Abstract
Background:
The role of craving in alcohol dependence and its relationship with relapse has been studied widely in the past decade. The present study was undertaken to assess the role of craving in short-term relapse of patients seeking treatment for alcohol dependence and changes in craving score at the end of detoxification and at follow-up.
Materials and Methods:
A total of 34 male individuals with alcohol dependence (excluding comorbid drug dependence, organic or psychiatric disorder), after detoxification and discharge, consented. No anticraving medicine, aversive or psychotherapy, was advised. They were diagnosed on the International Statistical Classification of Diseases-10 using Diagnostic Interview for Genetic Studies. Severity of Alcohol Dependence Questionnaire (SADQ) and Clinical Institute Withdrawal Assessment Scale–Alcohol-Revised (CIWA-AR) were administered at the time of admission. Penn Alcohol Craving Scale (PACS) was applied at the time of discharge and follow-up to measure craving for alcohol.
Results:
Out of a total of thirty patients analyzed after dropout, 21 relapsed at the end of 1 month. On comparing PACS scores between relapsed and nonrelapsed patients, the difference was significant at both time points, i.e., at discharge and follow-up (t = 4.15, P < 0.0001 and t = 4.01, P < 0.001, respectively). In the total sample, SADQ and CIWA-AR scores were positively correlated (r = 0.47, P = 0.009). PACS at discharge was compared with PACS at follow-up, of which the correlation was high (r = 0.832, P < 0.0001).
Conclusion:
Craving seems to be a main factor related to relapse. Its measurement with PACS can be a useful tool to predict subsequent drinking and to identify individual risk for relapse during treatment.
Keywords: Alcohol dependence, craving, early relapse
INTRODUCTION
Treatment of substance dependence in the short term may be quite effective, but ensuring abstinence in the long term is a challenge and relapse is common. The two most common definitions of relapse are (a) drinking a specified number and frequency of drinks, for example, more than 60 g/day for men or 40 g/day for women or more than five drinks for men and four drinks for women on one occasion[1] and (b) any drinking of alcohol irrespective of the amount of alcohol drunk (most common definition).[2,3,4,5,6,7]
Awareness of factors influencing relapse will make it possible to develop strategies to minimize their effects on relapse. A factor that can be determined before relapse, and is known as a risk, is craving for alcohol.[8,9,10] Individuals experiencing a high level of craving during the treatment phase are more likely to drop out.[11] Severity of craving reported at the end of treatment can predict a relapse to alcohol abuse after a 3-month follow-up[12] and a 6-month follow-up.[8,13]
The rate of relapse after detoxification varies, depending on criteria, treatment received for de-addiction, and severity of the disorder. Some authors[14] reported relapse rates up to 85%, independent of treatment as inpatients until complete remission of physical withdrawal symptoms. Up to 68% relapsed over 12 months even while on anticraving medications.[15] Miller et al.[16] in their review reported a relapse rate of 75% over 1 year of treatment. Even after intensive psychological intervention, 32% relapsed over 12 months.[8]
The final pathway for relapse may be craving.[17] Three craving types were described in the “three-pathway psycho-biologic model” of Hillemacher et al., i.e. “reward craving,” “relief craving,” and “obsessive craving,” and that different personal characteristics and different neurotransmitter systems played a role in different types of craving, and different risk factors may cause craving as a common result. The craving in patients involved in outpatient-care programs determined both relapse during treatment and relapse based on intensive use of alcohol during the 12 months following treatment.[8] In outpatient-care alcohol-dependent patients, there was a link between increasing craving during abstinence and dropouts who relapsed.[18] A high level of craving and not attending outdoor treatment program were factors predicting relapse.[15] The important factor in relapse may be the severity of craving but not the severity of alcohol-related problems.[19,20] Higher Penn Alcohol Craving Scale (PACS) scores at the time of admission and discharge are associated with relapse even after residential addiction treatment (Schneekloth et al., 2017). Alcohol craving class but not depressive symptoms was predictive of time to relapse to any drinking during 6 months after residential treatment.[21] Craving was strongly associated with alcohol use at every weekly evaluation in the COMBINE study among 1370 alcohol-dependent patients across several sites in the US.[22] In their study, for each 1-unit increase in the craving scale, the likelihood of drinking in the following week was 31% higher.
Indian literature has focused on craving chiefly to evaluate the efficacy of different medications,[23,24,25,26,27,28,29,30] but craving has been less studied.[31,32] The present study was undertaken to assess the role of craving in short-term relapse of patients seeking treatment for alcohol dependence and changes in craving score at the end of detoxification and at follow-up.
MATERIALS AND METHODS
The study was conducted in the Department of Psychiatry and De-addiction, Centre of Excellence in Mental health, Postgraduate Institute of Medical Education and Research Dr. Ram Manohar Lohia Hospital, New Delhi, a tertiary care teaching, free of cost government hospital in North India, from November 2014 to March 2016. Institutional ethics committee approval was obtained at the outset. Male patients between 18 and 50 years old, diagnosed as alcohol dependence (International Statistical Classification of Diseases-10 criteria), admitted for alcohol detoxification, and fulfilling inclusion criteria and willing to participate in the study were recruited. Individuals with comorbid drug dependence (except for nicotine), comorbid organic or psychiatric disorders which could interfere with diagnosis, or craving or relapse or on any anticraving medication, aversive therapy or psychotherapy, at discharge were excluded from the study. The following instruments were applied and the procedure was followed.
Instruments used
Diagnostic Interview for Genetic Studies, Hindi version
Diagnostic Interview for Genetic Studies (DIGS)[33] is a structured clinical interview developed by Nurnberger et al.[34] It was specially designed by a collaboration of investigators in the National Institute of Mental Health genetics initiative for the purpose of genetic studies in psychiatry. It aims to facilitate in the assessment of major affective disorders, schizophrenia, alcohol or drug dependence, and their spectrum disorders. It involves a detailed evaluation of the course and chronology of the symptoms as well as the comorbidities and also has algorithmic scoring capability. All participants were interviewed using the DIGS and diagnosis was reconfirmed in research review meetings headed by a board-certified psychiatrist.
Clinical Institute Withdrawal Assessment Scale–Alcohol-Revised
Clinical Institute Withdrawal Assessment Scale–Alcohol-Revised (CIWA-AR)[35] was developed for monitoring alcohol withdrawal. This is a best known and a most extensively studied scale with well-documented reliability, reproducibility, and validity. It consists of a total of 10 items, each item score ranging from 0 to 7. All scores are added for total scoring.
Severity of Alcohol Dependence Questionnaire
Severity of Alcohol Dependence Questionnaire (SADQ) (20 items)[36] was developed to study the severity of alcohol dependence. It is a 20-item scale. Each item score ranges from 0 to 3 (almost never to nearly always). On the basis of total scoring, individuals are assessed for severity of alcohol dependence. Scores 0–3 represent no dependence, 4–19 mild dependence, 20–30 moderate dependence, 31–44 severe dependence, and 45+ very severe dependence.
Penn Alcohol Craving Scale
This scale is used to measure craving for alcohol. It contains five questions about frequency, intensity, and duration of craving, the ability to resist drinking, and asks for an overall rating of craving for alcohol for the previous week. For each of the five questions, there are seven possible responses. At the end of each response, there is a small number ranging from 0 to 6 in parentheses, for example (0). This number is an “item score.” To determine a patient's PACS score, the five item scores are added together. There is no established “cutoff” score. However, researchers at the University of Pennsylvania reported that total scores of 10 or higher during treatment were associated with an increased risk for relapse.[37] The Hindi version of the scale was used after due translation by trained mental health professionals. Back translation and validation was carried out on a small group of similar individuals at the same treatment center.
Definition of relapse
Relapse is defined as a return to any drinking of alcohol irrespective of the amount of alcohol drunk. In the Indian context, this is more feasible as it is easier to obtain information.
Procedure
The individuals were explained the study, the time required, advantage and disadvantages, and that she/he would not receive any compensation. Thereafter, written informed consent was obtained. Participation by accompanying relatives was solicited. Participants were assessed in detail using DIGS and SADQ. CIWA-AR was administered 8 hourly and participants were detoxified using lorazepam in required doses. With decreasing CIWA-AR score, lorazepam was gradually decreased and discontinued. The participants were discharged after they scored 0 on the CIWA-AR and were off lorazepam for at least 7 days. PACS was applied at the time of discharge. The participants did not receive any pharmacotherapy or psychotherapy except tablet thiamine at the time discharge and were followed up after 1 month. Participants, and if not available their family members, were contacted telephonically every week. Those who relapsed were requested to attend the hospital within 1 week of relapse, while those who did not were requested to attend the hospital after 1 month, for assessment of craving by applying PACS.
Statistical analysis
Statistical Package for the Social Sciences (SPSS v 21) (IBM Corp, Released 2012 )[38] was used for statistical analysis. A database specific to the study was made in Microsoft Office Excel. All the data including both quantitative and qualitative variables were entered in this database for easy retrieval. Relevant data were extracted from DIGS database and from other scales. The complete master chart was made including sociodemographic and broad clinical variables of both quantitative and qualitative variables. Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± standard deviation (SD) and median. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected, nonparametric test was used. Quantitative variables were compared using unpaired t-test/Mann–Whitney U-test (when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using Chi-square test/Fisher's exact test. P < 0.05 was considered statistically significant.
RESULTS
A total of 34 male patients, after detoxification and discharge from male de-addiction psychiatry ward, consented for the study. Four individuals were subsequently excluded. One left against medical advice on the second day after admission, one had comorbid depression, and two had comorbid medical complications (seizure and liver cirrhosis). Out of the 30 patients finally analyzed, 21 relapsed at the end of 1 month and 9 did not.
Those who did not and those who relapsed were comparable as to sociodemographic characteristics (age, years of education, religion, type of family, marital status, and employment status) [Table 1]; General Assessment of Functioning (from the DIGS) and CIWA-AR ratings at the time of admission were not significantly different.
Table 1.
Demographic and alcohol-related parameters among nonrelapsed and relapsed groups
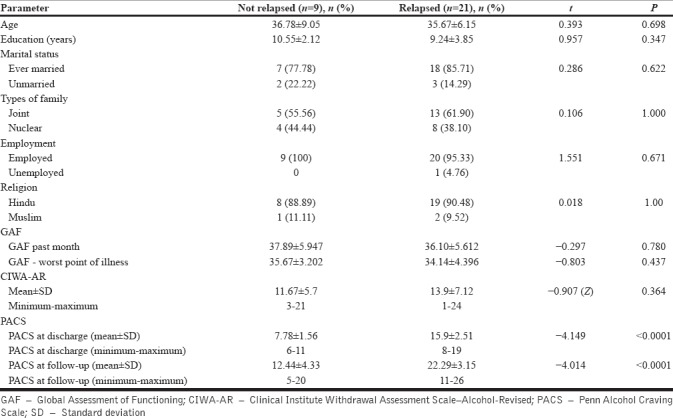
On comparing PACS score at discharge and follow-up between relapsed and nonrelapsed groups, the difference was highly significant at both time points (t = 4.15, P < 0.0001 and t = 4.01, P < 0.0001, respectively). Patients who relapsed not only had significantly higher craving score on PACS score at the time of discharge but also on PACS score at follow-up/relapse. While relapsed group had PACS score of 15.9 ± 2.51, that of nonrelapsed group was 7.78 ± 1.56 at the time of discharge [Table 1].
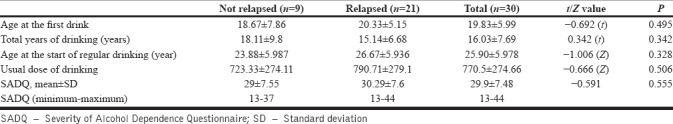
The two groups were significantly different on the basis of SADQ score also at the time of admission. The mean SADQ score of the total sample was 30, indicating moderate-to-severe dependence. In terms of absolute amount of alcohol drunk, the relapsed group seemed to drink a higher quantity, but started later, although not statistically significantly so, the two groups were similar in terms of problems and social complication due to the use of alcohol [Table 2].
Table 2.
Comparison of alcohol drinking parameters between relapsed and nonrelapsed patients and severity of alcohol dependence measure with Severity of Alcohol Dependence Questionnaire
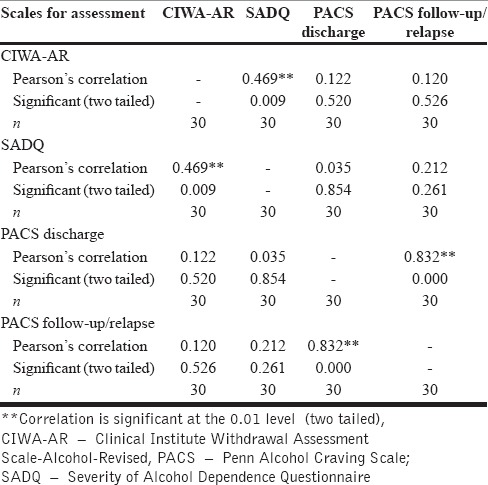
In the total sample, SADQ and CIWA-AR scores were highly positively correlated (Pearson's correlation, 0.469 [0.009]), indicating that high SADQ score correlated with high CIWA-AR score. SADQ and CIWA-AR scores also correlated positively with PACS score both at discharge and at follow-up/relapse, but correlation was not statistically significant. PACS score at discharge was positively correlated with PACS at follow-up/relapse with Pearson's correlation of 0.832 (0.000). Thus, when PACS at discharge was high, PACS at follow-up/relapse was also high [Table 3].
Table 3.
Pearson's correlations of Penn Alcohol Craving Scale score with Severity of Alcohol Dependence Questionnaire and Clinical Institute Withdrawal Assessment Scale-Alcohol-Revised
DISCUSSION
Craving is an established cause for relapse after detoxification. Different studies have used various methods and scales to measure different aspects of craving. However, most previous samples included persons with comorbid axis I or axis II diagnoses, because of which craving as a sole factor in relapse could not be investigated. In the present study, by excluding comorbidity, the authors tried to clinically evaluate the role of craving alone in relapse.
The PACS used in this study is a simple 5-item, scale which includes questions about the frequency, intensity, and duration of craving, and the ability to resist drinking. By its simple structure, the PACS facilitates evaluation of craving as an aversive, appetitive, or both states. It also helps in evaluating the severity of craving and thus can be administered repeatedly. As yet, it has not been widely used in the Indian setting. We used a reliably translated Hindi version.
The study utilized a sample size of 30. Both groups, relapsed and nonrelapsed, were statistically similar in demographic and alcohol use parameters. However, this sample was recruited from a tertiary care teaching institute and thus may or may not represent primary care samples.
Alcohol use parameters did not differ significantly between the nonrelapsed and relapsed groups. The mean total duration of alcohol intake in our study groups was 15.14 and 18.11 years in the nonrelapsed and relapsed groups, respectively. The mean daily alcohol intake was 790.71 ml and 723.33 ml (mostly whiskey, rum, and vodka) in the nonrelapsed group and relapsed groups, respectively. The SD and the ranges of amount of usual daily alcohol intake were wide in both the groups and were comparable statistically. Higher volume intake was associated with high craving score but at admission when withdrawal symptoms were probably still present.[39] In our study, PACS was applied when detoxification was complete and the patients were completely off lorazepam.
Mean age of the first drink was 18.67 years in nonrelapsed group and 20.33 years in relapsed group. Age of regular drinking (defined as having a drink at least once a week, for 6 months) was 24 years in nonrelapsed and 27 years in relapsed groups, while in the study by Bottlender and Soyka,[8] the sample became “dependent drinkers” at a much younger age – 14 years in the nonrelapsed group and 16 years in the relapsed group. In our sample, the relapsed group started their first drink later, become regular drinker later, and reported lesser number of years of drinking as compared to nonrelapsed group. However, relapsed group started alcohol-related problems such as binge drinking, trouble driving, socio-occupational impairment, neglect of household work, and blackouts earlier as compared to nonrelapsed group although not significantly so.
Global Assessment of Functioning (GAF) score in the past month was approximately 38 in nonrelapsed and 36 in relapsed groups, while GAF score at worst point of illness was approximately 36 in nonrelapsed and 34 in relapsed groups. Among most of the samples, GAF score ranged from 30 to 40. This range indicates major impairment in several areas such as work, family relationships, unable to do housework, and was the time when patient or family members came to seek help – at worst point of GAF score, when there was impairment in almost all areas of functioning. The CIWA-AR rating at admission was statistically similar. The mean CIWA-AR score (out of a possible total score of 67) in the nonrelapsed group was 11.67 with a range of 3–21 and in the relapsed group was 13.9 with a range of 1–24, implying that majority of our sample suffered from moderate-to-severe withdrawal.
After the 1-month follow-up, 21 (70%) patients relapsed. Previous rates have varied from a low of 57% in 12 months[5] to 85% in 3 months.[14] Our definition of relapse was wide – any amount of alcohol was considered a relapse. We also included a group which did not access psychotherapy or pharmacotherapy (anticraving or aversive) after discharge.
In our sample, high craving score at the time of discharge correlated very highly with the risk of early relapse within a month (mean PACS scores at both discharge and relapse were approximately double of the nonrelapsed group), similar differences have been reported.[15] Severity of craving reported at the end of the treatment was used to predict a relapse to alcohol abuse after 3 months,[12] 6 months,[21] and 12 months.[8] Craving (and relapse in some studies) has been linked to the severity of the psychopathology, especially the negative affect (such as depression and anxiety,[8,16] severity of alcohol dependence,[40] or withdrawal symptoms).[18] Relapse rate was approximately 72% in our sample and was highly significantly correlated with craving (P ≤ 0.001).
We compared PACS mean score at discharge with respect to weeks of abstinence. Those relapsed in the 1st week (n = 11) had slightly lower mean PACS score as compared to those who relapsed in the 2nd (n = 5) and 3rd weeks (n = 5). Relapsed group had consistently higher PACS scores than the nonrelapse group. We could not find comparable analyses in other studies.
Different mechanisms may underlie the craving for alcohol among different patient subtypes.[6] Our patients did not suffer from comorbidity except for tobacco dependence. Thus, craving could be the final pathway for relapse. PACS or other craving scales could be useful to identify those who need more intensive interventions and follow-ups. Using additional relapse prevention approaches which may help the person to recognize cues that lead to drinking and drugs that decrease craving may be the other strategies that need to be followed.
However, this study suffered from certain limitations – only males, those admitted for withdrawal, at a tertiary care center catering mainly to patients from surrounding areas, and primarily relying on patients and their family members for information regarding relapse. We included only those with alcohol dependence, and comorbid and other psychiatric diagnoses were excluded. This was both the strength and a weakness of our study. We also deliberately excluded those accessing any other intervention for alcohol dependence, either medication or psychological interventions.
CONCLUSION
Craving seems to be the main factor related with relapse. The study indicates that measurement of craving with the PACS can be a useful tool to predict subsequent drinking during treatment and monitoring patients to identify individuals at risk for relapse. Maybe those patients with elevated craving scores who are at a higher risk for relapsing would benefit from intensified aftercare and of additional anticraving medication such as naltrexone or acamprosate and psychological intervention. More focus should be on reducing the craving as compared to depressive or anxiety symptoms. Even after excluding psychiatric comorbidity, relapse rate was very high even at 1-month follow-up. Depressive and anxiety symptoms[18] may play a role in relapse, and hence treatment focus should be on management of craving too.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Peppers MP. Benzodiazepines for alcohol withdrawal in the elderly and in patients with liver disease. Pharmacotherapy. 1996;16:49–57. [PubMed] [Google Scholar]
- 2.Kumar CN, Andrade C, Murthy P. A randomized, double-blind comparison of lorazepam and chlordiazepoxide in patients with uncomplicated alcohol withdrawal. J Stud Alcohol Drugs. 2009;70:467–74. doi: 10.15288/jsad.2009.70.467. [DOI] [PubMed] [Google Scholar]
- 3.Geerlings PJ, Ansoms C, vanderBrink W. Acamprosate and prevention of relapse in alcoholics: Results of a randomized placebo controlled double-blind study in out patient alcoholics in the Netherlands, Belgium and Luxemburg. Eur Addict Res. 1997;3:129–37. [Google Scholar]
- 4.Poldrugo F. Acamprosate treatment in a long-term community-based alcohol rehabilitation programme. Addiction. 1997;92:1537–46. [PubMed] [Google Scholar]
- 5.Pelc I, Verbanck P, Le Bon O, Gavrilovic M, Lion K, Lehert P, et al. Efficacy and safety of acamprosate in the treatment of detoxified alcohol-dependent patients. A 90-day placebo-controlled dose-finding study. Br J Psychiatry. 1997;171:73–7. doi: 10.1192/bjp.171.1.73. [DOI] [PubMed] [Google Scholar]
- 6.Sass H, Soyka M, Mann K, Zieglgänsberger W. Relapse prevention by acamprosate. Results from a placebo-controlled study on alcohol dependence. Arch Gen Psychiatry. 1996;53:673–80. doi: 10.1001/archpsyc.1996.01830080023006. [DOI] [PubMed] [Google Scholar]
- 7.Whitworth AB, Fischer F, Lesch OM, Nimmerrichter A, Oberbauer H, Platz T, et al. Comparison of acamprosate and placebo in long-term treatment of alcohol dependence. Lancet. 1996;347:1438–42. doi: 10.1016/s0140-6736(96)91682-7. [DOI] [PubMed] [Google Scholar]
- 8.Bottlender M, Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol Alcohol. 2004;39:357–61. doi: 10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- 9.Miller WR, Westerberg VS, Harris RJ, Tonigan JS. What predicts relapse? Prospective testing of antecedent models. Addiction. 1996;91(12s1):155–72. [PubMed] [Google Scholar]
- 10.Cooney NL, Litt MD, Morse PA, Bauer LO, Gaupp L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J Abnorm Psychol. 1997;106:243–50. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- 11.Soyka M, Hasemann S, Scharfenberg CD, Löhnert B, Bottlender M. New possibilities in treatment and rehabilitation of alcohol-dependent patients – a catamnestic study on the efficiency of outpatient treatment programmes demonstrated by a model procedure. Nervenarzt. 2003;74:226–34. doi: 10.1007/s00115-002-1398-9. [DOI] [PubMed] [Google Scholar]
- 12.Gordon SM, Sterling R, Siatkowski C, Raively K, Weinstein S, Hill PC, et al. Inpatient desire to drink as a predictor of relapse to alcohol use following treatment. Am J Addict. 2006;15:242–5. doi: 10.1080/10550490600626556. [DOI] [PubMed] [Google Scholar]
- 13.Evren C, Cetin R, Durkaya M, Dalbudak E. Clinical variables related with relapse during 6 month follow-up in male alcohol dependents. Clin Psychopharmacol Bull. 2010;20:14–22. [Google Scholar]
- 14.Boothby LA, Doering PL. Acamprosate for the treatment of alcohol dependence. Clin Ther. 2005;27:695–714. doi: 10.1016/j.clinthera.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 15.Evren C, Durkaya M, Dalbudak E, Çelik S, Çetin R, Çakmak D. Factors related with relapse in male alcohol dependents: 12 months follow-up study. Dusunen Adam. 2010;23:92. [Google Scholar]
- 16.Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62:211–20. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- 17.Verheul R, van den Brink W, Geerlings P. A three-pathway psychobiological model of craving for alcohol. Alcohol Alcohol. 1999;34:197–222. doi: 10.1093/alcalc/34.2.197. [DOI] [PubMed] [Google Scholar]
- 18.O'Connor PG, Gottlieb LD, Kraus ML, Segal SR, Horwitz RI. Social and clinical features as predictors of outcome in outpatient alcohol withdrawal. J Gen Intern Med. 1991;6:312–6. doi: 10.1007/BF02597427. [DOI] [PubMed] [Google Scholar]
- 19.Boening JA, Lesch OM, Spanagel R, Wolffgramm J, Narita M, Sinclair D, et al. Pharmacological relapse prevention in alcohol dependence: From animal models to clinical trials. Alcohol Clin Exp Res. 2001;25:127S–31S. doi: 10.1097/00000374-200105051-00022. [DOI] [PubMed] [Google Scholar]
- 20.Soyka M, Chick J. Use of acamprosate and opioid antagonists in the treatment of alcohol dependence: A European perspective. Am J Addict. 2003;12(Suppl 1):S69–80. doi: 10.1111/j.1521-0391.2003.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 21.Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug Alcohol Depend. 2009;103:131–6. doi: 10.1016/j.drugalcdep.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McHugh RK, Fitzmaurice GM, Griffin ML, Anton RF, Weiss RD. Association between a brief alcohol craving measure and drinking in the following week. Addiction. 2016;111:1004–10. doi: 10.1111/add.13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chandiramani K, Tripathi BM. Psycho-educational group therapy for alcohol and drug dependence recovery. Indian J Psychiatry. 1993;35:169–72. [PMC free article] [PubMed] [Google Scholar]
- 24.De Sousa A, De Sousa A. A one-year pragmatic trial of naltrexone vs. disulfiram in the treatment of alcohol dependence. Alcohol Alcohol. 2004;39:528–31. doi: 10.1093/alcalc/agh104. [DOI] [PubMed] [Google Scholar]
- 25.de Sousa A, de Sousa A. An open randomized study comparing disulfiram and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2005;40:545–8. doi: 10.1093/alcalc/agh187. [DOI] [PubMed] [Google Scholar]
- 26.De Sousa AA, De Sousa J, Kapoor H. An open randomized trial comparing disulfiram and topiramate in the treatment of alcohol dependence. J Subst Abuse Treat. 2008;34:460–3. doi: 10.1016/j.jsat.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Narayana PL, Gupta AK, Sharma PK. Use of anti-craving agents in soldiers with alcohol dependence syndrome. Med J Armed Forces India. 2008;64:320–4. doi: 10.1016/S0377-1237(08)80009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mishra BR, Nizamie SH, Das B, Praharaj SK. Efficacy of repetitive transcranial magnetic stimulation in alcohol dependence: A sham-controlled study. Addiction. 2010;105:49–55. doi: 10.1111/j.1360-0443.2009.02777.x. [DOI] [PubMed] [Google Scholar]
- 29.Lohit K, Kulkarni C, Galgali RB. Factors influencing adherence to anti-craving medications and drinking outcomes in patients with alcohol dependence: A hospital-based study. J Pharmacol Pharmacother. 2016;7:72–9. doi: 10.4103/0976-500X.184770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta M, Verma P, Rastogi R, Arora S, Elwadhi D. Randomized open-label trial of baclofen for relapse prevention in alcohol dependence. Am J Drug Alcohol Abuse. 2017;43:324–31. doi: 10.1080/00952990.2016.1240797. [DOI] [PubMed] [Google Scholar]
- 31.Dhawan A, Kumar R, Yadav S, Tripathi BM. The enigma of craving. Indian J Psychiatry. 2002;44:138–43. [PMC free article] [PubMed] [Google Scholar]
- 32.Murthy P, Manjunatha N, Subodh BN, Chand PK, Benegal V. Substance use and addiction research in India. Indian J Psychiatry. 2010;52:S189–99. doi: 10.4103/0019-5545.69232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deshpande SN, Mathur MN, Das SK, Bhatia T, Sharma S, Nimgaonkar VL, et al. A Hindi version of the diagnostic interview for genetic studies. Schizophr Bull. 1998;24:489–93. doi: 10.1093/oxfordjournals.schbul.a033343. [DOI] [PubMed] [Google Scholar]
- 34.Nurnberger JI, Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J. Diagnostic interview for genetic studies Rationale, unique features, and training NIMH genetics initiative. Arch Gen Psychiatry. 1994;51:849–59. doi: 10.1001/archpsyc.1994.03950110009002. [DOI] [PubMed] [Google Scholar]
- 35.Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar) Addiction. 1989 Nov 1;84(11):1353–7. doi: 10.1111/j.1360-0443.1989.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 36.Stockwell T, Hodgson R, Edwards G, Taylor C, Rankin H. The development of a questionnaire to measure severity of alcohol dependence. Br J Addict Alcohol Other Drugs. 1979;74:79–87. doi: 10.1111/j.1360-0443.1979.tb02415.x. [DOI] [PubMed] [Google Scholar]
- 37.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res. 1999;23:1289–95. [PubMed] [Google Scholar]
- 38.Released. Armonk, NY: IBM Corp; 2012. IBM Corp. BM SPSS Statistics for Windows, Version 21.0. [Google Scholar]
- 39.Hillemacher T, Bayerlein K, Wilhelm J, Poleo D, Frieling H, Ziegenbein M, et al. Volume intake and craving in alcohol withdrawal. Alcohol Alcohol. 2006;41:61–5. doi: 10.1093/alcalc/agh235. [DOI] [PubMed] [Google Scholar]
- 40.Yates WR, Booth BM, Reed DA, Brown K, Masterson BJ. Descriptive and predictive validity of a high-risk alcoholism relapse model. J Stud Alcohol. 1993;54:645–51. doi: 10.15288/jsa.1993.54.645. [DOI] [PubMed] [Google Scholar]


