in newborn and children. Since studies have shown that poverty and mental health issues interact in a negative cycle,[16,17] there is an increased need to screen for and treat antenatal mental morbidities among communities of lower socioeconomic status. Further, migrant populations, who often reside in urban under-privileged areas, have been identified as a group that is at especially high risk for mental health issues during and after pregnancy.[18] However, very few studies have been done to examine antepartum mental morbidities in these vulnerable communities, which make up roughly 30% of urban Indians.[19]
The study was therefore conducted with the aim to screen antenatal women in an urban underprivileged area for mental health disorders during pregnancy and to determine the factors associated with these mental health disorders.
METHODS
This was a hospital-based study conducted during 2-month period in 2016 in an urban underprivileged area of Bengaluru. Permission was obtained from Bruhat Bengaluru Mahanagara Palike Chief Health Officer to conduct this study in a Government Maternity Hospital in that area. Approval from Institution Ethics Committee of St John's National Academy of Health Sciences was also obtained.
A sample size of 208 was calculated (with a 5% precision) based on a systematic review that estimated a 15.9% prevalence of mental health disorders among pregnant women in low- and middle-income countries.[7] Pregnant women aged more than 18 years, with gestational age more than 28 weeks, attending the antenatal clinic, were consecutively sampled and were invited to participate in the study. A gestational age ≥28 weeks was selected because the early gestational period is characterized by symptoms of physical morbidities which might mask psychiatric morbidities.
After obtaining written informed consent, the clinical interview schedule-revised (CIS-R), which is a standardized semi-structured questionnaire to assess the mental state of subjects, was administered by a trained person after translating it into the local language. The Schedule has 14 subsections: somatic symptoms, fatigue, concentration, sleep problems, irritability, worry about physical health, depression, depressive ideas, worry, anxiety, phobia, panic, obsessions, and compulsions. Scores of subsections range from 0 to 4. The ratings obtained at interview provide a score for each section, which together can be summed to yield an overall score.[20] Sociodemographic and obstetric data (including the obstetric sore, gestational age, complications of current and past pregnancy, number of living children, and number of abortions) were also collected. The presence of mental morbidity was indicated by a cutoff score of 12 on the CIS-R.[21] This cutoff has been shown to have a sensitivity of 87.88% and specificity of 96.15% in detecting mental health disorders.[22] Those women found to have a mental health problem were referred for further evaluation and treatment. On the other hand, CIS-R < 12 but scoring on one or more subsections may be termed as “presence of psychological symptoms.”
The data were entered into Microsoft Excel and analyzed using a Statistical Package for Social Sciences Version 16 (SPSS for windows version 16.0. Chicago. SPSS Inc). Descriptive analysis of sociodemographic and obstetric variables was done by calculating frequency, proportion, mean, median, and standard deviation. To determine statistical associations between mental health problems and various demographic factors, tests of significance such as Chi-square test and Fischer's exact were used as appropriate.
RESULTS
A total of 208 pregnant women were included in the study and screened for antenatal mental health disorders.
The mean age of the women in this study was 24.47 ± 3.93 years (range = 18–41 years).
The mean number of family members was 4 ± 2.26, and the median per capita monthly income was Rs. 2071. Majority of the women were homemakers and belonged to socioeconomic class II by BG Prasad classification [Table 1]. The mean gestational age of women in this study was 32.84 ± 3.31 weeks. The majority of the women were multigravidae (56.8%) [Table 2].
Table 1.
Sociodemographics of study subjects (n=208)
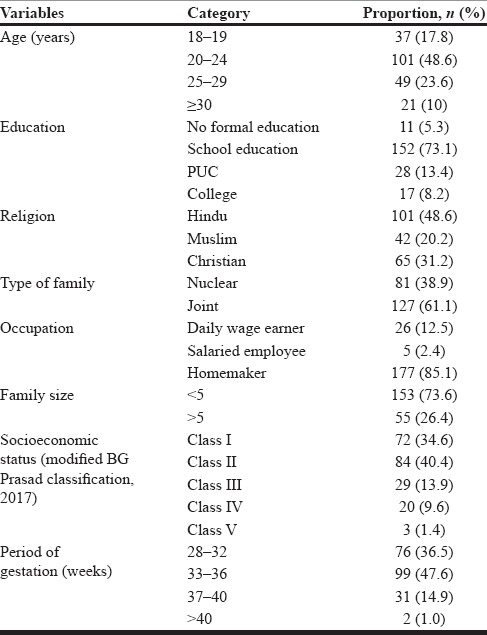
Table 2.
Obstetric details of the subjects (n=208)
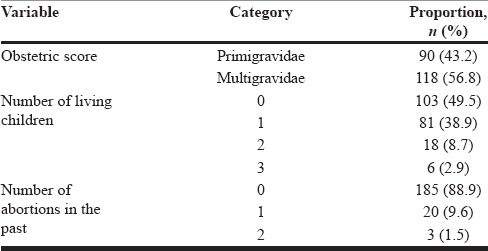
Out of 118 multigravidae women, 32 (27.6%) had a history of a pregnancy or delivery complication, with the cesarean section being the most common (68.8%). Of the 103 women with no living children, 90 were primigravidae and 13 had an abortion in the past. There was no history of postpartum depression among any of the women.
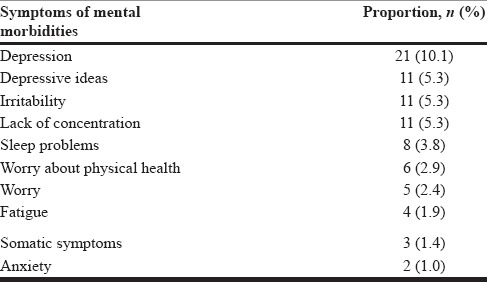
According to CIS-R, 12 (5.8%) pregnant women in this study screened positive for possible antepartum mental morbidity (score of ≥12). Eight of these women screened positive for depression, three had depressive ideas, and three had sleep or somatic symptoms. However, there were a total of 82 women (39.4%) who had the presence of psychological symptoms even though their total CISR score was below 12. The most commonly found symptoms were depression, followed by depressive ideas, lack of concentration, and irritability [Table 3].
Table 3.
Symptoms of antepartum mental morbidities screened using Clinical Interview Schedule-Revised
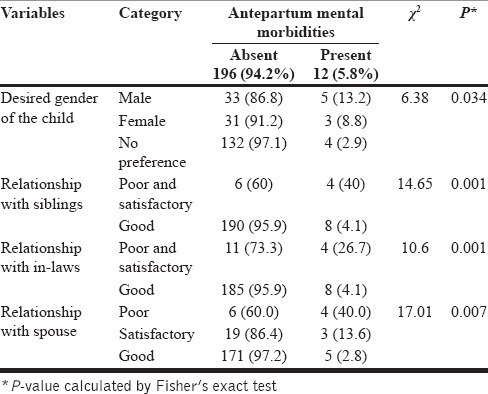
It was found that a poor relationship with spouse and poor/satisfactory relationship with siblings and in-laws were significantly associated with the presence of antepartum mental morbidities compared to women who reported good relationships. In addition, the presence of antepartum morbidities was higher in women who expressed a desire for a male child compared to women with no gender preference or a preference for a female child [Table 4]. There was no significant association of antepartum mental morbidities with other sociodemographic factors such as age, religion, education, family size, socioeconomic status, and occupation, and there was no significant association with obstetric variables such as gravid status, number of living children, or number of abortions in the past
Table 4.
Association of sociodemographic factors with antepartum morbidities (n=208)
DISCUSSION
The purpose of the study was to screen antenatal women for mental health disorders and to determine the factors associated with mental health disorders in pregnancy.
The CIS-R was used to screen for mental morbidities in the antepartum period after 28 weeks of gestation. According to CIS-R, 12 (5.8%) pregnant women in this study screened positive for possible antepartum mental morbidity (score of ≥12). Of these, eight had probable depression and three had depressive ideas. This was lower than the study done in Vellore, Tamil Nadu,[17] where 16.2% screened positive for depression using the same tool. This may be due to the higher education status of our study population and the fact that the women resided in an urban area where health services were easily accessible. However, age, educational status, family type, religion, and gravida status were similar to the Vellore study.[17]
The prevalence of antepartum mental morbidities in this study was lower than that found in an Iranian study of pregnant women in the third trimester, where the prevalence was 21.4%.[23] It was also lower than a study done during the second trimester of pregnancy among 1795 women in Northern Sweden, where psychiatric disorders were present in 14.1% of the women.[24]
The difference between these populations and the present study population is that majority of our women belonged to a joint family and had family support. However, in this study, there was no difference in antenatal mental morbidity among women in a joint family and those in a nuclear family.
In our study, 39.4% of women had the presence of one or more psychological symptoms even though their total CIS-R score was below cutoff of 12. The most common psychological symptoms were depression (10.1%), depressive ideas (5.3%), and irritability and lack of concentration (5.3%).
It is important to note that 10% of the pregnant women in our study had symptoms of depression, as it is a known fact that depression during pregnancy has been associated with adverse fetal outcomes as well as postpartum depression.[13,14]
In the present study, women also had symptoms such as worry, sleep problems, and fatigue. This could be because the majority of women were multigravidas in this study. These women had to take care of their children and were also involved in regular household chores, leading to decreased rest.
A Brazilian cross-sectional study reported the prevalence of antenatal anxiety to be 59.5%,[25] and in a study conducted in Hawaii among pregnant women between the age group of 18–35 years of age, 13% had anxiety.[26] In our study, the prevalence of anxiety was only 1%. This might be because the majority (61.1%) of study subjects belonged to a joint family, and mostly, they will be in their mother's house which will reduce the amount of psychological anxiety and stress.
The study population screened positive for physical problems, sleep problems, fatigue, and irritability. Reason can be stated that the majorities (56.8%) of women were multigravidas and had to take care of other living children in the family, leading to decreased rest. They are also involved in regular household chores.
We found that antepartum mental morbidities are associated with a desire of male child and poor or just satisfactory relationship with in-laws, siblings, and spouse, which was similar to many other studies.[27,28,29,30,31,32] Probably, women without a male child and desirous of the same were apprehensive and anxious about the outcome of their current pregnancy, leading to psychosomatic disorders which were picked up by CISR. These associations in our study may be because they may be young in their marriage career.
A similar study in Goa, India, showed a significant association of antenatal mental morbidity with factors such as illiteracy of mother, younger age of the mother, and nuclear family.[33] This was not the case with the present study where desire for male child and family relationship were significantly associated with mental morbidities and not education or age of mother and type of family.
The National Mental Health Survey of India 2015–2016 revealed that the prevalence of mental disorders in adult females was 7.5%, with predominance in depressive disorders and neurotic and stress-related disorders,[34] which were more than the present study maybe because all women more than 18 years were assessed in that survey. Another study done in rural South India among women also showed an increased presence of mental morbidities.[35] The pressures created by their multiple roles, gender discrimination, and associated factors of poverty, hunger, malnutrition, overwork, domestic violence, and sexual abuse combine to account for women's poor mental health.[36]
There are important public health implications our findings. Since 5.8% of pregnant women in the third trimester were found to have mental morbidity, this translates into thousands of pregnant women in the country suffering from mental morbidities which may be going undetected and untreated. This, in turn, could lead to several thousands of cases of postpartum depression, which could result in poor maternal and child health outcomes.
The present study lacked qualitative approach which prevented the researchers from probing deeper into the real issues faced by pregnant women which led to these mental morbidities. Overlapping of physical symptoms in the third trimester with psychological morbidities may have altered the results.
The findings of this study are the call for integration of psychological interventions in routine antenatal care, either universal or targeted, as part of maternal and child health activities of the accredited social health activists at the primary care level.
CONCLUSION
In the present study conducted among women availing antenatal care at a Government Maternity Hospital in an urban underprivileged area of Bengaluru, 5.8% of pregnant women in the third trimester screened positive for antepartum mental morbidities. Poor or just satisfactory relationship with spouse, siblings, and in-laws and desire for a male child were the predictors of antepartum mental morbidities. Considering the adverse fetal outcomes and poor maternal well-being of pregnant women with mental morbidity, it is important to include screening and treatment of mental morbidity as a part of routine antenatal care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 2.Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–73. doi: 10.1192/bjp.150.5.662. [DOI] [PubMed] [Google Scholar]
- 3.O’Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: Comparison of childbearing and nonchildbearing women. J Abnorm Psychol. 1990;99:3–15. doi: 10.1037//0021-843x.99.1.3. [DOI] [PubMed] [Google Scholar]
- 4.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summary) 2005;119:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watson JP, Elliott SA, Rugg AJ, Brough DI. Psychiatric disorder in pregnancy and the first postnatal year. Br J Psychiatry. 1984;144:453–62. doi: 10.1192/bjp.144.5.453. [DOI] [PubMed] [Google Scholar]
- 6.Stewart DE, Robertson E, Dennis CL, Grace SL, Wallington T. Toronto: University Health Network Women's Health Program; 2003. University Health Network Women's Health Programme Postpartum Depression: Literature Review of Risk Factors and Interventions. [Google Scholar]
- 7.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012;90:139G–49G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutter-Dallay AL, Giaconne-Marcesche V, Glatigny-Dallay E, Verdoux H. Women with anxiety disorders during pregnancy are at increased risk of intense postnatal depressive symptoms: A prospective survey of the MATQUID cohort. Eur Psychiatry. 2004;19:459–63. doi: 10.1016/j.eurpsy.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Adewuya AO, Ola BA, Aloba OO, Mapayi BM. Anxiety disorders among Nigerian women in late pregnancy: A controlled study. Arch Womens Ment Health. 2006;9:325–8. doi: 10.1007/s00737-006-0157-5. [DOI] [PubMed] [Google Scholar]
- 10.Guler O, Sahin FK, Emul HM, Ozbulut O, Gecici O, Uguz F, et al. The prevalence of panic disorder in pregnant women during the third trimester of pregnancy. Compr Psychiatry. 2008;49:154–8. doi: 10.1016/j.comppsych.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Uguz F, Gezginc K, Zeytinci IE, Karatayli S, Askin R, Guler O, et al. Obsessive-compulsive disorder in pregnant women during the third trimester of pregnancy. Compr Psychiatry. 2007;48:441–5. doi: 10.1016/j.comppsych.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, et al. Effects of posttraumatic stress disorder on pregnancy outcomes. J Affect Disord. 2007;102:137–43. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Field T, Diego M, Hernandez-Reif M. Prenatal depression effects on the fetus and newborn: A review. Infant Behav Dev. 2006;29:445–55. doi: 10.1016/j.infbeh.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Pagel MD, Smilkstein G, Regen H, Montano D. Psychosocial influences on new born outcomes: A controlled prospective study. Soc Sci Med. 1990;30:597–604. doi: 10.1016/0277-9536(90)90158-o. [DOI] [PubMed] [Google Scholar]
- 15.Teixeira JM, Fisk NM, Glover V. Association between maternal anxiety in pregnancy and increased uterine artery resistance index: Cohort based study. BMJ. 1999;318:153–7. doi: 10.1136/bmj.318.7177.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chandran M, Tharyan P, Muliyil J, Abraham S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry. 2002;181:499–504. doi: 10.1192/bjp.181.6.499. [DOI] [PubMed] [Google Scholar]
- 17.Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: Prospective study from Rawalpindi, Pakistan. J Affect Disord. 2007;100:115–21. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins CH, Zimmerman C, Howard LM. Refugee, asylum seeker, immigrant women and postnatal depression: Rates and risk factors. Arch Womens Ment Health. 2011;14:3–11. doi: 10.1007/s00737-010-0198-7. [DOI] [PubMed] [Google Scholar]
- 19.Government of India Ministry of Home Affairs. Migration. Census of India. [Last accessed on 2017 Dec 10]. Available from: http://www.censusindia.gov.in/Census_And_You/migrations.aspx .
- 20.Nambi SK, Prasad J, Singh D, Abraham V, Kuruvilla A, Jacob KS, et al. Explanatory models and common mental disorders among patients with unexplained somatic symptoms attending a primary care facility in Tamil Nadu. Natl Med J India. 2002;15:331–5. [PubMed] [Google Scholar]
- 21.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: A standardized assessment for use by lay interviewers. Psychol Med. 1992;22:465–86. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 22.Subramaniam K, Krishnaswamy S, Jemain AA, Hamid A, Patel V. The clinical interview schedule-revised (CIS-R)-Malay version, clinical validation. Malays J Med Sci. 2006;13:58–62. [PMC free article] [PubMed] [Google Scholar]
- 23.Abdollahi F, Rohani S, Sazlina GS, Zarghami M, Azhar MZ, Lye MS, et al. Bio-psycho-socio-demographic and obstetric predictors of postpartum depression in pregnancy: A prospective cohort study. Iran J Psychiatry Behav Sci. 2014;8:11–21. [PMC free article] [PubMed] [Google Scholar]
- 24.Andersson L, Sundström-Poromaa I, Bixo M, Wulff M, Bondestam K, Šström M, et al. Point prevalence of psychiatric disorders during the second trimester of pregnancy: A population-based study. Am J Obstet Gynecol. 2003;189:148–54. doi: 10.1067/mob.2003.336. [DOI] [PubMed] [Google Scholar]
- 25.Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health. 2007;10:25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- 26.Deborah G, Leslie M, Leighann F, Jane O, Courteney M. Mental health during pregnancy: A study comparing Asians, Caucasian and native Hawaiian women. Mater Child Health J. 2006;16:34–7. doi: 10.1007/s10995-006-0165-0. [DOI] [PubMed] [Google Scholar]
- 27.Vijayaselvi R, Beck MM, Abraham A, Kurian S, Regi A, Rebekah G. Risk Factors for Stress During Antenatal Period Among Pregnant Women in Tertiary Care Hospital of Southern India. Journal of Clinical and Diagnostic Research: JCDR. 2015;9:QC01–QC05. doi: 10.7860/JCDR/2015/13973.6580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abujilban SK, Abuidhail J, Al-Modallal H, Hamaideh S, Mosemli O. Predictors of antenatal depression among Jordanian pregnant women in their third trimester. Health Care Women Int. 2014;35:200–15. doi: 10.1080/07399332.2013.817411. [DOI] [PubMed] [Google Scholar]
- 29.Pajulo M, Savonlahti E, Sourander A, Helenius H, Piha J. Antenatal depression, substance dependency and social support. J Affect Disord. 2001;65:9–17. doi: 10.1016/s0165-0327(00)00265-2. [DOI] [PubMed] [Google Scholar]
- 30.Pereira PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF. Depression during pregnancy: Prevalence and risk factors among women attending a public health clinic in Rio de Janeiro, Brazil. Cad Saude Publica. 2009;25:2725–36. doi: 10.1590/s0102-311x2009001200019. [DOI] [PubMed] [Google Scholar]
- 31.Mina S, Balhara YP, Verma R, Mathur S. Anxiety and depression amongst the urban females of Delhi in ante-partum and post-partum period. Delhi Psychiatry J. 2012;15:347–51. [Google Scholar]
- 32.Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: Prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. 2013;22:37–40. doi: 10.4103/0972-6748.123615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: A study of mothers in Goa, India. Am J Psychiatry. 2002;159:43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 34.Bengaluru: In Collaboration with Partner Institutions; 2015-16. National Mental Health Survey of India, 2015-2016 Prevalence Patterns and Outcomes. Supported by Ministry of Health and Family Welfare Government of India and Implemented by National Institute of Mental Health and Neuro – Sciences. [Google Scholar]
- 35.Prasad J, Abraham S, Akila B, Joseph A, Jacob KS. Symptoms related to the reproductive tract and mental health among women in rural Southern India. Natl Med J India. 2003;16:303–8. [PubMed] [Google Scholar]
- 36.Malhotra S, Shah R. Women and mental health in India: An overview. Indian J Psychiatry. 2015;57:S205–11. doi: 10.4103/0019-5545.161479. [DOI] [PMC free article] [PubMed] [Google Scholar]


