Abstract
Objective
To evaluate the association between total medical contact, prehospital, and emergency department delays in antibiotic administration and in-hospital mortality among patient encounters with community-acquired sepsis.
Design
Retrospective cohort study.
Setting
Nine hospitals served by 21 emergency medical services agencies in southwestern Pennsylvania from 2010 through 2012.
Patients
All emergency medical services encounters with community acquired sepsis transported to the hospital.
Measurements and Main Results
Among 58,934 prehospital encounters, 2,683 had community-acquired sepsis, with an inhospital mortality of 11%. Median time from first medical contact to antibiotic administration (total medical contact delay) was 4.2 hours (interquartile range, 2.7–8.0 hr), divided into a median pre-hospital delay of 0.52 hours (interquartile range, 0.40–0.66 hr) and a median emergency department delay of 3.6 hours (inter-quartile range, 2.1–7.5 hr). In a multivariable analysis controlling for other risk factors, total medical contact delay was associated with increased in-hospital mortality (adjusted odds ratio for death, 1.03 [95% CI, 1.00–1.05] per 1-hr delay; p < 0.01), as was emergency department delay (p = 0.04) but not prehospital delay (p = 0.61).
Conclusions
Both total medical contact and emergency department delay in antibiotic administration are associated with inhospital mortality in community-acquired sepsis.
Keywords: antibiotic, prehospital care, sepsis, timing
Prompt administration of antibiotics is associated with improved outcomes in sepsis and septic shock. Every 1-hour delay in antibiotics after emergency department (ED) triage or the onset of organ dysfunction or shock may lead to a 3–7% increase in the odds of a poor outcome (1–3). But the association between timing of antibiotics with outcome may not be linear, as a recent meta-analysis showed no benefit to antibiotic administration within 3 hours of either ED triage or onset of organ dysfunction (4). Despite these uncertainties, multiple quality improvement initiatives designed to increase timely antibiotic administration in sepsis are underway, including a recently implemented program by the U.S. Centers for Medicare and Medicare Services. The benefits and drawbacks of such programs are widely debated (5, 6), with discussion focusing on whether time delays matter, how to measure them, and whether efforts to increase antibiotic timeliness may lead to antibiotic overuse.
One important challenge in the benchmarking of treatment delays is the definition of the starting point for care. The arrival to the ED is typically considered a “time zero,” yet more than 50% of sepsis patients are transported by emergency medical services (EMS) prior to hospital arrival (7). This means that modifiable delays in antibiotic administration could begin much sooner, and quality improvement initiatives designed to minimize ED or hospital time to antibiotics may miss opportunities to speed antibiotic administration and influence outcome. Yet the time from first healthcare contact to antibiotic administration in sepsis, termed “total medical contact delay,” is incompletely understood.
We sought to describe the association between total medical contact delay and in-hospital mortality among community-acquired sepsis patients in a large retrospective cohort. We analyzed data on total medical contact, prehospital, and ED delays from 21 EMS agencies linked to electronic health records (EHRs) at nine hospitals in southwestern Pennsylvania.
METHODS
Study Design
We performed a retrospective study using prehospital and hospital data from 21 EMS agencies and nine hospitals in southwestern Pennsylvania from January 1, 2010, to December 31, 2012. All EMS agencies received medical oversight from faculty at a single academic center, and each used a single electronic patient record that captures detailed information on dispatch, scene, and transport care (emsCharts; Warrendale, PA). The prehospital date/time stamps and hospital arrival times are logged in a Computer Aided Dispatch (CAD) program that is integrated with 9-1-1 dispatch. These data are entered in real-time based on computer-generated data and audio communications from the responding units. The CAD data are automatically uploaded into the prehospital patient care report in “emsCharts” upon initial creation of the patient care record. All study hospitals are part of UPMC, an integrated health system with a shared EHR (Cerner PowerChart; Cerner, Kansas City, MO). We linked encounters in emsCharts if transported to a UPMC hospitals using a hierarchical direct matching algorithm based on personal identifiers, as previously described (8). This seven-step match process using MS SQL Server 2010 (Microsoft, Redmond, WA) includes first name, last name, social security number, date of birth, date/time of incident, and hospital destination and was previously manually validated in 100 records. The final database included detailed prehospital data from emsCharts and vital signs, medications, laboratory values, microbiology, health-care utilization, and outcomes from the UPMC EHR. The institutional review board of the University of Pittsburgh approved the study design and deemed the study to pose minimal risk to participants, waiving the need for individual informed consent.
Patient Selection
Eligible encounters included those older than 17 years transported by ground ambulance from any location to a UPMC hospital with community-acquired sepsis. We defined “community-acquired sepsis” as instances in which encounters met criteria for suspected infection and organ dysfunction within 24 hours of ED arrival according to the Third International Consensus Sepsis Definitions (Sepsis-3) (9, 10). We defined “suspected infection” as the presence of both antibiotic administration (oral or parenteral) and a body fluid culture obtained (blood, urine, cerebrospinal fluid, etc). We defined “organ dysfunction” as having a total Sepsis-Related Organ Failure Assessment (SOFA) score of greater than or equal to 2 points within 24 hours of meeting infection criteria (10).
Variables
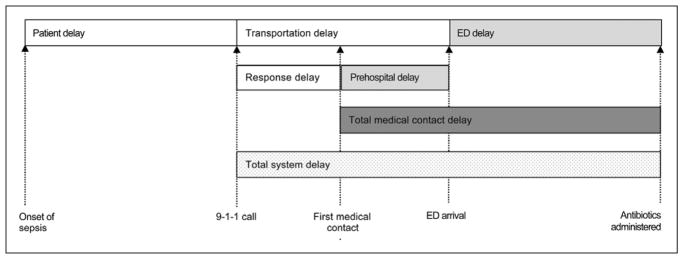
The primary outcome was in-hospital mortality. The primary exposure was the total medical contact delay in antibiotic administration, defined as the time in hours from first medical contact (from emsCharts) until the first antibiotic administration (from hospital EHR data). The “first medical contact” was defined by the time at patient side, and if not available, time of arrival at the referring location (in < 10% of encounters). Secondary exposures included: 1) prehospital delay, defined as the time in hours from first medical contact by EMS until the time of ED arrival; 2) response delay, defined as the time in hours from 9-1-1 activation to arrival at patient side; and 3) ED delay, defined as the time in hours from ED arrival to the first antibiotic administration in the hospital EHR data (Fig. 1) (11). We also performed analyses in which the exposure of interest was total system delay, defined as the total time in hours from the 9-1-1 notification until the first antibiotic administration (11). We did not study patient delay, as symptom recall and timing of sepsis onset prior to 9-1-1 activation are subject to recall bias.
Figure 1.
Delays in antibiotic administration in sepsis. ED = emergency department.
We included a priori identified covariates as potential confounders between medical contact delay and outcome based on prior studies. These were: demographic factors including age, race (black, white, other), and sex; comorbidity burden defined using a weighted Charlson score derived from International Classification of Diseases, 9th Edition, clinical modification codes; measures of prehospital illness severity including initial clinical assessments (heart rate, respiratory rate, systolic blood pressure, oxygen saturation, and Glasgow Coma Scale score) and use of lights and siren during transport; and use of selected prehospital treatments that are not only markers of illness severity but also may prolong scene time leading to longer system delays (bag mask ventilation, endotracheal intubation, electrocardiogram, or supplemental oxygen) (12–16).
Statistical Analysis
We described demographic and clinical characteristics of EMS encounters categorized by discrete intervals of medical contact delay (0 to ≤ 6, > 6 to ≤ 12, and > 12 hr) to illustrate the cohort. We used mean (SD) or median (interquartile range [IQR]) as appropriate to normality and used proportions for categorical variables. We modeled the association between delays and inhospital mortality using logistic regression adjusted for covariates specified as potential confounders, as described above. We modeled all categorical variables as indicator covariates. We modeled all continuous variables as linear covariates after a preliminary evaluation using fractional polynomials did not uncover any nonlinear relationships over the first 24 hours of the encounter (17). We used generalized estimating equations with robust variance estimators to account for hospital-level clustering. We assumed missing data were conditional on observed covariates, and we performed multiple imputation for all missing values using multiple imputation by chained equations (18). All models were run on 11 imputed datasets and the resulting risk estimates were combined using Rubin’s rules. Additional methodologic detail regarding imputation is provided in the online supplement (Supplemental Digital Content 1, http://links.lww.com/CCM/C371). We present our results as both odds ratios and as the predictive margins adjusted for covariates and specified for a typical patient of 40 and 70 years old (19).
Sensitivity Analyses
We performed several sensitivity analyses to assess the robustness of our results to key analytic assumptions. To examine the consistency of our findings across different criteria for sepsis, we repeated the analyses using three alternate criteria: 1) physiology-based criteria adapted from international guidelines (any of systolic blood pressure, ≤ 90 mm Hg; serum lactate, ≥ 2.0 mmol/L; Pao2/Fio2 ratio, ≤ 250; serum creatinine, > 2.0 mg/dL; total bilirubin, > 2.0 mg/dL; platelet count, < 100,000 μL; or international normalized ratio, > 1.5 in the setting of infection) (20); 2) more stringent criteria for suspected infection (at least two doses of antibiotics in the first 96 hr after ED arrival); and 3) more stringent criteria for organ dysfunction (three or more SOFA points) (21). We also repeated the analysis limiting the cohort to only those patients with evidence of physiologic compromise during prehospital care (either respiratory rate, ≥ 22 breaths/min; systolic blood pressure, ≤ 100 mm Hg; or Glasgow Coma Scale score, < 15, which corresponds to one or more qualified SOFA [qSOFA] points) (22). All analyses were performed with STATA 13.0 (StataCorp, College Station, TX). All tests of significance used a two-sided p value of less than or equal to 0.05.
RESULTS
Characteristics of Patients
Of 58,934 adult EMS encounters transported to UPMC hospitals, 48,411 did not have suspected infection within 24 hours (82%), and 7,686 had suspected community infection but no evidence of organ dysfunction (13%) (Fig. 2). The final cohort contained 2,683 encounters with community-acquired sepsis, with a median time from first medical contact to antibiotic administration of 4.2 hours (IQR, 2.7–8.0 hr). This delay comprised a median prehospital delay of 0.52 hours (IQR, 0.40–0.66 hr) and median ED delay of 3.6 hours (IQR, 2.1–7.5 hr). Examining clinical and demographic characteristics across categories of medical contact delay (Table 1), we found few differences with respect to age, gender, baseline comorbidities, and proportion with limitations to life-sustaining care. Encounters with a shorter medical contact delay were more often transported by lights and siren, more likely to receive selected prehospital interventions (e.g., supplemental oxygen, IV catheter), and more likely to be admitted to intensive care. The unadjusted in-hospital mortality was 11%, 10%, and 14% for medical contact delays 0–6, 6–12, and more than 12 hours, respectively.
Figure 2.

Patient accrual. EMS = emergency medical services.
TABLE 1.
Characteristics of Patients With Community-Acquired Sepsis Transported by Emergency Medical Services and Administered Antibiotics, Stratified by Total Medical Contact Delay (n = 2,683)
| Characteristic | Total Medical Contact Delay, hr | p | ||
|---|---|---|---|---|
|
| ||||
| 0–6 | 6–12 | ≥12 | ||
| n | 1,742 | 610 | 331 | |
|
| ||||
| Age, yr, mean (SD) | 68 (18) | 64 (19) | 65 (19) | 0.15 |
|
| ||||
| Male sex, n (%) | 814 (47) | 271 (44) | 142 (43) | 0.34 |
|
| ||||
| White race, n (%) | 1,371 (79) | 478 (78) | 268 (81) | 0.61 |
|
| ||||
| Weighted Charlson sum, mean (SD) | 1.4 (1.6) | 1.4 (1.6) | 1.3 (1.5) | 0.09 |
|
| ||||
| Surgery prior to suspected infection, n (%) | 141 (8) | 81 (13) | 46 (14) | < 0.01 |
|
| ||||
| Prehospital vital signs | ||||
| Systolic blood pressure, mm Hg, mean (SD) | 120 (31) | 119 (30) | 126 (29) | 0.30 |
| Respiratory rate, breaths/min, mean (SD) | 22 (7) | 21 (6) | 20 (5) | < 0.01 |
| Heart rate, beats/min, mean (SD) | 103 (25) | 100 (24) | 96 (23) | 0.07 |
| Glasgow Coma Scale score, mean (SD) | 12.4 (4) | 12.1 (5) | 12.4 (4) | 0.04 |
| O2 saturation, %, mean (SD) | 90 (11) | 92 (9) | 93 (8) | < 0.01 |
|
| ||||
| Prehospital interventions, n (%) | ||||
| Intubation | 63 (5) | 38 (8) | 27 (11) | < 0.01 |
| Peripheral IV catheter | 764 (62) | 268 (62) | 134 (53) | 0.03 |
| Supplemental O2 | 741 (60) | 238 (55) | 120 (48) | < 0.01 |
| Electrocardiogram performed | 168 (14) | 47 (11) | 29 (12) | 0·27 |
| Lights and sirens transport | 534 (31) | 161 (26) | 80 (24) | 0.02 |
|
| ||||
| Distance to hospital, miles, mean (SD) | 6.9 (6.4) | 8.7 (9.3) | 8.1 (8.5) | < 0.01 |
|
| ||||
| Hospital physiology on day 1, mean (SD) | ||||
| Maximum systemic inflammatory response syndrome criteria | 1.9 (1.1) | 2.0 (1.1) | 1.9 (1.2) | 0.27 |
| Maximum Sepsis-Related Organ Failure Assessment score | 4.3 (2.8) | 4.4 (3.0) | 4.1 (2.6) | < 0.01 |
|
| ||||
| Healthcare utilization, n (%) | ||||
| ICU | 1,474 (85) | 497 (81) | 251 (76) | < 0.01 |
| Mechanical ventilation within 24 hr | 461 (26) | 171 (28) | 103 (31) | 0.20 |
| Vasopressors within 24 hr | 278 (16) | 87 (14) | 41 (12) | 0.20 |
|
| ||||
| In-hospital mortality, n (%) | 193 (11) | 58 (10) | 47 (14) | 0.09 |
Total Medical Contact Delay and Mortality
In a multivariable model that included a priori confounders (Table 2), total medical contact delay was associated with greater in-hospital mortality (odds ratio of death for each hour of medical contact delay, 1.03; 95% CI, 1.01–1.05; p < 0.01). A model testing total system delay (the time from 9-1-1 notification to antibiotic administration) found a similar association as the primary analysis (odds ratio of death for each hour of system delay, 1.03; 95% CI, 1.00–1.05; p = 0.03). In a model separating all components of system delay (response delay, prehospital delay, and ED delay), we found that response delay (odds ratio of death for each hour of response delay, 2.34; 95% CI, 0.80–6.9; p = 0.12) and prehospital delay were not independently associated with in-hospital mortality (odds ratio of death for each hour of prehospital delay, 1.14; 95% CI, 0.60–2.16; p = 0·70), whereas ED delay remained independently associated with in-hospital mortality (odds ratio of death for each hour of ED delay, 1.03; 95% CI, 1.00–1.05; p = 0.04).
TABLE 2.
Regression Analysis of Total Medical Contact Delay and A Priori Covariates Associated With In-Hospital Mortality in Community-Acquired Sepsis Patients Treated With Antibiotics
| Covariate | OR (95% CI) | p |
|---|---|---|
| Total medical contact delay, by hour | 1.03 (1.01–1.05) | 0·02 |
|
| ||
| Age, yra | 1.02 (1.02–1.03) | < 0.01 |
|
| ||
| Male gender | 1.22 (0.92–1.62) | 0.16 |
|
| ||
| Race | ||
| Other | Ref | |
| Black | 1.69 (1.06–2.68) | 0.03 |
| White | 1.94 (1.26–3.00) | < 0.01 |
|
| ||
| Weighted Charlson suma | 1.14 (1.08–1.21) | < 0.01 |
|
| ||
| Prehospital vital signs | ||
| Glasgow Coma Scale score | 0.95 (0.90–1.01) | 0.11 |
| Heart rate | 1.00 (1.00–1.01) | 0.58 |
| Respiratory rate | 0.99 (0.97–1.01) | 0.53 |
| O2 saturation | 0.99 (0.98–1.01) | 0.51 |
| Systolic blood pressure | 0.99 (0.98–0.99) | < 0.01 |
|
| ||
| Prehospital interventions | ||
| Endotracheal intubation | 1.90 (0.73–4.96) | 0.19 |
| Electrocardiogram | 0.97 (0.62–1.49) | 0.88 |
| Supplemental O2 | 0.88 (0.66–1.16) | 0.37 |
| IV fluid administration | 0.95 (0.61–1.48) | 0.81 |
|
| ||
| EMS urgencyb | 2.51 (1.53–4.11) | < 0.01 |
OR = odds ratio.
Odds ratio corresponds to a one unit change in either age (years) or weighted Charlson sum.
Emergency medical services urgency defined as transported with lights and sires versus not (0/1).
In analyses of cohorts with alternate criteria for sepsis, we found that using a more specific definition of infection (≥ 2 doses of antibiotics within 96 hr; n = 2,101) did not change the association of medical contact delay and hospital mortality (odds ratio of death for each hour of medical contact delay, 1.03; 95% CI, 1.00–1.06; p = 0·04). When we defined organ dysfunction as greater than or equal to three SOFA points (n = 1,782) or defined sepsis using international guideline criteria (n = 4,625), the results were also unchanged. The association between medical contact delay and in-hospital mortality was similar in sepsis encounters who already had abnormal qSOFA points (n = 1,354) (Fig. 3).
Figure 3.
Association between medical contact delay and in-hospital mortality in community-acquired sepsis. The Surviving Sepsis campaign (SSC) criteria for organ dysfunction that were measurable in our electronic health record extract included: hypotension (SBP, ≤ 90 mm Hg), lactate greater than or equal to 2.0 mmol/L, Pao2/Fio2 ratio less than or equal to 250, serum creatinine greater than 2.0 mg/dL, total bilirubin greater than 2.0 mg/dL, platelet count less than 100,000 μL, or international normalized ratio greater than 1.5. OR = odds ratio, SBP = systolic blood pressure, SOFA = Sepsis-Related Organ Failure Assessment score.
We illustrate the model predicted probability of inhospital mortality across a range of medical contact delay (in hours) for typical 40- and 70-year-old subjects in the primary cohort of community sepsis (eFig. 1, Supplemental Digital Content 1, http://links.lww.com/CCM/C371). This analysis demonstrates an increase in the risk of in-hospital mortality across the range of total medical contact delay for both young and old encounters.
DISCUSSION
In a retrospective cohort study of community-acquired sepsis encounters transported by EMS, we observed an association between delay from first medical contact to antibiotic administration and in-hospital mortality. The association of greater medical contact delay (the total modifiable time after health-care contact prior to antibiotics) with increased risk-adjusted in-hospital mortality was robust to alternate criteria for infection, organ dysfunction, and prehospital illness severity.
A key component of guideline-recommended care in sepsis is the early administration of appropriate antibiotics (20). However, when measuring delays in antibiotic administration, there are many options for when the clock starts (23). Among options that use a fixed time point, we consider: 1) the time of first medical contact during prehospital care or 2) the time of arrival to the ED. They are both objective and typically captured in EHR data, but they have important differences. The time from first medical contact by EMS measures more accurately reflects the moment when a patient with suspected sepsis enters the healthcare system. However, it is difficult to routinely capture, since it requires linking of data from both EMS systems and hospitals. In contrast, ED delay is a simpler measure based on a single time interval at a single facility. However, it may miss an important and modifiable time in the system of care. Our analysis adds new data that the first medical contact delay is both substantial and associated with in-hospital mortality.
There are many potential approaches to reduce total medical contact delay in sepsis. First, greater awareness and education about sepsis for first responders could lead to earlier diagnosis, allowing for earlier treatment and advanced notification to hospitals. Recent consensus sepsis definitions propose various clinical prompts among infected patients likely to be septic that could be tested prospectively during prehospital care (22). If accurate criteria for both infection and organ dysfunction are validated, they could inform prehospital sepsis alerts for testing in randomized trials. The results herein were furthered strengthened in that the association between medical contact delays and outcome were robust to alternate criteria for sepsis. Second, total medical contact delays in antibiotic administration could be reduced through triage to centers of excellence in sepsis care. Our data do not explicitly support that EMS providers ought to “drive faster,” in that response and prehospital delays were not statistically significant. But we note observational data suggest that ED or hospital care of sepsis at high-volume centers may improve risk-adjusted mortality, perhaps by improving early processes of care (24, 25). Finally, total medical contact delay could be reduced if EMS directly administered prehospital antibiotics to high-risk septic patients, rather than delaying until arrival in the ED. Such a strategy is analogous to direct prehospital therapy for stroke, trauma, or myocardial infarction, and is undergoing evaluation in clinical trials (NCT01988428). There are many barriers facing such trials, including reliable, low cost, accurate strategies to identify prehospital patients at greatest risk for sepsis, feasibility of obtaining body fluid cultures, assessing for safety and medication allergies, and managing downstream care in the ED.
Based on our findings, it is also reasonable for health systems to consider routinely measuring total medical contact delay in sepsis. To do this, it would be necessary to routinely link prehospital data to hospital EHRs. We acknowledge that limitations to this goal are logistic, regulatory, and bioinformatics barriers in creating EMS to hospital linkages that are sustainable and generalizable across health systems. Despite the challenges underlying such an effort, furthering prehospital-hospital partnerships offers an opportunity to further sepsis education and awareness of clinicians participating in prehospital care. A more collective approach to the system of sepsis care could also lead to quality metrics that span the typical silos of emergency care. By encouraging and incentivizing providers with different training and expertise to focus on sepsis, important delays may be avoided.
We note several limitations to our analysis. First, we included only sepsis encounters transported by EMS, a distinct subgroup who maybe more acutely ill than comparable encounters transported by other means, and our results are not generalizable to these other cohorts (26). We also included patients receiving unmeasured medical treatment or antibiotics at out-of-hospital locations, such as skilled nursing facilities or long-term acute care. Second, we were unable to study encounters diagnosed as “septic” at the moment of first medical contact, as no objective and reliable criteria exist for sepsis on presentation. We tested, however, a variety of criteria for community-acquired sepsis during the first 24 hours after arrival to the ED. We recognize that criteria for sepsis using the SOFA score may also include patients with chronic organ dysfunction such as end-stage renal disease or cirrhosis. Therefore, we conducted sensitivity analyses among patients with evidence of physiologic compromise during prehospital care (elevated qSOFA), with no change in the results. Third, we did not study time intervals in an episode-of-illness framework. For example, time delays in the hospital can be measured from the onset of symptoms (i.e., hypotension or new organ dysfunction) rather than a fixed time point. The onset and course of sepsis symptoms prior to prehospital care are variable, subject to patient recall, and unavailable in current data. Another source of error could derive from the missing data for prehospital times; yet, among only 10% of encounters were first medical contact the time at the referring location instead of the time at the patient’s side. Prehospital times may also have been systematically logged differently by transporting EMS agencies on arrival to different hospitals. Thus, we used clustering techniques at the hospital level in regression models, with agency-specific analyses as an important future direction. We did not determine the appropriateness of either the antibiotic selection or the antibiotic dose. Appropriate antibiotics are typically defined by the subsequently identified organism in culture and pattern of susceptibility, data available in a minority of patients with suspected sepsis (22).
CONCLUSIONS
Both total medical contact and ED delay in antibiotic administration are associated with greater in-hospital mortality in patients with community-acquired sepsis. These findings suggest that interventions aimed at reducing modifiable delays in the system of sepsis care are a potential target for further study.
Supplementary Material
Acknowledgments
Supported, in part, by a grant from the National Institutes of Health (primary investigator: Dr. Seymour, K23GM104022).
Dr. Seymour’s institution received funding from the National Institutes of Health (NIH)/National Institute of General Medical Sciences. He received funding from Beckman Coulter, Cytovale, and Edwards. He received support for article research from the NIH. Dr. Kahn’s institution received funding from U.S. Department of Health and Human Services (NIH and Health Resources & Services Administration) and Gordon and Betty Moore Foundation. Dr. Callaway received support for article research from NIH. Dr. Yealy received funding from American College of Emergency Physicians (editorial stipend), Lippincott (royalties), UpToDate (royalties), Oxford University Press (royalties), and from multiple legal firms (expert opinion). Dr. Scales institution received funding from Canadian Institute for Health Research (operating grants). He received funding from Physicians’ Services Incorporated Foundation (Fellowship in Translational Health Research). Dr. Angus received funding from Bayer HealthCare, Ferring Pharmaceuticals, and GlaxoSmithKline.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Martin-Gill has disclosed that he does not have any potential conflicts of interest.
References
- 1.Kumar A, Haery C, Paladugu B, et al. The duration of hypotension before the initiation of antibiotic treatment is a critical determinant of survival in a murine model of Escherichia coli septic shock: Association with serum lactate and inflammatory cytokine levels. J Infect Dis. 2006;193:251–258. doi: 10.1086/498909. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 3.Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit Care Med. 2014;42:1749–1755. doi: 10.1097/CCM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 4.Sterling SA, Miller WR, Pryor J, et al. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: A systematic review and meta-analysis. Crit Care Med. 2015;43:1907–1915. doi: 10.1097/CCM.0000000000001142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooke CR, Iwashyna TJ. Sepsis mandates: Improving inpatient care while advancing quality improvement. JAMA. 2014;312:1397–1398. doi: 10.1001/jama.2014.11350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rhee C, Gohil S, Klompas M. Regulatory mandates for sepsis care–reasons for caution. N Engl J Med. 2014;370:1673–1676. doi: 10.1056/NEJMp1400276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seymour CW, Rea TD, Kahn JM, et al. Severe sepsis in pre-hospital emergency care: Analysis of incidence, care, and outcome. Am J Respir Crit Care Med. 2012;186:1264–1271. doi: 10.1164/rccm.201204-0713OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seymour CW, Kahn JM, Martin-Gill C, et al. Creating an infrastructure for comparative effectiveness research in emergency medical services. Acad Emerg Med. 2014;21:599–607. doi: 10.1111/acem.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 10.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Terkelsen CJ, Sørensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 12.Seymour CW, Kahn JM, Cooke CR, et al. Prediction of critical illness during out-of-hospital emergency care. JAMA. 2010;304:747–754. doi: 10.1001/jama.2010.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seymour CW, Cooke CR, Hebert PL, et al. Intravenous access during out-of-hospital emergency care of noninjured patients: A population-based outcome study. Ann Emerg Med. 2012;59:296–303. doi: 10.1016/j.annemergmed.2011.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seymour CW, Cooke CR, Heckbert SR, et al. Prehospital systolic blood pressure thresholds: A community-based outcomes study. Acad Emerg Med. 2013;20:597–604. doi: 10.1111/acem.12142. [DOI] [PubMed] [Google Scholar]
- 15.Tobias AZ, Guyette FX, Seymour CW, et al. Pre-resuscitation lactate and hospital mortality in prehospital patients. Prehosp Emerg Care. 2014;18:321–327. doi: 10.3109/10903127.2013.869645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seymour CW, Cooke CR, Heckbert SR, et al. Prehospital intravenous access and fluid resuscitation in severe sepsis: An observational cohort study. Crit Care. 2014;18:533. doi: 10.1186/s13054-014-0533-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Royston P, Sauerbrei W. Building multivariable regression models with continuous covariates in clinical epidemiology–with an emphasis on fractional polynomials. Methods Inf Med. 2005;44:561–571. [PubMed] [Google Scholar]
- 18.Royston P. Multiple imputation of missing values. Stat J. 2004;4:227–241. [Google Scholar]
- 19.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stat J. 2012;12:308–331. [Google Scholar]
- 20.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup: Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 21.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 22.Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puskarich MA, Trzeciak S, Shapiro NI, et al. Emergency Medicine Shock Research Network (EMSHOCKNET): Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit Care Med. 2011;39:2066–2071. doi: 10.1097/CCM.0b013e31821e87ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walkey AJ, Wiener RS. Hospital case volume and outcomes among patients hospitalized with severe sepsis. Am J Respir Crit Care Med. 2014;189:548–555. doi: 10.1164/rccm.201311-1967OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banta JE, Joshi KP, Beeson L, et al. Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005–2010. Crit Care Med. 2012;40:2960–2966. doi: 10.1097/CCM.0b013e31825bc92f. [DOI] [PubMed] [Google Scholar]
- 26.Band RA, Gaieski DF, Hylton JH, et al. Arriving by emergency medical services improves time to treatment endpoints for patients with severe sepsis or septic shock. Acad Emerg Med. 2011;18:934–940. doi: 10.1111/j.1553-2712.2011.01145.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.